SUMMARY
Cyclothymic disorder is a chronic and impairing subtype of bipolar disorder, largely neglected in pediatric research. Consequently, it is rarely diagnosed clinically despite potentially being the most prevalent form of bipolar disorder. Lack of attention has added to confusion about the diagnosis and clinical presentation of cyclothymic disorder. In pediatric studies, cyclothymic disorder is commonly grouped with ‘subthreshold’ presentations of bipolar disorder under the undifferentiated label ‘bipolar disorder not otherwise specified’. However, research indicates that cyclothymic disorder can be reliably distinguished from the other forms of bipolar disorder and from other childhood disorders. Importantly, cyclothymic disorder may be a diathesis for more acute presentations of bipolar disorder, warranting a prominent role in dimensional models of mood and psychopathology. Current evidence suggests that cyclothymic disorder has the potential to make unique contributions to our understanding of the risk factors and outcomes associated with bipolar disorder. This potential has yet to be fully realized, limiting our knowledge and ability to intervene in a meaningful way with youth who are exhibiting symptoms of a major mood disorder. Including cyclothymic disorder in future research studies of children – particularly longitudinal outcome studies – is essential for understanding the developmental trajectory of bipolar spectrum disorders and learning how to accurately diagnosis and treat the full spectrum of bipolar disorders.
Cyclothymia has been part of the nomenclature in psychiatry since the 1880s, and during the time since then, has been conceptualized in a number of different ways across several theoretical models. Currently, some think of cyclothymic disorder as a subtype of bipolar disorder [1], characterized by a chronic presentation of low-grade depressive and hypomanic symptoms. Cyclothymia is also described as a temperament style [2], associated with moodiness and irritability. Cyclothymic temperament is thought to be a risk factor for psychopathology, particularly in the bipolar spectrum disorders [3]. The concept of ‘temperament as diathesis’ aligns well with the conceptualization of cyclothymic disorder as a prodrome or intermediate stage in the development of bipolar I or II [4]. Cyclothymia has also been considered a character trait that might not have any direct relation to psychopathology [5]. This range of definitions, applied to a single term, has led to confusion, misinterpretation and, ultimately, limited attention. As a dimensional model of diagnosis gains favor, cyclothymic disorder may become an increasingly important developmental construct between nonclinical levels of mood fluctuation and acute bipolar disorder. Pediatric bipolar disorder continues to be controversial, with questions regarding its phenomenology and course remaining unresolved. Cyclothymic disorder may be an important key to understanding the progression from ‘childhood moodiness’ into a mood disorder. The anticipated publication of new versions of both the DSM and International Classification of Diseases provides an opportunity to examine the data on cyclothymic disorder in youth and to decide how it best fits in with contemporary psychiatry and psychology.
Available data on cyclothymic disorder in youth are limited. To date there are fewer than five clinical studies published that have included it as a diagnostic category and it is not specifically included in epidemiological studies. The lack of published information about cyclothymic disorder is not related to its prevalence or degree of associated impairment. The goal of this review is to bring attention to the data available on cyclothymic disorder and to highlight areas in need of future research. A comprehensive review of the extant literature was performed through PubMed and PsycInfo using the following search terms: cyclothymia, cyclothymic disorder, subthreshold bipolar disorder, youth, pediatric and pediatric bipolar disorder.
Epidemiology
Cyclothymic disorder, characterized by chronic mood instability – duration of at least 1 year in children – is a debilitating, but rarely recognized disorder [6]. Although there is evidence that cyclothymic disorder may be the most prevalent subtype of bipolar disorder in both youth and adults [7–9], it is rarely diagnosed in children and is largely ignored in research studies as most groups focus solely on the broad ‘bipolar not otherwise specified category’ (BP NOS) [10,11]. A recent meta-analysis of all the epidemiological studies of pediatric psychiatric illness found that no component studies included cyclothymic disorder as a distinct category. However, presentations of bipolar disorder that did not meet criteria for bipolar I or II – but could be consistent with cyclothymic disorder – were the most prevalent in young people [12]. These data are consistent with epidemiological studies in adults, which also show that presentations of bipolar symptomatology that do not meet full criteria for bipolar I or II are the most prevalent [13–15]. It can be inferred from these findings that cyclothymic disorder is real and that it may persist into adulthood. However, the lack of delineation of bipolar sutbtypes in pediatric epidemiological studies limits our knowledge of cyclothymic disorder.
Assessment & diagnosis
The dearth of research on pediatric cyclothymic disorder compromises the field’s ability to appropriately diagnose and treat youth with mood disorders. Because cyclothymic disorder is not often included in research studies, it is likely that the diagnostic groups that are used instead – primarily BP NOS – include youth with cyclothymic disorder. This ‘contamination’ of the diagnostic subgroup interferes with attempts to learn about the etiology, course and optimal treatment for each of the bipolar subtypes.
The criteria for cyclothymic disorder are formally defined [1], whereas those for BP NOS are intentionally vague, in order to capture presentations of bipolar disorder that fall outside the DSM-defined subtypes. To meet criteria for the diagnosis of cyclothymic disorder, a youth must have experienced 1 year for the duration of which they had hypomanic and depressive symptoms without ever meeting the criteria for mania or major depression. By contrast, a diagnosis of BP NOS is made when a person experiences symptoms of hypomania and/or depression that do not meet criteria for mania or major depression. Relying on the catchall diagnosis of BP NOS over a diagnosis of cyclothymic disorder is understandable. The criteria for cyclothymic disorder raise challenges for clinicians. Specifically, the chronic nature of cyclothymic disorder can be hard to differentiate from temperamental differences in young people. The diagnosis of any mood disorder requires a discrete episode with cyclothymic disorder requiring a year-long episode, so details about the timing of symptoms matter, but this does not mean that the clinician will have access to reliable information. Retrospective reporting is notoriously fallible [16] and, when inquiring about symptoms over the past year, it can be hard for the parent of a 7-year-old child to delineate a year-long episode from ‘always’. Additionally, it can be hard to tell whether symptoms of hypomania – irritability, elated mood and increased energy – are pathological, or simply the signs of an active child. In such cases, another diagnosis – ADHD in the case of predominantly elevated mood or depression in the case of low mood – may seem more appropriate.
Further complicating diagnosis, diagnostic criteria for cyclothymic disorder overlap with other disorders. In older adolescents and young adults, symptoms of cyclothymic disorder may be confused with borderline personality disorder [17,18] or atypical depression [19,20]. These disorders all include significant mood instability and irritability and, in some cases, may share an underlying cyclothymic temperament, making differential diagnosis challenging. In youth, ADHD and depression, may both share characteristics with cyclothymic disorder, including irritability, restlessness, moodiness and distractibility [1]. Both ADHD and depression are more common than cyclothymic disorder [21,22]; consequently, clinicians are more likely to have experience diagnosing and treating youth with depression and/or ADHD.
