Abstract
A 24 year-old Malay lady presented with high grade fever, myalgia, generalized rashes, severe headache and was positive for dengue serology test. Her lowest platelet count was 45 × 109 cells/L. She complained of sudden onset of painlessness, profound loss of vision bilaterally 7 days after the onset of fever. On examination, her right eye best corrected vision was 6/30 and left eye was 6/120. Her anterior segment examination was unremarkable. Funduscopy revealed there were multiple retinal haemorrhages found at posterior pole of both fundi and elevation at fovea area with subretinal fluid. Systemic examination revealed normal findings except for residual petechial rashes. She was managed conservatively. Her vision improved tremendously after 2 months. The retinal hemorrhages and foveal elevation showed sign of resolving. Ocular manifestations following dengue fever is rare. However, bilateral visual loss can occur if both fovea are involved.
Keywords: Dengue fever, Maculopathy, Foveolitis
1. Introduction
Dengue fever is a viral infection transmitted through the bite of an infected female Aedes aegypti/albopictus mosquito[1]. Although dengue fever has afflicted mankind for centuries, the first case with ophthalmic manifestation was reported only in the late 1980s[2]. The ocular manifestation has been neglected and its importance been ignored. Its complication ranges from mild blurring of vision to significant morbidity with severe visual impairment[2]. We present a case of a young lady who presented with sudden onset of bilateral profound loss of vision following dengue fever.
2. Case report
A 24 year-old Malay lady was diagnosed to have dengue fever based on serological test and the lowest platelet count was 45 × 109 cells/L. She presented with sudden onset of painlessness, profound loss of vision of both eyes. She was just discharged from another hospital for dengue fever. She denied any history of bleeding or blood transfusion during the previous admission.
She noticed sudden loss of vision upon awaken from sleep, a day after she was discharged from the hospital. It was not preceded by metamorphopsia or micropsia. There was no eye discharge or eye redness. She denied any pain associated with eye movement. There was no history of floaters or flashes of light and no history of recent head trauma or any injury to the eyes. She also denied any change in her colour saturation. She has no underlying medical problem.
Ocular examination showed her right eye best corrected vision was 6/30 and left eye was 6/120. Refraction of right eye was -1.75D and left eye was -1.25D. There was absence of any conjunctival or subconjunctival haemorrhages and no sign of blood in anterior chamber. Funduscopic examination had shown the presence of multiple retinal haemorrhages at the macula of both fundi. There was elevation of fovea area of about 1 disc diameter with the presence of subretinal fluid. There was absence of yellow deposits or any hard exudates.
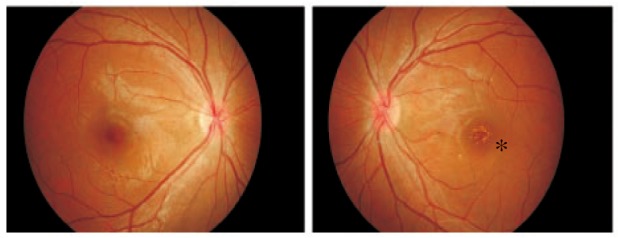
She was treated conservatively and reviewed after one month. Her right eye vision improved to 6/7.5. However, the left eye did not show any improvement in visual acuity. Retinal hemorrhages and foveal elevation were resolved but there were multiple retinal yellowish deposits at fovea of left eye (Figure 1).
Figure 1. Multiple retinal yellowish deposits at fovea of left eye (*).
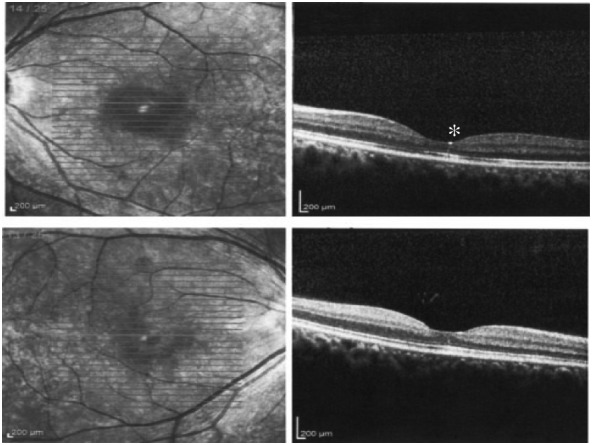
Amsler grid test had shown the presence of central scotoma in the left eye but no significant finding in the right eye. Fundus fluorescein angiography (FFA) revealed no leakage or any hyperfluorescence or hypofluorescence in both eyes (Figure 2). The presence of retinal exudates was further visualized by OCT imaging (Figure 3).
Figure 2. FFA showed normal findings.
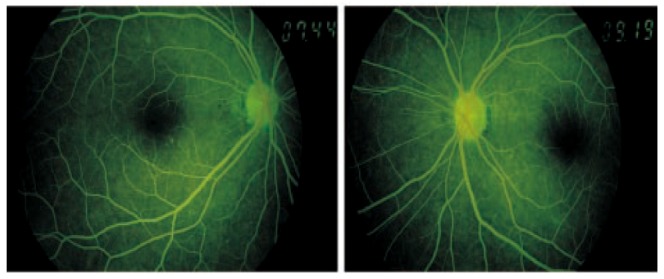
Figure 3. OCT imaging showed normal findings of the right eye but presence of retinal exudates in the left eye (*).
