Abstract
Proximal humeral fractures are frequently encountered in the elderly population. While the majority of these fractures can be managed nonoperatively, 2-, 3-, and 4-part fractures, head splitting, and complex fracture dislocations typically require operative management. Open reduction and internal fixation (ORIF) is a popular treatment option for displaced fractures. Advent of locking plates potentially imparts a better option for patients with osteoporotic bone. Hemiarthroplasty has traditionally been used in proximal humeral fractures not amendable to ORIF. While typically providing good pain control, results of hemiarthroplasty have demonstrated inconsistent shoulder motion. Tuberosity malposition or poor healing is a major culprit in unsatisfactory postoperative range of motion. Reverse shoulder arthroplasty has been used in the setting of rotator cuff arthropathy with successful results. Reverse shoulder arthroplasty has recently been used in the setting of acute proximal humeral fractures of the elderly individuals. This technology has shown promising results with mean active anterior elevation from 97° to 122° reported with complication rates of 15% to 28% in short-term studies. Long-term studies and higher level evidence studies with comparison to hemiarthroplasty and ORIF are needed.
Keywords: upper extremity surgery, trauma surgery, physical therapy, geriatric trauma, fragility fractures
Introduction
Proximal humeral fractures are the second most common fracture of the upper extremity, represent 10% of all fractures in those older than 65 years and are increasing in frequency as the elderly population grows.1–3 In light of these facts, it is not surprising that these fractures are very commonly encountered by orthopedic surgeons serving a geriatric population. Proximal humeral fractures are typically classified by the Neer Classification which is based on the 4-part anatomy of the proximal humerus. The anatomical components are the humeral head, greater tuberosity, lesser tuberosity, and proximal humeral shaft. A “part” is considered significant in the setting of either displacement >1 cm or angulation >45° of the individual components.4,5 Approximately 80% of proximal humeral fractures are nondisplaced or minimally displaced and can be conservatively treated successfully.6 The remaining fractures are typically 2-, 3-, and 4-part fractures, head splitting, and complex fracture dislocations. These fractures impart the greatest articular disruption and may produce higher risk of disruption of the proximal humeral blood supply.6,7 Nonoperative treatment of these fractures resulted in poor outcomes with complications including nonunion, disabling malunion, humeral head resorption, and osteonecrosis.5,8 Open reduction and internal fixation (ORIF) of proximal humerus fractures is the treatment of choice in fracture patterns amendable to fixation.9–15 Hemiarthroplasty is an option for the geriatric complex proximal humerus fracture that is not amendable to ORIF. This treatment provides for good pain relief but functional limitations persist.16,17 A review of shoulder hemiarthroplasty in the elderly individuals by Anjum et al found that 80% of their patients had no or minimal pain but had median active forward flexion of 65°, median active abduction of 60°, internal rotation to the lumbosacral junction and median external rotation was 10°, and a mean constant score16 of 47.5. Tanner et al reported similar pain relief with higher but still limited range of motion.17 Tuberosity malposition and nonunion after hemiarthroplasty have been identified as a significant risk of superior migration of the prosthesis, stiffness or weakness, unsatisfactory results, and persistent pain by Boileau et al.18 Significant risk factors for final tuberosity malposition were poor initial position of the prosthesis or greater tuberosity and women over the age of 75 years to which they attributed the presence of osteopenic bone.18 The postoperative rehabilitation for shoulder hemiarthroplasty typically is quite extensive and lengthy with elements of passive and active joint movements, muscular strengthening and stretching, hydrotherapy, physiotherapy, and occupational therapy. With emphasis on avoiding tuberosity displacement, the slowed rehabilitation also places prolonged significant functional limitations on the patient while some geriatric patients may not have the abilities to satisfactorily complete the desired rehab protocol. In light of the risk of tuberosity malunion and nonunion with its subsequent poor range of motion and unsatisfactory functional outcomes coupled with the necessity of a long and intense postoperative rehabilitation, one can appreciate the great challenge the orthopedist faces when treating geriatric proximal humeral fractures especially in the setting of osteoporosis, significant comorbidities, and cognitive or functional deficits. Reverse shoulder arthroplasty (RSA) may address some of these difficulties in fractures precluding ORIF through a decreased need for postoperative rehabilitation and with design aspects that decrease the importance of the rotator cuff on forward elevation.
