Abstract
Objective
To determine the prevalence of intestinal parasitic infections among mentally retarded residents of rehabilitation center of Bandar Abbas, Hormozgan province, southern Iran.
Methods
A cross-sectional study was carried out in central rehabilitation institute of Hormozgan province in summer 2010. Fecal samples of all 133 residents (72 males, 61 females) aged 3–52, were collected in triplicate. Specimens were examined by direct smear, formalin-ether concentration techniques and stained by permanent Trichrome, Ziehl-Neelsen stains. Statistical analysis was conducted by SPSS 13.5.
Results
Intestinal parasitic infections were seen in 48.5% (64 out of 133 subjects: 53.4% in males and 46.6% in females). Strongyloides stercoralis with 17.3% showed the highest incidence followed by Entamoeba coli (9.8%), Blastocystis hominis (7.5%), Giardia lamblia (2.3%), Endolimax nana (2.3%), Hymenolepis nana (0.8%), Oxyuris vermicularis (0.8%), and Chilomasix mesnili (0.8%). Double infections were found to be as: Strongyloides stercoralis + Giardia lamblia (2.3%), Entamoeba coli + Giardia lamblia (1.5%), Entamoeba coli + Blastocystis hominis (1.5%), Oxyuris vermicularis + Entamoeba coli (0.8%), Strongyloides stercoralis + Entamoeba coli (0.8%), respectively.
Conclusions
Our findings reveal that strongyloidiasis is a common disease among mentally retarded population in southern Iran.
Keywords: Intestinal pararsites, Mentally retarded, Hormozgan, Iran, Strongyloides stercoralis, Strongyloidiasis, Parasitic infection, Rehabilitation centre
1. Introduction
Intestinal parasites infections are major public health problems worldwide, especially in developing countries[1]–[3].The rate of infections varies according to socio-economical situations and hygienic behaviors[2],[4]–[7]. Contamination of water and food sources with human wastes and insufficient hygiene are main causes of fecal-oral transmitted intestinal parasitic infections[8]–[10].
Soil-transmitted helminthes (STH) as a major health problem caused by Ascaris lumbricoides, Trichuris trichiura and the hookworms are the most prevalent worldwide[7] and, Strongyloides stercoralis (S. stercoralis) is the most neglected one among them[9],[11],[12]. It is estimated that over 1 billion people are infected with STH and 30–100 millions with S. stercoralis worldwide[7],[11]–[14]. S. stercoralis's unique life cycle makes it possible to survive in human host and causes autoinfection to lead chronic disease which could have remained for several years[13]–[15]. Although most of infections are asymptomatic, disseminated and hyper infection may occur in immunocompromised and immune deficient individuals as a fatal disease[16]–[20].
Strongyloidiasis is endemic in several countries including Iran with the prevalence of 0.3% in general population[14],[21]. Suitable hygiene plays a key role in prevention of intestinal parasitic infections[22].
Mental retardation and consequently poor hygiene increase the risk of infection with intestinal parasitic infections[8],[23]. Few epidemiological studies carried out in mentally retarded populations in Iran[24],[25] and other parts of the world have indicated the prevalence of intestinal parasitic infections among them[26]–[29]. The present article evaluates the prevalence of intestinal parasites among mentally retarded residents in rehabilitation center of Hormozgan province, southern Iran.
2. Materials and methods
A cross-sectional study was conducted in central institution for mentally retarded population which located in Bandar Abbas city of Hormozgan province. The province was located in the South of Iran in tropical region, attached to Persian Gulf with high humidity (20%-100%) and warm climate. The institute is the biggest one in province and affiliated to welfare organization. All mentally retards, including children and adults from almost every part of the province were institutionalized there. All studied populations were residents of the institution and participated to this study from May to June 2010, aged 3–52 years (22.84±9.39). Three stool samples were taken from each participant every other day and taken to Parasitology Laboratory of Bandar Abbas Paramedical School. Specimens were examined with light microscope using normal saline, iodine stain and formaline-ether concentration techniques. Modified Ziel-Neelsen and Trichrome stains were also used for more confirmation as well. Statistical analysis was carried out by ANOVA and Chi-square test using SPSS software version 13.5, and P value of <0.05 was considered significant.
3. Results
All of the 133 institutionalized residents in the institute aged 3–52 participated in the study. Stool examination showed that 64 (48.5%) of participants were infected with one or two parasites, among whom 55 cases (41.6%) showed single infection, 9 (6.9%) double infections, and 69 (51.5%) showed no intestinal parasitic infections.
