Abstract
BRCA1-associated breast and ovarian cancer risks can be modified by common genetic variants. To identify further cancer risk-modifying loci, we performed a multi-stage GWAS of 11,705 BRCA1 carriers (of whom 5,920 were diagnosed with breast and 1,839 were diagnosed with ovarian cancer), with a further replication in an additional sample of 2,646 BRCA1 carriers. We identified a novel breast cancer risk modifier locus at 1q32 for BRCA1 carriers (rs2290854, P = 2.7×10−8, HR = 1.14, 95% CI: 1.09–1.20). In addition, we identified two novel ovarian cancer risk modifier loci: 17q21.31 (rs17631303, P = 1.4×10−8, HR = 1.27, 95% CI: 1.17–1.38) and 4q32.3 (rs4691139, P = 3.4×10−8, HR = 1.20, 95% CI: 1.17–1.38). The 4q32.3 locus was not associated with ovarian cancer risk in the general population or BRCA2 carriers, suggesting a BRCA1-specific association. The 17q21.31 locus was also associated with ovarian cancer risk in 8,211 BRCA2 carriers (P = 2×10−4). These loci may lead to an improved understanding of the etiology of breast and ovarian tumors in BRCA1 carriers. Based on the joint distribution of the known BRCA1 breast cancer risk-modifying loci, we estimated that the breast cancer lifetime risks for the 5% of BRCA1 carriers at lowest risk are 28%–50% compared to 81%–100% for the 5% at highest risk. Similarly, based on the known ovarian cancer risk-modifying loci, the 5% of BRCA1 carriers at lowest risk have an estimated lifetime risk of developing ovarian cancer of 28% or lower, whereas the 5% at highest risk will have a risk of 63% or higher. Such differences in risk may have important implications for risk prediction and clinical management for BRCA1 carriers.
Author Summary
BRCA1 mutation carriers have increased and variable risks of breast and ovarian cancer. To identify modifiers of breast and ovarian cancer risk in this population, a multi-stage GWAS of 14,351 BRCA1 mutation carriers was performed. Loci 1q32 and TCF7L2 at 10q25.3 were associated with breast cancer risk, and two loci at 4q32.2 and 17q21.31 were associated with ovarian cancer risk. The 4q32.3 ovarian cancer locus was not associated with ovarian cancer risk in the general population or in BRCA2 carriers and is the first indication of a BRCA1-specific risk locus for either breast or ovarian cancer. Furthermore, modeling the influence of these modifiers on cumulative risk of breast and ovarian cancer in BRCA1 mutation carriers for the first time showed that a wide range of individual absolute risks of each cancer can be estimated. These differences suggest that genetic risk modifiers may be incorporated into the clinical management of BRCA1 mutation carriers.
Introduction
Breast and ovarian cancer risk estimates for BRCA1 mutation carriers vary by the degree of family history of the disease, suggesting that other genetic factors modify cancer risks for this population [1]–[4]. Studies by the Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA) have shown that a subset of common alleles influencing breast and ovarian cancer risk in the general population are also associated with cancer risk in BRCA1 mutation carriers [5]–[11]. In particular, the breast cancer associations were limited to loci associated with estrogen receptor (ER)-negative breast cancer in the general population (6q25.1, 12p11 and TOX3) [8]–[11].
To systematically search for loci associated with breast or ovarian cancer risk for BRCA1 carriers we previously conducted a two-stage genome-wide association study (GWAS) [12]. The initial stage involved analysis of 555,616 SNPs in 2383 BRCA1 mutation carriers (1,193 unaffected and 1,190 affected). After replication testing of 89 SNPs showing the strongest association, with 5,986 BRCA1 mutation carriers, a locus on 19p13 was shown to be associated with breast cancer risk for BRCA1 mutation carriers. The same locus was also associated with the risk of estrogen-receptor (ER) negative and triple negative (ER, Progesterone and HER2 negative) breast cancer in the general population [12], [13].
The Collaborative Oncological Gene-environment Study (COGS) consortium recently developed a 211,155 SNP custom genotyping array (iCOGS) in order to provide cost-effective genotyping of common and rare genetic variants to identify novel loci that explain the residual genetic variance of breast, ovarian and prostate cancers and fine-map known susceptibility loci. A total of 32,557 SNPs on the iCOGS array were selected on the basis of the BRCA1 GWAS for the purpose of identifying breast and ovarian cancer risk modifiers for BRCA1 mutation carriers. Genotype data from the iCOGS array were obtained for 11,705 samples from BRCA1 carriers and the 17 most promising SNPs were then genotyped in an additional 2,646 BRCA1 carriers. In this manuscript we report on the novel risk modifier loci identified by this multi-stage GWAS. No study has previously shown how the absolute risks of breast and ovarian cancer for BRCA1 mutation carriers vary by the combined effects of risk modifying loci. Here we use the results from this study, in combination with previously identified modifiers, to obtain absolute risks of developing breast and ovarian cancer for BRCA1 mutation carriers based on the joint distribution of all known genetic risk modifiers.
Materials and Methods
Ethics statement
All carriers participated in clinical or research studies at the host institutions, approved by local ethics committees.
Study subjects
BRCA1 mutation carriers were recruited by 45 study centers in 25 countries through CIMBA. The majority were recruited through cancer genetics clinics, and enrolled into national or regional studies. The remainder were identified by population-based sampling or community recruitment. Eligibility for CIMBA association studies was restricted to female carriers of pathogenic BRCA1 mutations age 18 years or older at recruitment. Information collected included year of birth, mutation description, self-reported ethnic ancestry, age at last follow-up, ages at breast or ovarian cancer diagnoses, and age at bilateral prophylactic mastectomy and oophorectomy. Information on tumour characteristics, including ER-status of the breast cancers, was also collected. Related individuals were identified through a unique family identifier. Women were included in the analysis if they carried mutations that were pathogenic according to generally recognized criteria.
GWAS stage 1 samples
A total of 2,727 BRCA1 mutation carriers were genotyped on the Illumina Infinium 610K array (Figure 1). Of these 1,426 diagnosed with a first breast cancer under age 40 were considered “affected” in the breast cancer association analysis and 683 diagnosed with an ovarian cancer at any time were considered as “affected” in the ovarian cancer analysis. “Unaffected” in both analyses were over age 35 (Table S1) [12].
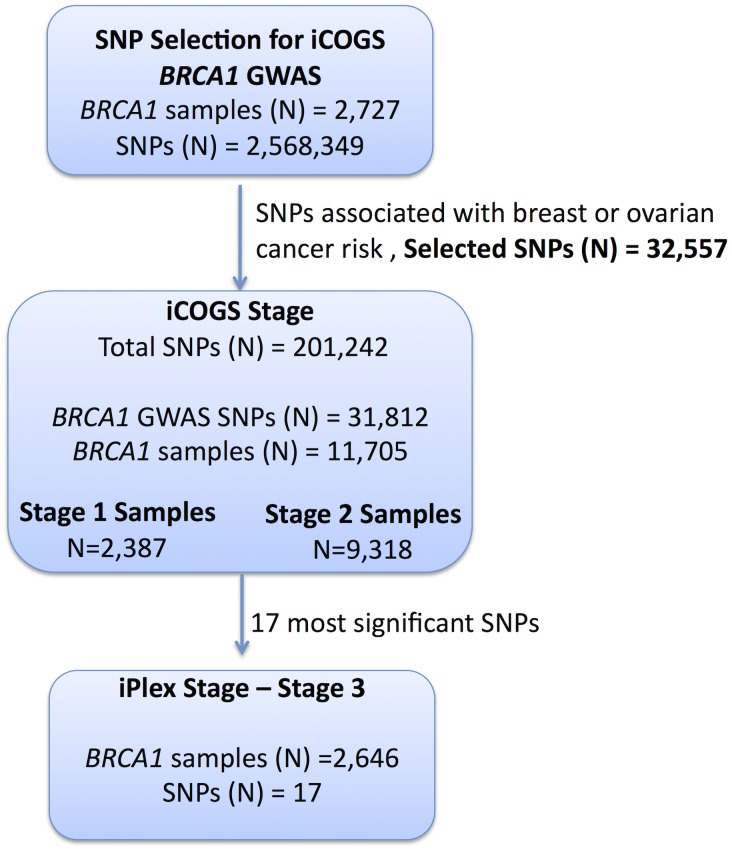
Figure 1. Study design for selection of the SNPs and genotyping of BRCA1 samples.
