Abstract
Diatal radius fractures (DRFs) are typical fractures of relatively fit persons with osteoporotic bone who remain active into older age. Traditionally, DRFs in older patients have been treated with closed reduction and cast immobilization. Considering the increasing life expectancy of the elderly population, appropriate management of these fractures is of growing importance. Decision making for surgical or nonsurgical approach to osteoporotic DRFs is difficult. These decisions are often made based on the data from treatments of much younger patients. The current literature concerning the treatment of DRFs in the elderly individuals is more controversial. Some investigators have recommended open reduction internal fixation (ORIF) as treatment for unstable DRFs in older patients, while others have suggested that elderly patients should be treated nonsurgically even if there is an unstable fracture situation because fracture reduction is not associated with functional outcomes as in younger patients. This article reviews the different treatment options for DRFs in the elderly individuals reported in the recent literature.
Keywords: distal radius fracture, osteoporosis, elderly, treatment, geriatric trauma
Introduction
Diatal radius fractures (DRFs) are typical fractures of relatively fit persons with osteoporotic bone. Traditionally, DRFs in older patients have been treated with closed reduction and cast immobilization.1 In unstable fracture patterns cast immobilization fails to maintain fracture reduction until bone union and therefore leads to malunion in more than 50%.2 Some authors have recommended anatomic restoration of displaced, unstable DRFs in young patients to achieve best clinical results.3 Many of the very old and frail individuals with low functional demands can accept and live with deformity and dysfunction of the wrist.4
Considering the increasing life expectancy of the elderly population, appropriate management of these fractures is of growing importance. Decision making for surgical or nonsurgical approach to osteoporotic DRFs is difficult. These decisions are often made based on the data from treatments of much younger patients.3 The current literature concerning the treatment of DRFs in the elderly individuals is more controversial. There is unanimity in the literature that stable fractures can be treated with closed reduction and cast immobilization with satisfactory outcome.5 In unstable intra-articular DRFs, where fracture reduction cannot be maintained with cast immobilization, additional fixation is suggested.6
Epidemiology and Incidence
Osteoporosis is one of the most common problems affecting the elderly population.7 According to the World Health Organization (WHO), it is 1 of the 10 most costly diseases worldwide. Some recent studies have defined the relationship of a prior wrist fracture with subsequent osteoporotic fractures at other sites.8,9 In women, the risk of a hip fracture increases 1.4- to 1.8-fold if there was a previous wrist fracture. In older men, the risk of hip fracture increases 2.3- to 2.7-fold.10 Approximately 10% of white women older than 65 years will sustain a DRF during their remaining lifetime.11 Distal radius fractures have significant associated social–economic costs.
Relevant Anatomy
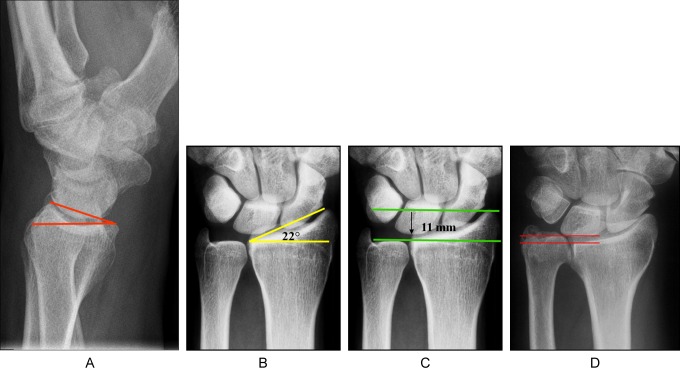
Specific radiographic parameters with biomechanical and clinical implications have been developed to assess the radiocarpal joint (Figure 1).
Figure 1.
Anatomy of the distal radius. A, Palmar tilt. B, Radial inclination. C, Radial length. D, Ulnar variance.
Palmar Tilt
Palmar tilt is measured as the angle subtended by the line perpendicular to the long axis of the radius and a second line drawn from the dorsal to volar cortex of the distal radius (average: 10°-12°).