Comorbid ADHD, which is common among children with bipolar disorder [23–27], further clouds the diagnostic picture. In the typical clinic, with a focus on present symptomatology and a desire to provide both children and parents with relief, a diagnosis of cyclothymic disorder is not likely to be the most obvious choice, even if it is the most accurate.
Validation studies
Importantly, the diagnosis of cyclothymic disorder can be made reliably in youth. Two validation studies on cyclothymic disorder in youth, using the criteria set out by Robins and Guze [28], found that it can be reliably differentiated from other nonbipolar childhood disorders, and that cyclothymic disorder falls on the bipolar spectrum based on multiple criteria [29–31]. The first study, Improving the Assessment of Juvenile Bipolar Disorder, included 827 youth, 52 of whom had a diagnosis of cyclothymic disorder (NIH R01MH066647) [29]. The second study, using data collected under the auspices of a grant from the Stanley Medical Research Institute (to RL Findling), provided a replication and extension of the first, and included 894 youth, among whom 53 were cyclothymic disorder cases [31]. Youth meeting DSM criteria for cyclothymic disorder were compared on a variety of constructs with other youth with bipolar spectrum disorders (bipolar I and II, and BP NOS), and to youth with nonbipolar spectrum disorders.
In both samples, youth with cyclothymic disorder experienced significantly higher levels of irritability than nonbipolar youth – across both low and hypomanic mood states. Importantly, youth with cyclothymic disorder also exhibited high levels of sleep disturbance – significantly higher than nonbipolar cases. A decreased need for sleep is a hallmark symptom of bipolar disorder and is often one of the best ways by which to differentiate cyclothymic disorder, or other bipolar disorder subtypes, from nonbipolar childhood disorders [32,33]. Youth with cyclothymic disorder also reported an early age of symptom onset. Three-quarters had symptom onset before they were aged 10 years, and the average age of onset for youth with cyclothymic disorder was 6 years. In the Improving the Assessment of Juvenile Bipolar Disorder sample, youth with cyclothymic disorder had symptom onset significantly earlier than youth with bipolar II or depression, suggesting that cyclothymic presentation might be a way of identifying those at risk of developing more acute mood episodes prospectively.
Cyclothymic disorder was also associated with high comorbidity. Nearly all youth with cyclothymic disorder, in both samples, had at least one comorbid axis I disorder, most commonly ADHD. Related youth with cyclothymic disorder had high rates of psychiatric illness among their family members: 100% of youth from the Stanley sample and 94% of youth from the Improving the Assessment of Juvenile Bipolar Disorder sample had at least one family member with a psychiatric illness, and most had a family member with bipolar disorder. High comorbidity rates, along with the variability in heritable risk factors, could provide some insight into the shared mechanisms across disorders, including bipolar disorder, depression, ADHD, anxiety and borderline personality disorder. Across all the constructs of interest – irritability, sleep disturbances, age of symptom onset, comorbid diagnoses and family history – the two validation studies told a consistent story: cyclothymic disorder occurs in young people, it can be reliably diagnosed and it shares more in common with the other bipolar spectrum disorders than it does with the nonbipolar spectrum disorders.
Genetics & temperament
Family studies and genome investigations offer another compelling piece of evidence that cyclothymic disorder belongs on the bipolar spectrum [8,34–37]. The rates of familial bipolar I are similar among people with cyclothymic disorder and those with bipolar I [38,39]. Interestingly, this shared diathesis may manifest initially as cyclothymic temperament [40,41]. Both people with bipolar disorder and their relatives tend to have higher rates of cyclothymic temperament than healthy controls [42,43]. In children with depression, cyclothymic temperament has been associated with a higher risk of bipolar disorder and may be helpful in the prediction of future bipolarity among youth presenting with depressed mood [44]. This could be particularly important because the treatment guidelines for unipolar depression and bipolar depression are not the same [45,46]. Given the aforementioned challenges of diagnosing cyclothymic disorder in youth, assessing for both cyclothymic temperament and a family history of bipolar disorder can offer valuable diagnostic information as part of a thorough evaluation.
Course
Cyclothymic disorder may begin earlier than other childhood disorders, perhaps owing to its relation with temperament [44]. Early-onset bipolar disorder is thought to have a greater genetic contribution than presentations of bipolar disorder that begin in late adolescence or early adulthood [47]. In a study of young people whose parents had bipolar disorder, almost a quarter of the offspring met criteria for cyclothymic disorder [36]. Additionally, in a study of subsyndromal mania, youth who had at least one parent with a bipolar spectrum disorder were more likely to exhibit bipolar symptoms, including irritability and mood lability, than those youth whose parents did not have bipolar disorder [48]. Early-onset bipolar disorder is associated with a more difficult course, including delayed diagnosis, treatment-resistant symptoms, more frequent episodes and longer episodes [49,50], consistent with the characteristics of cyclothymic disorder.
Although we know relatively little about the specific course of cyclothymic disorder in youth because it has not been included in any longitudinal studies to date, adult studies suggest that it is just as impairing as other subtypes of bipolar disorder [15]. Pediatric studies indicate that symptom presentations consistent with cyclothymic disorder – chronic moodiness as well as symptoms of both hypomania and depression – are associated with as much impairment as bipolar I and II [10,51]. In our two validation studies, we found that youth with cyclothymic disorder had Children’s Global Assessment scores similar to those with other bipolar spectrum disorders, but significantly worse than youth with nonbipolar disorders [29–31]. Similarly, youth with bipolar spectrum disorders had a lower quality of life than youth with serious medical illness, including heart disease, oxygen dependency, arthritis, asthma, and obesity [52]. Although youth with cyclothymic disorder were not directly compared with the other subtypes of bipolar disorder by Freeman et al., other studies have found that the chronic nature of their symptoms results in fewer days of good quality of life than others with bipolar I or II, for whom periods of euthymic mood are more common [52].
Youth with cyclothymic disorder may experience factors contributing to poor quality of life more often than other youth. In analyses concentrating on a case series at a community mental health clinic, those with a diagnosis of cyclothymic disorder reported high rates of abuse. According to parent reports, 26% of children had a history of neglect, 26% had a history of sexual abuse and 20% had been physically abused. The rates of neglect and sexual abuse were significantly higher than those reported by the parents of other treatment-seeking youths with non-bipolar spectrum disorders [30]. Beyond this preliminary investigation, the relationship between abuse and cyclothymic disorder in youth has not been specifically explored. However, high rates are consistent with other research showing that abuse is more prevalent among youth with bipolar spectrum disorders than youth with other psychiatric disorders [53] and that abuse is associated with poor outcomes, including longer duration of illness, both axis I and axis II comorbid diagnoses and a family history of mood disorders [54–56].
