Abstract
Adult β-cell dysfunction, a hallmark of type 2 diabetes, can be programmed by adverse fetal environment. We have shown that fetal glucocorticoids (GCs) participate in this programming through inhibition of β-cell development. Here we have investigated the molecular mechanisms underlying this regulation. We showed that GCs stimulate the expression of peroxisome proliferator–activated receptor-γ coactivator-1α (PGC-1α), a coregulator of the GCs receptor (GR), and that the overexpression of PGC-1α represses genes important for β-cell development and function. More precisely, PGC-1α inhibited the expression of the key β-cell transcription factor pancreatic duodenal homeobox 1 (Pdx1). This repression required the GR and was mediated through binding of a GR/PGC-1α complex to the Pdx1 promoter. To explore PGC-1α function, we generated mice with inducible β-cell PGC-1α overexpression. Mice overexpressing PGC-1α exhibited at adult age impaired glucose tolerance associated with reduced insulin secretion, decreased β-cell mass, and β-cell hypotrophy. Interestingly, PGC-1α expression in fetal life only was sufficient to impair adult β-cell function whereas β-cell PGC-1α overexpression from adult age had no consequence on β-cell function. Altogether, our results demonstrate that the GR and PGC-1α participate in the fetal programming of adult β-cell function through inhibition of Pdx1 expression.
β-Cell failure and insulin resistance are the key factors in the pathogenesis of type 2 diabetes. Yet, the etiology of these defects is far from being completely understood. Recently, it has been proposed that an adverse fetal environment may affect organ development and function at adult age, a concept called “fetal programming of adult diseases.” Evidence has been gathered that altered fetal environment is actually associated with increased risks to develop several disorders such as diabetes, hypertension, or psychiatric illness (1). In the case of diabetes, it has been suggested that the function of the organs implicated in glucose homeostasis may be programmed during fetal life (2–4) and, more specifically, that adult β-cell dysfunction may originate from alterations of β-cell development caused by abnormal fetal environment (5).
To define how fetal environment controls β-cells, we designed and studied rodent models of maternal undernutrition associated with impaired fetal growth and altered β-cell function and mass (6–8). In these models, we showed that food restriction during the last week of pregnancy led to increased glucocorticoids (GCs) concentrations in the pregnant females and in their fetuses (6,8). GCs are primary stress hormones that regulate many biological processes, including reproduction, cell proliferation, and organ development. Yet, an excess of GCs during fetal development can also alter fetal growth (9), and recent studies proposed that excess stress and GCs during fetal life may participate in the onset of adult diseases (10). In fact, in our rodent models, fetal GCs overexposure impairs β-cell development (6,8) and leads to impaired glucose tolerance in adults due to decreased insulin secretion and β-cell mass (8). More precisely, we demonstrated that these effects depend on the presence in pancreatic precursor cells of the GCs receptor (GR), a member of the nuclear receptor superfamily (8). We thus provided strong evidence that fetal GCs are potent inhibitors of β-cell mass and function and can therefore have an important role in the fetal programming of β-cell failure in adults.
Among crucial genes for β-cell maturation, the transcription factor pancreatic duodenal homeobox 1 (Pdx1) has an essential role for pancreatic development and β-cell function. In humans (11) and mice (12), mutations or deletions of this gene are associated with pancreatic agenesis. Heterozygous loss-of-function Pdx1 mutations are linked to common human type 2 diabetes and cause heritable maturity-onset diabetes of the young type 4 (13,14). Pdx1-haploinsufficient mice exhibit small pancreatic islets with greatly reduced β-cell numbers and defects in insulin secretion leading to diabetes (12,15). Interestingly, we have shown that Pdx1 expression was greatly reduced in the pancreata of GCs-overexposed mouse fetuses (8), suggesting that Pdx1 expression is regulated by GCs.
To identify molecular mechanisms that participate in GC control of Pdx1 and β-cells, we investigated the GCs signaling pathway. GCs bind to the GRs in the cytoplasm that then migrate to the nucleus and act as a nuclear receptor to modulate the expression of target genes (16). Recent studies have shed light on how transcriptional coregulators that do not possess DNA-binding domain but interact with nuclear receptors can also regulate gene expression. For example, the protein peroxisome proliferator–activated receptor-γ coactivator-1α (PGC-1α) is a transcriptional coregulator that is recruited to the chromatin where it interacts with the GR and other proteins such as p300 and steroid receptor coactivator 1. This multiprotein complex then regulates gene transcription. Interestingly, PGC-1α controls the expression of genes involved in the regulation of cellular energy metabolism (17), and its expression is stimulated by the GCs in the liver (18). In β-cells, PGC-1α participates in regulating insulin secretion in vitro (19); yet, its involvement in vivo in β-cells and its regulation by GCs remained to be elucidated.
In the present work, we aimed at defining the role of PGC-1α in β-cells in vivo and its potential implication in the programming of β-cell dysfunction and Pdx1 expression. We showed that GCs increased PGC-1α expression in a β-cell line, in islets, and in the developing pancreas. We demonstrated that the GR and PGC-1α directly repress Pdx1 expression. We next generated mice with β-cell–inducible PGC-1α overexpression and showed that these adult mice are glucose intolerant, with decreased insulin secretion, decreased β-cell mass and size, and reduced Pdx1 expression. Finally, we showed that fetal PGC-1α overexpression is sufficient to alter adult β-cell function but not β-cell mass. Our results therefore place GCs and PGC-1α as important actors in the fetal programming of β-cell dysfunction.
RESEARCH DESIGN AND METHODS
Mouse islet isolation and cell culture.
Mouse islets were isolated with collagenase solution (1 mg/mL, Sigma-Aldrich, St. Louis, MO), separated on Histopaque (Sigma-Aldrich) gradient, and handpicked under a binocular microscope (Leica Microsystems GmbH, Wetzlar, Germany). Fetal rat islets were isolated from embryonic day 21 pancreata and cultured, as previously described (20). Islets were treated with 10−7 mol/L dexamethasone (Dex, Sigma-Aldrich). Min6 cells were similarly treated and cultured as described (21).
Mice and food restriction protocol.
CD1 Swiss pregnant mice underwent food restriction (50% of the control daily food intake) from 11.5 days of pregnancy until 18.5 days, as previously described (8). At 18.5 days of pregnancy, fetal pancreata were dissected.
Adenovirus-mediated protein overexpression.
PGC-1α overexpression was achieved using an adenovirus expressing the human PGC-1α cDNA under the control of a cytomegalovirus promoter (22). Islets from mutant mice with a GR deletion in β-cells (GRRipCre mice) (23) and control mice were isolated, as described above.
Chromatin immunoprecipitation.
DNA were extracted from Min6 cells and cross-linked with formaldehyde, and the sonicated protein-DNA complexes were isolated, incubated overnight at 4°C with anti-GR (M20, Santa Cruz Biotechnology, Santa Cruz, CA) or anti–PGC-1α antibody, and immunoprecipitated. In another set of experiments, protein-DNA complexes were immunoprecipitated first with the anti-GR antibody then with the anti–PGC-1α antibody. PCR was performed with AmpliTaq Gold Polymerase (Applied Biosystems, Life Technologies). Primers sequences are available upon request.
β-Cell–specific PGC-1α overexpressing mice.