Radial Inclination
Radial inclination is assessed as the angle between the longitudinal axis of the radius and a line connecting the radial cortex of the apex of the radial styloid and the central point of the sigmoid notch of the distal radius (average: 22°-23°)
Radial Length
Radial length is assessed as the distance between the apex of the radial styloid and the level of the ulna head at the distal radioulnar joint (DRUJ) (average: 11 mm-12 mm):
Ulnar Variance
Ulnar variance is defined as the difference in axial length between the central point of the ulnar corner of the sigmoid notch of the distal radius and the most distal extent of the ulnar head on the PA view.
Classification and Imaging
In the literature many classifications for DRFs exits. They have been developed to predict prognosis, guide a treatment plan, and improve scientific communication between treating surgeons. Mostly used classifications systems include the Frykman,12 Melone,13 Jupiter and Fernandez,14 and the AO classifications.15 None of them have been shown to be superior in clinical use. From the scientific and research point of view, the AO classification has been accepted and used in the latest literature. As each of the classification systems relies on individual radiographic assessment, there are limitations due to either the fracture pattern or radiographic technique. This results in poor interobserver and intraobserver reliability.16 Computer tomography may be used in complex intra-articular fractures for preoperative planning and to assess associated injuries.
Assessment of Instability
Initially all displaced DRFs are recommended to be reduced under local or general anesthesia in the emergency department and then immobilized. Fracture reduction is assessed using radiographs after manipulation. Primary reduction of the fracture is considered to be acceptable when dorsal tilt does not exceed 20°, radial shortening is not more than 3 mm, and intra-articular step off does not exceed 2 mm.4 Fracture instability is also defined as a failure to hold the reduced position of the fracture within the forearm cast with a loss of reduction at 1 or 2 weeks. Osteoporosis weakens the metaphyseal bone by decreasing trabecular bone volume,17 so osteoporotic DRFs very often show a large metaphyseal defect or void, which increases fracture instability.18 Nesbitt et al reported that the age was the only statistically significant risk factor in predicting secondary displacement and instability treating DRFs by closed reduction and immobilization. The risk for displacement with an unacceptable radiographic result was found to increase in patients older than 58 years.19 Sakai et al reported a significant correlation between increasing displacement of distal fracture fragment and lower bone mineral density.20
Treatment Options
The current literature concerning the optimal treatment options for osteoporotic DRFs is controversial. Traditionally, DRfs in the elderly individuals have been treated with closed reduction and cast immobilization.1 Stable fractures can be treated with closed reduction and cast immobilization with satisfactory outcome.5 In unstable DRFs, where fracture reduction cannot be maintained with cast immobilization, additional fixation is suggested.6
Closed Reduction and Cast Immobilization
Current protocol for nonoperative treatment of DRFs includes initially fracture reduction under local or general anesthesia in the emergency department and then immobilized with a below-forearm splint. After the primary swelling has decreased, the slab converted to a complete below-elbow cast at 1 or 2 weeks. Secondary loss of primary reduction can occur up to 2 weeks after primary closed reduction. In these cases repeated manipulation, specially in the osteoporotic bone, is insufficient and correlated with the incidence of Complex Regional Pain Syndrome type 1 and is not advised.4 In total, DRFs are immobilized in a forearm cast in neutral position of the wrist for 6 weeks. Active and passive finger motion is encouraged early. A therapy program after cast removal including active assisted motion of the wrist and grip strengthening is started at 6 weeks. No study has been able to show any significant differences between long- and short-arm cast for the treatment of DRFs. The morbidity associated with an above-elbow cast for 6 weeks in older patients is not justifiable. The elbow, fingers, and the thumb should be left free to avoid stiffness. In osteoporotic unstable DRFs, where maintenance of fracture reduction does not rely cast immobilization, the cast applied is for pain reduction and fracture support.
Young and Rayan,21 assessing the treatment outcome of nonoperative management for DRFs in patients older than 60 years, found no correlation between unsatisfactory radiographic results and functional outcomes. Six of 10 wrists with intra-articular fractures developed progression of radiocarpal and distal radioulnar joint arthrosis. Only 2 of these patients with radiographic signs of arthrosis had an unsatisfactory clinical outcome. Persistent nerve symptoms were present in 3 (12%) of 25 patients. An obvious clinical deformity (prominence of the ulnar head) was present in 14 (56%) of the 25 evaluated patients. None of the patients were dissatisfied with the appearance of the wrist. Gartland and Werley score revealed 22 patients (88%) with excellent to good results and 3 patients (12%) with fair or poor results. One patient developed a complex regional pain syndrome. Similar results were reported by Beumer et al.4
Closed Reduction and Percutaneous Pinning
A variety of different surgical techniques for percutaneous pinning have been described in the literature including pins (1.4 mm-1.6 mm K-wires) placed through the radial styloid, crossed pins entering the dorsal cortex and intrafocal pinning through the fracture site (Figure 2).