History of RSA
Early in shoulder arthroplasty development, Neer recognized the challenge of the rotator deficient shoulder, and in the 1970s, his work centered on increasing conformity and constraint for this situation. In 1974, he gave up on his efforts in constrained prosthesis and concluded that they could not account for rotator cuff repair. Throughout the 1970s, attempts at RSA with prosthesis with more anatomical rotation were produced with disappointing results. In 1985, Grammont would revolutionize the development of RSA with the medialization and lowering of the center of rotation and the subsequent design of the Delta III prosthesis. This prosthesis has been used extensively in Europe with long-term follow-up data for rotator arthropathy available.19 Modern RSA devices by Depuy (Warsaw, Indiana) and Tornier (Edina, Minnesota) were approved for use in the United States in 2003 and 2004, respectively. Reverse shoulder arthroplasty was first used in the setting of end-stage glenohumeral arthritis with rotator cuff insufficiency with encouraging results.20 Levy et al reported promising results in the use of RSA with or without proximal humeral allograft in failed mal- and nonunions of proximal humeral fractures.21 The results of these studies prompted the use of RSA in the setting of the acute proximal humeral fracture.
Reverse Shoulder Arthroplasty Design
In RSA, the humerus is changed into a concave socket while the glenoid becomes the convex articulating surface. This configuration imparts a fixed center of rotation and is constrained in nature, while increasing the length of the deltoid. Reverse shoulder arthroplasty also increases the moment arm of the deltoid by medializing the center of rotation and by shifting the deltoid insertion site distally. These changes decrease the importance of the rotator cuff in elevation and provide a mechanical advantage for the deltoid muscle and its elevating capabilities.22 Reverse shoulder arthroplasty by design has innate limitations of external rotation.
Reverse Shoulder Arthroplasty for Acute Proximal Humeral Fractures
Outcomes
There are currently 4 studies detailing the use of RSA in acute proximal humeral fractures with mean follow-up from 22 months to 6.6 years. The inciting fracture in all 4 studies were displaced 3- and 4-part fractures with a mean patient age from 74 to 78 years.23–26 The operation was within 15 days of the injury in the Bufquin series and performed at an average of 10 days by Klein et al.23,24 The mean active motion and constant scores are listed in Table 1. Mean disability of the arm, shoulder, and hand (DASH) scores from the contralateral limb are available from Cazenueve and Cristofari and Bufquin et al and reveal operative limb mean DASH scores of 67% and 64%, respectively, when compared to the contralateral limb.23,25 Sirveaux et al compared 15 RSA cases findings with a hemiarthroplasty group in the setting of acute proximal humeral fractures and found that while the mean active anterior elevation was similar between the 2, only 7% of RSA failed to achieve >90° of elevation, whereas 50% of hemiarthroplasty patients did not.26
Table 1.
Results of Reverse Shoulder Arthroplasty for Acute Proximal Humeral Fractures
| Study | Active forward elevation | Active abduction | Active external rotation | Mean constant score | Complication rate |
|---|---|---|---|---|---|
| Cazeneuve and Cristofari | 53 | 19% | |||
| Bufquin et al | 97° | 30° | 44 | 28% | |
| Klein et al | 122° | 112° | 25° | 68 | 15% |
| Sirveaux et al | 107° | 10° | 55 |
Complications
The overall complication rates were 15% to 28% and are listed in Table 1.23–26 Complications occurred in 12 of 43 patients in the Bufquin et al series and included an intra-operative glenoid fracture, neurologic injury with resultant parasthesias in 2 patients, 3 cases of reflex sympathetic dystrophy (RSD) which all resolved, a nontraumatic anterior dislocation, and 1 surgical wound complication.23 Klein et al reported dislocation in 1 patient, and 2 early infections successfully treated with 4 irrigation and debridements and antibiotics without implant removal.24 Cazeneuve and Cristofari reported complications included 2 cases of RSD that resolved, 1 early infection successfully treated by irrigation and debridement, and 4 cases of dislocation. An anterior dislocation was attributed to anteversion of the humeral component, and the 3 superior dislocations were thought to be secondary to impingement on the remnants of the tuberosities, thus all dislocations were attributed to surgical technique.25
