Abstract
Objective
To investigate a case of mass mortality of Garra rufa (G. rufa) from a fish hatchery farm in Slovakia.
Methods
Causative bacterial agent was swabbing out of affected fish skin area and subsequently identified using commercial test system. Antibiotic susceptibility was determined by the disk diffusion method.
Results
Infected G. rufa was characterized by abnormal swimming behaviour, bleeding of skin lesions and local haemorrhages. Despite of using recommended aquatic antibiotic treatment no improvement was achieved and Aeromonas sobria (A. sobria) was identified as a causative agent of fish mortality. Due to massive fish mortality, antibiotic susceptibility of pure isolated culture of A. sobria was evaluated employing eight antibiotics against human infections. A. sobria was resistant only against one antibiotic, namely ampicilin.
Conclusions
These results indicate that A. sobria can act as a primary pathogen of G. rufa and may be a potential risk factor for immunodeficient or immunoincompetent patients during the ichthyotherapy.
Keywords: Garra rufa, Ichthyotherapy, Aeromonas sobria, Antibiotic treatment, Antibiotic susceptibility
1. Introduction
Ichthyotherapy, an alternative biotherapeutic method, has been shown to be effective in the treatment of patients with psoriasis and eczema[1]–[3]. The Kangal Spa in the Central Anatolia region of Turkey is the place where ichthyotherapy was applied for therapeutic purposes for the first time. Two different types of therapeutic fish, Cyprinion macrostomus and Garra rufa (G. rufa), have been identified and recommended for therapeutic purposes[4].
Nowadays, ichthyotherapy is becoming a more popular method for treatment of skin diseases as well as for improving of skin regeneration in healthy subjects. With increasing application of ichthyotherapy there is a potential risk of zoonotic infection transmission from fish or water to humans.
Aeromonas infections are probably the most common bacterial diseases diagnosed in cultured warmwater fish[5]–[7]. The common occurrence of this disease relates to stress conditions such as poor water quality, overcrowding, or rough handling. Aeromonas spp. are known to cause diarrhea, necrotizing fasciitis and sepsis in patients with hepatic diseases, diabetes mellitus and immunocompromised status[8]–[10]. In addition, skin and soft-tissue infections, including wound infections, are the second most frequent location of isolations of Aeromonas spp. in clinical samples, after the gastrointestinal tract[7],[11],[12].
A very recent study has provided the first suggestive evidence of successful colonization and infection by particular strain of Aeromonas spp. after transmission from water to human[13]. Moreover, several reported cases have supported this evidence. Recently, Manresa et al described two pediatric cases of Aeromonas hydrophila (A. hydrophila) folliculitis associated with use of recreational water facilities[14]. Similarly, Mulholland and Yong-Gee reported two young adult patients with a severe inflammatory folliculitis eruption attributed to possible contamination of a poorly maintained home spa bath with A. hydrophila[15].
In this study, a case of mortality of G. rufa from a fish hatchery farm in Slovakia was investigated. We demonstrate that A. sobria, resistant to current recommended treatment, caused the mass mortality of fish. Additionally, an antibiotic susceptibility of isolated A. sobria was evaluated.
2. Materials and methods
2.1. Identification of causal agent of bacterial infection
For laboratory examination, four specimens of G. rufa with pronounced exophthalmus, bleeding of the eyes and fins, and locomotor ataxia were taken. For bacteriological analysis sterile cotton swabs were used to collect samples either from affected area of skin lesions and fins or from skin of clinically healthy fish. These samples were used to inoculate into Columbia sheep blood agar (MkB Test, Slovakia). The blood agar plates were incubated at 37 °C and 30 °C for a period of 2 days. Suspected single colonies on blood agar plates were re-streaked onto fresh media to obtain pure isolates. These isolates were identified using the Micro-LA test system (Erba Lachema, Czech Republic).