Family history of psychiatric illness may contribute to high rates of abuse and neglect among youth with cyclothymic disorder. As mentioned, family history of mental illness appears ubiquitous with cyclothymic disorder [29,31]. This may also lead to less stable home environments: 18% of youth with cyclothymic disorder in the Improving the Assessment of Juvenile Bipolar Disorder sample had been placed out of home at least once. Youth with cyclothymic disorder also experienced a significant disruption to their education: 78% had changed schools at least once, 36% had an individualized education plan, 45% received special services at school and 72% were expelled from school at some point. School problems are linked with a number of negative outcomes, including mental illness, poor social support and incarceration [57]. Of the youth with cyclothymic disorder, 8% already had a history of involvement with juvenile court, despite the average age of these youths being 10 years.
Problems at school and involvement in the court system, in addition to other factors that may be associated with having a child with mental illness, such as doctors’ appointments and turmoil at home, take a toll on the family as well as the child [58]. In our sample, the primary caregiver reported missing an average of 31 h of work in the preceding month due to their child’s needs. Additionally, over a quarter of parents reported needing to seek psychological treatment themselves, due to the stress of caring for their child [30]. Other associated stressors, such as financial difficulties due to parents’ lost wages and the expense of treating a chronic illness, are likely to further stress the family system and worsen the course of the child’s illness.
Considering the accumulated risk factors, including school problems, parental mental illness, and abuse that youth with cyclothymic disorder often experience, suggests a deteriorating prognosis is suggested [59]. The outcome most feared by families and clinicians is suicide. Bipolar disorder increases the risk for suicide, with a completion rate as much as 20 times higher than among other suicide attempters [60,61]. In the Improving the Assessment of Juvenile Bipolar Disorder sample, 45% of youth reported having suicidal thoughts, significantly higher than youth with nonbipolar disorders. Additionally, 18% reported having engaged in nonsuicidal self injury, and 2% had made a potentially lethal suicide attempt. These findings are concerning, but taking into account the young age of these participants, and the fact that stressful life events of the type common among youth with cyclothymic disorder [62] and prior suicidality are among the best predictors of future suicide behavior [63–66], more attention to this group of youth is warranted. These results align with the adult literature, consistently showing that subthreshold forms of bipolar disorder are associated with significant suffering and should be a major public health concern [15,67,68].
Sparse data leave ambiguity about the longterm prognosis for cyclothymic disorder. Studies of young adults and adults, and child studies that lump BP NOS and cyclothymic disorder together, suggest that approximately a third of cyclothymic disorder causes progress to bipolar I or II [2,38,51,69]. Cyclothymic disorder has been conceptualized as a prodrome to bipolar I or II [70]. In a longitudinal study of adolescents, approximately half of the participants with cyclothymic disorder progressed to bipolar II disorder (had a major depressive episode), whereas none of the participants who were diagnosed with ‘subthreshold bipolar’ disorder at enrollment continued to meet criteria for bipolar disorder at follow-up [71]. This highlights the need to differentiate between cyclothymic disorder and other subthreshold cases. Similarly, more than half (n = 7) of those with cyclothymic disorder (n = 11) experienced an episode of mania or depression during the 3-year follow-up [72]. Additionally, Kochman et al. found that 64% of youth with major depression combined with cyclothymic temperament converted to bipolar disorder, versus only 15% of youth who did not meet criteria for cyclothymic temperament [44]. Cyclothymic temperament was also associated with an increased risk of suicidal ideation or attempt, with more than twice as many youth with cyclothymic temperament than without reporting suicidal ideation or attempts. Cyclothymic temperament, along with other factors that influence whether youth with cyclothymic disorder develop bipolar I or II, has important clinical implications and may help to inform treatment [35,73].
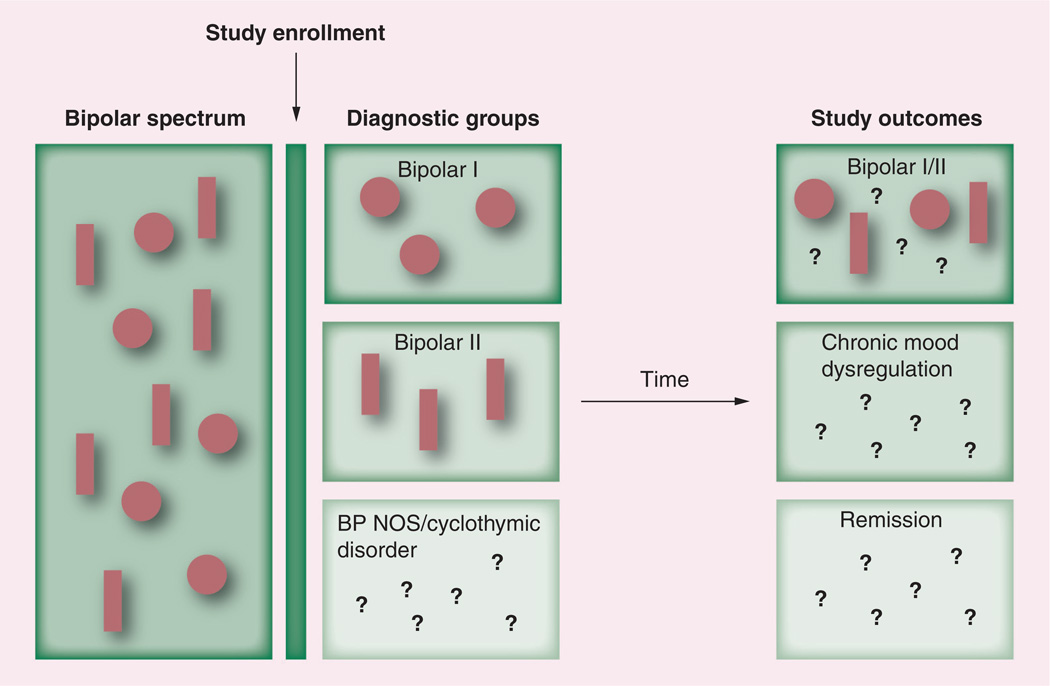
Intriguingly, there is also evidence for developmentally limited forms of bipolar disorder, suggesting that some people meeting criteria for bipolar disorder in childhood will experience permanent remission of their symptoms, beginning in young adulthood [74]. The ‘developmentally limited’ hypothesis may be one of the best arguments in favor of devoting more resources toward investigating pediatric bipolar subtypes. Although data indicate that a third of people with cyclothymic disorder develop bipolar I or II, the idea that subthreshold forms of the disorder may remit has not been systematically explored. Identification of factors moderating the progression of cyclothymic disorder would facilitate improved treatments and preventive interventions. Unfortunately, without greater precision in the diagnosis of bipolar spectrum disorders, the outcomes determined by the interaction of different phenotypes and the environment are obscure (Figure 1).