Transgenic mice expressing the tetracycline transactivator from a bacterial artificial chromosome transgene containing the Insulin1 gene regulatory elements (Ins-tTA) were generated in our laboratory (24) as were transgenic mice carrying the tetracycline response element (TRE) controlling PGC-1α expression (TetO PGC-1α), which were described previously (25). The two mouse lines were crossed to generate Ins-PGC-1α double-transgenic mice. To stop PGC-1α overexpression from conception until adult age, pregnant and lactating mice were given 0.1 g/L doxycycline (Dox, Sigma-Aldrich) in their drinking water, and weaned mice received 1 g/L until adult age. Mice with PGC-1α overexpression never received Dox. All animal experiments were done according to the “Principles of Laboratory Animal Care” and the French law, authorization No. 75-435 delivered to B.V. by the French Ministry of Agriculture.
Intraperitoneal glucose tolerance test.
Glucose (2 g/kg body weight) was injected intraperitoneally to fasted mice, and blood glucose levels were measured before and 15, 30, 60, and 120 min after injection using a glucometer (Freestyle Papillon Mini; Abbott Diabetes Care, Abbott Park, IL). Serum insulin levels were measured by ELISA (Mercodia, Uppsala, Sweden).
Insulin tolerance test.
After a 5-h fast, insulin (1 unit/kg body weight) was injected intraperitoneally. Blood glucose levels were measured before and 15, 30, 60, and 120 min after the insulin injection.
Pancreatic insulin content.
Pancreatic insulin contents were extracted at −20°C in acidic ethanol (1.5% [vol/vol] HCl in 75% [vol/vol] ethanol) and assayed by ELISA kit (Mercodia).
Pancreas processing and quantitative morphometry.
Pancreata from adult mice were dissected, fixed, and sectioned. β-Cell mass was evaluated on eight sections per animal, as previously described (8).
RNA preparation and real-time PCR.
Total RNAs were extracted using RNeasy Plus extraction kit (Qiagen, Hilden, Germany). RNAs were reverse-transcribed into cDNA using Superscript II reverse transcriptase (Invitrogen). Gene expression was quantified by real-time PCR with SybrGreen supermix in a MyIQ thermocycler (Biorad, Hercules, CA). Gene expression was normalized for the 18S ribosomal RNA. Primers sequences are available upon request.
Protein extraction and Western blot.
Total proteins were separated on SDS-PAGE gels and transferred to nitrocellulose membranes. Membranes were incubated with antibodies raised in rabbit against Pdx1 (gift of Dr. Raphael Scharfmann, INSERM, Paris, France), against PGC-1α (25) or against actin (Sigma-Aldrich). Band quantification was performed using a Kodak Imager (Kodak, Rochester, NY).
Statistical analysis.
All results are expressed as means ± SD. The statistical significance of variations was tested by a Mann-Whitney nonparametric test. P values <0.05 were considered significant.
RESULTS
GCs elevation increases PGC-1α that in return modulates the expression of Pdx1 and other β-cell genes.
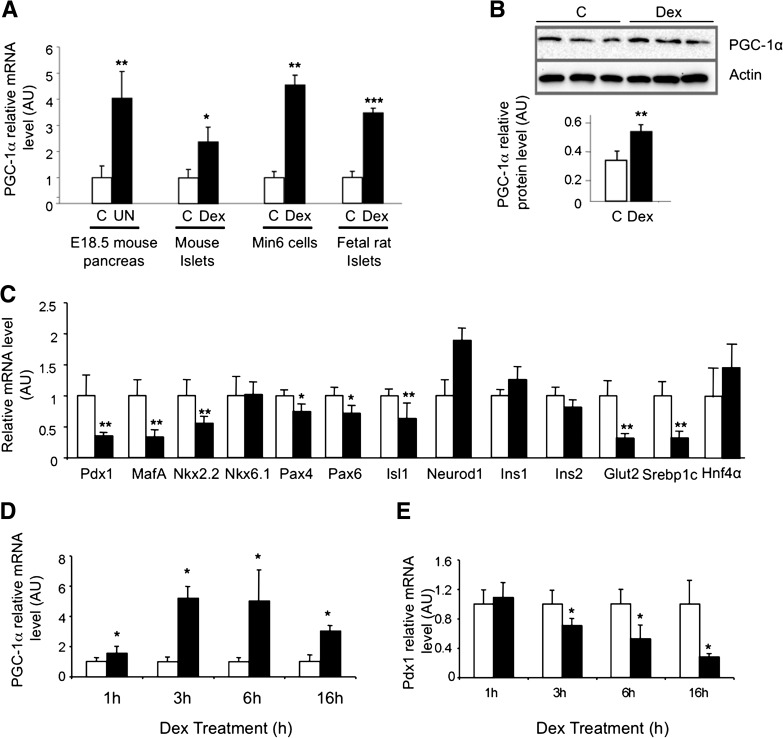
PGC-1α is a coactivator that plays major roles for several nuclear receptors, including the GR, and GCs increase PGC-1α expression in the liver (18) where it cooperates with the GR to modulate adaptative metabolic responses. To define if PGC-1α could participate in the GCs effects in the β-cells, we first asked whether GCs regulate PGC-1α in these cells. In a previous work, we showed that maternal undernutrition leads to overexposure of the fetuses to GCs (8). Here we showed that this GCs elevation in vivo increases PGC-1α expression in vivo in the pancreata of these fetuses. Similarly, in vitro, a 24-h Dex treatment increases PGC-1α expression in isolated mouse islets, in clonal Min6 cells, and in rat fetal islets (Fig. 1A). Dex treatment increases PGC-1α protein in isolated mouse islets (Fig. 1B). This GCs-induced increase of PGC-1α expression was associated with decreased expression of key β-cell genes in Min6 cells, such as Pdx1, Nkx2.2, Pax4, Pax6, Isl1, MafA, Srebp1c, and the glucose transporter Glut2 induced by Dex treatment (Fig. 1C).
FIG. 1.
GCs stimulate PGC-1α and inhibit Pdx1 in β-cells. A: PGC-1α expression in fetal pancreata at 18.5 days of pregnancy (E18.5) in control (C, white bars) or GCs overexposure conditions induced by maternal under nutrition (UN, black bars), in mouse islets, Min6 cells, and fetal rat islets cultured in control conditions (C, white bars) or treated with Dex (black bars) for 24 h. B: PGC-1α protein levels in mouse islets cultured in control conditions (C, white bar) or treated with Dex (black bar). C: Gene expression in Min6 cells cultured in control (white bars) or Dex-treated (black bars) conditions for 24 h. Time course effect of Dex on PGC-1α (D) and Pdx1 (E) expression measured after 1, 3, 6, and 16 h in control (white bars) or Dex-treated (black bars) Min6 cells. Results are expressed as means ± SD for n = 4 independent experiments. *P < 0.05, **P < 0.01, and ***P < 0.001 when comparing pancreata from control and fetuses overexposed to GCs and Dex-treated vs. control islets or Min6 cells, pancreata from control and fetuses overexposed to GCs using a Mann-Whitney nonparametric test.