2.2. Antibiotic susceptibility test
Antibiotic susceptibility was determined by the disk diffusion method with 8 antibiotic disks according to the criteria of the Clinical and Laboratory Standards Institute (CLSI)[16] on Mueller-Hinton agar (Oxoid, Hampshire, UK). The following antimicrobial agents (disk content indicated in parentheses) were tested: amikacin (10 µg), ampicillin (10 µg), cefalotin (30 µg), cefepime (30 µg), cefotaxime (30 µg), ceftazidime (30 µg), ceftriaxone (30 µg), gentamicin (10 µg). Escherichia coli ATCC 25922 was used as the control.
3. Results
3.1. Identification of Aeromonas sobria (A. sobria)
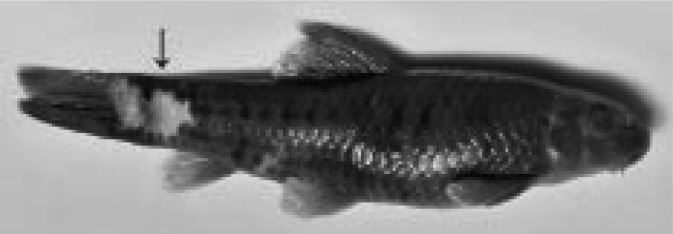
In all four specimens of G. rufa presenting skin ulcerations (Figure 1), bacteria can be isolated directly from skin lesions. The bacterial cultures were dominated by the appearance of white-grey colonies on blood agar plates. Using the Micro-LA test system, these bacteria were found to belong to the group of motile aeromonads. A. sobria isolated from affected fish was characterized by hemolytic colonies when grown at 30 °C. Only very weak growth was seen at 37 °C.
Figure 1. Erosion of the skin observed in therapeutic fish G. rufa. Arrow indicates affected skin.
3.2. Antibiotic susceptibility
Isolated causative bacterial agent of mortality of G. rufa, A. sobria, was tested on antibiotic susceptibility using eight antibiotics against human infections. Among all antibiotics, A. sobria isolate was resistant only against one antibiotic, namely ampicilin.
4. Discussion
An increasing popularity of ichthyotherapy and establishment of numerous ichthyotherapeutic centres are accompanied by more frequent monitoring of water quality and microbial contamination due to possible risk of infection development in humans after water-to-human transmission.
Ichthyotherapy, an alternative and complementary treatment, reduces illnesses such as psoriasis[4]. The skin lesions in patients with psoriasis can be secondary infected with bacteria[17],[18]. Many wound and skin infections that complicate skin lesions are caused by mixed bacterial flora. Aerobic and anaerobic; gram-negative and gram-positive organisms, whose origins are the oral, gastro-intestinal and skin flora may be present in such infections. Moreover, various microorganisms are associated with the provocation and/or exacerbation of psoriasis, but their roles in the disease pathogenesis are unknown[19],[20]. Brook and colleagues isolated 36 different bacteria from secondary infected psoriasis lesions in 23 specimens[17]. The most predominant bacteria were aerobic or facultative bacteria.
Another source of secondary infections in psoriasis lesions could be water or fish itself in bathing tub during ichthyotherapy procedure[21]. In this study, we identified A. sobria as a causative bacterial agent which caused mortality of therapeutic fish G. rufa. Similarly, author of recent study described a case of mass mortality of G. rufa from a private fish hatchery farm in Korea caused by fish pathogenic bacteria Citrobacter freundi[22]. However, healthy individuals exposed to this bacteria are not very likely to get disease, immunodeficient or immunoincompetent people as well as people with other disease problems such as psoriasis and atopic dermatitis are at the highest risk. In a very recent study[13], authors provide the first suggestive evidence of successful colonization and infection by Aeromonas species after transmission from water to human. In addition, there is an evidence that proteolytic extracellular products from bacterial pathogen A. hydrophila have the ability to inhibit skin antimicrobial peptides[23]. This evidence suggests that Aeromonas spp. could disrupt microbial skin barrier through inhibition of antimicrobial peptides.
