Abstract
Objective
To evaluate the hepatoprotective and immunotherapeutic effects of aqueous extract of turmeric rhizome in CCl4 intoxicated Swiss albino mice.
Methods
First group of mice (n=5) received CCl4 treatment at a dose of 0.5 mL/kg bw (i.p.) for 7 days. Second group was fed orally the aqueous extract of turmeric at a dose of 50 mg/kg bw for 15 days. The third group was given both the turmeric extract (for 15 days, orally) and CCl4 (for last 7 days, i.p.). The fourth group was kept as a control. To study the liver function, the transaminase enzymes (SGOT and SGPT) and bilirubin level were measured in the serum of respective groups. For assaying the immunotherapeutic action of Curcuma longa (C. longa), non specific host response parameters like morphological alteration, phagocytosis, nitric oxide release, myeloperoxidase release and intracellular killing capacity of peritoneal macrophages were studied from the respective groups.
Results
The result of present study suggested that CCl4 administration increased the level of SGOT and SGPT and bilirubin level in serum. However, the aqueous extract of turmeric reduced the level of SGOT, SGPT and bilirubin in CCl4 intoxicated mice. Apart from damaging the liver system, CCl4 also reduced non specific host response parameters like morphological alteration, phagocytosis, nitric oxide release, myeloperoxidase release and intracellular killing capacity of peritoneal macrophages. Administration of aqueous extract of C. longa offered significant protection from these damaging actions of CCl4 on the non specific host response in the peritoneal macrophages of CCl4 intoxicated mice.
Conclusions
In conclusion, the present study suggests that C. longa has immunotherapeutic properties along with its ability to ameliorate hepatotoxicity.
Keywords: Immune system, Hepatotoxicity, Curcuma longa, Immunotherapeutic agents, Hepatoprotectivity, Turmeric rhizome, Hepatoxicity, Transaminase enzyme, Liver function, Bilirubin, Nitric oxide, Morphological alteration
1. Introduction
The liver is the main organ responsible for the biosynthesis, uptake and degradation of proteins and enzymes. Liver function may therefore be reflected to some extent on the levels and/or the activities of these circulating biochemical compounds. The immune system is increasingly found to be involved in the development of several chronic illnesses, for which allopathic medicine has provided limited tools for treatment and especially prevention. In that context, it appears worthwhile to target the immune system in order to modulate the risk of certain chronic illnesses. Meanwhile, natural health products (NHPs) are generating renewed interest, particularly in the prevention and treatment of several chronic diseases. Herbal drugs are known to posses immunomodulatory properties and generally act by stimulating or suppressing both specific and non-specific immunity[1].
Turmeric is the dried rhizome powder of Curcuma longa (C. longa), a perennial herb of the Zingiberaceae family. C. longa is cultivated extensively in Asia (India and China). The major chemical principles of turmeric are curcuminoids, which impart characteristic yellow colour to it.
Previous works have shown that C. longa inhibited the growth of activity of some bacteria and fungi[2],[3]. Turmeric extract was found to possess in vitro free radical scavenging, ROS scavenging ability and cell proliferation activity in cell line[4]. Curcumin seems to regulate the immune function of mice in a dose-dependent fashion as curcumin treatment enhanced the phagocytosis of peritoneal macrophages and differentially regulates the proliferation of splenocytes[5]. The effect of curcumin in Alzheimer's disease is mediated through the downmodulation of cytokine (i.e. TNF-α and IL-1β) and chemokine (i.e. MIP-1b, MCP-1, and IL-8) activity in peripheral blood monocytes and reduces amyloid-β plaque formation[6]–[8]. Curcumin treatment modulates cellular and humoral immune responses of infected mice and leads to a significant reduction of parasite burden and liver pathology in acute murine schistosomiasis mansoni[9]. Curcumin also downregulates matrix metalloproteinase (MMP)-2 and upregulates tissue inhibitor of metalloproteinase (TIMP)-1, two common effectors molecules involved in cell invasion[10]. In one study, it was reported that postnatal modulation of hepatic biotransformation system enzymes via translactational exposure of F1 mouse pups to turmeric and curcumin[11].
Curcumin has been found to modulate the growth and cellular response of various cell types of the immune system. Numerous lines of evidence suggest that curcumin can modulate both the proliferation and the activation of T cells. Curcumin inhibited the proliferation induced by concanavalin A (Con A), phytohemagglutinin (PHA), and phorbol-12- myristate-13-acetate (PMA) of lymphocytes derived from fresh human spleen[12]. The curcumin can suppress the PHA-induced proliferation of human peripheral blood mononuclear cells (PBMCs) and inhibit IL-2 expression and NF-AB[13]. In another report, curcumin inhibited the activation of human V B CT cells induced cancer by phosphoantigens[14].
Anti-inflammatory activity of turmeric oil has been reported on pepper's model[15]. The volatile oil of C. longa was effective in anti-inflammatory and anti-hyaluronidase action[16]. They suggested the antioxidative effect as evidenced by inhibition of diffusion capability of the hyaluronidase enzyme by the oil. Further the cytotoxic, anti-inflammatory and antioxidant activity of curcumin I, II and III from C. longa was also reported[17]. They observed cytotoxic activity against leukemia, colon cancer, CNS melanoma, renal and breast cancer. The present investigation was aimed to see whether the chemical principles of C. longa can be used for promoting immunotherapeutic causes as well as ameliorating hepatotoxic dysfunctions.
2. Materials and methods
2.1. Preparation of extracts
After drying at 37 °C for 24 h the plant material was ground into powder. Exposure to sunlight was avoided to prevent the loss of active components.