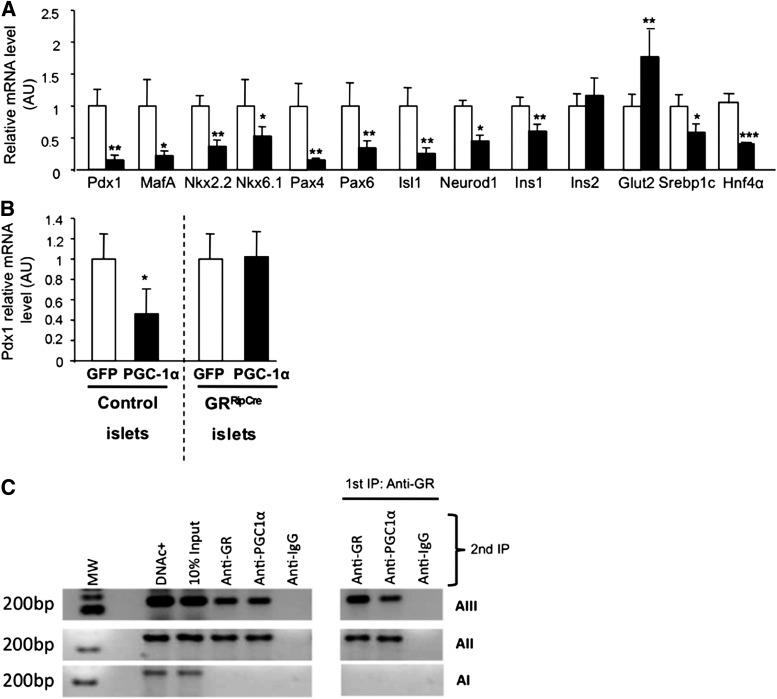
Because GCs repress most of the genes in β-cells but activate PGC-1α, we asked whether this increased PGC-1α expression could be implicated in the effects of GCs on β-cells. First, we made a time-course measurement of gene expression after Dex treatment. We observed that increased PGC-1α expression (1 h after treatment, Fig. 1D) preceded decreased Pdx1 expression (3 h after treatment, Fig. 1E), suggesting that GCs-stimulated PGC-1α may be involved in GC repression of Pdx1. To define this potential role, we overexpressed PGC-1α with an adenovirus in Min6 cells and found that it led to decreased mRNA levels of Pdx1 Nkx2.2, Pax4, Pax6, Isl1, MafA, Nkx6.1, Ins1, Srebp1c, and Hnf4a (Fig. 2A). The similarities between Dex treatment and PGC-1α overexpression on β-cell gene regulation suggested that PGC-1α participates in the GCs effects on β-cells.
FIG. 2.
PGC-1α inhibits Pdx1 expression through interaction with the GR. A: Gene expression in Min6 cells infected with adenoviruses expressing only the green fluorescent protein (GFP, white bars) or expressing PGC-1α and GFP (black bars). Gene expression was measured in Min6 cells by real-time PCR 24 h after infection and normalized to Min6 cells infected with adenovirus expressing GFP. B: Pdx1 expression in isolated islets from control mice (GRlox/lox) and mice lacking the GR in mature β-cells (GRRipCre) were infected with adenoviruses expressing GFP (white bars) or PGC-1α and GFP (black bars). C: ChIP of areas I, II, and III of the Pdx1 promoter with an anti-GR or an anti–PGC-1α antibody. Agarose gels showing (from left to right): molecular weight markers, positive control, input (DNA without IP), IP with anti-GR antibody, IP with anti–PGC-1α antibody, and IP with anti-IgG. Right panel shows sequential IP with first anti-GR antibody, then with anti-PGC-1α or anti-GR antibody. Lines 1, 2, and 3 show typical results obtained with primers located in area III, II, and I, respectively. Results are means ± SD on n = 4 independent experiments. *P < 0.05, **P < 0.01, and ***P < 0.001 using a Mann-Whitney nonparametric test.
Because PGC-1α associates with many nuclear receptors, we tried to specify if PGC-1α action on Pdx1 was mediated through the GR. Islets from mice deleted for the GR in β-cells, GRRipCre (23), and from control mice were infected with an adenovirus expressing PGC-1α (Fig. 2B). In control islets, PGC-1α overexpression decreased Pdx1 expression, whereas in the absence of GR, PGC-1α overexpression had no effect on the Pdx1 mRNA level, demonstrating that Pdx1 repression by PGC-1α requires the presence of the GR.
We next studied whether GR and PGC-1α regulate Pdx1 through direct repression of the Pdx1 promoter. First, we aimed at defining if a complex containing GR and PGC-1α could bind to the Pdx1 promoter. Chromatin immunoprecipitation (ChIP) with an anti-GR antibody of sheared DNA from Min6 cells revealed specific amplification bands for areas II and III of the Pdx1 promoter (Fig. 2C). ChIP with an anti–PGC-1α antibody revealed PCR products for the same areas (Fig. 2C), showing that PGC-1α is recruited onto these DNA regions. Then, sequential ChIP, first with an anti-GR antibody and then with an anti-PGC-1α antibody, led to PCR products for areas II and III, demonstrating that a complex containing PGC-1α and GR binds to areas II and III. Additional experiments using mutations in areas II and III showed that GCs actually repress Pdx1 promoter activity through binding of the GR to area II (Supplementary Data).
Because we had demonstrated in vitro that PGC-1α was implicated in the regulation of Pdx1 and other β-cell genes, we generated mice with β-cell specific PGC-1α overexpression to define how PGC-1α regulates β-cells in vivo.
β-Cell–specific PGC-1α overexpression alters insulin secretion and glucose homeostasis.
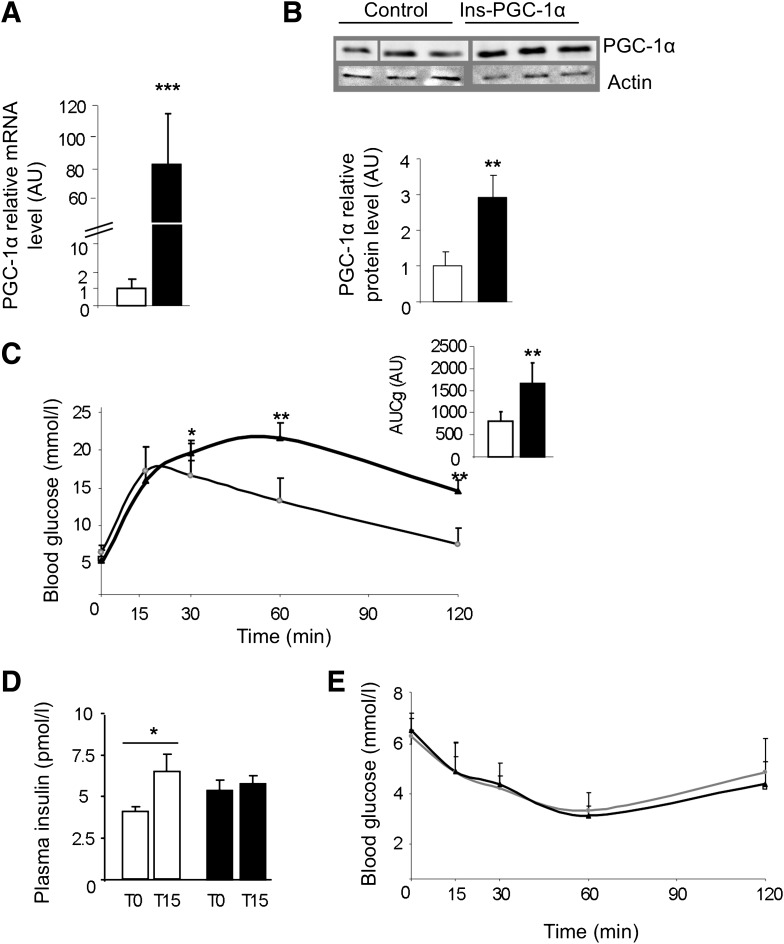
We used tetracycline-dependent inducible gene expression to generate mice overexpressing PGC-1α in β-cells. We crossed TetO-PGC-1α hemizygous mice carrying the cDNA coding PGC-1α under the control of a tetracycline-dependent promoter (25) with Ins-tTA mice hemizygous mice expressing the tetracycline transactivator (tTA) under regulatory elements of the Insulin1 gene recently generated in the laboratory (24). We obtained Ins-tTA + TetO-PGC-1α mice that will be referred as Ins-PGC-1α mice for the rest of the study and will be compared with Ins-tTA mice considered as controls.