The presence of skin lesions, local haemorrhages and locomotor ataxia in G. rufa infected with A. sobria is in agreement with the signs of disease found in fish suffering from aeromonad infections[24]. Aeromonad infections have often been related to changing water temperature[25]. Other factors, significantly related to increasing susceptibility of fish to aeromonad infections, are overcrowding, rough handling, transfer of fish, poor nutritional status and fungal and parasitic infections[26]. In addition, fish which are in poor environments due to unsatisfactory water quality such as high nitrite levels, low levels of dissolved oxygen, or high levels of carbon dioxide are more susceptible to infection by Aeromonas spp.
In conclusion, the findings of the present study provide the first evidence that A. sobria is a causative bacterial agent of mass mortality of therapeutic fish G. rufa. In addition, isolated A. sobria was resistant to ampicilin but sensitive to several antibiotics against human infections.
Acknowledgments
This work was supported by the Operational Program Research and Development and co-financed with European Fund for Regional Development (EFRD) with the grant number ITMS 26240220020 for establishment of biotherapeutic facility and technology proposal for production and development of bio-drugs.
Footnotes
Foundation Project: This work was financially supported by the Operational Program Research and Development and European Fund for Regional Development (EFRD) (grant No. ITMS 26240220020).
Conflict of interest statement: We declare that we have no conflict of interest.
References
- 1.Fackler R, Augustin M. Natural therapy of psoriasis. Biol Med. 2001;30:121–125. [Google Scholar]
- 2.De Groot A, Conemans J. Doctor fish for psoriasis? Ned Tijdschr Dermatol Venereol. 2004;14:406–408. [Google Scholar]
- 3.Grassberger M, Hoch W. Ichthyotherapy as alternative treatment for patients with psoriasis: a pilot study. Evid Based Complement Alternat Med. 2006;3:483–488. doi: 10.1093/ecam/nel033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Özcelik S, Polat HH, Akyol M, Yalcin AN. Kangal hot spring with fish and psoriasis treatment. J Dermatol. 2000;27:386–389. doi: 10.1111/j.1346-8138.2000.tb02188.x. [DOI] [PubMed] [Google Scholar]
- 5.Martinez-Murcia AJ, Saavedra MJ, Mota VR, Maier T, Stackebrandt E, Cousin S. Aeromonas aquariorum sp. nov., isolated from aquaria of ornamentak fish. Int J Syst Evol Microbiol. 2008;58:1169–1175. doi: 10.1099/ijs.0.65352-0. [DOI] [PubMed] [Google Scholar]
- 6.Jiravanichpaisal P, Roos S, Edsman L, Liu H, Soderhall K. A highly virulent pathogen, Aeromonas hydrophiia from the freshwater crayfish Pacifactacus leniesculus. J Invertebr Pathol. 2009;101:56–66. doi: 10.1016/j.jip.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Choresca CH, Gomez DK, Han JE, Shin SP, Kim JH, Jun JW, et al. Molecular detection of Aeromonas hydrophila isolated from albino catfish, Clarias sp. reared in an indoor commercial aquarium. Korean J Vet Res. 2010;50:331–333. [Google Scholar]
- 8.Ko WC, Lee HC, Chuang YC. Aeromonas bacteremia: review of 59 episodes. Clin Infect Dis. 1995;20:1298–1304. doi: 10.1093/clinids/20.5.1298. [DOI] [PubMed] [Google Scholar]
- 9.Hsueh PR, Teng LJ, Lee LN, Yang PC, Chen YC, Ho SW, et al. Indwelling device-related and recurrent infections due to Aeromonas species. Clin Infect Dis. 1998;26:651–658. doi: 10.1086/514587. [DOI] [PubMed] [Google Scholar]
- 10.Cui H, Hao S, Arous E. A distinct cause of necrotizing fasciitis: Aeromonas veronii biovar sobria. Surg Infect. 2007;8:523–528. doi: 10.1089/sur.2006.046. [DOI] [PubMed] [Google Scholar]