One liter of double distilled water was mixed with 200 g of powdered C. longa rhizome, filtered with nitrocellulose membrane and the extracted liquid was subjected to water bath evaporation to remove the water. For water bath evaporation, liquid extract material was then placed into a beaker and subjected to water bath evaporation at 70 °C temperature for 7-10 h daily for 2-3 days until a semisolid state of extracted liquid is obtained. The semisolid extract produced was kept in the deep freezer at -20 °C overnight and then subjected to freeze drying. Extract obtained by this method was be then weighed and stored at 22 °C in desiccators until further use.
2.2. Animals
20 mice weighing approximately (20±1.0) g were taken and these mice were divided into four groups of five mice each. The first group was kept as control. The second group consisted of CCl4 at a dose of 0.5 mL/kg bw (i.p.) from the 8th day to 15th day of the experiment. In the third group, the mice were fed with extract of turmeric at a concentration of 50 mg/kg bw (orally) by feeding needle for 15 days. In the fourth group, the mice were given both turmeric extract (for 15 days, orally) and CCl4 (for last 7 days, i.p.). Animal experiments were in accordance with the instructions for the care and use provided by the institution at which the research was carried out.
2.3. Collection of blood
Blood was collected from the retro-orbital plexus of the animals and serum isolated from the blood samples. The animals were sacrificed on the 16th day of treatment. Peritoneal macrophages were isolated from the sacrificed mice.
2.4. Determination of serum bilirubin level
The formation of pink-colored azo-bilirubin by the reaction between bilirubin and a diazo reagent was utilized. In practice, one estimation was done with addition of alcohol and the other without alcohol. The former yields total bilirubin and latter conjugated bilirubin[18].
2.5. Estimation of serum glutamate oxaloacetate transaminase (aspartate transaminase) and serum glutamate pyruvate transaminase (alanine transaminase) levels in serum
For each enzyme, 0.1 mL of non-hemolyzed serum was mixed respectively with 0.5 mL of glutamic-oxaloacetic transaminase (SGOT or AST) substrate and 0.5 mL glutmatic-pyruvate transaminase (SGPT or ALT) substrate and incubated for 1 h at 37 °C. Then 0.5 mL of 2, 4-dinitrophenyl hydrazine solution was added to the respective test tubes and allowed to stand for 15 min at room temperature. Then, 5 mL of 0.4 (N) NaOH was added, mixed and kept at room temperature for 20 min. The intensity of the developed color was read at 540 nm after setting the instrument to zero density with water. The decrease in density represents the decrease in α-ketoglutarate from which the activity was calculated[19].
2.6. Isolation of peritoneal macrophages
On the 13th day, all the mice were injected with 50 µL of 3% starch (i.p.). After two days they were sacrificed by cervical dislocation. Following this 5 mL of ice-cold RPMI-1640 were injected (i.p.) in all the dead mice and the injected area was lavaged softly. A small perforation was made to withdraw the RPMI-1640 containing peritoneal fluid. The process was repeated to accumulate the remaining fluid by aspirating and collecting in plastic centrifuge tubes. The samples were then centrifuged for 30 min at 3 500 rpm. All the samples were then washed in RPMI-1640 twice and the pellet were collected separately and incubated for 2 h at 37 °C. The supernatant was decanted and the adhered macrophages present in the micro centrifuge tubes were resuspended in 1 mL RPMI-1640. A portion of entire cell samples (100 µL) isolated from all the mice, were then aspirated and smeared on a glass slide and incubated for 1 h, fixed with 4.1% formaldehyde, kept for 30 min before staining with Giemsa and all these assays were performed separately for each group of mice. After that the slides were washed, air dried and observed under microscope. The other portions of cell samples were kept intact for further assays[20].
2.7. Morphological alteration assay
100 µL sample cells in HBSS-BSA from all mice were taken separately and fixed in an equal volume of 2.5% glutaraldehyde in HBSS. After 10 min, cells were centrifuged at 2 000 rpm for 5 min. The supernatant was removed and the pellet was resuspended in HBSS. Smears of cells were drawn on glass slides, air dried, fixed in methanol and stained with Giemsa. Cells were observed under oil immersion microscope. Any cell having intensive rough surface was scored as polarized and this was expressed as a percentage of the total number of cells counted[21].
2.8. In vitro cell adhesion assay
Cells were seeded separately for different groups in 96-well microtitre plates and allowed to adhere for different times. In time, wells were washed with HBSS, and then 100µL of 0.5 % crystal violet in 12% neutral formaldehyde, and 10% ethanol was added to each well and incubated for 4 h to fix and stain the cells. Wells were washed and air dried for 30 min. crystal violet was extracted from the macrophage adhered in the wells by lysing with 0.1% SDS in HBSS. Absorbance was measured spectrophotometrically at 570 nm. Cell adhesion was expressed as increased absorbance at 570 nm[22].
2.9. Phagocytosis assay
100 µL of cells from all mice were allowed to adhere separately on glass slides whereas non adherent cells were washed out with DPBS (1×). To the glass slides containing adhered macrophages 10% heat killed Staphylococcus aureus was added and incubated for 3 h at 37 °C which were then washed with DPBS (1×) and dried. The cells were at last fixed in 50% methanol, stained with Giemsa, observed under oil immersion microscope and counted for number of bacterial cells ingested[23].
2.10. Myeloperoxidase release assay
200 µL of cells from different groups were taken into micro centrifuge tubes and stimulated with LPS (100 ng/mL) for 1 h at 37 °C and centrifuged at 13 000 rpm for 10 min. The supernatant thus obtained from different sets was recovered separately and kept at -20 °C until further use. The cell free supernatant was used for assay of the partial MPO release for different groups. The pellet that recovered from all the four groups were lysed in 0.01% SDS and then centrifuged again. The supernatant was recovered as before for total MPO release assay. Subsequently 100 µL of cell free supernatant as well as from lysis of cells were reacted with 100µL substrate buffer and kept at 37 °C for 20 min, then the reaction was stopped by adding 100 µL of 2(N) H2SO4 and absorbance was measured at 492 nm[24].