GWAS data from 2,727 BRCA1 mutation carriers were analysed for associations with breast and ovarian cancer risk and 32,557 SNPs were selected for inclusion on the iCOGS array. A total of 11,705 BRCA1 samples (after quality control (QC) checks) were genotyped on the 31,812 BRCA1-GWAS SNPs from the iCOGS array that passed QC. Of these samples, 2,387 had been genotyped at the SNP selection stage and are referred to as “stage 1” samples, whereas 9,318 samples were unique to the iCOGS study (“Stage 2” samples). Next, 17 SNPs that exhibited the most significant associations with breast and ovarian cancer were selected for genotyping in a third stage involving an additional 2,646 BRCA1 samples (after QC).
Replication study samples
All eligible BRCA1 carriers from CIMBA with sufficient DNA were genotyped, including those used in Stage 1. In total, 13,310 samples from 45 centers in 25 countries were genotyped using the iCOGS array (Table S2). Among the 13,310 samples, those that were genotyped in the GWAS stage 1 SNP selection stage are referred to as “stage 1” samples, and the remainder are “stage 2” samples. An additional 2,646 BRCA1 samples “stage 3” were genotyped on an iPLEX Mass Array of 17 SNPs from 12 loci selected after an interim analysis of iCOGS array data and were available for analysis after quality control (QC) (Figure 1). Carriers of pathogenic mutations in BRCA2 were drawn from a parallel GWAS of genetic modifiers for BRCA2 mutation carriers. BRCA2 mutation carriers were recruited from CIMBA through 47 studies which were largely the same as the studies that contributed to the BRCA1 GWAS with similar eligibility criteria. Samples from BRCA2 mutation carriers were also genotyped using the iCOGS array. Details of this experiment are described elsewhere [14]. A total of 8,211 samples were available for analysis after QC.
iCOGS SNP array
The iCOGS array was designed in a collaboration among the Breast Cancer Association Consortium (BCAC), Ovarian Cancer Association Consortium (OCAC), the Prostate Cancer Association Group to Investigate Cancer Associated Alterations in the Genome (PRACTICAL) and CIMBA. The general aims for designing the iCOGS array were to replicate findings from GWAS for identifying variants associated with breast, ovarian or prostate cancer (including subtypes and SNPs potentially associated with disease outcome), to facilitate fine-mapping of regions of interest, and to genotype “candidate” SNPs of interest within the consortia, including rarer variants. Each consortium was given a share of the array: nominally 25% of the SNPs each for BCAC, PRACTICAL and OCAC; 17.5% for CIMBA; and 7.5% for SNPs of common interest between the consortia. The final design comprised 220,123 SNPs, of which 211,155 were successfully manufactured. A total of 32,557 SNPs on the iCOGS array were selected based on 8 separate analyses of stage 1 of the CIMBA BRCA1 GWAS that included 2,727 BRCA1 mutation carriers [12]. After imputation for all SNPs in HapMap Phase II (CEU) a total of 2,568,349 (imputation r2>0.30) were available for analysis. Markers were evaluated for associations with: (1) breast cancer; (2) ovarian cancer; (3) breast cancer restricted to Class 1 mutations (loss-of-function mutations expected to result in a reduced transcript or protein level due to nonsense-mediated RNA decay); (4) breast cancer restricted to Class 2 mutations (mutations likely to generate stable proteins with potential residual or dominant negative function); (5) breast cancer by tumor ER-status; (6) breast cancer restricted to BRCA1 185delAG mutation carriers; (7) breast cancer restricted to BRCA1 5382insC mutation carriers; and (8) breast cancer by contrasting the genotype distributions in BRCA1 mutation carriers, against the distribution in population-based controls. Analyses (1) and (2) were based on both imputed and observed genotypes, whereas the rest were based on only the observed genotypes. SNPs were ranked according to the 1 d.f. score-test for trend P-value (described below) and selected for inclusion based on nominal proportions of 61.5%, 20%, 2.5%, 2.5%, 2.5%, 0.5%, 0.5% and 10.0% for analyses (1) to (8). SNP duplications were not allowed and SNPs with a pairwise r2≥0.90 with a higher-ranking SNP were only allowed (up to a maximum of 2) if the P-value for association was <10−4 for analyses (1) and (2) and <10−5 for other analyses. SNPs with poor Illumina design scores were replaced by the SNP with the highest r2 (among SNPs with r2>0.80 based on HapMap data) that had a good quality design score. The analysis of associations with breast and ovarian cancer risks presented here included all 32,557 SNPs on iCOGS that were selected on the basis of the BRCA1 GWAS.
Genotyping and quality control
iCOGS genotyping
Genotyping was performed at Mayo Clinic. Genotypes for samples genotyped on the iCOGS array were called using Illumina's GenCall algorithm (Text S1). A total of 13,510 samples were genotyped for 211,155 SNPs. The sample and SNP QC process is summarised in Table S3. Of the 13,510 samples, 578 did not fulfil eligibility criteria based on phenotypic data and were excluded. A step-wise QC process was applied to the remaining samples and SNPs. Samples were excluded due to inferred gender errors, low call rates (<95%), low or high heterozygosity and sample duplications (cryptic and intended). Of the 211,155 markers genotyped, 9,913 were excluded due to Y-chromosome origin, low call rates (<95%), monomorphic SNPs, or SNPs with Hardy-Weinberg equilibrium (HWE) P<10−7 under a country-stratified test statistic [15] (Table S3). SNPs that gave discordant genotypes among known sample duplicates were also excluded. Multi-dimensional scaling was used to exclude individuals of non-European ancestry. We selected 37,149 weakly correlated autosomal SNPs (pair-wise r2<0.10) to compute the genomic kinship between all pairs of BRCA1 carriers, along with 197 HapMap samples (CHB, JPT, YRI and CEU). These were converted to distances and subjected to multidimensional scaling (Figure S1). Using the first two components, we calculated the proportion of European ancestry for each individual [12] and excluded samples with >22% non-European ancestry (Figure S1). A total of 11,705 samples and 201,242 SNPs were available for analysis, including 31,812 SNPs selected by the BRCA1 GWAS. The genotyping cluster plots for all SNPs that demonstrated genome-wide significance level of association or are presented below, were checked manually for quality (Figure S2).
iPLEX analysis
The most significant SNPs from 4 loci associated with ovarian cancer and 8 loci associated with breast cancer were selected (17 SNPs in total) for stage 3 genotyping. Genotyping using the iPLEX Mass Array platform was performed at Mayo Clinic. CIMBA QC procedures were applied. Samples that failed for ≥20% of the SNPs were excluded from the analysis. No SNPs failed HWE (P<0.01). The concordance among duplicates was ≥98%. Mutation carriers of self-reported non-European ancestry were excluded. A total of 2,646 BRCA1 samples were eligible for analysis after QC.
Statistical methods
The main analyses were focused on the evaluation of associations between each genotype and breast cancer or ovarian cancer risk separately. Analyses were carried out within a survival analysis framework. In the breast cancer analysis, the phenotype of each individual was defined by age at breast cancer diagnosis or age at last follow-up. Individuals were followed until the age of the first breast cancer diagnosis, ovarian cancer diagnosis, or bilateral prophylactic mastectomy, whichever occurred first; or last observation age. Mutation carriers censored at ovarian cancer diagnosis were considered unaffected. For the ovarian cancer analysis, the primary endpoint was the age at ovarian cancer diagnosis. Mutation carriers were followed until the age of ovarian cancer diagnosis, or risk-reducing salpingo-oophorectomy (RRSO) or age at last observation. In order to maximize the number of ovarian cancer cases, breast cancer was not considered as a censoring event in this analysis, and mutation carriers who developed ovarian cancer after a breast cancer diagnosis were considered as affected in the ovarian cancer analysis.
Association analysis
The majority of mutation carriers were sampled through families seen in genetic clinics. The first tested individual in a family is usually someone diagnosed with cancer at a relatively young age. Such study designs tend to lead to an over-sampling of affected individuals, and standard analytical methods like Cox regression may lead to biased estimates of the risk ratios [16], [17]. To adjust for this potential bias the data were analyzed within a survival analysis framework, by modeling the retrospective likelihood of the observed genotypes conditional on the disease phenotypes. A detailed description of the retrospective likelihood approach has been published [17], [18]. The associations between genotype and breast cancer risk at both stages were assessed using the 1 d.f. score test statistic based on this retrospective likelihood [17], [18]. To allow for the non-independence among related individuals, we accounted for the correlation between the genotypes by estimating the kinship coefficient for each pair of individuals using the available genomic data [16], [19], [20] and by robust variance estimation based on reported family membership [21]. We chose to present P-values based on the kinship adjusted score test as it utilises the degree of relationship between individuals. A genome-wide level of significance of 5×10−8 was used [22]. These analyses were performed in R using the GenABEL [23] libraries and custom-written functions in FORTRAN and Python.