We measured increased PGC-1α mRNA (Fig. 3A) and protein (Fig. 3B) levels in islets from Ins-PGC-1α mice at age 6 months compared with control islets. Ins-PGC-1α mice were hyperglycemic in the fed state (9.9 ± 2.7 vs. 7.1 ± 1.6 mmol/L in controls, P < 0.05), with lower blood insulin levels (4.2 ± 1.6 vs. 7.8 ± 3.72 pmol/L, P < 0.05). The intraperitoneal glucose tolerance test (ipGTT) revealed glucose intolerance in mice overexpressing PGC-1α in β-cells (Fig. 3C) with altered glucose-stimulated insulin secretion (GSIS) during the ipGTT (Fig. 3D). Whole-body insulin sensitivity assessed by the insulin tolerance test showed no apparent differences between the two groups (Fig. 3E). Thus, β-cell–specific PGC-1α overexpression impairs glucose tolerance and decreases GSIS.
FIG. 3.
PGC-1α overexpression in β-cells impairs glucose tolerance. PGC-1α mRNA (A) and protein levels (B) in islets from control mice (white bars) and Ins-PGC-1α mice (black bars). C: The ipGTT of Ins-PGC-1α (black triangles) is compared with control mice (white circles). The inset shows the area under the curve from 0 to 120 min of plasma glucose of these mice. D: Serum insulin levels before and 15 min after glucose injection in control (white bars) and Ins-PGC-1α (black bars) mice. E: Insulin tolerance test was performed in Ins-PGC-1α (black triangles) and control (white circles) mice. All values are means ± SD. *P < 0.05, **P < 0.01, and ***P < 0.001 when comparing Ins-PGC-1α with control mice using a Mann-Whitney nonparametric test (n = 5 per group).
β-Cell–specific PGC-1α overexpression impairs β-cell gene expression and β-cell mass.
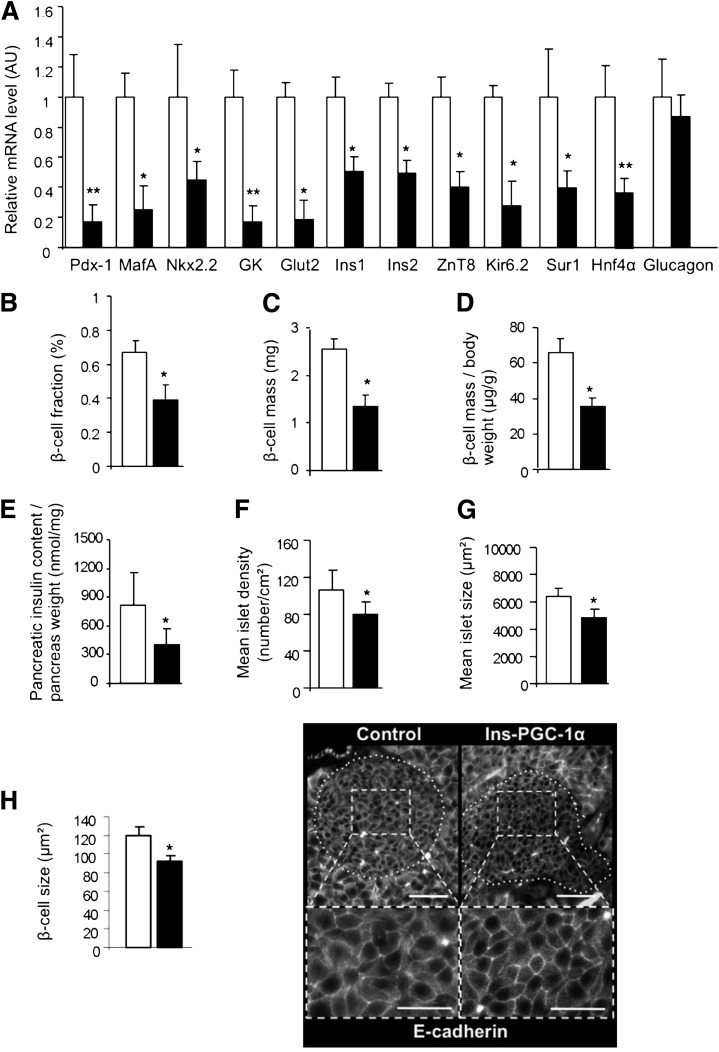
In islets from 6-month-old Ins-PGC-1α mice, β-cell PGC-1α overexpression was associated with dramatic reductions in the mRNA levels of several key β-cell genes, including Pdx1, MafA, Nkx2.2, Ins1, Ins2, ZnT-8, Glut2, glucokinase (GK), Kir6.2, Sur1, and Hnf4α (Fig. 4A). No change in glucagon expression was observed, suggesting that α-cells were not altered.
FIG. 4.
Impaired β-cell gene expression and mass in Ins-PGC-1α mice. A: Gene expression in islets from control (white bars) and Ins-PGC-1α (black bars) mice. Morphometric analysis of control (white bars) and Ins-PGC-1α (black bars) mice: β-cell fraction (B), absolute β-cell mass (C), and β-cell mass relative to body weight (D). E: Pancreatic insulin content from Ins-PGC-1α vs. control mice. Number of islets per cm2 (F) and mean islet size in Ins-PGC-1α and control mice (G). H: Individual β-cell size was morphometrically quantified in control (white bars) and Ins-PGC-1α (black bars) mice and illustrated by immunofluorescent staining for E-cadherin. Scale bar is 50 µm for upper panels and 25 µm for lower panels. Results are expressed as means ± SD. *P < 0.05, **P < 0.01 when comparing Ins-PGC-1α with control mice using a Mann-Whitney nonparametric test (n = 5 per group).
Analysis of the endocrine pancreas from Ins-PGC-1α mice showed a strong reduction of β-cell fraction (Fig. 4B), absolute β-cell mass (Fig. 4C), β-cell mass per unit of body weight (Fig. 4D), and pancreatic insulin content (Fig. 4E). Precise analysis revealed a decreased number of islets per tissue surface unit (Fig. 4F), decreased mean islet size (Fig. 4G), and β-cell hypotrophy (Fig. 4H) in Ins-PGC-1α mice.