2.11. Nitric oxide release assay
100 µL of macrophage cells were isolated from respective groups from 106 cells/mL dilution and then suspended in DPBS-BSA. The cells were than stimulated with LPS (100 ng/mL) for 1 h at 37 °C[25].
2.12. Intracellular killing assay
In this procedure, 100 µL of bacterial cells were incubated separately for all groups with macrophages in a total volume of 1 mL DPBS-BSA and kept in the shaker for 20 min at 37 °C. Non ingested bacteria were then removed by differential centrifugation for 10 min at 10 000 rpm at 4 °C. Following that, two washes were given with ice-cold DPBS-BSA. The cells containing ingested bacteria were resuspended in DPBS-BSA containing 10% normal serum and incubated at 37 °C for 25 min. At 0 min and after 15, 30 and 45 min time intervals 0.1 mL sample was removed each time and treated with gentamycin. The above content was then plated onto nutrient agar petriplate and the number of viable intracellular bacteria was determined by counting the individual colony formed[26].
2.13. Statistical analysis
A one-tailed Student's t test as well as ANOVA was performed to compare the mean values of control and turmeric extract group. The results were expressed as mean±standard error mean and all the experiment was done in triplicates.
3. Result
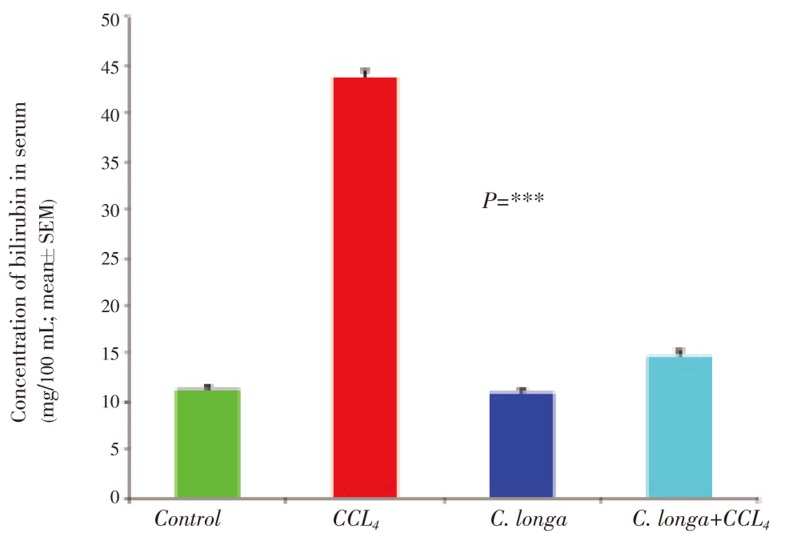
3.1. Effect of C. longa on serum bilirubin level in CCl4 intoxicated male albino mice
Figure 1 showed the effect of C. longa on bilirubin level in serum of CCl4 intoxicated male albino mice. The control had shown the bilirubin level in serum of (11.34±0.41) mg/100 mL but after CCl4 treatment, it increased to (43.65±0.81) mg/100 mL. Whereas after administration of C. longa at a dose of 60 mg/kg bw in CCl4 intoxicated mice, the bilirubin level reduced to (14.65±0.69) mg/100 mL. The reduced level of bilirubin was also observed (10.92±0.37) mg/100 mL in control group after C. longa administration (Figure 1, P =***).
Figure 1. Effect of C. longa on serum bilirubin level in CCl4 intoxicated male albino mice.
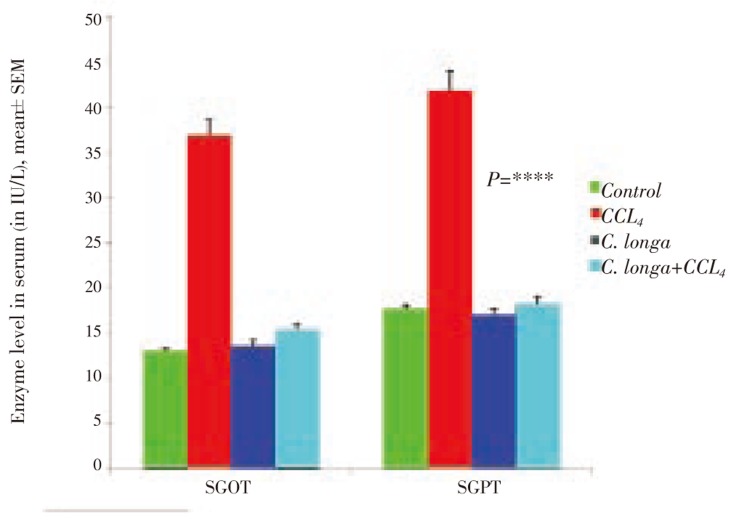
3.2. Effect of C. longa on serum SGOT (AST) level in CCl4 intoxicated male albino mice
Figure 2 showed the effect C. longa on SGOT (AST) level in serum of CCl4 intoxicated male albino mice. The control had shown the SGOT (AST) level in serum of (12.99±0.24) IU/L but after CCl4 treatment, it increased to (36.68±0.52) IU/L. Whereas after administration of C. longa at a dose of 60 mg/kg bw in CCl4 intoxicated mice, the SGOT (AST) level reduced to (15.22±0.36) IU/L. The reduced level of SGOT (AST) was also observed (13.54±0.36) IU/L in control group after C. longa administration (Figure 2; P =****).