Scapular Notching
Scapular notching as evidenced by plain radiographs, carries with it much controversy with unknown long-term clinical implications. Lévigne et al found a 62% prevalence of scapular notching in 326 patients with RSA treated for a variety of indications with a mean follow-up of 47 months. In their findings, the notching was progressive but did not affect shoulder range or motion or constant score.27 Sirveaux et al, however, found that scapular notching had negative effect on outcome with a significant negative influence of grades 3 and 4 notching on the constant score.28 Cazeneuve and Cristofari found evidence of scapular notching in 19 of 36 patients at an average follow-up of 6.6 years which was an increase from 14 of 36 in an earlier publication. The notching was broken down into mechanical (10), as caused by the impingement between the humeral component and the inferior scapular pillar and were stable with regard to bone loss, and biological (9) which was attributed to polyethylene wear and were noted to be progressive in their bone loss.25 Sapular notching was present in 25% of patients in the Bufquin et al series with notching reaching the inferior screw in 1 patient.23 Klein et al reported notching in 1 of 20 patients with a classification of Nerot grade I.24
Malunion
In the Bufquin series, secondary displacement of the tuberosities occurred in 53% of patients leading to a 13.8% malunion rate and a 38.8% nonunion rate. This had only moderate and insignificant effects on the constant score and on external rotation.23 Cazeneuve and Cristofari excised the remnants of the tuberosities in their series.25 Sirveaux found that in their comparison of RSA and hemiarthroplasty in acute proximal humeral fractures that in cases of malunion or nonunion of the greater tuberosity, the active anterior elevation was 75° in the hemiarthroplasty group and 116° in the RSA group. This difference helps explain the significant percent of patients in the hemiarthroplasty group with ≤90° of elevation. The mean constant score in the setting of greater tuberosity mal- or nonunion was 55 points in patients with RSA and 41 in hemiarthroplasty. These results stress the importance of greater tuberosity positioning and healing in shoulder hemiarthroplasty.26
Loosening
Cazeneuve and Cristofari reported 1 case of aseptic loosening of the baseplate at 12 years.25 Klein et al and Bufquin et al found no evidence of baseplate or stem loosening at mean follow-ups of 33 and 22 months, respectively.23,24
Discussion
A benefit of RSA in proximal humeral fractures is the decreased immobilization and rehabilitation necessary for successful outcomes as compared to shoulder hemiarthroplasty. This is especially important in the geriatric patient in which physiologic or mental limitations may thwart successful rehabilitation. Reverse shoulder arthroplasty is a complex procedure and Rockwood recommends that extensive shoulder arthroplasty experience coupled with thorough knowledge of the implant used is necessary to minimize serious complications.29 Salvage of a failed RSA is a challenging problem with conversion to a hemiarthroplasty with allograft supplementation as an option. Cazeneuve and Cristofari noted progressive notching and a decrease in constant score in their series with a mean follow-up of 6.6 years.25 Walch and colleagues found significant levels of component loosening and functional deterioration in a study of RSA for multiple etiologies with a minimum follow-up of 60 months leading them to recommend the use of RSA in patients over 70 years.30 The senior author will offer RSA in the setting of acute proximal humeral fracture only in patients over the age of 70 with fractures not amendable to ORIF after a discussion of the risks and benefits of RSA and hemiarthroplasty. An example case is illustrated in Figures 1 to 5. Future studies regarding the long-term results as well as higher level of evidence studies comparing RSA to ORIF and hemiarthroplasty for acute proximal humeral fractures are needed.
Figure 1.
Anteroposterior and axillary lateral radiographs of right shoulder of an 86-year-old male patient. The patient lives alone and is independent with the activities of daily living.
Figure 5.