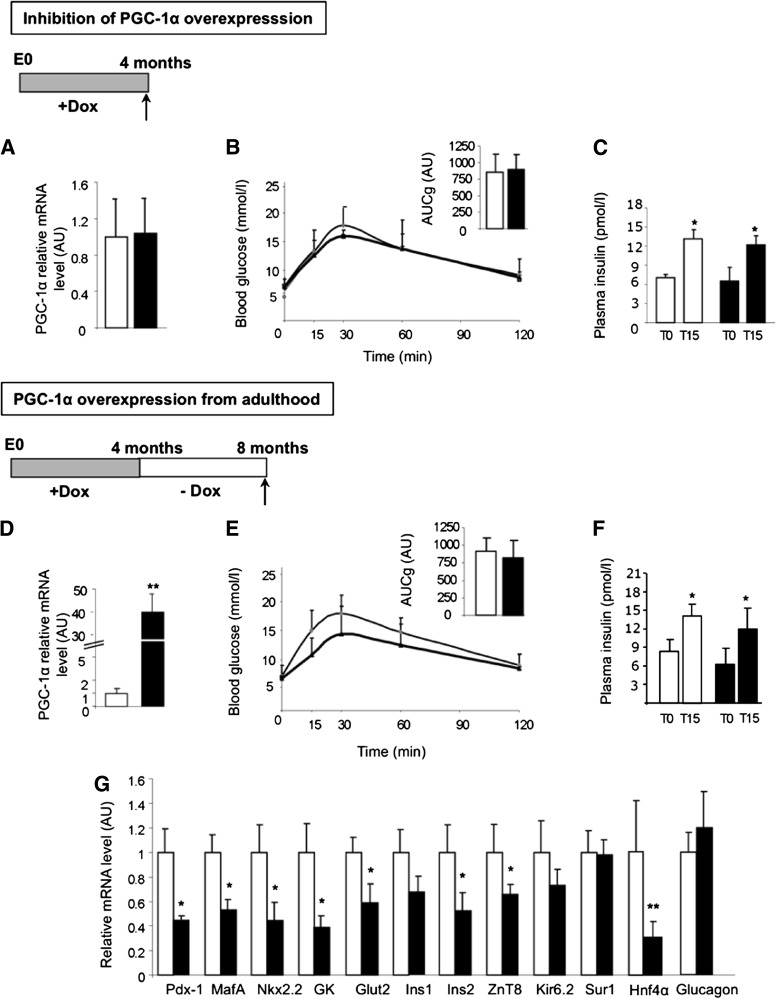
To clearly prove that the phenotype of Ins-PGC-1α mice was caused by PGC-1α overexpression, control and Ins-PGC-1α mice were treated with Dox in their drinking water from conception to adulthood to inhibit PGC-1α overexpression. PGC-1α mRNA levels in islets from Dox-treated Ins-PGC-1α mice were comparable with Dox-treated controls (Fig. 5A), and these animals presented normal glucose tolerance (Fig. 5B) and GSIS (Fig. 5C).
FIG. 5.
PGC-1α overexpression from adult age does not alter insulin secretion. A: PGC-1α expression in islets of 4-month-old control (white bars) and Ins-PGC-1α (black bars) mice after Dox treatment from conception. B: IpGTT performed on Ins-PGC-1α (black triangles) and control (white circles) mice. Inset shows the area under the curve for 0–120 min (AUC0–120 min) of plasma glucose of these mice. C: Serum insulin levels before and 15 min after intraperitoneal glucose in control (white bars) and Ins-PGC-1α (black bars) mice. D: PGC-1α expression in islets of control (white bars) and Ins-PGC-1α (black bars) mice 4 months after stopping Dox treatment. E and F: IpGTT and GSIS in Ins-PGC-1α (black triangles) and control (white circles) mice. Inset shows AUC0–120 min of plasma glucose of these mice. G: Islet gene expression in islets of control (white bars) and Ins-PGC-1α (black bars) mice 4 months after stopping Dox treatment. All values are means ± SD. *P < 0.05, **P < 0.01 when comparing Ins-PGC-1α with control mice using a Mann-Whitney nonparametric test (n = 5 per group).
PGC-1α overexpression from adult age does not impair GSIS and glucose homeostasis.
To determine whether β-cell–specific PGC-1α overexpression starting from adult stage could impair β-cell function and glucose tolerance, Ins-PGC-1α mice were given Dox from conception to adulthood, and Dox treatment was stopped at age 4 months to induce PGC-1α overexpression. Four months after the arrest of Dox treatment, we observed that although PGC-1α mRNA levels in the islets were increased as expected (Fig. 5D), Ins-PGC-1α mice presented normal glucose tolerance (Fig. 5E) and GSIS (Fig. 5F). Yet, the increased PGC-1α expression in Ins-PGC-1α islets was still associated with decreased Pdx1, MafA, Glut2, GK, or Ins2 mRNA levels, whereas Ins1, Kir6.1 and Sur-1 mRNA levels remained unchanged (Fig. 5G).
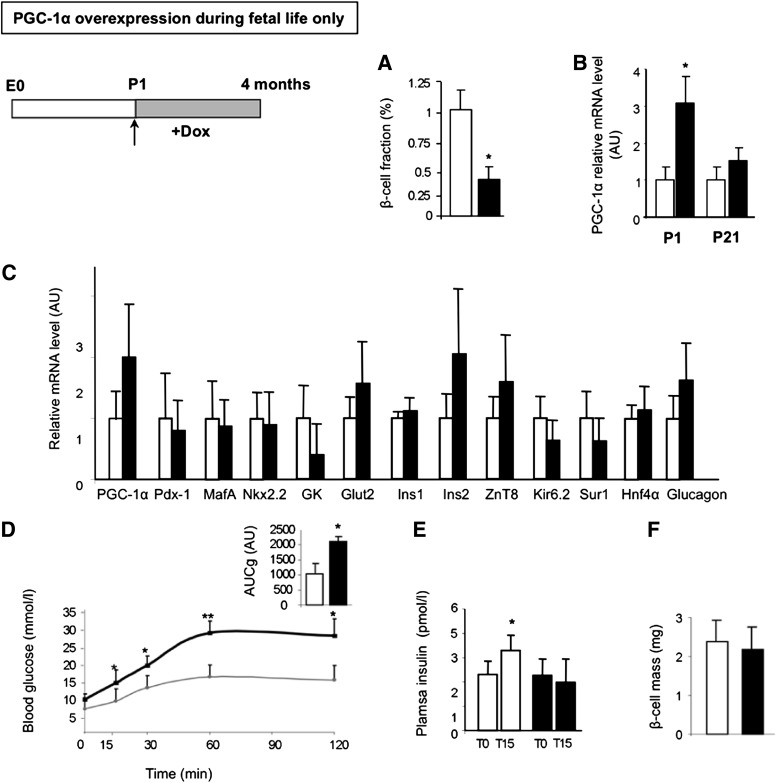
PGC-1α overexpression during fetal life only is sufficient to alter adult β-cell function.
To investigate the consequences of PGC-1α overexpression only during fetal life, we stopped PGC-1α overexpression by giving Dox to Ins-PGC-1α mice from birth onwards. At birth (P1), just before Dox treatment, we observed decreased β-cell fraction in Ins-PGC-1α neonates (Fig. 6A) together with PGC-1α overexpression (Fig. 6B, P1). When Dox treatment was given from birth, PGC-1α overexpression was stopped, as illustrated by normal mRNA levels in Ins-PGC-1α at postnatal day 21 (P21; Fig. 6B). Dox treatment was continued until adulthood, ∼6 months old. In mice with PGC-1α expression only during fetal life, we found no difference at adult age in islet PGC-1α or other β-cell gene mRNA levels compared with control mice (Fig. 6C). Yet, those mice showed impaired glucose tolerance (Fig. 6D) and decreased GSIS (Fig. 6E). Interestingly, their β-cell mass was similar to that of controls (Fig. 6F). Thus, β-cell–specific PGC-1α overexpression during fetal life only was sufficient to impair adult β-cell function without altering β-cell mass.
FIG. 6.