Figure 2. Effect of C. longa on serum level of SGOT and SGPT enzyme in CCl4 intoxicated Swiss albino mice.
3.3. Effect of C. longa on serum SGPT (AST) level in CCl4 intoxicated male albino mice
Besides the measurements of serum SGOT level in CCl4 intoxicated male albino mice, it is also important to see the effects of C. longa on serum SGPT level (Figure 2). After CCl4 treatment in control mice, the serum SGPT level increased from (17.57±0.27) IU/L to (41.85±0.73) IU/L. However, administration of C. longa reduced the serum SGPT level to (18.14±0.46) IU/L. Administration of C. longa in control mice also showed some reduction of SGPT level i.e. up to (16.78±0.41) IU/L in serum (Figure 2; P =****).
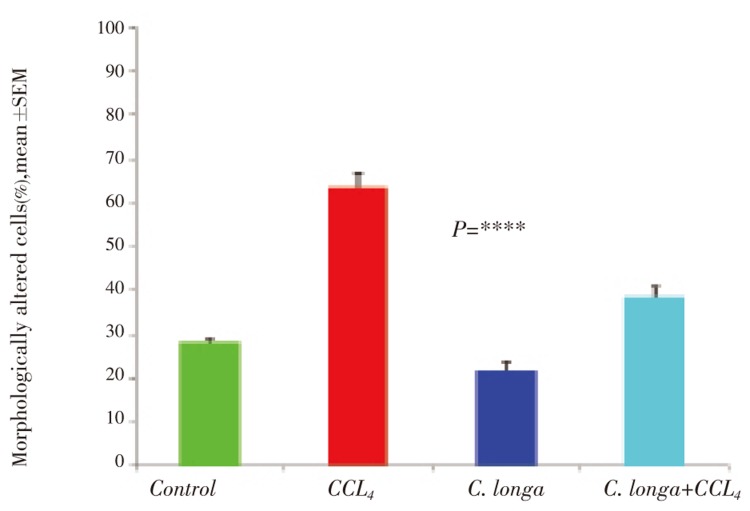
3.4. Effect of C. longa on morphology of peritoneal macrophages isolated from CCl4 intoxicated male albino mice
Morphology of macrophage plays a prominent part of their function. To demonstrate the effect of both CCl4 and C. longa on the number of differentiated macrophages, the macrophage cells deviated from spherical outline were measured and counted as morphologically altered macrophage. From this experiment, it was found that CCl4 treatment increased the number of undifferentiated macrophages from (28.04±0.75)% to (63.24±3.36)%. However the administration of C. longa in CCl4 intoxicated mice, the number of undifferentiated macrophages became almost normal level of (38.59±2.17)%. Administration of C. longa in control mice also showed some significant reduction of undifferentiated macrophages up to a level of (21.30±2.18)% (Figure 3; P=****).
Figure 3. Effect of C. longa on morphological alteration of peritoneal macrophages in CCl4 intoxicated Swiss albino mice.
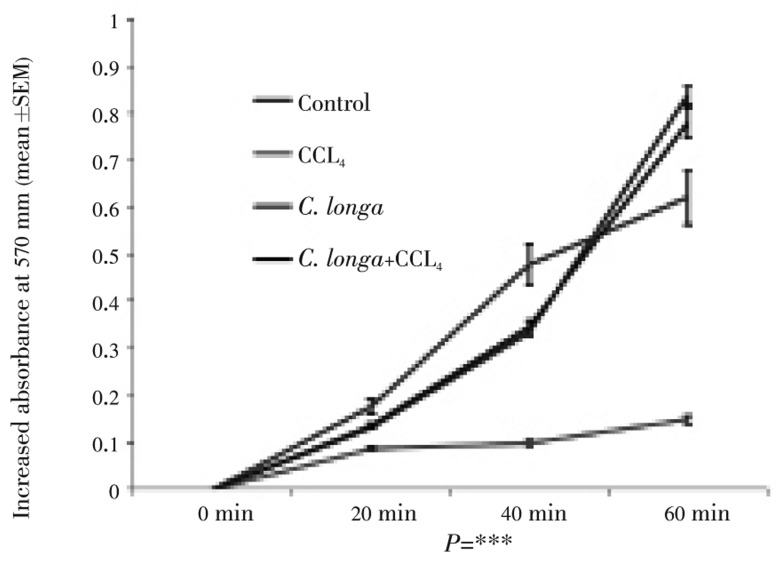
3.5. Effect of C. longa extract on the adhesion property of CCl4 intoxicated mice peritoneal macrophages
In vitro cell adherence assay may reflect the in vivo capacity for cellular adherence with treatment by C. longa extract hepatotoxic mice. In order to address this fundamental characteristic of macrophages, the cell adhesion property was assayed in vitro. Adhesion of cells increased gradually after C. longa administration (Figure 4; P=***).
Figure 4. Effect of C. longa extract on in vitro cell adhesion properties of peritoneal macrophages isolated from CCl4 intoxicated male albino mice.