Figure 1.
Common research practice of combining ‘bipolar not otherwise specified’ and cyclothymic disorder, thereby obstructing the ability to identify factors affecting the course of illness and subsequent outcomes.
BP NOS: Bipolar not otherwise specified.
Treatment
Little evidence guides effective intervention for cyclothymic disorder. Subthreshold symptoms tend to persist longer than symptoms meeting full criteria [75,76] and, although the discrete periods of hypomania and depression may be shorter than those associated with bipolar I or II, the frequent fluctuation between mood states in cyclothymic disorder results in fewer well (euthymic) days [77]. Youth with bipolar I or II tend to achieve remission faster and enjoy extended periods relatively symptom free [51,78], whereas people with cyclothymic disorder are generally symptomatic indefinitely [35]. Additionally, the more chronic symptom presentation typical of cyclothymic disorder often indicates a treatmentrefractory form of the disorder [51,78] associated with greater comorbidity [37,79].
Research on psychosocial treatments for cyclothymic disorder is limited [80] and has not been explored in a youth sample. Most studies of psychosocial treatments exclude subthreshold cases. As a result, although there is growing evidence for the efficacy of psychosocial treatment combined with pharmacotherapy for the treatment of bipolar disorder, we do not know the extent to which psychotherapy would benefit youth with cyclothymic disorder [81,82]. There are two published studies that evaluate the use of cognitive behavioral therapy techniques to improve the symptoms of cyclothymic disorder in adults [83,84]. Both produced results suggesting that the prognosis and quality of life for people with cyclothymic disorder could be enhanced through augmented cognitive behavioral therapy. Future research should build upon these results and progress toward clear treatment guidelines for cyclothymic disorder, particularly in youth.
Psychopharmacological treatment
There are no randomized clinical trials focused on pharmacological treatment of cyclothymic disorder, and extant treatment guidelines do not differentiate between cyclothymic disorder and other bipolar disorders [85,86]. Studies that include youth with symptom presentations similar to the diagnostic profile of cyclothymic disorder indicate that the bipolar subtypes appear to respond to pharmaceutical treatment similarly [36,87]. Limited data from adult samples treating cyclothymic disorder with mood-stabilizing agents suggest potential positive responses to agents such as lithium, valproate and other anticonvulsants or antipsychotics [80,88]. Secondary analyses of the Improving the Assessment of Juvenile Bipolar Disorder study data found that 63% of youth with cyclothymic disorder were treated with a psychotropic medication, including stimulants, antidepressants, mood stabilizers, antipsychotics (both typical and atypical), anticonvulsants and lithium [30]. The lack of consistency regarding whether or not a child with cyclothymic disorder is treated with medication and, if so, which medication is used, highlights the large gap between the need for effective pharmaceutical interventions for cyclothymic disorder and the current evidence. Although lacking rigorous scientific investigation, data suggest that cyclothymic disorder responds to treatment as if it were on the bipolar spectrum, and prudent approaches to treatment should use similar algorithms but perhaps start with lower doses, titrating slowly.
Future directions
This review highlights that there are few data available specific to cyclothymic disorder in youth. The literature has focused on bipolar I disorder and, when subtypes are included in research projects, cyclothymic disorder is usually combined with cases that do not meet full diagnostic criteria under a broad ‘bipolar disorder not otherwise specified’ category. Some of these cases will continue to experience chronic mood dysregulation into adulthood. Others will have a manic episode or major depressive episode and subsequently meet criteria for bipolar I or II. However, some of these youth get better. Failing to carefully differentiate the youth within this category greatly limits understanding of factors that influence prognosis and intervention response.
The proposed addition of disruptive mood dysregulation disorder (DMDD) to the DSM-V [101] could potentially lead to confusion with regard to cyclothymic disorder. DMDD and its predecessors, severe mood dysregulation disorder and temper dysregulation disorder with dysphoria, are based on limited data and have significant symptom overlap with other childhood disorders [89]. Specifically, irritable mood with temper outbursts is the primary criterion for DMDD and irritable mood can be the primary symptom of mania seen in cyclothymic disorder. Furthermore, both diagnoses require a duration of 1 year. Alhough DMDD has exclusion criteria that preclude the presence of other symptoms of mania, in the case of cyclothymic disorder full criteria for mania are never met, making a differential diagnosis challenging [1,101]. Adult studies show that cyclothymic disorder is a prevalent and impairing disorder. Further obscuring it in child research seems unwise. Research needs to examine the boundaries between DMDD versus cyclothymic disorder and other childhood disorders.
Conclusion & future perspective
As a whole, pediatric bipolar disorder is likely both under- and over-diagnosed [32], but cyclothymic disorder is almost always undiagnosed in young people. Failing to consider a diagnosis of cyclothymic disorder forces clinicians either to mislabel the disorder as not on the bipolar spectrum (with the associated risks for treatment mismatch), to bundle it with BP NOS or to ‘upgrade’ the diagnosis to bipolar I, contributing to concerns about overdiagnosis and harmful treatment side effects. Early intervention is associated with a more positive prognosis [73], but without accurate diagnosis there may be no benefits. Opportunities for substantial amelioration of symptoms appear to be best with the subthreshold presentations [90–92].
Cyclothymic disorder is well suited to a developmental psychopathology approach. The use of longitudinal studies is necessary in order to better understand the risk factors, course, treatment and outcomes of cyclothymic disorder in youth. This will also help to shed light on the impairment associated with cyclothymic disorder and increase our awareness of the burden of chronic mood dysregulation compared with acute mood symptomatology. There are data suggesting that the chronicity of cyclothymic disorder results in greater impairment than the relatively more severe symptoms found in bipolar I. Without prospective studies that clearly delineate each of the bipolar subtypes, we will not know the answer to this question, which is of high importance to public health.