S. stercoralis with 23 cases (17.3%) alone and 4 (3.1%) with double infection (Figure 1) showed the highest prevalence among others. Entamoeba coli (E. coli) with 13 cases (9.8%) alone and 6 (4.6%) with double infection, and Blastocystis hominis (B. hominis) with 10 cases (7.5%) alone and 2 (1.5%) with double infection consequently were the most common parasitic infections in our studied population (Table 1). After that, single infections of Giardia lamblia (G. lamblia) (2.3%), Endolimax nana (E. nana) (2.3%), Hymenolepis nana (H. nana) (0.8%), Oxyuris vermicularis (O. vermicularis) (0.8%), Chilomasix mesnili (C. mesnili) (0.8%) were observed.
Figure 1. S. stercoralis larva in stool smear.
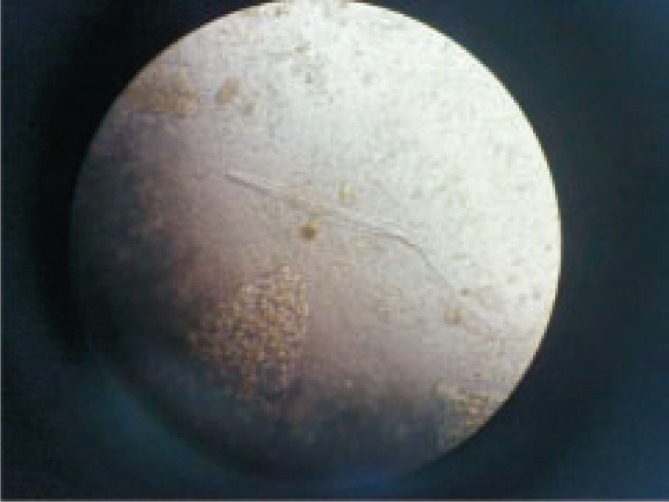
Table 1. Prevalence of intestinal parasitic infection among 133 residents of central institute of southern Iran [n (%)].
| Intestinal parasites | Prevalence | |
| Single | S. stercoralis | 23 (17.3) |
| E. coli | 13 (9.8) | |
| B. hominis | 10 (7.5) | |
| G. lamblia | 3 (2.3) | |
| E. nana | 3 (2.3) | |
| H. nana | 1 (0.8) | |
| O. vermicularis | 1 (0.8) | |
| C. mesnili | 1 (0.8) | |
| Double | S. stercoralis + G. lamblia | 3 (2.3) |
| E. coli + G. lamblia | 2 (1.5) | |
| E. coli + B. hominis | 2 (1.5) | |
| E. coli + O. vermicularis | 1 (0.8) | |
| E. coli + S. stercoralis | 1 (0.8) | |
The infection rates in males and females were 38 (53.5%) and 26 (41.9%), respectively. Age distribution of intestinal parasitic infection in studied population was shown in Table 2. No significant difference was found between age groups and intestinal parasitic infection (P=0.290) and neither between genders (P=0.182).
Table 2. Age distribution of intestinal parasitic infection in studied population (n=133) [n (%)].
| Age group (years) | Number examined | Number infected | P |
| <10 | 13 (9.8) | 4 (30.6) | 0.290 |
| 10–20 | 47 (35.3) | 25 (53.2) | – |
| 21–30 | 48 (36.1) | 20 (41.7) | – |
| 31–40 | 20 (15.1) | 12 (60.0) | – |
| >40 | 5 (3.7) | 3 (60.0) | – |
χ2=15.3, df=13.
4. Discussion
The results of the present study showed that prevalence of parasitic infections is high among institutionalized mentally retarded residents in rehabilitation center of Bandar Abbas.
Our study showed that 48.5% of residents in mentioned center were infected with one or more parasites. Although eight different parasite species were diagnosed either alone or in double form of infection, it was determined that the highest prevalence belonged to S. stercoralis (17.3%), E. coli (9.8%) and B. hominis (7.5%), respectively.
Also nonpathogenic parasites such as C. mesnili and E. nana were seen in this group, so these infections relate to the environment contaminated with feces[8].
High frequency of S. stercoralis in our studied group suggests that it must be considered as a health threatening agent in this institute, despite strongyloidiasis is not common in general population of Bandar Abbas[30],[31].