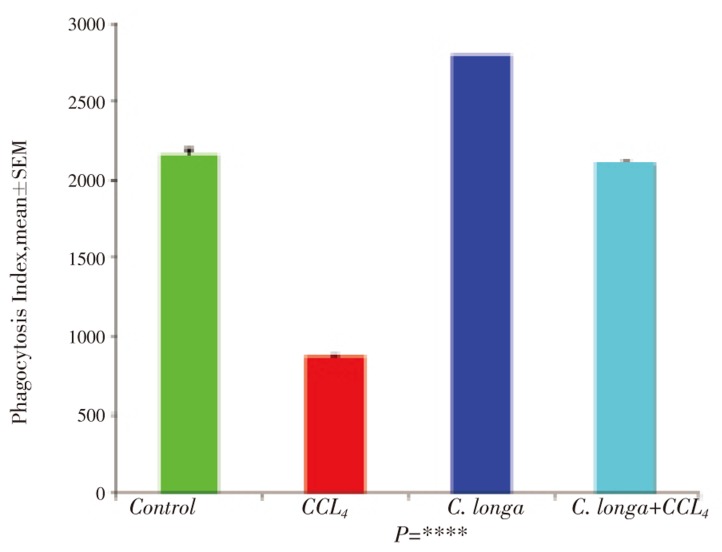
3.6. Effect of C. longa on phagocytosis capacity of peritoneal macrophages isolated from CCl4 intoxicated male albino mice
To evaluate the effect of C. longa on phagocytosis capacity of peritoneal macrophages, the phagocytosis index was measured. CCl4 administration in control mice reduced the phagocytosis index from (2 160.00±36.22) to (872.00±10.35).But after the administration of C. longa, the phagocytosis index of CCl4 intoxicated peritoneal macrophages increased to (2 104.00±10.81). Apart from increasing the phagocytosis index of CCl4 intoxicate peritoneal macrophages, C. longa treatment also increased the phagocytosis index of control peritoneal macrophages to the level of (2 783.4±9.4) (Figure 5; P=****).
Figure 5. Effect of C. longa on phagocytosis of peritoneal macrophages in CCl4 intoxicated Swiss albino mice.
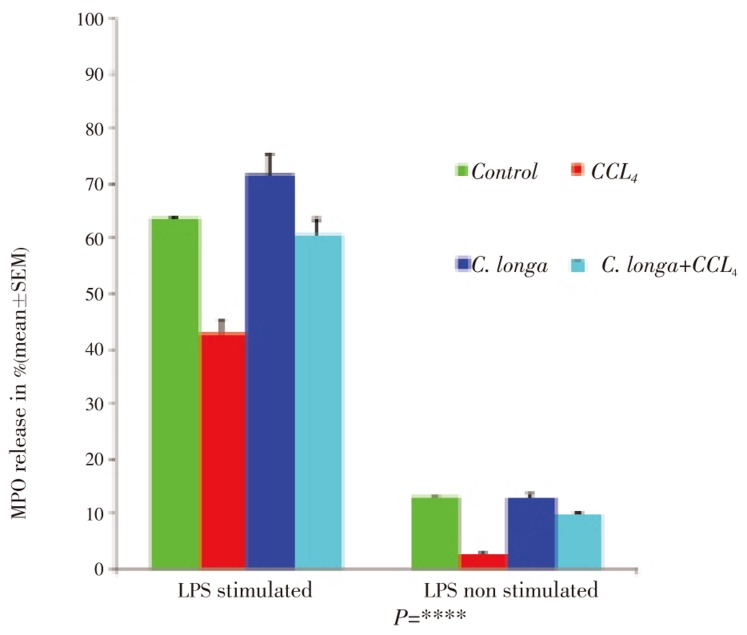
3.7. Effect of C. longa on myeloperoxidase (MPO) enzyme release from peritoneal macrophages isolated from CCl4 intoxicated male albino mice
MPO reduced the free radical level in our system. CCl4 caused an increase in the level of CCl3 production, but whether C. longa causes any alteration in the level of free radicals or not was the present objective of our study. CCl4 intoxication reduces the enzyme release from (63.56±0.33)to (42.82±1.25) as in the case of a control group. However, administration of C. longa extract in CCl4 intoxicated mice sufficed to protect the macrophage and induce (60.46±0.39)%. Administration of C. longa in control group also shows significant increase of MPO release from target cell up to (71.67±0.31)% with LPS stimulation. The same trend was also observed in LPS non-stimulation (Figure 6; P =****).
Figure 6. Effect of C. longa on myeloperoxidase enzyme release from peritoneal macrophages isolated from CCl4 intoxicated male albino mice.
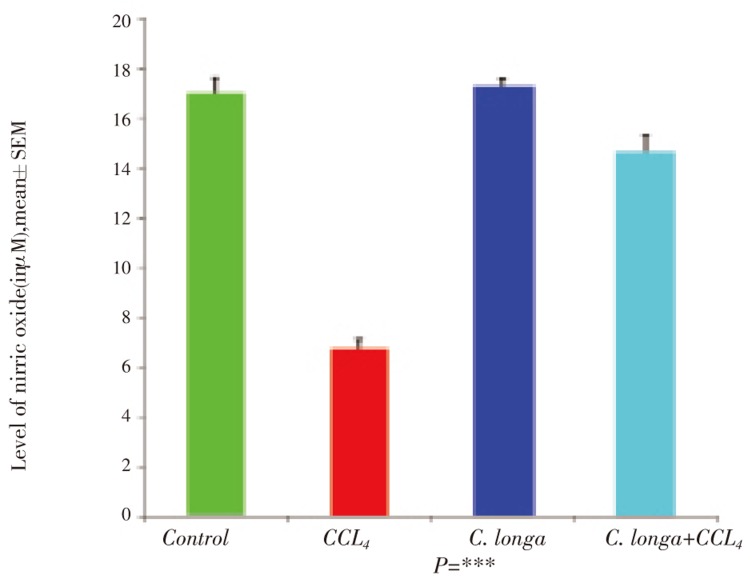
3.8. Effect of C. longa on nitric oxide (NO) release from peritoneal macrophages isolated from CCl4 intoxicated male albino mice
Nitric oxide plays an important part to kill the microbial pathogen inside the macrophage by forming sodium hypochloride (NaOCl). CCl4 intoxication significantly lowered the nitric oxide release to (6.7±0.4) µM from (17.15±0.66) µM as in the case of control group. However, C. longa administration ameliorated the effect of CCl4 in CCl4 intoxicated male albino mice (Figure 7; P =***).