Cyclothymic disorder is a prevalent and impairing disorder across the lifespan. Cyclothymic disorder appears to belong on the bipolar spectrum, given the validation study data and genetic data, but we know little about its course or its relation to temperament, depressive disorders and other subthreshold bipolar disorders. The DSM and International Classification of Diseases revisions provide an opportunity to consider how to best conceptualize cyclothymic disorder: as a subtype of bipolar disorder, an affective temperament, a diathesis, a prodrome or a personality style. The field would profit from attention invested in cyclothymic disorder, a concept described for the past 130 years and largely ignored for the past 20 years, at the expense of many young people and their future quality of life.
Practice points.
-
▪
Cyclothymic disorder occurs in youth and can be highly impairing.
-
▪
Cyclothymic disorder should be ruled out before a diagnosis of ‘bipolar not otherwise specified’ is considered.
-
▪
The key to diagnosing cyclothymic disorder in youth is assessing for an episode at least 1 year long, during which symptoms of both hypomania and depression are present.
-
▪
An episode must be marked by a change in functioning and, for diagnosis of cyclothymic disorder, associated with impairment.
-
▪
Treatment of cyclothymic disorder should follow the same guidelines that exist for other bipolar spectrum disorders in youth.
-
▪
Psychosocial treatment for youth with cyclothymic disorder and their families likely augments pharmacotherapy and contributes toward a better prognosis.
Acknowledgments
E Youngstrom has received grant funding from the NIH and Ohio Department of Mental Health, travel support from Bristol-Myers Squibb, and consulted about neurocognitive assessment with Lundbeck.
Footnotes
Financial & competing interests disclosure
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
▪ of interest
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Revised Edition. DC, USA: American Psychiatric Association; 2001. [Google Scholar]
- 2.Akiskal H, Khani M, Scott-Strauss A. Cyclothymic temperamental disorders. Psychiatr. Clin. North. Am. 1979;2:527–554. [Google Scholar]
- 3.Akiskal H, Akiskal K. Cyclothymic, hyperthymic, and depressive temperaments as subaffective variants of mood disorders. Am. Psych. Pr. Rev. Psych. 1992;11:43–62. [Google Scholar]
- 4.Vieta E, Reinares M, Rosa AR. Staging bipolar disorder. Neurotox. Res. 2011;19(2):279–285. doi: 10.1007/s12640-010-9197-8. [DOI] [PubMed] [Google Scholar]
- 5.Brieger P, Marneros A. Dysthymia and cyclothymia: historical origins and contemporary development. J. Affect. Disord. 1997;45(3):117–126. doi: 10.1016/s0165-0327(97)00053-0. [DOI] [PubMed] [Google Scholar]
- 6. Youngstrom E. Definitional issues in bipolar disorder across the life cycle. Clin. Psychol. Sci. Pr. 2009;16(2):140–160. ▪ Reviews the diagnostic criteria for bipolar disorders, with a focus on gaps and limitations. Also discusses the pros and cons of using a categorical versus dimensional model of bipolar disorder.
- 7. Lewinsohn P, Klein D, Seeley J. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J. Am. Acad. Child Psy. 1995;34(4):454–463. ▪ In a population of 1709 adolescents with bipolar spectrum disorders, 5.7% of the sample reported symptoms consistent with cyclothymic disorder; these ‘core positive’ youth exhibited impairment, treatment utilization and suicide attempts at the same level as youth with other bipolar spectrum disorders.
- 8.Akiskal H, Lancrenon S, Hantouche E. Validating the soft bipolar spectrum in the French National EPIDEP Study: the prominence of BP-II 1/2. J. Affect. Disord. 2006;96(3):207–213. doi: 10.1016/j.jad.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 9.Hantouche E. Validating Cyclothymia as a Distinct Variant of Bipolarity. Lisbon, Portugal: International Review of Bipolar Disorders; 2009. [Google Scholar]
- 10.Kessler R, Avenevoli S, Merikangas K. Mood disorders in children and adolescents: an epidemiologic perspective. Biol. Psychiatry. 2001;49(12):1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- 11.Youngstrom E, Birmaher B, Findling R. Pediatric bipolar disorder: validity, phenomenology, and recommendations for diagnosis. Bipolar Disord. 2008;10:194–214. doi: 10.1111/j.1399-5618.2007.00563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Meter A, Moreira A, Youngstrom E. Meta-analysis of epidemiologic studies of pediatric bipolar disorder. J. Clin. Psychiatry. 2011;72(9):1250–1256. doi: 10.4088/JCP.10m06290. [DOI] [PubMed] [Google Scholar]
- 13.Akiskal H, Bourgeois M, Angst J, Post R, Möller HJ, Hirschfeld R. Re-evaluating the prevalence of and diagnostic composition within the broad clinical spectrum of bipolar disorders. J. Affect. Disord. 2000;59(Suppl. 1):S5–S30. doi: 10.1016/s0165-0327(00)00203-2. [DOI] [PubMed] [Google Scholar]
- 14.Angst J, Gamma A, Benazzi F, Ajdacic V, Eich D, Rössler W. Toward a re-definition of subthreshold bipolarity: epidemiology and proposed criteria for bipolar-II, minor bipolar disorders and hypomania. J. Affect. Disord. 2003;73(1–2):133–146. doi: 10.1016/s0165-0327(02)00322-1. [DOI] [PubMed] [Google Scholar]
- 15.Judd L, Akiskal H. The prevalence and disability of bipolar spectrum disorders in the US population: re-analysis of the ECA database taking into account subthreshold cases. J. Affect. Disord. 2003;73(1–2):123–131. doi: 10.1016/s0165-0327(02)00332-4. [DOI] [PubMed] [Google Scholar]
- 16.Maughan B, Rutter M. Retrospective reporting of childhood adversity: issues in assessing long-term recall. J. Pers. Disord. 1997;11(1):19–33. doi: 10.1521/pedi.1997.11.1.19. [DOI] [PubMed] [Google Scholar]
- 17.Perugi G. Cyclothymic temperament and/or borderline personality disorder. Ann. Gen. Psychiatry. 2009;9(Suppl. 1):S77. [Google Scholar]
- 18.Ruggero CJ, Zimmerman M, Chelminski I, Young D. Borderline personality disorder and the misdiagnosis of bipolar disorder. J. Psychiatr. Res. 2010;44(6):405–408. doi: 10.1016/j.jpsychires.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perugi G, Akiskal H. Are bipolar II, and atypical depression, and borderline personality overlapping manifestations of a common cyclothymic-sensitive diathesis? World Psychiatry. 2011;10:45–51. doi: 10.1002/j.2051-5545.2011.tb00013.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perugi G, Toni C, Travierso M, Akiskal H. The role of cyclothymia in atypical depression: toward a data-based reconceptualization of the borderline-bipolar II connection. J. Affect. Disord. 2003;73(1–2):87–98. doi: 10.1016/s0165-0327(02)00329-4. [DOI] [PubMed] [Google Scholar]
- 21.Kessler R, Avenevoli S, Green J, et al. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J. Am. Acad. Child Psy. 2009;48(4):386–399. doi: 10.1097/CHI.0b013e31819a1cbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merikangas K, He J, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) J. Am. Acad. Child Psy. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biederman J, Faraone S, Wozniak J, et al. Clinical correlates of bipolar disorder in a large, referred sample of children and adolescents. J. Psychiatr. Res. 2005;39(6):611–622. doi: 10.1016/j.jpsychires.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 24.Chang K, Steiner H, Ketter T. Psychiatric phenomenology of child and adolescent bipolar offspring. J. Am. Acad. Child Psychiatry. 2000;39(4):453. doi: 10.1097/00004583-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 25. Faraone S, Biederman J, Wozniak J, Mundy E. Is comorbidity with ADHD a marker for juvenile-onset mania? J. Am. Acad. Child Psychiatry. 1997;36(8):1046–1055. doi: 10.1097/00004583-199708000-00012. ▪ Compared youth with cyclothymic disorder to youth with other bipolar spectrum disorders and nonbipolar childhood disorders. Results support the inclusion of cyclothymic disorder on the bipolar spectrum. Additionally, cyclothymic disorder could be reliably differentiated from non-mood disorders based on irritability, sleep disturbance, age of symptom onset, comorbid diagnoses and family history.