According to the high prevalence of strongyloidiasis in the rehabilitation care center, the true prevalence would be higher if specific diagnostic methods such as Baermann technique and agar plate culture method were used[11],[32],[33].
Serological methods can reveal light infections in asymptomatic individuals and should be used for further studies among those population[11],[15],[32] and in order to achieve real prevalence, screening procedures must be applied.
Previous studies in Iran have indicated that intestinal protozoan infections are common problems in such institutions[1],[24].
The prevalence of intestinal helminthic infections in general population varies between 0% to 3.6% in different parts of Iran[1] and the decrease in prevalence of helminthic infections is determined by epidemiological researches[6],[21],[34].
Protozoan infections are still more frequent in most parts and the rate of infections varies from 1% to 23%[24]. G. lamblia was frequently found in most parts of Iran and S. stercoralis as a soil-transmitted helminth was considered endemic in some parts with the frequency of about 0.3%[21].
A recent study among geriatric and disabled people in Kashan revealed that 87.6% of population were infected with pathogenic and nonpathogenic intestinal protozoan and the frequency of intestinal parasitic infection in mentally retarded students in Tehran was 56.8% showing no evidence of infection with S. stercoralis[24].
Other study carried out in Isfahan among mentally retarded students showed the frequency of infection with O. vermicularis (20.7%) and H. nana (1.3%), respectively[24], but they didn't find S. sterocralis among them.
Apart from O. vermicularis and H. nana infections in our studied population, other pathogenic and nonpathogenic parasites frequently alone or double were also observed among them.
The results from the study in an institution for mentally retarded adults showed only two cases of strongyloidiasis[28] while our study revealed 23 cases.
Results from other study among mentally disabled population in Japan showed frequency of intestinal amoebiasis[27], but we didn't find any case of Entamoeba histolytica in our population.
Study among mentally retarded people in the Philippines showed high frequency of Entamoeba histolytica in the population[26]. The same results were found among mentally retarded residents of Italian institution, but no infection with S. stercoralis was observed[35].
Among all parasitic infections in this center, S. stercoralis is the more frequent and the most important to care about. Our country is endemic for S. stercoralis, especially the north of Iran with temperate[17] and the south with warm and humid climate. Our studied people included severely mentally retarded individuals with unusual behaviors such as geophagia and coprophagia and strongyloidiasis was found to be high among them as we expected.
Unexpectedly, our findings contrasted with the results from northern Iran, as they didn't find S. stercoralis infection in mentally retarded inhabitants in spite of high humidity like southern Iran[1].
The origin of parasitic infections in densely populated places deemed to be person to person transmission[8],[9].
Crowdedness, mental retardation, pica, geophagia, coprophagia, contact with human waste and poor hygiene are important risk factors making residents of mental retards institutes more susceptible to infection with S. stercoralis[23]. Moreover, asymptomatic infection can remain for decades due to the occurrence of several auto infection cycles[15],[17].
Improvement of hygienic condition and prevention of person to person transmission along with better nutrition can limit the transmission of disease among this mentally retarded population. Although all infected individuals were treated with proper prescribed medicine, permanent care and screening are needed to eradicate infection in this institute.
Acknowledgments
We thank all staff of mentally retarded rehabilitation affiliated to social welfare organization of Hormozgan province, Bandar Abbas city for their collaboration in this study. We thank Abroshan H for his assistance in collecting samples. This work was financially supported by Research Deputy of Hormozgan University of Medical Sciences, Iran with grant number 90/108/1977.
Footnotes
Foundation Project: This work was financially supported by Research Deputy of Hormozgan University of Medical Science (grant No. 90/108/1977).
Conflict of interest statement: We declare that we have no conflict of interest.