Figure 7. Effect of C. longa on NO release of peritoneal macrophages in CCl4 intoxicated Swiss albino mice.
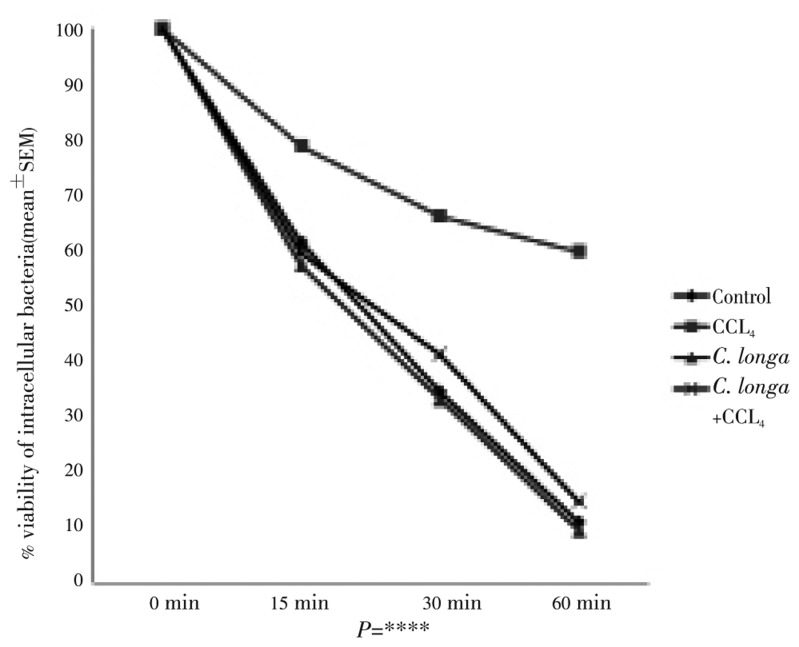
3.9. Effect of C. longa on intracellular killing capacity of peritoneal macrophages isolated from CCl4 intoxicated male albino mice
Whether C. longa administration in CCl4 intoxicated mice has any effect in the killing capacity of peritoneal macrophages was the last and foremost important objective our study. Our results suggested that CCl4 intoxication in control mice reduced the intra cellular killing capacity by five folds but after administration of C. longa aqueous extract in CCl4 intoxicated mice restores the killing capacity of peritoneal macrophages (Figure 8; P =****).
Figure 8. Effect of C. longa extract on the killing capacity of peritoneal macrophages isolated from CCl4 intoxicated male albino mice.
4. Discussion
This study was undertaken to determine the effect of C. longa on liver function as well as the immune functional activities of peritoneal macrophages in CCl4 intoxicated Swiss albino mice. Our results provide evidence for the adverse effect of CCl4 on the liver functions when enzymes such as SGOT and SGPT were found elevated in the serum. Since the estimation of serum enzymes such as SGOT and SGPT was a good indicator for the pathological manifestation of jaundice, there was no doubt that CCl4 induces liver damages in these experimental animals. However, in vivo administration of C. longa aqueous extract causes hepatoprotective activities in CCl4 toxicity. The enzyme level goes back to the normal level, as in the case of control group. In our study, administration of C. longa was found to provide significant protection against a CCl4-induced increase in level of SGOT, SGPT and serum bilirubin. CCl4-induce elevated levels may indicate liver damage, since the major site transamination reaction is in the liver. In transaminases, pyridoxal phosphate (PLP) the prosthetic group of the enzyme, forms a Schiff base intermediate which remains tightly bound to the enzyme by multiple non-covalent interactions. Turmeric treatment during CCl4 intoxication may enhance the above mentioned molecular mechanism of enzyme action.
When old red blood cells are destroyed the in the tissue macrophage system, the globin portion of the hemoglobin molecule is split off, and the heme is converted to biliverdin. In humans, most of the biliverdin is converted to bilirubin and excreted in the bile. The iron from the heme is reused for hemoglobin synthesis. The bilirubin is bound to albumin in the circulation. Some of its tightly bound, but most of it can dissociate in the liver, and free bilirubin enters liver cells, where it is bound to cytoplasmic proteins. It is next conjugated to glucuronic acid in a reaction catalyzed by the enzyme glucuronyl transferase. Each bilirubin molecule reacts with two uridine diphosphaglucuronic acid (UDPGA) molecules to form bilirubin diglucuronide. This glucuronide, which is more water soluble than the free bilirubin, is then transported against a concentration gradient by a presumably active process into the bile canaliculi. A small amount of the bilirubin glucuronide escapes into the blood, where it is bound less tightly to albumin than is free bilirubin, and is excreted in the urine. Thus, the total plasma bilirubin normally includes free bilirubin plus a small amount of conjugated bilirubin. Most of the bilirubin glucuronide passes via the bile ducts to the intestine. When any hepatotoxicity appears, the total bilirubin (either free or conjugated bilirubin) rises in the blood and this may be due to five reasons i.e. 1) excess production of bilirubin; 2) decreased uptake of bilirubin into hepatic cells; 3) disturbed intracellular protein binding or conjugation; 4) disturbed secretion of conjugated bilirubin into the bile canaliculi; or 5) intrahepatic or extrahepatic bile duct obstruction. Our results showed after CCl4 intoxication in male albino mice, the total bilirubin rises in serum and it suggested that liver damages occur. However, administration of C. longa in CCl4 intoxicated mice restores the level of bilirubin in serum and this may be due to the obstruction of any above mentioned mechanism. Another consequence of this protective effect of C. longa may be due to the obstruction of all the bilirubin increasing mechanism by different compounds of the extract simultaneously.
