Nonketotic hyperglycemia is a rare cause of hemichorea-hemiballismus. It is more common among postmenopausal woman and can be the first presentation of diabetes mellitus (1). This case report illustrates the importance of distinguishing this cause from other intracranial pathologies as prompt glycemic control leads to complete resolution of the symptoms and signs.
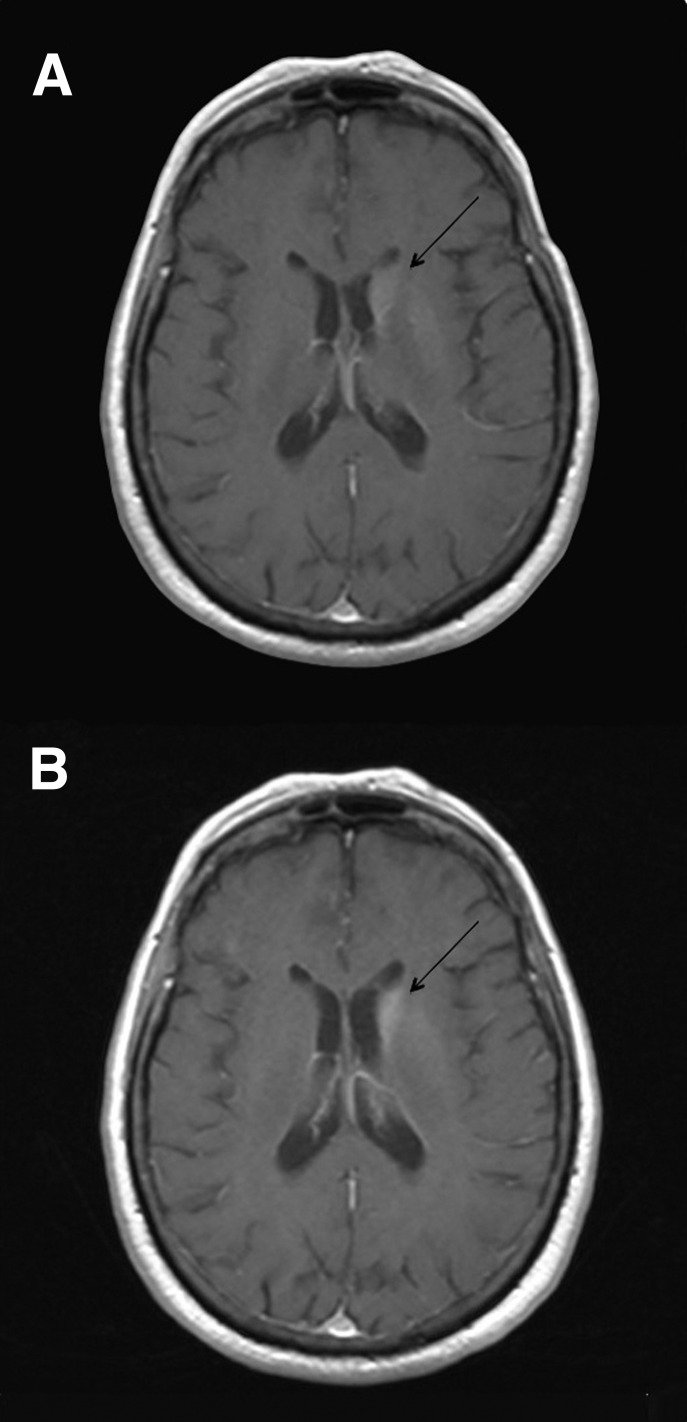
A 76-year-old female presented to our emergency department following a 24-h history of involuntary right upper- and lower-limb movements. There was no history of stroke or preceding trauma. Her neurological examination was notable for right-sided periodic choreiform and ballistic movements, which improved during sleep. Initial biochemistry revealed a blood glucose of 24.4 mmol/L (439.6 mg/dL), normal venous pH (7.37), and negative blood ketones (<0.5 mmol/L). Her HbA1c was 17.3% consistent with a prolonged period of undiagnosed diabetes mellitus. Computerized tomography (CT) revealed diffuse hyperdensity of the left basal ganglia, which was further characterized on magnetic resonance imaging (MRI) as increased T1-weighted signal change with abnormal enhancement in the caudate and lentiform nuclei (Fig. 1A). A twice-daily mixed insulin preparation (NovoMix 30) was commenced, and glycemic control was optimized with resolution of her symptoms within 72 h. At her 2-month follow-up she remained symptom-free despite persistent abnormalities in the left basal ganglia, as seen on her MRI (Fig. 1B).