- 26.Reich W, Neuman R, Volk H, Joyner C, Todd R. Comorbidity between ADHD and symptoms of bipolar disorder in a community sample of children and adolescents. Twin Res. Hum. Genet. 2005;8:459–466. doi: 10.1375/183242705774310105. [DOI] [PubMed] [Google Scholar]
- 27.Sachs GS, Baldassano CF, Truman CJ, Guille C. Comorbidity of attention deficit hyperactivity disorder with early- and late-onset bipolar disorder. Am. J. Psychiatry. 2000;157(3):466–468. doi: 10.1176/appi.ajp.157.3.466. [DOI] [PubMed] [Google Scholar]
- 28.Robins E, Guze S. Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am. J. Psychiatry. 1970;126(7):983–987. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- 29.Van Meter A, Youngstrom E, Youngstrom J, Feeny N, Findling R. Examining the validity of cyclothymic disorder in a youth sample. J. Affect. Disord. 2011;132(1–2):55–63. doi: 10.1016/j.jad.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Youngstrom E, Van Meter A. Validating Cyclothymic Disorder in Youth. Nice, France: International Review of Bipolar Disorders; 2012. [Google Scholar]
- 31.Van Meter A, Youngstrom E, Demeter C, Findling R. Examining the validity of cyclothymic disorder in a youth sample: replication and extension. Presented at: 2011 Pediatric Bipolar Disorder Conference; 24–25 March 2011; MA, USA. [DOI] [PubMed] [Google Scholar]
- 32.Geller B, Zimmerman B, Williams M, DelBello M, Frazier J, Beringer L. Phenomenology of prepubertal and early adolescent bipolar disorder: examples of elated mood, grandiose behaviors, decreased need for sleep, racing thoughts and hypersexuality. J. Child Adolesc. Psychopharmacol. 2002;12(1):3–9. doi: 10.1089/10445460252943524. [DOI] [PubMed] [Google Scholar]
- 33.Harvey A, Mullin B, Hinshaw S. Sleep and circadian rhythms in children and adolescents with bipolar disorder. Dev. Psychopathol. 2006;18(4):1147–1168. doi: 10.1017/S095457940606055X. [DOI] [PubMed] [Google Scholar]
- 34.Edvardsen J, Torgersen S, Røysamb E, et al. Heritability of bipolar spectrum disorders. Unity or heterogeneity. J. Affect. Disord. 2008;106(3):229–240. doi: 10.1016/j.jad.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 35.Howland R, Thase M. A comprehensive review of cyclothymic disorder. J. Nerv. Ment. Dis. 1993;181(8):485–493. doi: 10.1097/00005053-199308000-00003. [DOI] [PubMed] [Google Scholar]
- 36. Klein D, Depue R, Slater J. Inventory identification of cyclothymia: IX. Validation in offspring of bipolar I patients. Arch. Gen. Psychiatry. 1986;43(5):441–445. doi: 10.1001/archpsyc.1986.01800050043005. ▪ Comparing the offspring of people with bipolar disorder to the offspring of healthy controls, responses on the General Behavior Inventory demonstrated a strong familial relationship between cyclothymic disorder and bipolar affective disorder.
- 37.Schraufnagel C, Brumback R, Harper C, Weinberg W. Affective illness in children and adolescents: patterns of presentation in relation to pubertal maturation and family history. J. Child Neurol. 2001;16(8):553–561. doi: 10.1177/088307380101600803. [DOI] [PubMed] [Google Scholar]
- 38. Akiskal H, Djenderedjian A, Rosenthal R, Khani M. Cyclothymic disorder: validating criteria for inclusion in the bipolar affective group. Am. J. Psychiatry. 1977;134(11):1227–1233. doi: 10.1176/ajp.134.11.1227. ▪ Validation study comparing 46 adults with cyclothymic disorder with 50 people with bipolar I, and 50 people with personality disorders prospectively. Comparisons provide evidence that cyclothymic disorder is on the bipolar spectrum.