Exposure of organisms to bacterial infection results in the activation of a variety of host defense mechanisms which include phagocytosis, degradative enzyme release and respiratory burst response. The first step in macrophage function is the activation or differentiation of macrophages. However intensive rough surface or almost spherical macrophages can be considered as abnormal macrophages because after getting encountered with the antigen, the macrophages must have perfect surface morphology. In our study, it was found that CCl4 intoxication increases this abnormal type of macrophages by two folds but after administration of C. longa aqueous extract in that CCl4 intoxicated mice renders the macrophages to become acquiring abnormal surface morphology so that they can be function normally. The mechanism involving this protection by C. longa extract probably somehow related to the production of monocyte colony stimulating factor or granulocyte-monocyte stimulating factor (M-CSF/GM-CSF).
In order for circulating macrophages to enter inflamed tissue or peripheral lymphoid organs, the cells must adhere to and pass between the endothelial cells lining the walls of blood vessels, a process called extravasation. Endothelial cells express leukocyte-specific cell adhesion molecules (CAMs). Some of these membrane proteins are expressed constitutively; others are expressed only in response to local concentrations of cytokines produced during an inflammatory response. Recirculating macrophage bears receptors that bind to CAMs on the vascular endothelium, enabling these cells to extravasate into the tissues. The increase in cell adherence in CCl4 intoxicated group after C. longa extract treatment might be primarily caused by an increase expression of cell adhesion molecules on the surface of macrophage cells.
As is evident from the phagocytic index after CCl4 intoxication, it can be suggested that CCl4 groups are more prone to infection, as they cannot phagocytose efficiently and, as a result, cannot clear out the invading microorganism, which may lead to a diseased state upon bacterial invasion. However, administration of C. longa increases the phagocytosis capacity of peritoneal macrophages isolated from CCl4 intoxicated mice and this may due to increased number of cells present in the peritoneum as well as alteration of the ability of those that remain functioning normally.
Macrophage secretes lysosomal proteolytic enzymes active at tissue pH that may be important in their ability to kill tumor and bacterial cells. As macrophage mature, there is a progressive rise in lysosomes and hydrolytic content. Continuous CCl4 treatment may also lead to immaturation of macrophages in vivo, and it can be assumed that due to this exposure they have lesser lysosomal conent and hence are less capable of secreting myeloperoxidase (MPO) and nitric oxide (NO). Due to this lesser lysosomal enzyme, these CCl4 intoxicated peritoneal macrophages could not able to kill the intracellular Staphylococcus aureus and this was evident from our finding increased viability of Staphylococcus aureus in CCl4 treated group. However, treatment by C. longa extract during CCl4 intoxication may somehow alter the maturation of macrophages, so that they regain their lysosomal hydrolytic content and release more MPO and NO following activation and following this CCl4 intoxicated peritoneal macrophages could be able to regain their intracellular killing capacity.
From our results it can be suggested that turmeric would be effective in ameliorating jaundice with good efficacy and toleration. Additionally, its immunostimulatory effect prevents pathogenic insults in jaundice induced immunocompromised state.
Footnotes
Foundation Project: Supported by a grant form Assam University.
Conflict of interest statement: We declare that we have no conflict of interest.
References
- 1.Bishayi B, Roychowdhury S, Ghosh S, Sengupta M. Hepatoprotective and immunomodulatory properties of Tinospora cordifolia in CCl4 intoxicated mature albino rats. J Toxicol Sci. 2002;27:139–146. doi: 10.2131/jts.27.139. [DOI] [PubMed] [Google Scholar]
- 2.Apisariyakul A, Vanittanakom N, Buddhasukh D. Antifunga activity of turmeric oil extracted from Curcuma longa (Zingiberaceae) J Ethnopharmacol. 1995;49:163–169. doi: 10.1016/0378-8741(95)01320-2. [DOI] [PubMed] [Google Scholar]
- 3.Singh R, Chandra R, Bose M, Luthra M. Antimicrobial activity of C. longa rhizome extract on pathogenic bacteria. Curr Sci. 2002;83(6):737. [Google Scholar]
- 4.Suhit G, Meghana K, Ramesh B, Anant P. Activity of water-soluble turmeric extract using hydrophilic excipients. Food Sci Technol. 2010;43(1):59–66. [Google Scholar]
- 5.Li X, Liu X. Effect of curcumin on immune function of mice. J Huazhong Univ Sci Technol Med Sci. 2005;25(2):137–140. doi: 10.1007/BF02873559. [DOI] [PubMed] [Google Scholar]
- 6.Giri RK, Rajagopal V, Kalra VK. Curcumin, the active constituent of turmeric, inhibits amyloid peptide-induced cytochemokine gene expression and CCR5-mediated chemotaxis of THP-1 monocytes by modulating early growth response-1 transcription factor. J Neurochem. 2004;91(5):1199–1210. doi: 10.1111/j.1471-4159.2004.02800.x. [DOI] [PubMed] [Google Scholar]