To estimate the magnitude of the associations (HRs), the effect of each SNP was modeled either as a per-allele HR (multiplicative model) or as genotype-specific HRs, and were estimated on the log-scale by maximizing the retrospective likelihood. The retrospective likelihood was fitted using the pedigree-analysis software MENDEL [17], [24]. As sample sizes varied substantially between contributing centers heterogeneity was examined at the country level. All analyses were stratified by country of residence and used calendar-year and cohort-specific breast cancer incidence rates for BRCA1 [25]. Countries with small number of mutation carriers were combined with neighbouring countries to ensure sufficiently large numbers within each stratum (Table S2). USA and Canada were further stratified by reported Ashkenazi Jewish (AJ) ancestry due to large numbers of AJ carriers. In stage 3 analysis involving several countries with small numbers of mutation carriers, we assumed only 3 large strata (Europe, Australia, USA/Canada). The combined iCOGS stage and stage 3 analysis was also stratified by stage of the experiment. The analysis of associations by breast cancer ER-status was carried out by an extension of the retrospective likelihood approach to model the simultaneous effect of each SNP on more than one tumor subtype [26] (Text S1).
Competing risk analysis
The associations with breast and ovarian cancer risk simultaneously were assessed within a competing risk analysis framework [17] by estimating HRs simultaneously for breast and ovarian cancer risk. This analysis provides unbiased estimates of association with both diseases and more powerful tests of association in cases where an association exists between a variant and at least one of the diseases [17]. Each individual was assumed to be at risk of developing either breast or ovarian cancer, and the probabilities of developing each disease were assumed to be independent conditional on the underlying genotype. A different censoring process was used, whereby individuals were followed up to the age of the first breast or ovarian cancer diagnosis and were considered to have developed the corresponding disease. No follow-up was considered after the first cancer diagnosis. Individuals censored for breast cancer at the age of bilateral prophylactic mastectomy and for ovarian cancer at the age of RRSO were assumed to be unaffected for the corresponding disease. The remaining individuals were censored at the last observation age and were assumed to be unaffected for both diseases.
Imputation
For the SNP selection process, the MACH software was used to impute non-genotyped SNPs based on the phased haplotypes from HapMap Phase II (CEU, release 22). The IMPUTE2 software [27] was used to impute non-genotyped SNPs for samples genotyped on the iCOGS array (stage 1 and 2 only), based on the 1,000 Genomes haplotypes (January 2012 version). Associations between each marker and cancer risk were assessed using a similar score test to that used for the observed SNPs, but based on the posterior genotype probabilities at each imputed marker for each individual. In all analyses, we considered only SNPs with imputation information/accuracy r2>0.30.
Absolute breast and ovarian cancer risks by combined SNP profile
We estimated the absolute risk of developing breast and ovarian cancer based on the joint distribution of all SNPs that were significantly associated with risk for BRCA1 mutation carriers based on methods previously applied to BRCA2 carriers [28]. We assumed that the average, age-specific breast and ovarian cancer incidences for BRCA1 mutation carriers, over all modifying loci, agreed with published penetrance estimates for BRCA1 [25]. The model assumed independence among the modifying loci and we used only the SNP with the strongest evidence of association from each region. We used only loci identified through the BRCA1 GWAS that exhibited associations at a genome-wide significance level, and loci that were identified through population-based GWAS of breast or ovarian cancer risk, but were also associated with those risks for BRCA1 mutation carriers. For each SNP, we used the per-allele HR and minor allele frequencies estimated from the present study. Genotype frequencies were obtained under the assumption of HWE.
Results
Samples from 11,705 BRCA1 carriers from 45 centers in 25 countries yielded high-quality data for 201,242 SNPs on the iCOGS array. The array included 31,812 BRCA1 GWAS SNPs, which were analyzed here for their associations with breast and ovarian cancer risk for BRCA1 mutation carriers (Table S2). Of the 11,705 BRCA1 mutation carriers, 2,387 samples had also been genotyped for stage 1 of the GWAS and 9,318 were unique to the stage 2 iCOGS study.
Breast cancer associations
When restricting analysis to stage 2 samples (4,681 unaffected, 4,637 affected), there was little evidence of inflation in the association test-statistic (λ = 1.038; Figure S3). Combined analysis of stage 1 and 2 samples (5,784 unaffected, 5,920 affected) revealed 66 SNPs in 28 regions with P<10−4 (Figure S4). These included variants from three loci (19p13, 6q25.1, 12p11) previously associated with breast cancer risk for BRCA1 mutation carriers (Table 1). Further evaluation of 18 loci associated with breast cancer susceptibility in the general population found that only the TOX3, LSP1, 2q35 and RAD51L1 loci were significantly associated with breast cancer for BRCA1 carriers (Table 1, Table S4).
Table 1. Associations with breast or ovarian cancer risk for loci previously reported to be associated with cancer risk for BRCA1 mutation carriers.
| Locus | Previously published association in BRCA1 | Strongest association in current set of 31,812 BRCA1 GWAS SNPs | Association for published SNP in set of all iCOGS SNPs | ||||||||||
| SNP | all1/all2 (freq) | HR (95%CI) | P | SNP | all1/all2 (freq) | r2 | HR (95%CI) | P | Best tag SNP (r2) | all1/all2 (freq) | HR (95%CI) | P | |
| Loci previously associated with breast cancer risk for BRCA1 carriers | |||||||||||||
| 19p13 | rs8170 | G/A (0.17) | 1.26 (1.17–1.35) | 2.3×10−9 | rs8100241 | G/A (0.52) | 0.31 | 0.84 (0.80–0.88) | 4.3×10−13 | rs8170 (1.0) | G/A (0.17) | 1.22 (1.14–1.29) | 4.8×10−10 |
| 6q25.1 | rs2046210 | C/T (0.35) | 1.17 (1.11–1.23) | 4.5×10−9 | rs3734805 | A/C (0.08) | 0.25 | 1.28 (1.18–1.39) | 5×10−9 | rs2046210* (1.0) | G/A (0.35) | 1.15 (1.10–1.21) | 2.8×10−8 |
| 12p11 | rs10771399 | A/G (0.11) | 0.87 (0.81–0.94) | 3.2×10−4 | rs7957915 | A/G (0.14) | 0.85 | 0.85 (0.79–0.91) | 8.1×10−6 | rs10771399* | A/G (0.11) | 0.85 (0.79–0.92) | 2.7×10−5 |
| TOX3 | rs3803662 | C/T (0.29) | 1.09 (1.03–1.16) | 0.0049 | rs4784220 | A/G (0.38) | 0.52 | 1.08 (1.03–1.13) | 0.0021 | rs3803662* | G/A (0.29) | 1.05 (1.00–1.11) | 0.075 |
| 2q35 | rs13387042a | G/A (0.52) | 1.02 (0.96–1.07) | 0.57 | rs13389571 | A/G (0.05) | 0.02 | 0.86 (0.77–0.96) | 0.011 | rs13387042* | A/G (0.48) | 1.01 (0.96–1.06) | 0.74 |
| Known ovarian cancer susceptibility loci | |||||||||||||
| 9p22 | rs3814113 | T/C (0.34) | 0.78 (0.72–0.85) | 4.8×10−9 | rs3814113 | A/G (0.34) | 1.00 | 0.77 (0.71–0.83) | 5.9×10−11 | rs3814113 (1.0) | A/G (0.34) | 0.77 (0.71–0.83) | 5.9×10−11 |
| 2q31 | rs2072590 | T/C (0.31) | 1.06 (0.98–1.14) | 0.16 | rs1026032 | A/G (0.26) | 0.75 | 1.08 (0.99–1.17) | 0.064 | rs2072590* (1.0) | C/A (0.32) | 1.05 (0.97–1.14) | 0.20 |
| 8q24 | rs10088218 | G/A (0.13) | 0.89 (0.81–0.99) | 0.029 | rs9918771 | A/C (0.17) | 0.31 | 0.86 (0.78–0.95) | 0.0021 | rs10088218 (1.0) | G/A (0.13) | 0.86 (0.78–0.96) | 0.0096 |
| 3q25 | rs2665390 | T/C (0.075) | 1.25 (1.10–1.42) | 2.7×10−3 | rs7651446 | C/A (0.043) | 0.71 | 1.46 (1.25–1.71) | 6.6×10−6 | rs344008 (1.0) | G/A (0.075) | 1.21 (1.07–1.38) | 3.8×10−3 |
| 17q21 | rs9303542 | T/C (0.26) | 1.08 (1.00–1.17) | 0.06 | rs11651753 | G/A (0.43) | 0.36 | 1.14 (1.06–1.23) | 4.6×10−4 | rs9303542* (1.0) | A/G (0.26) | 1.12 (1.04–1.22) | 8.0×10−3 |
| 19p13b | rs67397200 | C/G (0.28) | 1.16 (1.05–1.29) | 3.8×10−4 | c19_pos17158477 | G/C (0.038) | 0.01 | 0.64 (0.49–0.83) | 7.0×10−4 | rs67397200 (c19_pos17262404) | G/C (0.28) | 1.12 (1.01–1.23) | 0.027 |
Freq = frequency of allele 2 in unaffected BRCA1 carriers.