Figure 2.
Osteoporotic distal radius fracture with concomitant distal ulna fracture stabilized with K-wires.
Pinning alone may not be enough to maintain articular and metaphyseal support, as K-wires are not load-bearing devices. Additionally a forearm splint is necessary to neutralize the bending forces across the metaphysis. The wires are left up to 4 weeks and the forearm cast left for 6 weeks. Percutaneous pinning is a relative simple method of fixation that is recommended for reducible extra-articular and simple intra-articular DRFs without metaphyseal comminution and with good bone quality. The primary risk of this technique is the injury of the superficial radial nerve. The other consideration is pin track infection.
Azzopardi et al22 performed a prospective, randomized study with 57 patients older than 60 years of age with unstable, extra-articular DRFs to compare the results of immobilization in a forearm cast alone with that using additional, percutaneous pinning. Patients treated by pinning had statistically significant improvement in radiological parameters at 1 year. There was no significant difference in clinical results according to pain, range of motion, grip strength, activities of daily living, and the SF-36 score. One patient suffered from pin track infection, which required removal of the K-wires at 2 weeks. The authors concluded that percutaneous pinning of unstable, extra-articula DRFs provides just a minimal improvement in the radiological parameters compared with immobilization in a cast alone. This did not correlate with an improved functional outcome in the elderly population. Similar findings were described by McQueen et al.5
External Fixation
External fixation (EF) as treatment option for DRFs was primarily reserved for highly unstable and severely comminuted fractures. Its use is simple and rapid. This technique relies on ligamentotaxis, which indirectly pulls the fracture fragments out to length through longitudinal traction (Figure 3). External fixator in DRFs was a joint spanning (wrist bridging) implant with fixation in the radius diaphysis and in the metacarpal. Relying on this technique, the EF does not directly address the reduction and maintenance of the dorsal tilt and intra-articular fragments. In a prospective randomized study, Roumen et al compared EF with closed reduction and immobilization for redisplaced DRFs in patients over 55 years. Patients treated with EF had significant better radiological results while the functional results did not show any difference.23
Figure 3.
Osteoporotic distal radius fracture with concomitant distal ulna fracture stabilized with K-wires and additional external fixator. Neither the radial inclination nor the radial length could be restored in this unstable fracture.
The other option of application of EF in DRFs is the nonbridging technique where the distal pins are placed into the distal fracture fragment without spanning the wrist joint. This technique limits joint stiffness and maintains the reconstructed dorsal tilt but is only applicable where there is sufficient space in the distal fragment. Atroshi et al compared in a randomized study the 2 different methods of EF in a cohort of older patients. They reported a better radial length at 1 year in the nonbridging group but no significant differences in functional results of both groups. Aketin et al described similar findings in a retrospective study with patients older than 65 years.24
In complex intra-articular DRFs with great metaphyseal void, additional intrafragmentary K-wires are required to directly maintain fracture reduction. Biomechanical studies have proven to increase fracture stability using supplementary K-wires.25 In this combination the joint spanning EF unloads and protects the reduced fracture until bone healing. Fu et al compared the combination of EF and buttress-maintain pinning method in patients older than 65 year with patients less than 60 years old. Neither the radiological results nor the functional results showed any significant difference between both the treatment groups.
Complications associated with EF are pin-track infection, iatrogenic lesion of the superficial radial nerve. Overdistraction of the wrist joint may lead to complex regional pain syndrome (CRPS). Usually the EF is applied for 6 weeks. Especially in osteoporotic bone quality with weak hold of the pins, loosening of the pins occurs quite early so that they have to be removed before definitive bone healing.