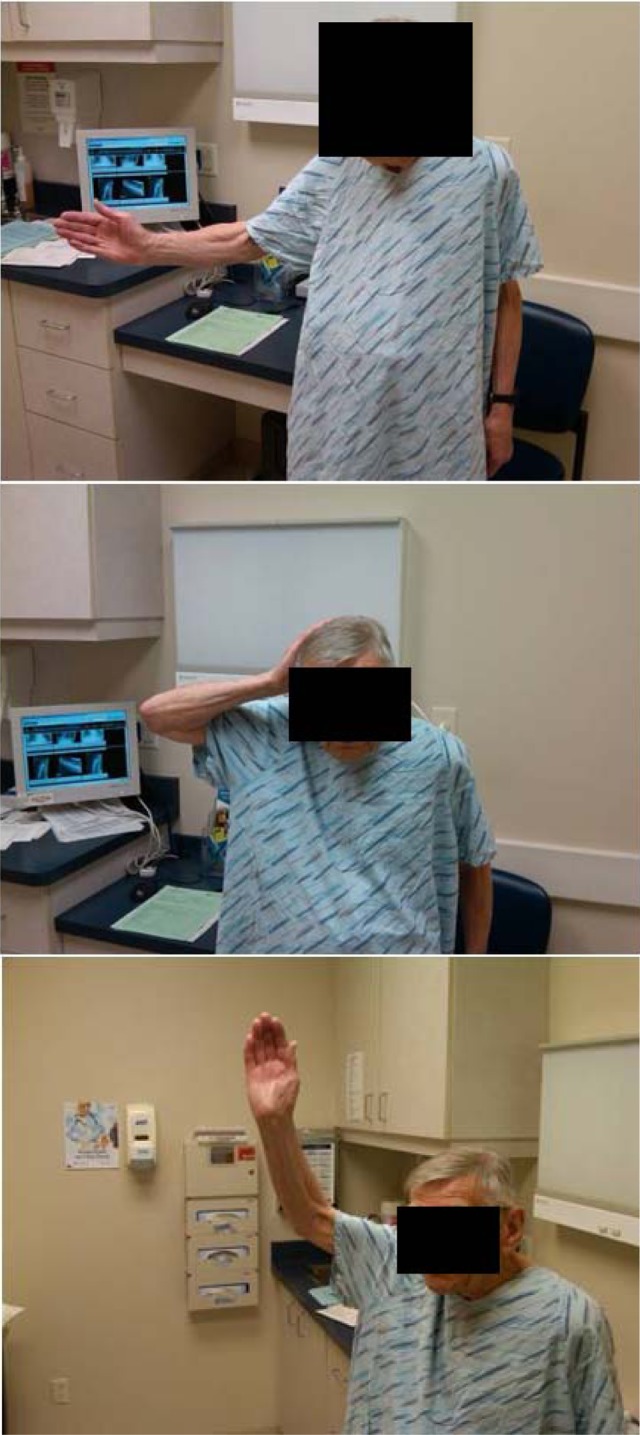
Clinical active range of motion 1 year after reverse shoulder arthroplasty in the patient from Figures 1 to 4
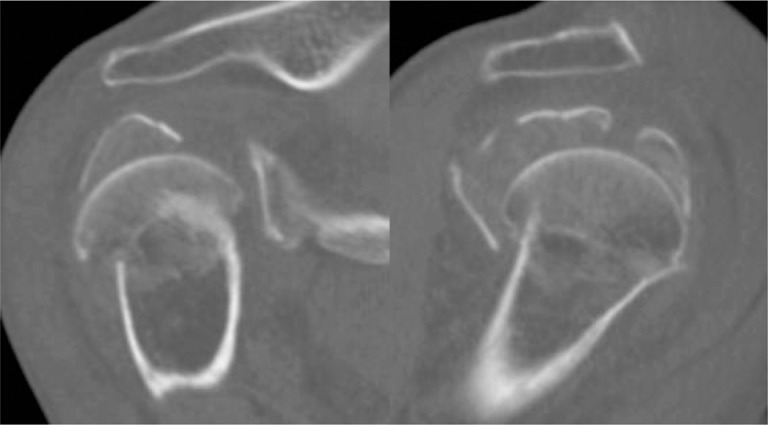
Figure 2.
Computed tomography scan of the right shoulder of the patient from Figure 1 reveals a comminuted head splitting proximal humeral fracture.
Figure 3.

Three-dimensional reconstruction of computed tomography scan from Figure 2.