HR = Per allele Hazard Ratio associated with allele 2, under a single disease risk model, unless specified.
r2: correlation between the SNP in the present study and the published SNP.
SNP not in BRCA1 GWAS SNP allocation on iCOGS chip.
: rs13387042 was previously found to be associated only under the 2-df model.
: analysis under a competing risks model.
After excluding SNPs from the known loci, there were 39 SNPs in 25 regions with P = 1.2×10−6–1.0×10−4. Twelve of these SNPs were genotyped by iPLEX in an additional 2,646 BRCA1 carriers (1,252 unaffected, 1,394 affected, “stage 3” samples, Table S5). There was additional evidence of association with breast cancer risk for four SNPs at two loci (P<0.01, Table 2). When all stages were combined, SNPs rs2290854 and rs6682208 (r2 = 0.84) at 1q32, near MDM4, had combined P-values of association with breast cancer risk of 1.4×10−7 and 4×10−7,respectively. SNPs rs11196174 and rs11196175 (r2 = 0.96) at 10q25.3 (in TCF7L2) had combined P-values of 7.5×10−7 and 1.2×10−6. Analysis within a competing risks framework, where associations with breast and ovarian cancer risks are evaluated simultaneously [17], revealed stronger associations with breast cancer risk for all 4 SNPs, but no associations with ovarian cancer (Table 3). In particular, we observed a genome-wide significant association between the minor allele of rs2290854 from 1q32 and breast cancer risk (per-allele HR: 1.14; 95%CI: 1.09–1.20; p = 2.7×10−8). Country-specific HR estimates for all SNPs are shown in Figure S5. Analyses stratified by BRCA1 mutation class revealed no significant evidence of a difference in the associations of any of the SNPs by the predicted functional consequences of BRCA1 mutations (Table S6). SNPs in the MDM4 and TCF7L2 loci were associated with breast cancer risk for both class1 and class2 mutation carriers.
Table 2. Associations with breast and ovarian cancer risk for SNPs found to be associated with risk at all 3 stages of the experiment.
| SNP, Chr, Position, Allele1/Allele2 | Stage | Number | Allele 2 Frequency | HR* (95% CI) | |||||
| Unaffected | Affected | Unaffected | Affected | Per Allele | Heterozygote | Homozygote | P-trend | ||
| Breast Cancer | |||||||||
| rs2290854, 1q32, 202782648, G/A | Stage 1 | 1104 | 1283 | 0.30 | 0.34 | 1.19 (1.08–1.30) | 1.28 (1.12–1.47) | 1.31 (1.06–1.61) | 4.2×10−4 |
| Stage 2 | 4681 | 4637 | 0.31 | 0.33 | 1.09 (1.03–1.16) | 1.10 (1.02–1.19) | 1.18 (1.03–1.35) | 0.003 | |
| Stages1+2 | 5785 | 5920 | 0.31 | 0.33 | 1.12 (1.06–1.17) | 1.15 (1.07–1.23) | 1.21 (1.08–1.36) | 1.7×10−5 | |
| Stage 3 | 1252 | 1393 | 0.30 | 0.33 | 1.19 (1.07–1.32) | 1.24 (1.07–1.43) | 1.36 (1.06–1.74) | 0.0013 | |
| Combined | 7037 | 7313 | 0.31 | 0.33 | 1.13 (1.08–1.18) | 1.16 (1.09–1.24) | 1.24 (1.11–1.37) | 1.4×10−7 | |
| rs6682208, 1q32, 202832806, G/A | Stage 1 | 1104 | 1283 | 0.32 | 0.35 | 1.14 (1.04–1.25) | 1.24 (1.09–1.42) | 1.20 (0.98–1.47) | 0.0070 |
| Stage 2 | 4681 | 4637 | 0.32 | 0.34 | 1.10 (1.04–1.17) | 1.09 (1.01–1.19) | 1.21 (1.06–1.38) | 0.0014 | |
| Stages1+2 | 5785 | 5920 | 0.32 | 0.34 | 1.11 (1.05–1.17) | 1.13 (1.05–1.21) | 1.21 (1.08–1.35) | 5.4×10−5 | |
| Stage 3 | 1250 | 1394 | 0.30 | 0.34 | 1.19 (1.07–1.32) | 1.31 (1.14–1.51) | 1.28 (1.01–1.63) | 8.6×10−4 | |
| Combined | 7035 | 7314 | 0.32 | 0.34 | 1.12 (1.07–1.17) | 1.16 (1.09–1.23) | 1.22 (1.11–1.35) | 4.3×10−7 | |
| rs11196174, 10q25.3, 114724086, A/G | Stage 1 | 1103 | 1282 | 0.27 | 0.32 | 1.15 (1.05–1.27) | 1.17 (1.03–1.34) | 1.31 (1.05–1.63) | 0.0038 |
| Stage 2 | 4681 | 4636 | 0.29 | 0.31 | 1.10 (1.04–1.17) | 1.13 (1.04–1.23) | 1.17 (1.01–1.35) | 0.0017 | |
| Stages1+2 | 5784 | 5918 | 0.28 | 0.31 | 1.12 (1.06–1.18) | 1.14 (1.06–1.23) | 1.21 (1.07–1.37) | 3.1×10−5 | |
| Stage 3 | 1251 | 1393 | 0.28 | 0.31 | 1.16 (1.05–1.29) | 1.08 (0.93–1.25) | 1.46 (1.15–1.85) | 0.0057 | |
| Combined | 7035 | 7311 | 0.28 | 0.31 | 1.13 (1.07–1.18) | 1.13 (1.06–1.21) | 1.26 (1.13–1.40) | 7.5×10−7 | |
| rs11196175, 10q25.3, 114726604, A/G | Stage 1 | 1101 | 1280 | 0.27 | 0.31 | 1.15 (1.05–1.27) | 1.18 (1.03–1.35) | 1.29 (1.03–1.62) | 0.0043 |
| Stage 2 | 4674 | 4627 | 0.28 | 0.30 | 1.10 (1.03–1.17) | 1.13 (1.04–1.22) | 1.17 (1.01–1.35) | 0.0020 | |
| Stages1+2 | 5775 | 5907 | 0.28 | 0.30 | 1.12 (1.06–1.18) | 1.14 (1.06–1.22) | 1.21 (1.07–1.37) | 3.9×10−5 | |
| Stage 3 | 1251 | 1394 | 0.27 | 0.31 | 1.16 (1.04–1.29) | 1.06 (0.91–1.22) | 1.48 (1.17–1.87) | 0.0075 | |
| Combined | 7026 | 7301 | 0.28 | 0.31 | 1.12 (1.07–1.18) | 1.12 (1.05–1.20) | 1.26 (1.13–1.41) | 1.2×10−6 | |
| Ovarian Cancer | |||||||||
| rs17631303, 17q21, 40872185, A/G | Stage 1 | 1797 | 574 | 0.19 | 0.25 | 1.46 (1.22–1.74) | 1.36 (1.01–1.68) | 2.46 (1.53–3.96) | 1.3×10−5 |
| Stage 2 | 7996 | 1257 | 0.19 | 0.21 | 1.20 (1.07–1.35) | 1.10 (0.96–1.26) | 1.83 (1.34–2.48) | 1.5×10−3 | |
| Stages1+2 | 9793 | 1831 | 0.19 | 0.22 | 1.27 (1.16–1.40) | 1.15 (1.03–1.29) | 2.03 (1.16–2.61) | 3.0×10−7 | |
| Stage 3 | 2204 | 442 | 0.17 | 0.21 | 1.27 (1.07–1.51) | 1.24 (0.99–1.56) | 1.67 (1.07–2.62) | 0.014 | |
| Combined | 11997 | 2273 | 0.19 | 0.22 | 1.27 (1.17–1.38) | 1.17 (1.06–1.29) | 1.95 (1.57–2.42) | 1.4×10−8 | |
| rs183211, 17q21, 42143493, G/A | Stage 1 | 1812 | 575 | 0.22 | 0.28 | 1.45 (1.23–1.71) | 1.37 (1.11–1.69) | 2.29 (1.53–3.41) | 2.5×10−5 |
| Stage 2 | 8054 | 1264 | 0.23 | 0.25 | 1.20 (1.07–1.33) | 1.13 (0.99–1.28) | 1.62 (1.22–2.14) | 1.1×10−3 | |
| Stages1+2 | 9866 | 1839 | 0.23 | 0.26 | 1.25 (1.15–1.37) | 1.16 (1.04–1.29) | 1.83 (1.46–2.28) | 5.7×10−7 | |
| Stage 3 | 2204 | 442 | 0.22 | 0.26 | 1.25 (1.06–1.48) | 1.15 (0.92–1.44) | 1.79 (1.21–2.67) | 0.018 | |
| Combined | 12070 | 2281 | 0.23 | 0.26 | 1.25 (1.16–1.35) | 1.16 (1.05–1.27) | 1.82 (1.5–2.21) | 3.1×10−8 | |
| rs4691139, 4q32.3, 166128171, A/G | Stage 1 | 1812 | 575 | 0.47 | 0.53 | 1.24 (1.08–1.42) | 1.46 (1.13–1.88) | 1.55 (1.16–2.05) | 3.6×10−3 |
| Stage 2 | 8054 | 1264 | 0.48 | 0.52 | 1.18 (1.08–1.29) | 1.29 (1.10–1.50) | 1.40 (1.17–1.67) | 1.3×10−4 | |
| Stages1+2 | 9866 | 1839 | 0.48 | 0.52 | 1.20 (1.11–1.29) | 1.33 (1.17–1.52) | 1.44 (1.24–1.67) | 1.1×10−6 | |
| Stage 3 | 2204 | 441 | 0.47 | 0.52 | 1.20 (1.04–1.39) | 1.19 (0.91–1.54) | 1.44 (1.08–1.94) | 9×10−3 | |
| Combined | 12070 | 2280 | 0.48 | 0.52 | 1.20 (1.17–1.38) | 1.30 (1.16–1.46) | 1.44 (1.26–1.65) | 3.4×10−8 | |
HRs estimated under the single disease risk models.