Open Reduction and Volar Locking Plate Fixation
The advantages of open reduction and internal fixation of DRFs are possibility of anatomical reduction and stable fixation allowing early postoperative wrist mobilization. As DRFs are hyperextension injuries and the dorsal cortex of the distal radius is weak, most of the fractures are displaced dorsally. Traditionally, all dorsally displaced DRFs were treated through a dorsal approach using a dorsal buttress plate. The problems of dorsal plating are extensor tenosynovitis with tendon rupture due to hardware prominence. To improve this tendon irritation, special low-profile steel plates and the Pi-plate were designed.26 To adapt to the anatomy of the dorsal distal radius, the Pi-plate (Synthes, Switzerland) was strapped to fit close to the dorsal aspect around the Lister’s tubercle. However, Campbell reported attrition ruptures of extensor tendons after dorsal Pi-plate application, and Kambouroglou and Axelrod described tendon ruptures and failure of the Pi-plate system.27
To overcome these problems of dorsal plating many authors favored the volar approach.28 Placing the plate to the almost flat contour of the volar cortex and the good exposure to main fragments, especially the ulnar dye punch fragment, are benefits of this approach.
Conventional volar plates require additional metaphyhseal support (bone graft, bone substitute, or additional dorsal plates) to avoid loss of reduction due to metaphyseal instability. The invention of volar fixed-angle plates led to increased mechanical rigidness and made dorsal metapyhseal bone grafting redundant.29 They act like an internal fixator unloading the usually comminuted dorsal metaphyseal bone. In a biomechanical study, the volar fixed-angle plate proved efficient in restoring the normal axial force distribution, superior to conventional palmar and dorsal T-plate fixation.30 The fixed-angle screws lock into the plate and do not rely on engagement of the screw threads in bone leading to better fixation in osteoporotic bone. The other advantage of locking plates is the good subchondral support of the distal fragments even in very short distal fracture fragments.
There are some studies that support the goal of anatomical reconstruction of the articular congruity and the radial length to achieve a satisfactory functional outcome in older aged population.
Jupiter et al31 evaluated 20 patients 60 years and older treated with open reduction internal fixation (ORIF) using palmar locking plates for re-displaced Colles’ type DRF. At an average follow-up of 38 months, they reported 7 excellent, 11 good, and 2 fair results using the patient rated wrist evaluation (PRWE) score and the Physical Activity Scale for the elderly. They described 1 patient with postoperative loss of reduction, 1 patient with transient neuritis of the radial sensory nerve, and another having a flexor pollicis longus rupture treated with tendon transfer. In 6 patients, hardware was removed due to dorsal wrist pain. The authors suggest ORIF as a treatment of older patients with displaced DRFs that have failed conservative management (Figure 4).
Figure 4.
Osteoporotic distal radius fracture treated with volar locking plate.
In our study, we reported 19 patients with a mean age of 61 years with dorsally displaced DRF were treated using a volar locking plate system.32 At final follow-up, the dorsal tilt was +1°, radial inclination 19.8°, and ulnar variance 1.0 mm. Mean loss of palmar tilt measured 1.9°, radial inclination 1.3°, and ulnar variance 0.4 mm. Mean wrist extension measured 58°, wrist flexion 41°, pronation 83°, and supination 84°. The Mayo Wrist Score showed 21% excellent, 58% good, 16% fair, and 5% poor results. No additional bone graft was used to fill the metaphyseal void. Two patients developed a CRPS and 1 patient developed a carpal tunnel syndrome 6 months after surgery, which was treated by open release and implant removal.
Despite these reports about good radiological and functional results Egol et al33 retrospectively compared outcomes for patients over the age of 65 years with a displaced DRF, who were treated surgically (plate fixation or EF) or nonsurgically (cast fixation). At 24 weeks, patients who underwent surgery had better wrist extension than those treated nonsurgically. At 1 year, this difference was not seen. No difference in disabilities of the arm, shoulder and hand (DASH) and pain scores at any time of the follow-up period was seen between the groups. Grip strength at 1 year was significantly better in the operative group. Radiographic results were better for patients in the operative group at each follow-up visit. There was no difference between the 2 groups with regard to complications. The authors concluded that minor limitations in the range of wrist motion and diminished grip strength, as seen with nonoperative treatment, did not limited functional recovery at 1 year.