- 39.Dunner DL, Russek FD, Russek B, Fieve RR. Classification of bipolar affective disorder subtypes. Compr. Psychiatry. 1982;23(2):186–189. doi: 10.1016/0010-440x(82)90064-5. [DOI] [PubMed] [Google Scholar]
- 40.Evans L, Akiskal H, Keck P, et al. Familiality of temperament in bipolar disorder: support for a genetic spectrum. J. Affect. Disord. 2005;85(1–2):153–168. doi: 10.1016/j.jad.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 41.Gonda X, Rihmer Z, Zsombok T, Bagdy G, Akiskal KK, Akiskal HS. The 5HTTLPR polymorphism of the serotonin transporter gene is associated with affective temperaments as measured by TEMPS-A. J. Affect. Disord. 2006;91(2–3):125–131. doi: 10.1016/j.jad.2005.12.048. [DOI] [PubMed] [Google Scholar]
- 42.Evans LM, Akiskal HS, Greenwood TA, et al. Suggestive linkage of a chromosomal locus on 18p11 to cyclothymic temperament in bipolar disorder families. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2008;147B(3):326–332. doi: 10.1002/ajmg.b.30601. [DOI] [PubMed] [Google Scholar]
- 43.Vázquez GH, Kahn C, Schiavo CEM, et al. Bipolar disorders and affective temperaments: a national family study testing the “endophenotype” and “subaffective” theses using the TEMPS-A Buenos Aires. J. Affect. Disord. 2008;108(1–2):25–32. doi: 10.1016/j.jad.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 44.Kochman F, Hantouche E, Ferrari P, Lancrenon S, Bayart D, Akiskal H. Cyclothymic temperament as a prospective predictor of bipolarity and suicidality in children and adolescents with major depressive disorder. J. Affect. Disord. 2005;85(1–2):181–189. doi: 10.1016/j.jad.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 45.Biederman J, Mick E, Spencer T, Wilens T, Faraone S. Therapeutic dilemmas in the pharmacotherapy of bipolar. Depression in the young. J. Child Adolesc. Psychopharmacol. 2000;10(3):185–192. doi: 10.1089/10445460050167296. [DOI] [PubMed] [Google Scholar]
- 46.Chang K, Saxena K, Howe M. An open-label study of lamotrigine adjunct or monotherapy for the treatment of adolescents with bipolar depression. J. Am. Acad. Child Psy. 2005;45(3):298–304. doi: 10.1097/01.chi.0000194566.86160.a3. [DOI] [PubMed] [Google Scholar]
- 47.Faraone S, Glatt S, Tsuang M. The genetics of pediatric-onset bipolar disorder. Biol. Psychiatry. 2003;53(11):970–977. doi: 10.1016/s0006-3223(02)01893-0. [DOI] [PubMed] [Google Scholar]
- 48.Findling R, Youngstrom E, McNamara N, et al. Early symptoms of mania and the role of parental risk. Bipolar Disord. 2005;7(6):623–634. doi: 10.1111/j.1399-5618.2005.00260.x. [DOI] [PubMed] [Google Scholar]
- 49.Lish J, Dime-Meenan S, Whybrow P, Price R, Hirschfeld R. The National Depressive and Manic-Depressive Association (DMDA) survey of bipolar members. J. Affect. Disord. 1994;31(4):281–294. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- 50.James A. Early-Onset Bipolar Disorder. Child Psychology and Psychiatry. NJ, USA: John Wiley and Sons; 2011. pp. 210–216. [Google Scholar]
- 51. Birmaher B, Axelson D, Goldstein B, et al. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the course and outcome of bipolar youth (COBY) study. Am. J. Psychiatry. 2009;166(7):795–804. doi: 10.1176/appi.ajp.2009.08101569. ▪ Longitudinal study of 413 youth with bipolar disorder did not specifically assess for cyclothymic disorder. However, the broad category of bipolar not otherwise specified was associated with poorer outcomes across several categories. Additionally, 38% of youth with bipolar not otherwise specified converted to bipolar I or II.
- 52.Freeman A, Youngstrom E, Michalak E, Siegel R, Meyers O, Findling R. Quality of life in pediatric bipolar disorder. Pediatrics. 2009;123(3):e446–e452. doi: 10.1542/peds.2008-0841. [DOI] [PubMed] [Google Scholar]
- 53.Romero S, Birmaher B, Axelson D, et al. Prevalence and correlates of physical and sexual abuse in children and adolescents with bipolar disorder. J. Affect. Disord. 2009;112(1–3):144–150. doi: 10.1016/j.jad.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the national comorbidity survey. Am. J. Public Health. 2001;91(5):753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Putnam FW. Ten-year research update review: child sexual abuse. J. Am. Acad. Child Psychiatry. 2003;42(3):269–278. doi: 10.1097/00004583-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 56.Silverman AB, Reinherz HZ, Giaconia RM. The long-term sequelae of child and adolescent abuse: a longitudinal community study. Child Abuse Negl. 1996;20(8):709–723. doi: 10.1016/0145-2134(96)00059-2. [DOI] [PubMed] [Google Scholar]
- 57.Leone PE, Christle CA, Nelson MC, Skib R, Frey AJ, Jolivette K. School Failure, Race, and Disability: Promoting Positive Outcomes, Decreasing Vulnerability for Involvement with the Juvenile Delinquency System. MD, USA: National Center on Education, Disability and Juvenile Justice; 2003. [Google Scholar]
- 58.Angold A, Messer SC, Stangl D, Farmer EM, Costello EJ, Burns BJ. Perceived parental burden and service use for child and adolescent psychiatric disorders. Am. J. Public Health. 1998;88(1):75–80. doi: 10.2105/ajph.88.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Appleyard K, Egeland B, van Dulmen MHM, Alan Sroufe L. When more is not better: the role of cumulative risk in child behavior outcomes. J. Child Psychol. Psyc. 2005;46(3):235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- 60.Baldessarini R, Tondo L. Suicide risk and treatments for patients with bipolar disorder. JAMA. 2003;290(11):1517–1519. doi: 10.1001/jama.290.11.1517. [DOI] [PubMed] [Google Scholar]
- 61.The Global Burden Of Disease: 2004 Update. Geneva, Switzerland: WHO; 2008. [Google Scholar]
- 62.Beautrais AL. Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am. J. Psychiatry. 2003;160(6):1093–1099. doi: 10.1176/appi.ajp.160.6.1093. [DOI] [PubMed] [Google Scholar]
- 63.Baldessarini R, Pompili M, Tondo L. Suicide in bipolar disorder: risks and management. CNS Spectr. 2006;11(6):465. doi: 10.1017/s1092852900014681. [DOI] [PubMed] [Google Scholar]
- 64.Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a reexamination. Am. J. Psychiatry. 2000;157(12):1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- 65.Brent D, Perper J, Goldstein C, et al. Risk factors for adolescent suicide. Arch. Gen. Psychiatry. 1988;45:581–588. doi: 10.1001/archpsyc.1988.01800300079011. [DOI] [PubMed] [Google Scholar]