Table 3. Analysis of associations with breast and ovarian cancer risk simultaneously (competing risks analysis) for SNPs found to be associated with breast or ovarian cancer.
| SNP, Chr, Position, Allele1/Allele2 | Unaffected (Allele2 Freq) | Ovarian Cancer (Allele2 Freq) | Breast Cancer (Allele2 Freq) | Ovarian Cancer | Breast Cancer | ||
| HR (95% CI) | P | HR (95% CI) | P | ||||
| SNPs found to be associated with breast cancer risk. | |||||||
| rs2290854, 1q32, 202782648, G/A | 5473 (0.31) | 1618 (0.31) | 7259 (0.33) | 1.08 (0.99–1.18) | 0.08 | 1.14 (1.09–1.20) | 2.7×10−8 |
| rs6682208, 1q32, 202832806, G/A | 5471 (0.32) | 1618 (0.33) | 7260 (0.34) | 1.08 (1.00–1.18) | 0.06 | 1.13 (1.08–1.19) | 1.2×10−7 |
| rs11196174, 10q25.3, 114724086, A/G | 5471 (0.28) | 1618 (0.29) | 7257 (0.31) | 1.07 (0.98–1.16) | 0.16 | 1.14 (1.08–1.19) | 3.2×10−7 |
| rs11196175, 10q25.3, 114726604, A/G | 5465 (0.28) | 1615 (0.29) | 7247 (0.31) | 1.07 (0.97–1.16) | 0.16 | 1.14 (1.08–1.19) | 3.9×10−7 |
| SNPs found to be associated with ovarian cancer risk | |||||||
| rs17631303, 17q21, 40872185, A/G | 5445 (0.19) | 1610 (0.22) | 7215 (0.19) | 1.26 (1.14–1.39) | 1.0×10−5 | 1.02 (0.96–1.08) | 0.52 |
| rs183211, 17q21, 42143493, G/A | 5473 (0.23) | 1618 (0.26) | 7260 (0.23) | 1.25 (1.14–1.38) | 3.5×10−6 | 1.02 (0.97–1.08) | 0.42 |
| rs4691139, 4q32.3, 166128171, A/G | 5473 (0.48) | 1617 (0.53) | 7269 (0.48) | 1.21 (1.12–1.31) | 2.8×10−6 | 0.98 (0.93–1.02) | 0.28 |
Both the 1q32 and 10q25.3 loci were primarily associated with ER-negative breast cancer for BRCA1 (rs2290854: ER-negative HR = 1.16, 95%CI: 1.10–1.22, P = 1.2×10−7; rs11196174: HR = 1.14, 95%CI: 1.07–1.20, P = 9.6×10−6), although the differences between the ER-negative and ER-positive HRs were not significant (Table S7). Given that ER-negative breast cancers in BRCA1 and BRCA2 mutation carriers are phenotypically similar [29], we also evaluated associations between these SNPs and ER-negative breast cancer in 8,211 BRCA2 mutation carriers. While the 10q25.3 SNPs were not associated with overall or ER-negative breast cancer risk for BRCA2 carriers, the 1q32 SNPs were associated with ER-negative (rs2290854 HR = 1.16, 95%CI:1.01–1.34, P = 0.033; rs6682208 HR = 1.19, 95%CI:1.04–1.35, P = 0.016), but not ER-positive breast cancer (rs2290854 P-diff = 0.006; rs6682208 P-diff = 0.001). Combining the BRCA1 and BRCA2 samples provided strong evidence of association with ER-negative breast cancer (rs2290854: P = 1.25×10−8; rs6682208: P = 2.5×10−7).
The iCOGS array included additional SNPs from the 1q32 region that were not chosen based on the BRCA1 GWAS. Of these non-BRCA1 GWAS SNPs, only SNP rs4951407 was more significantly associated with risk than the BRCA1-GWAS selected SNPs (P = 3.3×10−6, HR = 1.12, 95%CI:1.07–1.18, using stage 1 and stage 2 samples). The evidence of association with breast cancer risk was again stronger under the competing risks analysis (HR = 1.14, 95%CI: 1.08–1.20, P = 6.1×10−7). Backward multiple regression analysis, considering only the genotyped SNPs (P<0.01), revealed that the most parsimonious model included only rs4951407. SNPs from the 1000 Genomes Project, were imputed for the stage 1 and stage 2 samples (Figure S6). Only imputed SNP rs12404974, located between PIK3C2B and MDM4 (r2 = 0.77 with rs4951407), was more significantly associated with breast cancer (P = 2.7×10−6) than any of the genotyped SNPs. None of the genotyped or imputed SNPs from 10q25.3 provided P-values smaller than those for rs11196174 and rs11196175 (Figure S7).
Ovarian cancer associations
Analyses of associations with ovarian cancer risk using the stage 2 samples (8,054 unaffected, 1,264 affected) revealed no evidence of inflation in the association test-statistic (λ = 1.039, Figure S3). In the combined analysis of stage 1 and 2 samples (9866 unaffected, 1839 affected), 62 SNPs in 17 regions were associated with ovarian cancer risk for BRCA1 carriers at P<10−4 (Figure S3). These included SNPs in the 9p22 and 3q25 loci previously associated with ovarian cancer risk in both the general population and BRCA1 carriers [6], [7] (Table 1). Associations (P<0.01) with ovarian cancer risk were also observed for SNPs in three other known ovarian cancer susceptibility loci (8q24, 17q21, 19p13), but not 2q31 (Table 1). For all loci except 9p22, SNPs were identified that displayed smaller P-values of association than previously published results [5]–[7].
After excluding SNPs from known ovarian cancer susceptibility regions, there were 48 SNPs in 15 regions with P = 5×10−7 to 10−4. Five SNPs from four of these loci were genotyped in the stage 3 samples (2,204 unaffected, 442 with ovarian cancer). Three SNPs showed additional evidence of association with ovarian cancer risk (P<0.02, Table 2; Table S5). In the combined stage 1–3 analyses, SNPs rs17631303 and rs183211 (r2 = 0.68) on chromosome 17q21.31 had P-values for association of 1×10−8 and 3×10−8 respectively, and rs4691139 at 4q32.3 had a P-value of 3.4×10−8 (Table 2).
The minor alleles of rs17631303 (HR = 1.27, 95%CI:1.17–1.38) and rs183211 (HR = 1.25, 95%CI: 1.16–1.35) at 17q21.31 were associated with increased ovarian cancer risk (Table 2). Analysis of the associations within a competing risks framework, revealed no association with breast cancer risk (Table 3). The ovarian cancer effect size was maintained in the competing risk analysis but the significance of the association was slightly weaker (P = 2×10−6–1×10−5). This is expected because 663 ovarian cancer cases occurring after a primary breast cancer diagnosis were excluded for this analysis. The evidence of association was somewhat stronger under the genotype-specific model (2-df P = 1.6×10−9 and P = 2.6×10−9 for rs17631303 and rs183211 respectively in all samples combined) with larger HR estimates for the rare homozygote genotypes than those expected under a multiplicative model (Table 2).