In our retrospective study, we compared the clinical and radiological results of nonoperative treatment with volar locking plating of unstable DRFs in patients over 70 years.34 Radiographic results (dorsal tilt, radial inclination, and radial shortening) after unstable dorsally displaced DRFs were significantly better in patients treated by ORIF using a volar fixed-angle plate rather than those treated by cast immobilization. At a mean follow-up time of 4 years and 7 months, the clinical outcomes of active range of motion, the PRWE, DASH, and Green and O’Brien scores do not differ between the 2 methods of treatment. The pain level was significantly less in the CAST group, and this group experienced no complications. There was no difference between the subjective and functional outcomes for the surgical and the nonsurgical treatments in a cohort of patients older than 70 years.
Conclusion
As the population in some countries continues to age, the number of DRFs will increase as well. Even though these fractures are among the most common injuries treated by orthopedic, trauma, and hand surgeons, the treatment options are variable and remain a topic of debate. The weak osteoporotic bone quality makes fractures fixation of using various devices and implants difficult. Traditionally these fractures have been treated nonoperatively in older patients. With the evolution of the fixed-angle plates, there has been a change in the treatment of DRFs in the elderly individuals. Although locking plate systems provide superior stiffness and axial loading strength with improved fixation compared to standard plates they still have their limits.35 In our study over a mean 15-month period, 141 patients with a mean age of 57 years were treated for unstable dorsally displaced DRFs using a volar locking plate system. The overall complication rate was 27% (31 of 114). The most frequent problems were flexor and extensor tendon irritation (57% of the total number of complications), with 2 ruptures of the flexor pollicis longus tendon, 2 ruptures of the extensor pollicis longus tendon, 4 cases of extensor tendon tenosynovitis, and 9 cases of flexor tendon tenosynovitis. Carpal tunnel syndrome was observed in 3 patients, and CRPS occurred in 5 patients. In 2 cases, loosening of a single screw was seen. Delayed fracture union occurred in 3 patients, and intraoperative intra-articular screw displacement was observed in 1 patient.
Fixation of unstable dorsally displaced distal radius fractures with a fixed-angle plate provides sufficient stability with minimal loss of reduction. The very distal volar plate position may interfere with the flexor tendon system, too long screws can penetrate the extensor compartments, and distal screws in comminuted fracture patterns can cut through the subchondral bone and penetrate into the radiocarpal joint.
In the literature there is still no consensus regarding the best treatment option for unstable DRFs in the elderly individuals.36 Stable and reducible Colles fractures, which do not re-displace in a cast in the first 10 days after reduction, are treated nonoperatively with satisfactory radiologic and functional results.37
Chung et al systematically reviewed the current literature for the treatment options of DRFs in patients over the age of 60 years treated with 5 common techniques: volar locking plate system, nonbriding EF, bridging EF, percutaneous K-wire fixation, and cast immobilization.1 The authors concluded that despite worse radiographic results in the group with cast immobilization, functional results were no different from those in the surgically treated groups for patients above the age of 60 years. There were significant differences for all 5treatment groups regarding active range of motion, grip strength, or the DASH scores. Significant better radiological results were observed in the group of volar locking plates. Major complications requiring no surgery were mostly observed in the group of bridging EF. Major complications requiring secondary surgeries were observed in the group of the volar locking plates.
The poor correlation between the radiographic and functional outcomes in older people might be related to decreased functional demand on the wrist that is thought to be associated with aging.21 Anzarut et al38 found no correlation between dorsal angulation and wrist function, using the SF-12 and DASH questionnaires
From the patients’ point of view, the final result is largely determined by the presence or absence of pain while performing daily living activities. In our patients, the pain level was significantly less in the group treated nonoperatively. Patients of the ORIF group where the flexor tendons abraded against the volar plate and where dorsally protruding screws caused extensor tenosynovitis complained about wrist pain, requiring an additional surgery.