Figure 1.
Axial brain MRI T1-weighted images postgadolinium with abnormal enhancement in the left caudate nucleus (arrows) at diagnosis (A) and 2-month follow-up (B).
This rare cause of hemichorea-hemiballismus is characterized by unilateral, involuntary, poorly patterned movements developing over a period of hours. The mean age of onset is 72 years with women affected more commonly than men. As demonstrated in our case, hemichorea-hemiballismus may be the first manifestation of decompensated diabetes mellitus, although it can also occur after years of poor glycemic control (2). The pathogenesis is thought to be related to hyperglycemia-induced perfusion changes in the contralateral striatum and ischemic excitotoxicity of GABAergic neurons. This results in excessive inhibition of the subthalamic nuclei and excitatory cortical output (3).
The diagnosis is made in the context of typical clinical and radiological features including the presence of ballistic or choreiform movements in the setting of marked hyperglycemia and the absence of ketoacidosis. CT scans typically show an area of hyperdensity in the basal ganglia, which can be distinguished from hypertensive hemorrhage as there is no associated mass effect, edema, or volume loss, and the internal capsule is usually spared. The characteristic finding on the T1-weighted MRI is high signal intensity in the contralateral putamen, which may persist for months despite clinical improvement (4).
The mainstay of treatment is aggressive glycemic control with resolution of hemichorea-hemiballismus in the majority of cases. In refractory cases, drugs that block postsynaptic dopamine (D2) receptors, such as haloperidol or risperidone, can be used. More recently there have been reports of improvement with topiramate, most likely through its GABAergic properties (5).
In summary, nonketotic hyperglycemia is an unusual but important differential diagnosis in patients with hemichorea-hemiballismus as prompt diagnosis and treatment of hyperglycemia has an excellent prognosis. All patients with this clinical presentation should be screened for diabetes.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
S.P. wrote the manuscript and researched the data. A.S.Z. and A.M.P. reviewed and edited the manuscript. S.P. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Crausman RS, Wen J, Al-Shalabi S. Choreoathetosis and diabetes. Diabetes Care 1997;20:1209–1210 [DOI] [PubMed] [Google Scholar]
- 2.Lin JJ, Lin GY, Shih C, Shen WC. Presentation of striatal hyperintensity on T1-weighted MRI in patients with hemiballism-hemichorea caused by non-ketotic hyperglycemia: report of seven new cases and a review of literature. J Neurol 2001;248:750–755 [DOI] [PubMed] [Google Scholar]
- 3.Shan DE, Ho DM, Chang C, Pan HC, Teng MM. Hemichorea-hemiballism: an explanation for MR signal changes. AJNR Am J Neuroradiol 1998;19:863–870 [PMC free article] [PubMed] [Google Scholar]
- 4.Oh SH, Lee KY, Im JH, Lee MS. Chorea associated with non-ketotic hyperglycemia and hyperintensity basal ganglia lesion on T1-weighted brain MRI study: a meta-analysis of 53 cases including four present cases. J Neurol Sci 2002;200:57–62 [DOI] [PubMed] [Google Scholar]
- 5.Dewey RB, Jr, Jankovic J. Hemiballism-hemichorea. Clinical and pharmacologic findings in 21 patients. Arch Neurol 1989;46:862–867 [DOI] [PubMed] [Google Scholar]