PGC-1α overexpression during fetal life only is sufficient to impair β-cell function. A: β-Cell fraction was morphometrically measured on pancreatic sections from control (white bars) and Ins-PGC-1α (black bars) newborn mice. B: PGC-1α mRNA levels in pancreata of control (white bars) and Ins-PGC-1α (black bars) mice at postnatal day 1 (P1) and 21 (P21, left to right) upon Dox treatment from birth. C: PGC-1α and β-cell genes mRNA levels in islets and β-cell mass of 4-month-old control (white bars) and Ins-PGC-1α (black bars) mice upon Dox treatment from birth. D: IpGTT performed on 4-month-old Ins-PGC-1α (black triangles) compared with control (white circles) mice under Dox treatment from birth. Inset shows the area under the curve for 0–120 min of plasma glucose of these mice. E: Serum insulin levels before and 15 min after intraperitoneal glucose injection in control (white bars) and Ins-PGC-1α (black bars) mice. F: β-Cell mass of control (white bars) and Ins-PGC-1α (black bars) mice. All values are means ± SD. *P < 0.05, **P < 0.01 when comparing control with Ins-PGC-1α mice using a Mann-Whitney nonparametric test (n = 5 per group).
DISCUSSION
Exciting hypotheses suggest that type 2 diabetes may originate from alterations in the development of organs involved in glucose homeostasis as a consequence of an adverse fetal environment (26). We proposed that β-cell development is impaired when fetal homeostasis is perturbed, especially when fetuses are exposed to an excess of GCs (6,8). Here, we have characterized the molecular mechanisms through which GCs regulate β-cell development and function. We first showed that GCs upregulate the expression of the GR coregulator PGC-1α in β-cells and that PGC-1α participates in the GCs effects on these cells. Then, we showed that GCs potently repress the expression of the key transcription factor, Pdx1, in β-cells through a direct binding of a GR/PGC-1α complex to the Pdx1 promoter on a crucial region for β-cell–specific promoter activity. We generated mice overexpressing PGC-1α in β-cells that display impaired glucose tolerance associated with decreased insulin secretion, Pdx1 expression, and β-cell mass with β-cell hypotrophy. Finally, we demonstrated that PGC-1α overexpression during fetal life only is sufficient to induce β-cell dysfunction in adult mice.
We had previously shown with rodent models of fetal undernutrition that GCs are potent inhibitors of β-cell development (6) by targeting pancreatic precursor cells engaged in the endocrine lineage (23). We also suggested that a similar regulation was likely to take place in humans because the GR was expressed early in the human fetal pancreas in precursor cells at the time when they cluster and start to express Pdx1 (27). Moreover, we recently provided genetic evidence in mice that the GR was required for the negative effects of GCs on β-cell development (8). However, the precise molecular mechanisms and partners implicated remained unclear. During pancreas development and β-cell differentiation, Pdx1 has been shown to play crucial roles (28,29). Pdx1 levels are tightly regulated, and any impairment of this regulation results in the inability to regulate glucose levels (30) and β-cell mass (31). We, and others, have reported that GCs treatment leads to a decreased Pdx1 expression in rodent β-cells and islets (32–34). Here, we show that GR binds to area II of the mouse Pdx1 promoter and decreases its activity. Binding of GR is thought to require GCs response elements (GRE), but we could not identify any GRE in area II, based on consensus sequence (35). Yet, physical interaction of the GR to area II was proven by ChIP experiments. Because the area II region is conserved in the Pdx1 promoter in humans (36), it is likely that GR would bind to and also inhibit the human Pdx1 promoter, a hypothesis that requires further investigation. In line with these results, GC has been shown to inhibit the human insulin gene through the binding of the GR on a negative GRE located upstream of the gene (37).
GR is a nuclear receptor that can activate or repress gene expression, a role that depends on coregulators. PGC-1α is known to coregulate several nuclear receptors, including the GR (38). We thus investigated if PGC-1α could participate in Pdx1 regulation together with the GR. PGC-1α plays a major role in the control of gluconeogenic genes in the liver and in mitochondrial biogenesis (39), and its expression is upregulated by GC treatment in the liver (18). Here, we present data showing that GCs increase PGC-1α expression in β-cells and that PGC-1α contributes to the repression of Pdx1 expression mediated by the GCs. This places PGC-1α as an actor of the GCs regulation of β-cells. PGC-1α is usually described as a coactivator of nuclear receptors (17). We propose that PGC-1α also represses gene expression, thereby acting as a corepressor. In fact, a study showed that PGC-1α is involved in the GR-mediated repression of the human insulin gene (40). We suggest that PGC-1α plays a similar role in the GR-mediated repression of Pdx1 in β-cells. In line with this, a recent article showed that GCs treatment decreased Pdx1, increased PGC-1α expression, and inhibited porcine neonatal pancreas cell cluster differentiation into β-cells (41). Thus, similarly to what we show in murine fetal pancreas, PGC-1α is stimulated by GCs in porcine cells.
We found that GCs and PGC-1α had similar effects on most of the β-cell genes in vitro. Yet, Neurod1 and Glut2 seem to be differentially regulated. We found that Neurod1 expression is unchanged by GCs treatment and decreased by PGC-1α overexpression. Similar observations are found in the literature: PGC-1α downregulates its expression in islets (42), and in neurons GCs have no effect on Neurod1 expression (43). We found that Glut2 expression is decreased by GCs and increased by PGC-1α overexpression. GCs-induced Glut2 inhibition has been reported (44). Glut2 upregulation by PGC-1α may be due to an interaction between PGC-1α and members of the peroxisome proliferator–activated receptor (PPAR) family because a PPAR response element upregulating Glut2 expression has been identified in the Glut2 promoter (45).
Several studies in animal models and in humans suggest a link between PGC-1α and diabetes (39). Here, we show that β-cell–specific PGC-1α overexpression in transgenic mice leads at adult age to impaired GSIS and strongly decreased β-cell mass, associated with impaired glucose tolerance. So far, the cellular mechanisms explaining these defects are unknown. PGC-1α overexpression in cultured islets or β-cell lines suppressed glucose-stimulated membrane depolarization, induced glucose-6-phosphatase, and thereby reduced insulin secretion together with changes in expression of genes involved in energy metabolism and control of β-cell function (19). In addition, reduced insulin secretion has been observed after PGC-1α–induced uncoupling protein 2 (UCP2) expression in β-cells (46). An increased respiration uncoupling in islet mitochondria through UCP2 might lead to a lower ATP/ADP ratio, which could explain the impaired insulin secretion described here. Such modifications will be investigated in Ins-PGC-1α mice. In addition, we have shown that Ins-PGC-1α mice display β-cell hypotrophy, a defect that may participate in the phenotype because another study negatively correlated β-cell size with GSIS (47). The deletion of the S6K gene reduces β-cell size (48), while deletion of LKB1 increases β-cell size (49). The implication of these molecules in the PGC-1α–mediated β-cell hypotrophy deserves further investigation.
A growing body of evidence suggests that prenatal stress, most likely resulting in fetal GCs overexposure, is a major adverse intrauterine environment that alters organ development, with important implications for the developmental programming of adult diseases, including hypertension, dysregulations of the hypothalamo-pituitary-adrenal axis, and glucose homeostasis disorders (50). Our results place PGC-1α as a GCs-induced gene implicated in the β-cell programming by the fetal environment. In fact, in our model of fetal food restriction, the increased GC concentrations stimulated PGC-1α expression and reduced Pdx1 in the pancreas (8). This reinforces the idea that PGC-1α may act as an intermediate of GCs’ negative action on β-cells. Moreover, PGC-1α overexpression during fetal life only is sufficient to permanently impair adult glucose homeostasis, reinforcing the implication of this transcriptional regulator in the fetal programming of β-cells by GCs.