Volar fixed-angle plate systems have made plate osteosynthesis popular in elderly individuals with osteoporotic bone. In our study at 12 months after surgery, active range of motion (ROM), the pain level, the PRWE and the DASH scores were not different between the groups treated with cast immobilization or with volar locking plate. Although patients treated with ORIF had better grip strength through the entire time period, achieving an almost anatomical reconstruction did not convey any improved motion or better ability of daily living activities.39 If there is no significant difference between functional outcomes in the long-term after nonsurgical treatment or surgical treatment of unstable DRFs in the elderly individuals, indication of surgery factors like patient’s age, patient’s comfort (short immobilization time, early return to daily and sport activities), pre-injury daily activity level, lifestyle requirements, current medical conditions, and stage of osteoporosis should be included in the decision-making process.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91(8):1868–1873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88(9):1944–1951 [DOI] [PubMed] [Google Scholar]
- 3. McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function?. J Bone Joint Surg Br. 1988;70(4):649–651 [DOI] [PubMed] [Google Scholar]
- 4. Beumer A, McQueen MM. Fractures of the distal radius in low-demand elderly patients: closed reduction of no value in 53 of 60 wrists. Acta Orthop Scand. 2003;74(1):98–100 [DOI] [PubMed] [Google Scholar]
- 5. McQueen MM, Hajducka C, Court-Brown CM. Redisplaced unstable fractures of the distal radius: a prospective randomised comparison of four methods of treatment. J Bone Joint Surg Br. 1996;78(3):404–409 [PubMed] [Google Scholar]
- 6. McQueen MM, MacLaren A, Chalmers J. The value of remanipulating Colles’ fractures. J Bone Joint Surg Br. 1986;68(2):232–233 [DOI] [PubMed] [Google Scholar]
- 7. Kanis JA. The incidence of hip fracture in Europe. Osteoporos Int. 1993;3(suppl 1):10–15 [DOI] [PubMed] [Google Scholar]
- 8. Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. Study of osteoporotic fractures research group. N Engl J Med. 1995;332(12):767–773 [DOI] [PubMed] [Google Scholar]
- 9. Schousboe JT, Fink HA, Taylor BC, et al. Association between self-reported prior wrist fractures and risk of subsequent hip and radiographic vertebral fractures in older women: a prospective study. J Bone Miner Res. 2005;20(1):100–106 [DOI] [PubMed] [Google Scholar]
- 10. Jaglal SB, Weller I, Mamdani M, et al. Population trends in BMD testing, treatment, and hip and wrist fracture rates: are the hip fracture projections wrong?. J Bone Miner Res. 2005;20(6):898–905 [DOI] [PubMed] [Google Scholar]
- 11. Cummings SR, Black DM, Nevitt MC, et al. Appendicular bone density and age predict hip fracture in women. The study of osteoporotic fractures research group. JAMA. 1990;263(5):665–668 [PubMed] [Google Scholar]
- 12. Frykman G. Fracture of the distal radius including sequelae--shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function. A clinical and experimental study. Acta Orthop Scand. 1967;(suppl 108):143–153 [DOI] [PubMed] [Google Scholar]
- 13. Melone CP., Jr Articular fractures of the distal radius. Orthop Clin North Am. 1984;15(2):217–236 [PubMed] [Google Scholar]
- 14. Jupiter JB, Fernandez DL. Comparative classification for fractures of the distal end of the radius. J Hand Surg Am. 1997;22(4):563–571 [DOI] [PubMed] [Google Scholar]
- 15. Jupiter JB. Complex articular fractures of the distal radius: classification and management. J Am Acad Orthop Surg. 1997;5(3):119–129 [DOI] [PubMed] [Google Scholar]
- 16. Andersen DJ, Blair WF, Steyers CM, Jr, Adams BD, el-Khouri GY, Brandser EA. Classification of distal radius fractures: an analysis of interobserver reliability and intraobserver reproducibility. J Hand Surg Am. 1996;21(4):574–582 [DOI] [PubMed] [Google Scholar]
- 17. Crilly RG, Delaquerriere Richardson L, Roth JH, Vandervoort AA, Hayes KC, Mackenzie RA. Postural stability and Colles’ fracture. Age Ageing. 1987;16(3):133–138 [DOI] [PubMed] [Google Scholar]
- 18. Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20(4):208–210 [DOI] [PubMed] [Google Scholar]