References
- 1.Sharif M, Daryani A, Asgarian F, Nasrolahei M. Intestinal parasitic infections among intellectual disability children in rehabilitation centers of northern Iran. Res Dev Disabil. 2010;31(4):924–928. doi: 10.1016/j.ridd.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Belinelo JV, Milaneze BA, da Rosa AB, Bussular JPB, Moraes AN, Filho SAV, et al. Intestinal parasites in students 10 to 15 years of school of São Mateus's periphery, ES, Brazil. Eur J Sci Res. 2011;53(2):171–178. [Google Scholar]
- 3.Taheri F, Namakin K, Zarban A, Sharifzadeh G. Intestinal parasitic infection among school children in South Khorasan Province, Iran. J Res Health Sci. 2011;11(1):45–50. [PubMed] [Google Scholar]
- 4.Norhayati M, Fatmah MS, Yusof S, Edariah AB. Intestinal parasitic infections in man: a review. Med J Malays. 2003;58(2):296–305. [PubMed] [Google Scholar]
- 5.Al-Mohammed HI, Amin TT, Aboulmagd E, Hablus HR, Zaza BO. Prevalence of intestinal parasitic infections and its relationship with sociodemographics and hygienic habits among male primary schoolchildren in Al-Ahsa, Saudi Arabia. Asian Pac J Trop Med. 2010;3(11):906–912. [Google Scholar]
- 6.Akhlaghi L, Shamseddin J, Meamar AR, Razmjou E, Oormazdi H. Frequency of intestinal parasites in Tehran. Iran J Parasitol. 2009;4(2):44–47. [Google Scholar]
- 7.Alemu A, Atnafu A, Addis Z, Shiferaw Y, Teklu T, Mathewos B, et al. Soil transmitted helminths and Schistosoma mansoni infections among school children in zarima town, northwest Ethiopia. BMC Infect Dis. 2011;11:189. doi: 10.1186/1471-2334-11-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giacometti A, Cirioni O, Balducci M, Drenaggi D, Quarta M, De Federicis M, et al. Epidemiologic featurse of intestinal parasitic infections in Italian mental institutions. Eur J Epidemiol. 1997;13:825–830. doi: 10.1023/a:1007306630301. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed AM, Afifi AA, Malik EM, Adam I. Intestinal protozoa and intestinal helminthic infections among schoolchildren in Central Sudan. Asian Pac J Trop Med. 2010;3(4):292–293. [Google Scholar]
- 10.Alyousefi NA, Mahdy MAK, Mahmud R, Lim YAL. Factors associated with high prevalence of intestinal protozoan infections among patients in Sana'a City, Yemen. PLoS One. 2011;6(7):e22044. doi: 10.1371/journal.pone.0022044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steinmann P, Zhou XN, Du ZW, Jiang JY, Wang LB, Wang XZ, et al. Occurrence of Strongyloides stercoralis in Yunnan Province, China, and comparison of diagnostic methods. PLoS Negl Trop Dis. 2007;1(1):e75. doi: 10.1371/journal.pntd.0000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knopp S, Mohammed KA, Khamis IS, Mgeni AF, Stothard JR, Rollinson D, et al. Spatial distribution of soil-transmitted helminths, including Strongyloides stercoralis, among children in Zanzibar. Geospat Health. 2008;3(1):47–56. doi: 10.4081/gh.2008.231. [DOI] [PubMed] [Google Scholar]
- 13.Keiser PB, Nutman TB. Strongyloides stercoralis in the immunocompromised population. Clin Microbial Rev. 2004;17(1):208–217. doi: 10.1128/CMR.17.1.208-217.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tabei SZ, Asadian F, Fakhar M, Safaei A. Gastrointestinal hyper infection due to Strongyloides stercoralis in a patient with Behcet's syndrome. Comp Clin Pathol. 2009;18:89–91. [Google Scholar]
- 15.Krolewiecki AJ, Ramanathan R, Fink V, McAuliffe I, Cajal SP, Won K, et al. Improved diagnosis of Strongyloides stercoralis using recombinant antigen-based serologies in a community-wide study in northern Argentina. Clin Vaccine Immunol. 2010;17(10):1624–1630. doi: 10.1128/CVI.00259-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marcos LA, Terashima A, Dupont HL, Gotuzzo E. Strongyloides hyperinfection syndrome: an emerging global infectious disease. Trans R Soc Trop Med Hyg. 2008;102(4):314–318. doi: 10.1016/j.trstmh.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 17.Meamar AR, Rezaian M, Mohraz M, Hadighi R, Kia EB. Strongyloides stercoralis hyperinfection syndrome in HIV+/AIDS patients in Iran. Parasitol Res. 2007;101(3):663–665. doi: 10.1007/s00436-007-0531-x. [DOI] [PubMed] [Google Scholar]