- 7.Yang F, Lim GP, Begum AN, Ubeda OJ, Simmons MR, Ambegaokar SS, et al. Curcumin inhibits formation of amyloid beta oligomers and fibrils, binds plaques, and reduces amyloid in vivo. J Biol Chem. 2005;280(7):5892–5901. doi: 10.1074/jbc.M404751200. [DOI] [PubMed] [Google Scholar]
- 8.Zhang L, Fiala M, Cashman J, Sayre J, Espinosa A, Mahanian M, et al. Curcuminoids enhance amyloid-β uptake by macrophages of Alzheimer's disease patients. J Alzheimers Dis. 2006;10:1–7. doi: 10.3233/jad-2006-10101. [DOI] [PubMed] [Google Scholar]
- 9.Gamal Allam. Immunomodulatory effects of curcumin treatment on murine schistosomiasis mansoni. Immunobiology. 2009;214(8):712–727. doi: 10.1016/j.imbio.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 10.Shao ZM, Shen ZZ, Liu CH, Sartippour MR, Go VL, Heber D, et al. Curcumin exerts multiple suppressive effects on human breast carcinoma cells. Int J Cancer. 2002;98:234–240. doi: 10.1002/ijc.10183. [DOI] [PubMed] [Google Scholar]
- 11.Singh S, Aggarwal BB. Activation of transcription factor NF-kB is suppressed by curcumin (diferuloylmethane) J Biol Chem. 1995;270:24995–25000. doi: 10.1074/jbc.270.42.24995. [DOI] [PubMed] [Google Scholar]
- 12.Ranjan D, Chen C, Johnston TD, Jeon H, Nagabhushan M. Curcumin inhibits mitogen stimulated lymphocyte proliferation, NF-_B activation, and IL-2 signaling. J Surg Res. 2004;121(2):171–177. doi: 10.1016/j.jss.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 13.Joe B, Lokesh BR. Dietary n-3 fatty acids, curcumin and capsaicin lower the release of lysosomal enzymes and eicosanoids in rat peritoneal macrophages. Mol Cell Biochem. 2000;203(1–2):153–161. doi: 10.1023/a:1007005605869. [DOI] [PubMed] [Google Scholar]
- 14.Yadav VS, Mishra KP, Singh DP, Singh ML. Immunomodulatory effects of curcumin. Immunopharmacol Immunotoxicol. 2005;27:485–497. doi: 10.1080/08923970500242244. [DOI] [PubMed] [Google Scholar]
- 15.Cipriani B, Borsellino G, Knowles H, Tramont D, Cavaliere F, Bernardi G, et al. CF Curcumin inhibits activation of V_9V_2 T cells by phosphoantigens and induces apoptosis involving apoptosis-inducing factor and large scale DNA fragmentation. J Immunol. 2001;167(6):3454–3462. doi: 10.4049/jimmunol.167.6.3454. [DOI] [PubMed] [Google Scholar]
- 16.Ramchandran SV, Bhide SD, Lambe CS, Vaidya BD. Antiinflammatory activity of turmeric oil in arthritis model in rat. Chennai: Proceeding of International Congress on Ayurveda; 2000. pp. 199–200. [Google Scholar]
- 17.Mishra N, Gupta SS. Anti-inflammatory and anti-hyaluronidase activity of volatile oil of Curcuma longa. J Res Ayur Siddha. 1997;1-2(18):56–62. [Google Scholar]
- 18.Bergmeyer J, Marianne G. Total bilirubin. In: Bergmeyer H, editor. Methods of enzymatic analysis. New York: Academic Press Inc; 1985. pp. 591–598. [Google Scholar]
- 19.Reitman S, Frankel S. A colorometric method for the determination of serum glutamate oxaloacetate and serum glutamate pyruvate transaminase. Am J Clin Pathol. 1957;28(1):28–56. doi: 10.1093/ajcp/28.1.56. [DOI] [PubMed] [Google Scholar]
- 20.Matsumoto H, Naraba M, Murakami I, Kudo K, Yamaki A, Ueno A. Concordant induction of prostaglandin E2 synthase with cycloxygenase-2 leads to preferred production of prostaglandin E2 over thrombaxane and prostaglandin D2 in LPS stimulated rat peritoneal macrophages. Biochem Biophys Res Commun. 1997;230:110–116. doi: 10.1006/bbrc.1996.5894. [DOI] [PubMed] [Google Scholar]
- 21.Qu J, Condliffe MA, Lawson M, Pelvin RJ, Chlivers E. Lack of effect of recombinant platelet derived growth factor on human neuttrophil function. J Immunol. 1997;159:2952–2959. [PubMed] [Google Scholar]
- 22.Lin TH, Roselles C, Mondol KL, Bolen JB, Haskell, Juliano RL. Integrin mediated tyrosine phosphorylation and message induction in monocytic cells. J Biol Chem. 1995;270:16189–16202. doi: 10.1074/jbc.270.27.16189. [DOI] [PubMed] [Google Scholar]
- 23.Czuprynski CJ, Henson PM, Campbell PA. Killing of Listeria monocytogenes by inflammatory neutrophils and mononuclear phagocytes from immune and non immune mice. J Leuk Biol. 1984;35:193–208. doi: 10.1002/jlb.35.2.193. [DOI] [PubMed] [Google Scholar]
- 24.Bos AR, Weaver R, Roos D. Characterization and qualification of the peroxidase in human neutrophils. Biochem Biophys Acta. 1990;525:4133–4141. [Google Scholar]
- 25.Sasaki M, Gonzales ZM, Huang H, Herring WJ, Ahn S, Ginty DD, et al. Dynamic regulation of neuronal nitric oxide synthase transcription by calcium influx through a CREB family transcription factor-dependant mechanism. Proc Nalt Acad Sci. 2000;18:8617–8622. doi: 10.1073/pnas.97.15.8617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leigh PCJ, Van FR, Zwet TL. In vitro determination of phagocytosis and intracellular killing by polymorphonuclear neutrophils and mononuclear phagocytes. In: Weir DM, editor. Handbook of experimental immunology. 4th ed. Oxford: Blackwell Scientific Publications; 1986. pp. 1–19. [Google Scholar]