- 19. Nesbitt KS, Failla JM, Les C. Assessment of instability factors in adult distal radius fractures. J Hand Surg Am. 2004;29(6):1128–1138 [DOI] [PubMed] [Google Scholar]
- 20. Sakai A, Oshige T, Zenke Y, Suzuki M, Yamanaka Y, Nakamura T. Association of bone mineral density with deformity of the distal radius in low-energy Colles’ fractures in Japanese women above 50 years of age. J Hand Surg Am. 2008;33(6):820–826 [DOI] [PubMed] [Google Scholar]
- 21. Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000;25(1):19–28 [DOI] [PubMed] [Google Scholar]
- 22. Azzopardi T, Ehrendorfer S, Coulton T, Abela M. Unstable extra-articular fractures of the distal radius: a prospective, randomised study of immobilization in a cast versus supplementary percutaneous pinning. J Bone Joint Surg Br. 2005;87(6):837–840 [DOI] [PubMed] [Google Scholar]
- 23. Roumen RM, Hesp WL, Bruggink ED. Unstable Colles’ fractures in elderly patients. A randomised trial of external fixation for redisplacement. J Bone Joint Surg Br. 1991;73(2):307–311 [DOI] [PubMed] [Google Scholar]
- 24. Aktekin CN, Altay M, Gursoy Z, Aktekin LA, Ozturk AM, Tabak AY. Comparison between external fixation and cast treatment in the management of distal radius fractures in patients aged 65 years and older. J Hand Surg Am. 2010;35(5):736–742 [DOI] [PubMed] [Google Scholar]
- 25. Wolfe SW, Austin G, Lorenze M, Swigart CR, Panjabi MM. A biomechanical comparison of different wrist external fixators with and without K-wire augmentation. J Hand Surg Am. 1999;24(3):516–524 [DOI] [PubMed] [Google Scholar]
- 26. Carter PR, Frederick HA, Laseter GF. Open reduction and internal fixation of unstable distal radius fractures with a low-profile plate: a multicenter study of 73 fractures. J Hand Surg Am. 1998;23(2):300–307 [DOI] [PubMed] [Google Scholar]
- 27. Campbell DA. Open reduction and internal fixation of intra articular and unstable fractures of the distal radius using the AO distal radius plate. J Hand Surg Br. 2000;25(6):528–534 [DOI] [PubMed] [Google Scholar]
- 28. Hove LM, Nilsen PT, Furnes O, Oulie HE, Solheim E, Molster AO. Open reduction and internal fixation of displaced intraarticular fractures of the distal radius. 31 patients followed for 3-7 years. Acta Orthop Scand. 1997;68(1):59–63 [DOI] [PubMed] [Google Scholar]
- 29. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29(1):96–102 [DOI] [PubMed] [Google Scholar]
- 30. Leung F, Zhu L, Ho H, Lu WW, Chow SP. Palmar plate fixation of AO type C2 fracture of distal radius using a locking compression plate--a biomechanical study in a cadaveric model. J Hand Surg Br. 2003;28(3):263–266 [DOI] [PubMed] [Google Scholar]
- 31. Jupiter JB, Ring D, Weitzel PP. Surgical treatment of redisplaced fractures of the distal radius in patients older than 60 years. J Hand Surg Am. 2002;27(4):714–723 [DOI] [PubMed] [Google Scholar]
- 32. Arora R, Lutz M, Fritz D, Zimmermann R, Oberladstatter J, Gabl M. Palmar locking plate for treatment of unstable dorsal dislocated distal radius fractures. Arch Orthop Trauma Surg. 2005;125(6):399–404 [DOI] [PubMed] [Google Scholar]
- 33. Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92(9):1851–1857 [DOI] [PubMed] [Google Scholar]
- 34. Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21(5):316–322 [DOI] [PubMed] [Google Scholar]
- 35. Voigt C, Lill H. [What advantages does volar plate fixation have over K-wire fixation for distal radius extension fractures in the elderly?]. Unfallchirurg. 2006;109(10):845–854 [DOI] [PubMed] [Google Scholar]
- 36. Handoll HH, Madhok R. Withdrawn: surgical interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2009;3:1–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Warwick D, Field J, Prothero D, Gibson A, Bannister GC. Function ten years after Colles’ fracture. Clin Orthop Relat Res. 1993;295:270–274 [PubMed] [Google Scholar]
- 38. Anzarut A, Johnson JA, Rowe BH, Lambert RG, Blitz S, Majumdar SR. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg Am. 2004;29(6):1121–1127 [DOI] [PubMed] [Google Scholar]
- 39. Arora R, Gabl M, Gschwentner M, Deml C, Krappinger D, Lutz M. A comparative study of clinical and radiologic outcomes of unstable colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009;23(4):237–242 [DOI] [PubMed] [Google Scholar]