Previous studies of the known common ovarian cancer susceptibility alleles found significant associations with ovarian cancer for both BRCA1 and BRCA2 carriers [6], [7]. Thus, we evaluated the associations between the 17q21.31 SNPs and ovarian cancer risk for BRCA2 carriers using iCOGS genotype data (7580 unaffected and 631 affected). Both rs17631303 and rs183211 were associated with ovarian cancer risk for BRCA2 carriers (P = 1.98×10−4 and 9.26×10−4), with similar magnitude and direction of association as for BRCA1 carriers. Combined analysis of BRCA1 and BRCA2 mutation carriers provided strong evidence of association (P = 2.80×10−10 and 2.01×10−9, Table 4).
Table 4. Associations with SNPs at the novel 17q21 region with ovarian cancer risk for BRCA1 and BRCA2 mutation carriers.
| SNP, Allele1/Allele2 | BRCA1 (Stage 1 & 2 samples) | BRCA2 | BRCA1 & BRCA2 samples combined | ||||||
| Unaffected (All2 freq) | Ovarian Cancer (All2 freq) | HR* (95%CI) | P-trend | Unaffected (All2 freq) | Ovarian Cancer (All2 freq) | HR* (95%CI) | P-trend | P-trend | |
| rs17631303, A/G | 9793 (0.19) | 1831 (0.22) | 1.27 (1.16–1.40) | 3.04×10−7 | 7481 (0.19) | 626 (0.24) | 1.32 (1.15–1.52) | 1.98×10−4 | 2.80×10−10 |
| rs2077606, G/A | 9736 (0.19) | 1810 (0.22) | 1.27 (1.15–1.40) | 5.51×10−7 | 7421 (0.19) | 613 (0.23) | 1.31 (1.13–1.50) | 5.60×10−4 | 1.27×10−9 |
| rs2532348, A/G | 9511 (0.21) | 1789 (0.24) | 1.25 (1.14–1.37) | 8.71×10−7 | 7407 (0.23) | 615 (0.28) | 1.33 (1.17–1.51) | 4.62×10−5 | 2.49×10−10 |
| rs183211, G/A | 9866 (0.23) | 1839 (0.26) | 1.25 (1.15–1.37) | 5.67×10−7 | 7580 (0.25) | 631 (0.30) | 1.26 (1.11–1.43) | 9.26×10−4 | 2.01×10−9 |
| rs169201, A/G | 9865 (0.20) | 1839 (0.23) | 1.27 (1.15–1.37) | 5.04×10−7 | 7578 (0.21) | 631 (0.26) | 1.36 (1.19–1.55) | 1.72×10−5 | 6.24×10−11 |
| rs199443, G/A | 9849 (0.20) | 1835 (0.23) | 1.26 (1.15–1.39) | 5.15×10−7 | 7580 (0.21) | 631 (0.26) | 1.35 (1.18–1.54) | 2.57×10−5 | 8.87×10−11 |
| rs199534, A/C | 9865 (0.20) | 1839 (0.23) | 1.26 (1.15–1.39) | 6.26×10−7 | 7575 (0.21) | 630 (0.26) | 1.35 (1.18–1.55) | 1.90×10−5 | 8.57×10−11 |
HRs estimated under the single disease risk model.
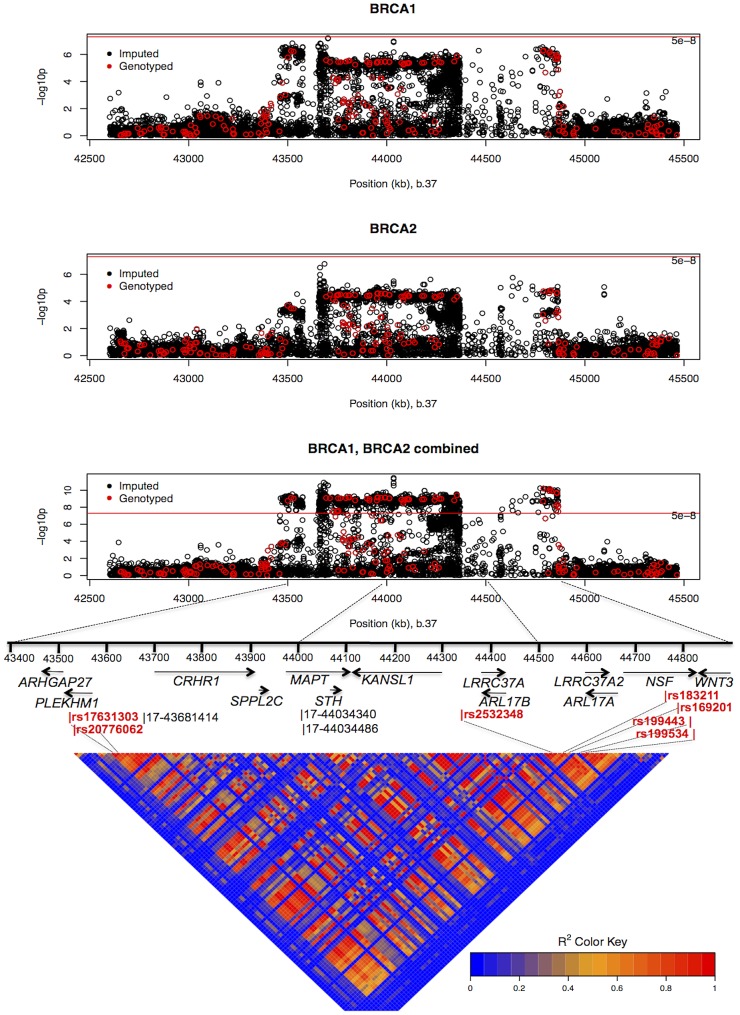
The combined analysis of stage 1 and 2 samples, and BRCA2 carriers, identified seven SNPs on the iCOGS array (pairwise r2 range: 0.68–1.00) from a 1.3 Mb (40.8–42.1 Mb, build 36.3) region of 17q21.31 that were strongly associated (P<1.27×10−9) with ovarian cancer risk (Table 4, Figure 2). Stepwise-regression analysis based on observed genotype data retained only one of the seven SNPs in the model, but it was not possible to distinguish between the SNPs. Imputation through the 1000 Genomes Project, revealed several SNPs in 17q21.31 with stronger associations (Figure 2, Table S8) than the most significant genotyped SNP in the combined BRCA1/2 analysis (rs169201, P = 6.24×10−11). The most significant SNP (rs140338099 (17-44034340), P = 3×10−12), located in MAPT, was highly correlated (r2 = 0.78) with rs169201 in NSF (Figure 2). This locus appears to be distinct from a previously identified ovarian cancer susceptibility locus located >1 Mb distal on 17q21 (spanning 43.3–44.3 Mb, build 36.3) [30]. None of the SNPs in the novel region were strongly correlated with any of the SNPs in the 43.3–44.3 Mb region (maximum r2 = 0.07, Figure S8). The most significantly associated SNP from the BRCA1 GWAS from the 43.3–44.3 Mb locus was rs11651753 (p = 4.6×10−4) (Table 1) (r2<0.023 with the seven most significant SNPs in the novel 17q21.31 region). An analysis of the joint associations of rs11651753 and rs17631303 from the two 17q21 loci with ovarian cancer risk for BRCA1 carriers (Stage 1 and 2 samples) revealed that both SNPs remained significant in the model (P-for inclusion = 0.001 for rs11651753, 1.2×10−6 for rs17631303), further suggesting that the two regions are independently associated with ovarian cancer for BRCA1 carriers.
Figure 2. Mapping of the 17q21 locus.
Top 3 panels: P-values of association (−log10 scale) with ovarian cancer risk for genotyped and imputed SNPs (1000 Genomes Project CEU), by chromosome position (b.37) at the 17q21 region, for BRCA1, BRCA2 mutation carriers and combined. Results based on the kinship-adjusted score test statistic (1 d.f.). Fourth panel: Genes in the region spanning (43.4–44.9 Mb, b.37) and the location of the most significant genotyped SNPs (in red font) and imputed SNPs (in black font). Bottom panel: Pairwise r2 values for genotyped SNPs on iCOG array in the 17q21 region covering positions (43.4–44.9 Mb, b.37).