- 11.Altwegg M. Aeromonas and Plesiomonas. In: Muray PR, Barton EJ, Pfaller MA, Tenover FC, Yolken RH, editors. Manual of clinical microbiology. Washington, DC: Editorial American Society for Microbiology; 1999. pp. 507–516. [Google Scholar]
- 12.Behera B, Bhoriwal S, Mathur P, Sagar S, Singhal M, Misra MC. Post-traumatic skin and soft tissue infection due to Aeromonas hydrophila. Indian J Crit Care Med. 2011;15:49–51. doi: 10.4103/0972-5229.78228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khajanchi BK, Fadl AA, Borchardt MA, Berg RL, Horneman AJ, Stemper ME, et al. Distribution of virulence factors and molecular fingerprinting of Aeromonas species isolates from water and clinical samples: suggestive evidence of water-to-human transmission. Appl Environ Microbiol. 2010;76:2313–2325. doi: 10.1128/AEM.02535-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manresa MJ, Villa AV, Giralt AG, Gonzales-Ensenat MA. Aeromonas hydrophila folliculitis associated with an inflatable swimming pool: mimicking Pseudomonas aeruginosa infection. Pediatr Dermatol. 2009;5:601–603. doi: 10.1111/j.1525-1470.2009.00993.x. [DOI] [PubMed] [Google Scholar]
- 15.Mulholland A, Yong-Gee S. A possible new cause of spa bath folliculitis: Aeromonas hydrophila. Aust J Dermatol. 2008;49:39–41. doi: 10.1111/j.1440-0960.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 16.Clinical and Laboratory Standards Institute . Performance standards for antimicrobial susceptibility testing; 15th informational supplement. Philadephia: Clinical and Laboratory Standards Institute; 2005. pp. M100–S15. [Google Scholar]
- 17.Brook I, Frazier EH, Yeager JK. Microbiology of infected pustular psoriasis lesions. Int J Dermatol. 1999;38:579–581. doi: 10.1046/j.1365-4362.1999.00766.x. [DOI] [PubMed] [Google Scholar]
- 18.Wakkee M, de Vries E, van den Haak P, Nijsten T. Increased risk of infectious disease requiring hospitalization among patients with psoriasis: a population-based cohort. J Am Acad Dermatol. 2011 doi: 10.1016/j.jaad.2010.08.036. [DOI] [PubMed] [Google Scholar]
- 19.Buslau M, Menzel I, Holtzmann H. Fungal flora of human faeces in psoriasis and atopic dermatitis. Mycoses. 1990;33:90–94. doi: 10.1111/myc.1990.33.2.90. [DOI] [PubMed] [Google Scholar]
- 20.Gudjonsson JE, Johnston A, Sigmundsdottir H, Valdimarsson H. Immunopathogenic mechanisms in psoriasis. Clin Exp Immunol. 2004;135:1–8. doi: 10.1111/j.1365-2249.2004.02310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finkelstein R, Oren I. Soft tissue infections caused by marine bacterial pathogens: epidemiology, diagnosis, and management. Curr Infect Dis Rep. 2011 doi: 10.1007/s11908-011-0199-3. [DOI] [PubMed] [Google Scholar]
- 22.Baeck GW, Kim JH, Choresca C, Gomez DK, Shin SP, Han JE, et al. Mass mortality of doctor fish (Garra rufa obtuse) caused by Citrobacter freundii infection. J Vet Clin. 2009;26:150–154. [Google Scholar]
- 23.Schadich E, Cole AL. Inhibition of frog antimicrobial peptides by extracellular products of the bacterial pathogen Aeromonas hydrophila. Lett Appl Microbiol. 2009;49:384–387. doi: 10.1111/j.1472-765x.2009.02677.x. [DOI] [PubMed] [Google Scholar]
- 24.Austin B, Austin DA. Bacterial fish pathogens. West Sussex, England: Ellis Howard; 1987. pp. 225–247. [Google Scholar]
- 25.Roberts RJ. Motile aeromonad septicaemia. In: Inglis V, Roberts RJ, Cambell B, MacRae IH, editors. Bacterial diseases of fish. Oxford, England: Blackwell Science; 1993. pp. 143–156. [Google Scholar]
- 26.Aoki T. Motile aeromonads (Aeromonas hydrophila) In: Woo PT, Bruno DW, editors. Fish diseases and disorders. Wallingford: CABI Publishing; 1999. pp. 427–453. [Google Scholar]