The precise mechanisms underlying the effects of PGC-1α on β-cell programming remain to be defined. Such alterations could be mediated through epigenetic modulations occurring during the fetal period of PGC-1α overexpression. Actually, PGC-1α has been shown to control gene expression through epigenetic mechanisms: it regulates the expression of Bmal1, a clock gene involved in β-cell function, through alterations of histone methylation and acetylation (51). How epigenetic modifications could be involved in the fetal programming by PGC-1α remains to be investigated.
In conclusion, our data point out the implication of the GR and its coregulator PGC-1α in the negative control of Pdx1 expression and β-cell function. We depict the molecular mechanisms underlying the control of β-cell mass and function by GCs and also propose that PGC-1α may participate in the GCs inhibition of β-cells. Finally, we point out β-cell PGC-1α overexpression during fetal life as a potential mechanism participating in the programmed dysfunction of adult β-cells.
Supplementary Material
ACKNOWLEDGMENTS
B.V. received a fellowship from the Ministère de l’Enseignement Supérieur et de la Recherche and financial support from the Fondation pour la Recherche Médicale. These studies were supported by INSERM, CNRS, the European Union (FP5 Nutrix QLK1-CT-2000-00083 and FP6 Earnest Food-CT-2005-007036 programs), the Agence Nationale de la Recherche (Grant Gramsy No. A05245DS), Société Francophone du Diabète to J.-P.R., B.Bl., and B.Br.; Lilly to J.-P.R.; and Institut Benjamin Delessert to B.Bl. No other potential conflicts of interest relevant to this article were reported.
B.V. and J.-P.R. designed the studies, performed experiments, analyzed the data, and wrote, reviewed, and edited the manuscript. P.Z., A.S.-E., M.A., N.V., and A.B. performed experiments and analyzed the data. D.P.K. developed and provided the TRE-PGC-1α mice and reviewed the manuscript. F.T. developed and provided the GR floxed mice and reviewed the manuscript. P.F. and J.-F.G. reviewed the manuscript. B.Br. and B.Bl. designed the stud ies, and wrote, reviewed and edited the manuscript. B.Bl. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank Delphine Dorchene (INSERM, Paris, France) for mouse husbandry, Caroline Peschard (INSERM, Paris, France), Isabelle Hainault (INSERM, Paris, France), and Adriana Rodriguez-Trejo (Universidad Nacional Autónoma de México, Mexico City, Mexico) for technical assistance, and the Centre d’Imagerie Cellulaire et Cytometrie of UMRS 872 (INSERM, Paris, France). The authors thank Domonique Langin (INSERM, Toulouse, France) and Raphael Scharfmann (INSERM, Paris, France) for sharing reagents and Eric Ravussin (Pennington Biomedical Research Center, Baton Rouge, LA) and Catherine Postic (INSERM, Paris, France) for helpful advice.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db12-0314/-/DC1
REFERENCES
- 1.Calkins K, Devaskar SU. Fetal origins of adult disease. Curr Probl Pediatr Adolesc Health Care 2011;41:158–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia 1993;36:62–67 [DOI] [PubMed] [Google Scholar]
- 3.Hales CN, Barker DJ, Clark PM, et al. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ 1991;303:1019–1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lithell HO, McKeigue PM, Berglund L, Mohsen R, Lithell UB, Leon DA. Relation of size at birth to non-insulin dependent diabetes and insulin concentrations in men aged 50-60 years. BMJ 1996;312:406–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phipps K, Barker DJ, Hales CN, Fall CH, Osmond C, Clark PM. Fetal growth and impaired glucose tolerance in men and women. Diabetologia 1993;36:225–228 [DOI] [PubMed] [Google Scholar]
- 6.Blondeau B, Lesage J, Czernichow P, Dupouy JP, Bréant B. Glucocorticoids impair fetal beta-cell development in rats. Am J Physiol Endocrinol Metab 2001;281:E592–E599 [DOI] [PubMed] [Google Scholar]
- 7.Garofano A, Czernichow P, Bréant B. Effect of ageing on beta-cell mass and function in rats malnourished during the perinatal period. Diabetologia 1999;42:711–718 [DOI] [PubMed] [Google Scholar]
- 8.Valtat B, Dupuis C, Zenaty D, et al. Genetic evidence of the programming of beta cell mass and function by glucocorticoids in mice. Diabetologia 2011;54:350–359 [DOI] [PubMed] [Google Scholar]
- 9.Reinisch JM, Simon NG, Karow WG, Gandelman R. Prenatal exposure to prednisone in humans and animals retards intrauterine growth. Science 1978;202:436–438 [DOI] [PubMed] [Google Scholar]
- 10.Entringer S, Buss C, Wadhwa PD. Prenatal stress and developmental programming of human health and disease risk: concepts and integration of empirical findings. Curr Opin Endocrinol Diabetes Obes 2010;17:507–516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stoffers DA, Zinkin NT, Stanojevic V, Clarke WL, Habener JF. Pancreatic agenesis attributable to a single nucleotide deletion in the human IPF1 gene coding sequence. Nat Genet 1997;15:106–110 [DOI] [PubMed] [Google Scholar]
- 12.Jonsson J, Carlsson L, Edlund T, Edlund H. Insulin-promoter-factor 1 is required for pancreas development in mice. Nature 1994;371:606–609 [DOI] [PubMed] [Google Scholar]
- 13.Macfarlane WM, Frayling TM, Ellard S, et al. Missense mutations in the insulin promoter factor-1 gene predispose to type 2 diabetes. J Clin Invest 1999;104:R33–R39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stoffers DA, Stanojevic V, Habener JF. Insulin promoter factor-1 gene mutation linked to early-onset type 2 diabetes mellitus directs expression of a dominant negative isoprotein. J Clin Invest 1998;102:232–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Offield MF, Jetton TL, Labosky PA, et al. PDX-1 is required for pancreatic outgrowth and differentiation of the rostral duodenum. Development 1996;122:983–995 [DOI] [PubMed] [Google Scholar]
- 16.Tronche F, Kellendonk C, Reichardt HM, Schütz G. Genetic dissection of glucocorticoid receptor function in mice. Curr Opin Genet Dev 1998;8:532–538 [DOI] [PubMed] [Google Scholar]
- 17.Puigserver P, Spiegelman BM. Peroxisome proliferator-activated receptor-gamma coactivator 1 alpha (PGC-1 alpha): transcriptional coactivator and metabolic regulator. Endocr Rev 2003;24:78–90 [DOI] [PubMed] [Google Scholar]
- 18.Yoon JC, Puigserver P, Chen G, et al. Control of hepatic gluconeogenesis through the transcriptional coactivator PGC-1. Nature 2001;413:131–138 [DOI] [PubMed] [Google Scholar]
- 19.Yoon JC, Xu G, Deeney JT, et al. Suppression of beta cell energy metabolism and insulin release by PGC-1alpha. Dev Cell 2003;5:73–83 [DOI] [PubMed] [Google Scholar]
- 20.Hellerström CH, Lewis NJ, Borg H, Johnson R, Fréinkel N. Method for large-scale isolation of pancreatic islets by tissue culture of fetal rat pancreas. Diabetes 1979;28:769–776 [DOI] [PubMed] [Google Scholar]