The minor allele of rs4691139 at the novel 4q32.3 region was also associated with an increased ovarian cancer risk for BRCA1 carriers (per-allele HR = 1.20, 95%CI:1.17–1.38, Table 2), but was not associated with breast cancer risk (Table 3). No other SNPs from the 4q32.3 region on the iCOGS array were more significantly associated with ovarian cancer for BRCA1 carriers. Analysis of associations with variants identified through 1000 Genomes Project-based imputation of the Stage 1 and 2 samples, revealed 19 SNPs with stronger evidence of association (P = 5.4×10−7 to 1.1×10−6) than rs4691139 (Figure S9). All were highly correlated (pairwise r2>0.89) and the most significant (rs4588418) had r2 = 0.97 with rs4691139. There was no evidence for association between rs4691139 and ovarian cancer risk for BRCA2 carriers (HR = 1.08, 95%CI: 0.96–1.21, P = 0.22).
Absolute risks of developing breast and ovarian cancer
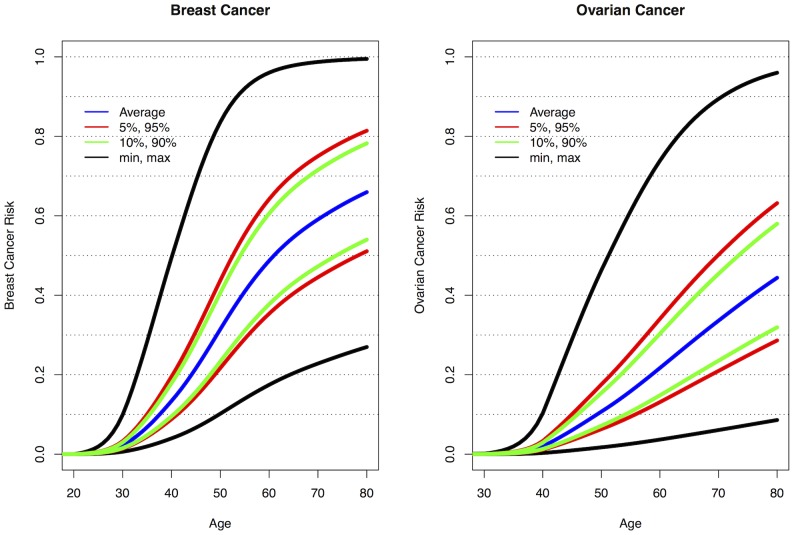
The current analyses suggest that 10 loci are now known to be associated with breast cancer risk for BRCA1 mutation carriers: 1q32, 10q25.3, 19p13, 6q25.1, 12p11, TOX3, 2q35, LSP1 and RAD51L1 all reported here and TERT [31]. Similarly, seven loci are associated with ovarian cancer risk for BRCA1 mutation carriers: 9p22, 8q24, 3q25, 17q21, 19p13, 17q21.31 and 4q32.3. Figure S10 shows the range of combined HRs at different percentiles of the combined genotype distribution, based on the single SNP HR and minor allele estimates from Table 1, Table 2, and Table S4 and for TERT from Bojesen et al [31] and assuming that all SNPs interact multiplicatively. Relative to BRCA1 mutation carriers at lowest risk, the median, 5th and 95th percentile breast cancer HRs were 3.40, 2.27, and 5.35 respectively. These translate to absolute risks of developing breast cancer by age 80 of 65%, 51% and 81% for those at median, 5th and 95th percentiles of the combined genotype distribution (Figure 3, Figure S10). Similarly, the median, 5th and 95th percentile combined HRs for ovarian cancer were 6.53, 3.75 and 11.12 respectively, relative to those at lowest ovarian cancer risk (Figure S10). These HRs translate to absolute risks of developing ovarian cancer of 44%, 28% and 63% by age 80 for the median, 5th and 95th percentile of the combined genotype distribution (Figure 3).
Figure 3. Predicted breast and ovarian cancer absolute risks for BRCA1 mutation carriers at the 5th, 10th, 90th, and 95th percentiles of the combined SNP profile distributions.
The minimum, maximum and average risks are also shown. Predicted cancer risks are based on the associations of known breast or ovarian cancer susceptibility loci (identified through GWAS) with cancer risk for BRCA1 mutation carriers and loci identified through the present study. Breast cancer risks based on the associations with: 1q32, 10q25.3, 19p13, 6q25.1, 12p11, TOX3, 2q35, LSP1, RAD51L1 (based on HR and minor allele frequency estimates from Table 1, Table 2, and Table S4) and TERT [31]. Ovarian cancer risks based on the associations with: 9p22, 8q24, 3q25, 17q21, 19p13 (Table 1) and 17q21.31, 4q32.3 (Table 2). Only the top SNP from each region was chosen. Average breast and ovarian cancer risks were obtained from published data [25]. The methods for calculating the predicted risks have been described previously [28].
Discussion
In this study we analyzed data from 11,705 BRCA1 mutation carriers from CIMBA who were genotyped using the iCOGS high-density custom array, which included 31,812 SNPs selected on the basis of a BRCA1 GWAS. This study forms the large-scale replication stage of the first GWAS of breast and ovarian cancer risk modifiers for BRCA1 mutation carriers. We have identified a novel locus at 1q32, containing the MDM4 oncogene, that is associated with breast cancer risk for BRCA1 mutation carriers (P<5×10−8). A separate locus at 10q23.5, containing the TCF7L2 gene, provided strong evidence of association with breast cancer risk for BRCA1 carriers but did not reach a GWAS level of significance. We have also identified two novel loci associated with ovarian cancer for BRCA1 mutation carriers at 17q21.31 and 4q32.2 (P<5×10−8). We further confirmed associations with loci previously shown to be associated with breast or ovarian cancer risk for BRCA1 mutation carriers. In most cases stronger associations were detected with either the same SNP reported previously (due to increased sample size) or other SNPs in the regions. Future fine mapping studies of these loci will aim to identify potentially causal variants for the observed associations.
Although the 10q25.3 locus did not reach the strict GWAS level of significance for association with breast cancer risk, the association was observed at all three independent stages of the experiment. Additional evidence for the involvement of this locus in breast cancer susceptibility comes from parallel studies of the Breast Cancer Association Consortium (BCAC). SNPs at 10q25.3 had also been independently selected for inclusion on the iCOGS array through population based GWAS of breast cancer. Analyses of those SNPs in BCAC iCOGS studies also found that SNPs at 10q25.3 were associated with breast cancer risk in the general population [32]. Thus, 10q25.3 is likely a breast cancer risk-modifying locus for BRCA1 mutation carriers. The most significant SNPs at 10q25.3 were located in TCF7L2, a transcription factor that plays a key role in the Wnt signaling pathway and in glucose homeostasis, and is expressed in normal and malignant breast tissue (The Cancer Genome Atlas (TCGA)). Variation in the TCF7L2 locus has previously been associated with Type 2 diabetes in a number of GWAS. The most significantly associated SNPs with Type 2 diabetes (rs7903146 and rs4506565) [22], [33] were also associated with breast cancer risk for BRCA1 mutation carriers in stage 1 and 2 analyses (p = 3.7×10−4 and p = 2.5×10−4 respectively); these SNPs were correlated with the most significant hit (rs11196174) for BRCA1 breast cancer (r2 = 0.40 and 0.37 based on stage 1 and 2 samples). This raises the possibility that variants in this locus influence breast cancer indirectly through effects on cellular metabolism.
We found that SNPs at 1q32 were primarily associated with ER-negative breast cancer risk for BRCA1 mutation carriers. There was also evidence of association with ER-negative breast cancer for BRCA2 mutation carriers. SNPs at the 1q32 region were independently selected for inclusion on iCOGS through GWAS of breast cancer in the general population by BCAC. In parallel analyses of iCOGS data by BCAC, 1q32 was found to be associated with ER-negative breast cancer [34] but not overall breast cancer risk [32]. Taken together, these results are in agreement with our findings and in line with the observation that the majority of BRCA1 breast cancers are ER-negative. However, they are not in agreement with a previous smaller candidate-gene study that found an association between a correlated SNP in MDM4 (r2>0.85) and overall breast cancer risk [35]. The 1q32 locus includes the MDM4 oncogene which plays a role in regulation of p53 and MDM2 and the apoptotic response to cell stress. MDM4 is expressed in breast tissue and is amplified and overexpressed along with LRRN2 and PIK3C2B in breast and other tumor types (TCGA) [36]–[38]. Although fine mapping will be necessary to identify the functionally relevant SNPs in this locus, we found evidence of cis-regulatory variation impacting MDM4 expression [39]–[41] (Text S1, Table S9, Figure S11), suggesting that common variation in the 1q32 locus may influence the risk of breast cancer through direct effects on MDM4 expression.