- 18.Kia EB, Rahimi HR, Mirhendi H, Nilforoushan MR, Talebi A, Zahabiun F, et al. A case of fatal strongyloidiasis in a patient with chronic lymphocytic leukemia and molecular characterization of the isolate. Korean J Parasitol. 2008;46(4):261–263. doi: 10.3347/kjp.2008.46.4.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pays JF. Combined infection with HTLV-1 and Strongyloides stercoralis. Bull Soc Pathol Exot. 2011 doi: 10.1007/s13149-011-0175-z. [DOI] [PubMed] [Google Scholar]
- 20.Azira NM, Zeehaida M. Strongyloides stercoralis hyperinfection in a diabetic patient: case report. Trop Biomed. 2010;27(1):115–119. [PubMed] [Google Scholar]
- 21.Rokni MB. The present status of human helminthic diseases in Iran. Ann Trop Med Parasitol. 2008;102(4):283–295. doi: 10.1179/136485908X300805. [DOI] [PubMed] [Google Scholar]
- 22.Ammoura AM. Impact of hygienic level on parasite infection. Asian Pac J Trop Med. 2010;3(2):148–149. [Google Scholar]
- 23.Sirivichayakul C, Pojjaroen-anant C, Wisetsing P, Siripanth C, Chanthavanich P, Pengsaa K. Prevalence of intestinal parasitic infection among Thai people with mental handicaps. Southeast Asian J Trop Med Public Health. 2003;34(2):259–263. [PubMed] [Google Scholar]
- 24.Sima R, Mohsen A, Hossein H. Prevalence of intestinal parasitic infections among the geriatric and disabled in Golabchi Center of Kashan during 2006-2007. J Kashan Univ Med Sci. 2009;12(4):78–82. [Google Scholar]
- 25.Mahyar A, Daneshi MM, Saghafi H, Rezai M. Intestinal parasites in mentally retarded children of Qazvin. J Qazvin Univ Med Sci. 2000 [Google Scholar]
- 26.Rivera WL, Santos SR, Kanbara H. Prevalence and genetic diversity of Entamoeba histolytica in an institution for the mentally retarded in the Philippines. Parasitol Res. 2006;98(2):106–110. doi: 10.1007/s00436-005-0024-8. [DOI] [PubMed] [Google Scholar]
- 27.Fujishima T, Nishise S, Ichihara M, Kobayashi S, Takeuchi T. Difficulties in the treatment of intestinal amoebiasis in mentally disabled individuals at a rehabilitation institution for the intellectually impaired in Japan. Chemotherapy. 2010;56(4):348–352. doi: 10.1159/000320187. [DOI] [PubMed] [Google Scholar]
- 28.Braun TI, Fekete T, Lynch A. Strongyloidiasis in an institution for mentally retarded adults. Arch Int Med. 1988;148(3):634–636. [PubMed] [Google Scholar]
- 29.Omar MS, al-Awad ME, al-Madani AA. Giardiasis and amoebiasis infections in three Saudi closed communities. J Trop Med Hyg. 1991;94(1):57–60. [PubMed] [Google Scholar]
- 30.Sarasiabi SK, Madani AH, Zare S. Prevalence of intestinal parasites in primary school pupils of Bandar Abbas. J Hormozgan Univ Med Sci. 2002;5(4):25–30. [Google Scholar]
- 31.Khademi Z, Arman M. Prevalence of intestinal parasites in children under 8 years old of kindergarten and school students of Bandar Abbas. J Infect Trop Dis. 2010;51:31–35. [Google Scholar]
- 32.Van Doorn HR, Koelewijn R, Hofwegen H, Gilis H, Wetsteyn JC, Wismans PJ, et al. Use of enzyme-linked immunosorbent assay and dipstick assay for detection of Strongyloides stercoralis infection in humans. J Clin Microbial. 2007;45(2):438–442. doi: 10.1128/JCM.01735-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anamnart W, Pattanawongsa A, Intapan PM, Maleewong W. Factors affecting recovery of Strongyloides stercoralis larvae: an approach to a newly modified formalin-ether concentration technique for diagnosis of strongyloidiasis. J Clin Microbiol. 2010;48(1):97–100. doi: 10.1128/JCM.01613-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nasiri V, Esmailnia K, Karim G, Nasir M, Akhavan O. Intestinal parasitic infections among inhabitants of Karaj City, Tehran province, Iran in 2006–2008. Korean J Parasitol. 2009;47(3):265–268. doi: 10.3347/kjp.2009.47.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gatti S, Lopes R, Cevini C, Ijaoba B, Bruno A, Bernuzzi AM, et al. Intestinal parasitic infections in an institution for the mentally retarded. Ann Trop Med Parasitol. 2000;94(5):453–460. doi: 10.1080/00034983.2000.11813564. [DOI] [PubMed] [Google Scholar]