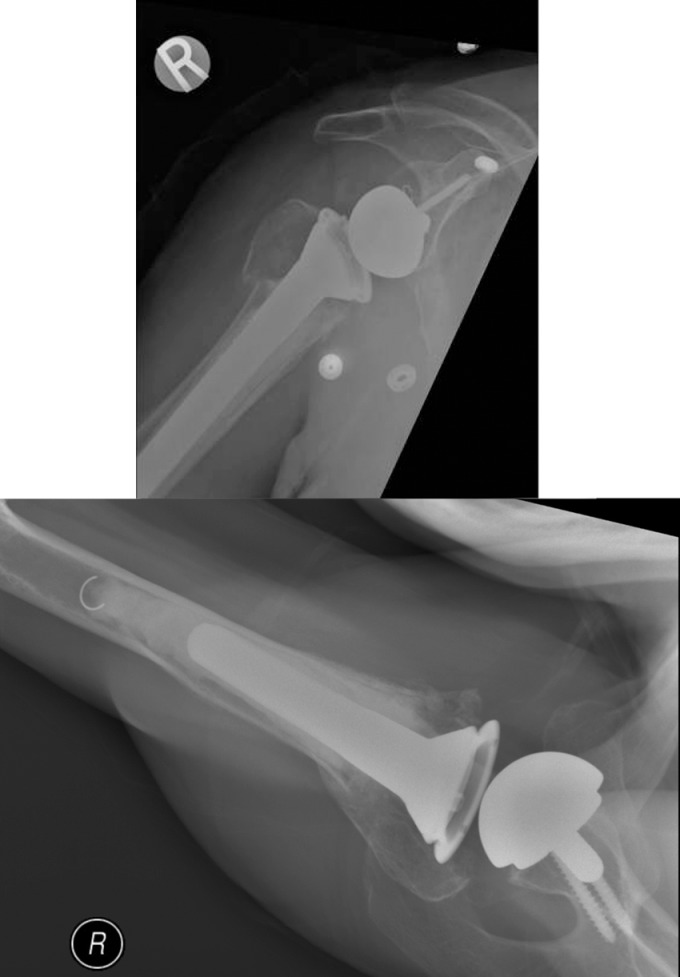
Figure 4.
Because of the head splitting nature of the fracture seen in Figures 1 to 3 and the high risk of osteonecrosis the patient underwent reverse shoulder arthroplasty. The tuberosities were fixed with nonabsorbable suture. Six-month postoperative radiographs.
Conclusion
Open reduction and internal fixation is the preferred method in the treatment of displaced proximal humeral fractures. In patients over the age of 70 with fractures precluding internal fixation, after the discussion of the benefits and risks versus hemiarthroplasty, the option for RSA is reasonable.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Baron JA, Barrett JA, Karagas MR. The epidemiology of peripheral fractures. Bone. 1996;18(3 suppl):209S–213S [DOI] [PubMed] [Google Scholar]
- 2. Hodgson S. Proximal humerus fracture réhabilitation. Clin Orthop Relat Res. 2006;442:131–138 [PubMed] [Google Scholar]
- 3. Baron JA, Karagas M, Barret J, et al. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7(6):612–618 [DOI] [PubMed] [Google Scholar]
- 4. Neer CS 2nd. Displaced proximal humeral fractures: part I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–1089 [PubMed] [Google Scholar]
- 5. Neer CS 2nd. Displaced proximal humeral fractures: part II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970;52(6):1090–1103 [PubMed] [Google Scholar]
- 6. Gerber C, Schneeberger AG, Vinh TS. The arterial vascularization of the humeral head: an anatomical study. J Bone Joint Surg Am. 1990;72(10):1486–1494 [PubMed] [Google Scholar]
- 7. Naranja RJ, Iannotti JP. Displaced three- and four-part proximal humerus fractures: evaluation and management. J Am Acad Orthop Surg. 2000;8(6):373–382 [DOI] [PubMed] [Google Scholar]
- 8. Stableforth PG. Four-part fractures of the neck of the humerus. J Bone Joint Surg Br. 1984;66(1):104–108 [DOI] [PubMed] [Google Scholar]
- 9. Esser RD. Treatment of three- and four-[art fractures of the proximal humerus with a modified cloverleaf plate. J Orthop Trauma. 1994;8(1):15–22 [DOI] [PubMed] [Google Scholar]
- 10. Savoie FH, Geissler WB, Vander Griend RA. Open reduction and internal fixation of three-part fractures of the proximal humerus. Orthopedics. 1989;12(1):65–70 [DOI] [PubMed] [Google Scholar]
- 11. Owsley K, Gorcyzka J. Displacement/screw cutout after open reduction and locked plate fixation of humeral fractures. J Bone Joint Surg Am. 2008;90(2):233–240 [DOI] [PubMed] [Google Scholar]
- 12. Kettler M, Biberthaler P, Braunstein V, Zeiler C, Kroetz M, Mutschler W. Treatment of proximal humeral fractures with the PHILOS angular stable plate: presentation of 225 cases of dislocated fractures. Unfallchirurg. 2006;109(12):1032–1040 [DOI] [PubMed] [Google Scholar]
- 13. Sudkamp N, Bayer J, Hepp P, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate: Results of a prostpective, multicenter, observational study. J Bone Joint Surg Am. 2009;91(6):1320–1328 [DOI] [PubMed] [Google Scholar]