2. Discussion
The earliest report of a dengue fever epidemic in the Malaysia Peninsula was from Singapore in 1901. The disease seems to become endemic with few major epidemics[3]. Ophthalmologists should thus be aware of the various ocular manifestations of dengue, as the incidence and geographic distribution of dengue has increased dramatically in the past several years. Furthermore, patients of dengue fever with marked thrombocytopenia (platelet count < 50×109 cells/L) are predisposed to be more likely accompanied by severe ocular disease that can lead to impairment of vision[4],[5].
Dengue fever is the most common mosquito borne viral disease in humans[6]. Dengue fever is characterized by an abrupt onset of fever after 2 to 7 day of incubation period, with temperature reaching 41 °C. Other symptoms include severe headaches, myalgias, arthralgias, nausea, vomiting and a rash[1],[7].
Dengue fever is known to affect various organs including the eye[2],[6]. Ocular manifestations in dengue fever are uncommon[1]. The main presenting complaint was blurring of vision[1]. The majority of ocular changes are in the posterior segment including intraretinal haemorrhages, cotton wool spots and diffuse retinal edema[1],[2],[6],[7]. The mean interval between the onset of visual symptoms and the systemic manifestations of dengue fever ranged between 6-7 days. The delay of ocular manifestation from the onset of systemic dengue fever raised the possibility of immune-mediated pathophysiology rather than direct viral infection. A week interval corresponds to the time of onset of antibody production, immune complex deposition, or production of autoantibodies[1].
Optical coherence tomography showed 3 patterns of maculopathy: 1) diffuse retinal thickening; 2) cystoid macular edema; and 3) foveolitis[8]. Our patient presented with a discrete and well-defined yellow lesion appeared to be localized to the outer retina. This condition is termed as foveolitis based on the unique features captured on OCT. There is evidence of focal disruption of the outer neurosensory retina at the fovea with normal foveal contour in OCT in all eyes of patients at presentation in one study done in Singapore[7]. In our case, the OCT was done quite later and the vital earlier finding on OCT was not detected.
Ocular alterations in dengue are usually self-limiting. The mode of treatment ranges from conservative treatment to immunosupression depending on the visual acuity[7]. Most of the cases resolve without specific treatment[8]. The resolution of the ocular manifestation in bilateral eyes involvement may not be symmetrical. Visual recovery usually corresponds with improving platelets levels, however, scotomata may persist for several weeks in some cases despite the resolution of ocular signs[9]. Our patient was not given any medications and noted improvement of vision on the subsequent visits. The right eye gained good vision earlier than the left eye which worse visual acuity at presentation.
In a retrospective study done in Singapore, patients presented with foveolitis were treated with immunosuppressive agents and improvements of vision were observed in all eyes. However, it was difficult to determine whether good visual outcome was the result of treatment or part of the natural course of the disease. Thus, a prospective, randomized clinical study is necessary to determine the effect of treatment on the course of foveolitis[1].
Footnotes
Conflict of interest statement: We declare that we have no conflict of interest.
References
- 1.Lim WK, Mathur R, Koh A, Yeoh R, Chee SP. Ocular manifestations of dengue fever. Ophthalmol. 2004;111:2057–2064. doi: 10.1016/j.ophtha.2004.03.038. [DOI] [PubMed] [Google Scholar]
- 2.Su DH, Bascal K, Chee SP, Flores JV, Lim WK, Cheng BC, et al. Prevalence of dengue maculopathy in patients hospitalized for dengue fever. Ophthalmol. 2007;114:1743–1747. doi: 10.1016/j.ophtha.2007.03.054. [DOI] [PubMed] [Google Scholar]
- 3.George R. Current status of the knowledge of dengue/DHF/DSS in Malaysia: Clinical aspects. Phil J Microbial Infect Dis. 1992;21:41–47. [Google Scholar]
- 4.Sumardi U, Nelwan EJ. Retinal hemorrhage in dengue hemorrhagic fever. Acta Med Indones. 2011;43:66–67. [PubMed] [Google Scholar]
- 5.Kumar V, Kataria R, Mehta V. Dengue hemorrhagic fever: A rare cause of pituitary tumor hemorrhage and reversible vision loss. Indian J Ophthalmol. 2011;59:311–312. doi: 10.4103/0301-4738.82002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bascal KE, Chee SP, Cheng CL, Flores JV. Dengue-associated maculopathy. Arch Ophthalmol. 2007;125:501–510. doi: 10.1001/archopht.125.4.501. [DOI] [PubMed] [Google Scholar]
- 7.Loh BK, Bacsal K, Chee SP, Cheng BC, Wong D. Foveolitis associated with dengue fever: A case series. Ophthalmologica. 2008;222:317–320. doi: 10.1159/000144074. [DOI] [PubMed] [Google Scholar]
- 8.Teoh SC, Chee CK, Laude A, Goh KY, Barkham T, Ang BS. Eye Institute Dengue-related Ophthalmic Complications Workgroup. optical coherence tomography patterns as predictors of visual outcome in dengue-related maculopathy. Retina. 2010;30:390–398. doi: 10.1097/IAE.0b013e3181bd2fc6. [DOI] [PubMed] [Google Scholar]
- 9.Ujiie M, Moi ML, Takeda N. Dengue maculopathy in a traveler. Am J Trop Med. 2011;85:965–966. doi: 10.4269/ajtmh.2011.11-0120. [DOI] [PMC free article] [PubMed] [Google Scholar]