- 66.Goldstein T, Birmaher B, Axelson D, et al. History of suicide attempts in pediatric bipolar disorder: factors associated with increased risk. Bipolar Disord. 2005;7(6):525–535. doi: 10.1111/j.1399-5618.2005.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Angst J, Cui L, Swendsen J, et al. Major depressive disorder with subthreshold bipolarity in the National Comorbidity Survey replication. Am. J. Psychiatry. 2010;167(10):1194–1201. doi: 10.1176/appi.ajp.2010.09071011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Akiskal H, Akiskal K, Lancrenon S, et al. Validating the bipolar spectrum in the French National EPIDEP Study: overview of the phenomenology and relative prevalence of its clinical prototypes. J. Affect. Disord. 2006;96(3):197–205. doi: 10.1016/j.jad.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 69.Alloy L, Urošević S, Abramson L, et al. Progression along the bipolar spectrum: a longitudinal study of predictors of conversion from bipolar spectrum conditions to bipolar I and II disorders. J. Abnorm. Psychol. 2011;121(1):16–27. doi: 10.1037/a0023973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Howes OD, Lim S, Theologos G, Yung AR, Goodwin GM, McGuire P. A comprehensive review and model of putative prodromal features of bipolar affective disorder. Psychol. Med. 2010;41(8):1567–1577. doi: 10.1017/S0033291710001790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lewinsohn P, Klein D, Seeley J. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disord. 2000;2:281–293. doi: 10.1034/j.1399-5618.2000.20309.x. [DOI] [PubMed] [Google Scholar]
- 72.Akiskal H, Downs J, Jordan P, Watson S, Daugherty D, Pruitt D. Affective disorders in referred children and younger siblings of manic-depressives: mode of onset and prospective course. Arch. Gen. Psychiatry. 1985;42(10):996–1003. doi: 10.1001/archpsyc.1985.01790330076009. [DOI] [PubMed] [Google Scholar]
- 73.Hauser M, Pfennig A, Özgürdal S, Heinz A, Bauer M, Juckel G. Early recognition of bipolar disorder. Eur. Psychiatry. 2007;22(2):92–98. doi: 10.1016/j.eurpsy.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 74.Cicero D, Epler A, Sher K. Are there developmentally limited forms of bipolar disorder? J. Abnorm. Psychol. 2009;118(3):431–447. doi: 10.1037/a0015919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Paykel E, Abbott R, Morriss R, Hayhurst H, Scott J. Sub-syndromal and syndromal symptoms in the longitudinal course of bipolar disorder. Br. J. Psychiatry. 2006;189(2):118–123. doi: 10.1192/bjp.bp.105.013870. [DOI] [PubMed] [Google Scholar]
- 76.Welner A, Welner Z, Leonard MA. Bipolar manic-depressive disorder: a reassessment of course and outcome. Compr. Psychiatry. 1977;18(4):327–332. doi: 10.1016/0010-440x(77)90003-7. [DOI] [PubMed] [Google Scholar]
- 77.Koukopoulos A, Sani G, Koukopoulos AE, et al. Duration and stability of the rapidcycling course: a long-term personal follow-up of 109 patients. J. Affect. Disord. 2003;73(1–2):75–85. doi: 10.1016/s0165-0327(02)00321-x. [DOI] [PubMed] [Google Scholar]
- 78.Birmaher B, Axelson D, Strober M, et al. Clinical course of children and adolescents with bipolar spectrum disorders. Arch. Gen. Psychiatry. 2006;63(2):175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McElroy S, Strakowski S, West S, Keck P, Jr, McConville B. Phenomenology of adolescent and adult mania in hospitalized patients with bipolar disorder. Am. J. Psychiatry. 1997;154(1):44–49. doi: 10.1176/ajp.154.1.44. [DOI] [PubMed] [Google Scholar]
- 80.Baldessarini RJ, Vazquez G, Tondo L. Treatment of cyclothymic disorder: commentary. Psychother. Psychosom. 2011;80:131–135. doi: 10.1159/000322234. [DOI] [PubMed] [Google Scholar]
- 81.Miklowitz D. Psychotherapy in combination with drug treatment for bipolar disorder. J. Clin. Psychopharmacol. 1996;16(Suppl. 1)(2):56S. doi: 10.1097/00004714-199604001-00007. [DOI] [PubMed] [Google Scholar]
- 82.Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar depression: a 1-year randomized trial from the systematic treatment enhancement program. Arch. Gen. Psychiatry. 2007;64(4):419–426. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Totterdell P, Kellett S. Restructuring mood in cyclothymia using cognitive behavior therapy: an intensive time-sampling study. J. Clin. Psychol. 2008;64(4):501–518. doi: 10.1002/jclp.20444. [DOI] [PubMed] [Google Scholar]
- 84.Fava GA, Rafanelli C, Tomba E, Guidi J, Grandi S. The sequential combination of cognitive behavioral treatment and well-being therapy in cyclothymic disorder. Psychother. Psychosom. 2011;80(3):136–143. doi: 10.1159/000321575. [DOI] [PubMed] [Google Scholar]
- 85.Goodwin G. Evidence-based guidelines for treating bipolar disorder: revised second edition recommendations from the British Association for Psychopharmacology. J. Psycholpharmacol. 2009;23(4):346–388. doi: 10.1177/0269881109102919. [DOI] [PubMed] [Google Scholar]
- 86.Kowatch R, Fristad M, Birmaher B, Wagner K, Findling R, Hellander M. Treatment guidelines for children and adolescents with bipolar disorder. J. Am. Acad. Child Psychiatry. 2005;44(3):213–235. doi: 10.1097/00004583-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 87.Findling R, Frazier T, Youngstrom E, et al. Double-blind, placebo-controlled trial of divalproex monotherapy in the treatment of symptomatic youth at high risk for developing bipolar disorder. J. Clin. Psychiatry. 2007;68(5):781–788. doi: 10.4088/jcp.v68n0519. [DOI] [PubMed] [Google Scholar]
- 88.Deltito J. The effect of valproate on bipolar spectrum temperamental disorders. J. Clin. Psychiatry. 1993;54(8):300–304. [PubMed] [Google Scholar]
- 89.Axelson DA, Birmaher B, Findling RL, et al. Concerns regarding the inclusion of temper dysregulation disorder with dysphoria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. J. Clin. Psychiatry. 2011;72(9):1257–1262. doi: 10.4088/JCP.10com06220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.DelBello M, Geller B. Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disord. 2001;3(6):325–334. doi: 10.1034/j.1399-5618.2001.30607.x. [DOI] [PubMed] [Google Scholar]
- 91.Miklowitz D, Chang K. Prevention of bipolar disorder in at-risk children: theoretical assumptions and empirical foundations. Dev. Psychopathol. 2008;20(3):881–897. doi: 10.1017/S0954579408000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shankman S, Lewinsohn P, Klein D, Small J, Seeley J, Altman S. Subthreshold conditions as precursors for full syndrome disorders: a 15-year longitudinal study of multiple diagnostic classes. J. Child Psychol. Psychiatry. 2009;50(12):1485–1494. doi: 10.1111/j.1469-7610.2009.02117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Website
- 101.American Psychiatric Association. D 00 Disruptive mood dysregulation disorder. [Accessed 19 June 2012]; www.dsm5.org/proposedrevision/pages/proposedrevision.aspx?rid=397.