- 14. Solberg B, Moon C, Franco D, Paiement GD. Locked Plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009;23(2):113–119 [DOI] [PubMed] [Google Scholar]
- 15. Felix B, Sommer C, Bahrs C, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009;23(3):163–172 [DOI] [PubMed] [Google Scholar]
- 16. Anjum SN, Butt MS. Treatment of comminuted proximal humerus fractures with shoulder hemiarthroplasty in elderly patients. Acta Orthop Belg. 2005;71(4):388–395 [PubMed] [Google Scholar]
- 17. Tanner MW, Cofield RH. Prosthetic arthroplasty for fractures and fracture dislocations of the proximal humerus. Clin Orthop. 1983;179:116–128 [PubMed] [Google Scholar]
- 18. Boileau P, Krishnan SG, Tinsi L, et al. Tuberostiy malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2002;11(5):401–412 [DOI] [PubMed] [Google Scholar]
- 19. Katz D, O’Toole G, Cogswell L, Sauzieres P, Valenti P. A history of the reverse shoulder prosthesis. Int J Shoulder Surg. 2007;1:108–113 [DOI] [PubMed] [Google Scholar]
- 20. Frankle M, Siegal S, Pupello D, Sallem A. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005;87(8):1697–1705 [DOI] [PubMed] [Google Scholar]
- 21. Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am. 2007;89(2):292–300 [DOI] [PubMed] [Google Scholar]
- 22. Martin TG, Iannotti JP. Reverse total shoulder arthroplasty for acute fractures and failed management after proximal humeral fractures. Orthop Clin North Am. 2008;39(4):451–457 [DOI] [PubMed] [Google Scholar]
- 23. Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly. J Bone Joint Surg (Br). 2007;89(4):B516–B520 [DOI] [PubMed] [Google Scholar]
- 24. Klein M, Juschka M, Hinkenjann B, Scherger B, Ostermann PAW. Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma. 2008;22(10):698–704 [DOI] [PubMed] [Google Scholar]
- 25. Cazeneuve JF, Cristofari DJ. The reverse shoulder prosthesis in the treatment of fractures of the proximal humerus in the elderly. J Bone Joint Surg (Br). 2010;92(4):535–539 [DOI] [PubMed] [Google Scholar]
- 26. Sirveaux F, Navez GN, Favard L, et al. Reverse prosthesis for acute proximal humerus fracture, the multicentric study. In: Walch G, Goileau P, Mole D, et al., eds. Reverse Shoulder Arthroplasty, Clinical Results-Complications-Revision. Montpellier, France: Sauramps Medical;2006:73–80 [Google Scholar]
- 27. Lévigne C, Boileau P, Favard L, et al. Scapular notching in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2008;17(6):925–935 [DOI] [PubMed] [Google Scholar]
- 28. Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86(3):388–395 [DOI] [PubMed] [Google Scholar]
- 29. Rockwood CA. The reverse total shoulder prosthesis: the new kid on the block. J Bone Joint Surg Am. 2007;89(2):292–300 [DOI] [PubMed] [Google Scholar]
- 30. Guerry J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty: survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742–1747 [DOI] [PubMed] [Google Scholar]