- 21.Miyazaki J, Araki K, Yamato E, et al. Establishment of a pancreatic beta cell line that retains glucose-inducible insulin secretion: special reference to expression of glucose transporter isoforms. Endocrinology 1990;127:126–132 [DOI] [PubMed] [Google Scholar]
- 22.Tiraby C, Langin D. Conversion from white to brown adipocytes: a strategy for the control of fat mass? Trends Endocrinol Metab 2003;14:439–441 [DOI] [PubMed] [Google Scholar]
- 23.Gesina E, Tronche F, Herrera P, et al. Dissecting the role of glucocorticoids on pancreas development. Diabetes 2004;53:2322–2329 [DOI] [PubMed] [Google Scholar]
- 24.Blondeau B, Sahly I, Massouridès E, et al. Novel transgenic mice for inducible gene overexpression in pancreatic cells define glucocorticoid receptor-mediated regulations of beta cells. PLoS ONE 2012;7:e30210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Russell LK, Mansfield CM, Lehman JJ, et al. Cardiac-specific induction of the transcriptional coactivator peroxisome proliferator-activated receptor gamma coactivator-1alpha promotes mitochondrial biogenesis and reversible cardiomyopathy in a developmental stage-dependent manner. Circ Res 2004;94:525–533 [DOI] [PubMed] [Google Scholar]
- 26.Phillips DI, Hirst S, Clark PM, Hales CN, Osmond C. Fetal growth and insulin secretion in adult life. Diabetologia 1994;37:592–596 [DOI] [PubMed] [Google Scholar]
- 27.Phan-Hug F, Guimiot F, Lelièvre V, et al. Potential role of glucocorticoid signaling in the formation of pancreatic islets in the human fetus. Pediatr Res 2008;64:346–351 [DOI] [PubMed] [Google Scholar]
- 28.Macfarlane WM, Cragg H, Docherty HM, et al. Impaired expression of transcription factor IUF1 in a pancreatic beta-cell line derived from a patient with persistent hyperinsulinaemic hypoglycaemia of infancy (nesidioblastosis). FEBS Lett 1997;413:304–308 [DOI] [PubMed] [Google Scholar]
- 29.Petersen HV, Peshavaria M, Pedersen AA, et al. Glucose stimulates the activation domain potential of the PDX-1 homeodomain transcription factor. FEBS Lett 1998;431:362–366 [DOI] [PubMed] [Google Scholar]
- 30.Brissova M, Shiota M, Nicholson WE, et al. Reduction in pancreatic transcription factor PDX-1 impairs glucose-stimulated insulin secretion. J Biol Chem 2002;277:11225–11232 [DOI] [PubMed] [Google Scholar]
- 31.Kulkarni RN, Jhala US, Winnay JN, Krajewski S, Montminy M, Kahn CR. PDX-1 haploinsufficiency limits the compensatory islet hyperplasia that occurs in response to insulin resistance. J Clin Invest 2004;114:828–836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bréant B, Gesina E, Blondeau B. Nutrition, glucocorticoids and pancreas development. Horm Res 2006;65(Suppl. 3):98–104 [DOI] [PubMed] [Google Scholar]
- 33.Nasir I, Kedees MH, Ehrlich ME, Teitelman G. The role of pregnancy hormones in the regulation of Pdx-1 expression. Mol Cell Endocrinol 2005;233:1–13 [DOI] [PubMed] [Google Scholar]
- 34.Sharma S, Jhala US, Johnson T, Ferreri K, Leonard J, Montminy M. Hormonal regulation of an islet-specific enhancer in the pancreatic homeobox gene STF-1. Mol Cell Biol 1997;17:2598–2604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Truss M, Beato M. Steroid hormone receptors: interaction with deoxyribonucleic acid and transcription factors. Endocr Rev 1993;14:459–479 [DOI] [PubMed] [Google Scholar]
- 36.Gerrish K, Van Velkinburgh JC, Stein R. Conserved transcriptional regulatory domains of the pdx-1 gene. Mol Endocrinol 2004;18:533–548 [DOI] [PubMed] [Google Scholar]
- 37.Goodman PA, Medina-Martinez O, Fernandez-Mejia C. Identification of the human insulin negative regulatory element as a negative glucocorticoid response element. Mol Cell Endocrinol 1996;120:139–146 [DOI] [PubMed] [Google Scholar]
- 38.Knutti D, Kaul A, Kralli A. A tissue-specific coactivator of steroid receptors, identified in a functional genetic screen. Mol Cell Biol 2000;20:2411–2422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Handschin C, Spiegelman BM. Peroxisome proliferator-activated receptor gamma coactivator 1 coactivators, energy homeostasis, and metabolism. Endocr Rev 2006;27:728–735 [DOI] [PubMed] [Google Scholar]
- 40.Jang WG, Kim EJ, Park KG, et al. Glucocorticoid receptor mediated repression of human insulin gene expression is regulated by PGC-1alpha. Biochem Biophys Res Commun 2007;352:716–721 [DOI] [PubMed] [Google Scholar]
- 41.Kim JW, Sun C, Jeon SY, et al. Glucocorticoid treatment independently affects expansion and transdifferentiation of porcine neonatal pancreas cell clusters. BMB Rep 2012;45:51–56 [DOI] [PubMed] [Google Scholar]
- 42.Kim JW, You YH, Ham DS, et al. Suppression of peroxisome proliferator-activated receptor gamma-coactivator-1alpha normalizes the glucolipotoxicity-induced decreased BETA2/NeuroD gene transcription and improved glucose tolerance in diabetic rats. Endocrinology 2009;150:4074–4083 [DOI] [PubMed] [Google Scholar]
- 43.Yu IT, Lee SH, Lee YS, Son H. Differential effects of corticosterone and dexamethasone on hippocampal neurogenesis in vitro. Biochem Biophys Res Commun 2004;317:484–490 [DOI] [PubMed] [Google Scholar]
- 44.Shao J, Qiao L, Friedman JE. Prolactin, progesterone, and dexamethasone coordinately and adversely regulate glucokinase and cAMP/PDE cascades in MIN6 beta-cells. Am J Physiol Endocrinol Metab 2004;286:E304–E310 [DOI] [PubMed] [Google Scholar]
- 45.Kim HI, Kim JW, Kim SH, Cha JY, Kim KS, Ahn YH. Identification and functional characterization of the peroxisomal proliferator response element in rat GLUT2 promoter. Diabetes 2000;49:1517–1524 [DOI] [PubMed] [Google Scholar]
- 46.Oberkofler H, Klein K, Felder TK, Krempler F, Patsch W. Role of peroxisome proliferator-activated receptor-gamma coactivator-1alpha in the transcriptional regulation of the human uncoupling protein 2 gene in INS-1E cells. Endocrinology 2006;147:966–976 [DOI] [PubMed] [Google Scholar]
- 47.Giordano E, Cirulli V, Bosco D, Rouiller D, Halban P, Meda P. B-cell size influences glucose-stimulated insulin secretion. Am J Physiol 1993;265:C358–C364 [DOI] [PubMed] [Google Scholar]
- 48.Pende M, Kozma SC, Jaquet M, et al. Hypoinsulinaemia, glucose intolerance and diminished beta-cell size in S6K1-deficient mice. Nature 2000;408:994–997 [DOI] [PubMed] [Google Scholar]
- 49.Granot Z, Swisa A, Magenheim J, et al. LKB1 regulates pancreatic beta cell size, polarity, and function. Cell Metab 2009;10:296–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marciniak B, Patro-Małysza J, Poniedziałek-Czajkowska E, Kimber-Trojnar Z, Leszczyńska-Gorzelak B, Oleszczuk J. Glucocorticoids in pregnancy. Curr Pharm Biotechnol 2011;12:750–757 [DOI] [PubMed] [Google Scholar]
- 51.Liu C, Li S, Liu T, Borjigin J, Lin JD. Transcriptional coactivator PGC-1alpha integrates the mammalian clock and energy metabolism. Nature 2007;447:477–481 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.