Several correlated SNPs at 17q21.31 from the iCOGS array provided strong evidence of association with ovarian cancer risk in both BRCA1 and BRCA2 mutation carriers. A subsequent analysis of these SNPs, which were selected through the BRCA1 GWAS, in case-control samples from the Ovarian Cancer Association Consortium (OCAC), revealed that the 17q21.31 locus is associated with ovarian cancer risk in the general population [Wey et al, personal communication]. Thus, 17q21.31 is likely a novel susceptibility locus for ovarian cancer in BRCA1 mutation carriers. The most significant associations at 17q21.31 were clustered in a large region of strong linkage disequilibrium which has previously been identified as a “17q21.31 inversion” (∼900 kb long) consisting of two haplotypes (termed H1 and H2) [42]. The minor allele of rs2532348 (MAF = 0.21), which tags H2, was associated with increased ovarian cancer risk for BRCA1 mutation carriers (Table 4). The 1.3 Mb 17q21.31 locus contains 13 genes and several predicted pseudogenes (Figure 2), several of which are expressed in normal ovarian surface epithelium and ovarian adenocarcinoma [43]. Variation in this region has been associated with Parkinson's disease (MAPT, PLEKHM1, NSF, c17orf69) progressive supranuclear palsy (MAPT), celiac disease (WNT3), bone mineral density (CRHR1) (NHGRI GWAS catalog) and intracranial volume [44]. Of the top hits for these phenotypes, SNP rs199533 in NSF, previously associated with Parkinson's disease [45] and rs9915547 associated with intracranial volume [44] were strongly associated with ovarian cancer (P<10−9 in BRCA1/2 combined). Whether these phenotypes have shared causal variants in this locus remains to be elucidated. Further exploration of the functional relevance of the strongest hits in the 17q21.31 locus (P<10−8 in BRCA1/2 combined) provided evidence that cis-regulatory variation alters expression of several genes at 17q21, including PLEKHM1, c17orf69, ARHGAP27, MAPT, KANSL1 and WNT3 [39], [41] (Table S9, Figure S12), suggesting that ovarian cancer risk may be associated with altered expression of one or more genes in this region.
Our analyses revealed that a second novel locus at 4q32.3 was also associated with ovarian cancer risk for BRCA1 mutation carries (P<5×10−8). However, we found no evidence of association for these SNPs with ovarian cancer risk for BRCA2 mutation carriers using 8,211 CIMBA samples genotyped using the iCOGS array. Likewise, no evidence of association was found between rs4691139 at 4q32.3 and ovarian cancer risk in the general population based on data by OCAC data derived from 18,174 cases and 26,134 controls (odds ratio = 1.00, 95%CI:0.97–1.04, P = 0.76) [46]. The confidence intervals rule out a comparable effect to that found in BRCA1 carriers. Therefore, our findings may represent a BRCA1-specific association with ovarian cancer risk, the first of its kind. The 4q32.2 region contains several members of the TRIM (Tripartite motif containing) gene family, c4orf39 and TMEM192. TRIM60, c4orf39 and TMEM192 are expressed in normal ovarian epithelium and/or ovarian tumors (TCGA).
In summary, we have identified a novel locus at 1q32 associated with breast cancer risk for BRCA1 mutation carriers, which was also associated with ER-negative breast cancer for BRCA2 carriers and in the general population. A separate locus at 10q23.5 provided strong evidence of association with breast cancer risk for BRCA1 carriers. We have also identified 2 novel loci associated with ovarian cancer for BRCA1 mutation carriers. Of these, the 4q32.2 locus was associated with ovarian cancer risk for BRCA1 carriers but not for BRCA2 carriers or in the general population. Additional functional characterisation of the loci will further improve our understanding of the biology of breast and ovarian cancer development in BRCA1 carriers. Taken together with other identified genetic modifiers, 10 loci are now known to be associated with breast cancer risk for BRCA1 mutation carriers (1q32, 10q25.3, 19p13, 6q25.1, 12p11, TOX3, 2q35, LSP1, RAD51L1 and TERT and seven loci are known to be associated with ovarian cancer risk for BRCA1 mutation carriers (9p22, 8q24, 3q25, 17q21, 19p13 and 17q21.31, 4q32.3).
As BRCA1 mutations confer high breast and ovarian cancer risks, the results from the present study, taken together with other identified genetic modifiers, demonstrate for the first time that they can result in large differences in the absolute risk of developing breast or ovarian cancer for BRCA1 between genotypes. For example, the breast cancer lifetime risks for the 5% of BRCA1 carriers at lowest risk are predicted to be 28–50% compared to 81–100% for the 5% at highest risk (Figure 3). Based on the distribution of ovarian cancer risk modifiers, the 5% of BRCA1 mutation carriers at lowest risk will have a lifetime risk of developing ovarian cancer of 28% or lower whereas the 5% at highest risk will have a lifetime risk of 63% or higher. Similarly, the breast cancer risk by age 40 is predicted to be 4–9% for the 5% of BRCA1 carriers at lowest risk compared to 20–49% for the 5% at highest risk, whereas the ovarian cancer risk at age 50 ranges from 3–7% for the 5% at lowest risk and from 18–47% for the 5% at highest risk. The risks at all ages for the 10% at highest or lowest risk of breast and ovarian cancer are predicted to be similar to those for the highest and lowest 5%. Thus, at least 20% of BRCA1 mutation carriers are predicted to have absolute risks of disease that are different from the average BRCA1 carriers. These large differences in cancer risks may have practical implications for the clinical management of BRCA1 mutation carriers, for example in deciding the timing of interventions. Such risks, in combination with other lifestyle and hormonal risk factors could be incorporated into cancer risk prediction algorithms for use by clinical genetics centers. These algorithms could then be used to inform the development of effective and consistent clinical recommendations for the clinical management of BRCA1 mutation carriers.
Supporting Information
Multidimensional scaling of stage 1 and stage 2 (genotyped on iCOGS) samples. Panel A: Graphical representation of the first two components, for the BRCA1 carriers, for subgroups defined by the common 185delAG (c.68_69delAG) BRCA1 Jewish founder mutation, the 5382insC (c.5266dupC) Eastern European founder mutation and Hapap individuals (CEU: European; ASI: Includes CHB and JPT populations; YRI: African). Panel B: Red dots represent the samples with >22% non-European ancestry, excluded from the analysis.
(PDF)
Genotyping cluster plots in the BRCA1 samples for the key associated SNPs.
(PDF)
Quantile-quantile plot for the kinship adjusted score test statistic for stage 2 samples (1 degree of freedom χ2 trend test) for the associations with breast cancer (panel A) and ovarian cancer (panel B) risk for BRCA1 mutation carriers. The y = x line corresponds to the expected distribution, under the hypothesis of no inflation. Inflation was estimated using the values of the lowest 90% test statistics.
(PDF)
P-values (on −log10 scale) by chromosomal position, for the associations of 31,812 BRCA1 GWAS SNPs with breast (panel A) and ovarian (panel B) cancer risk for BRCA1 mutation carriers in the combined stage 1 and stage 2 samples. Blue lines correspond to a P-value of 10−5; red lines correspond to P-value 5×10−8.
(PDF)
Forest plots of the associations by country of residence of BRCA1 mutation carriers in the combined stage 1, stage 2 and stage 3 samples for SNPs found to be associated with breast and ovarian cancer risk for BRCA1 mutation carriers. Squares indicate the country specific, per-allele HR estimates for the SNPs. The area of the square is proportional to the inverse of the variance of the estimate. Horizontal lines indicate 95% confidence intervals. There was some evidence of heterogeneity in country-specific HR estimates for the rs2290854 and rs6682208 SNP (P = 0.04 and 0.02 respectively, Figure S3), but after accounting for opposite effects of these SNPs in Finland/Denmark, there was no evidence of heterogeneity. There was some evidence of heterogeneity in the country-specific HRs for rs17631303 (P-het = 0.004, df = 19) but this was no longer present after excluding one country (Poland, P-het = 0.12, df = 18), or when restricting analyses to Stage 1 and 2 samples only (P-het = 0.09, df = 19). There was no evidence of heterogeneity for correlated SNP rs183211 (P-het = 0.10). There was no evidence of hereterogeneity in the country-specific HRs for any of the other SNPs (P>0.68).
(PDF)
MDM4 regional association plot using BRCA1 stage 1 and stage 2 samples. P-values for association (−log10 scale) with breast cancer risk for BRCA1 mutation carriers for genotyped SNPs (diamond symbols ◊) and SNPs imputed from the 1000 genomes project data (square symbols □), by position (hg18) on chromosome 1. Red gradient represents r2 value with the most significant genotyped SNP rs4951407. The blue peaks represent recombination rate in the region.
(PDF)
TCF7L2 regional association plot using BRCA1 stage 1 and stage 2 samples. P-values for association (−log10 scale) with breast cancer risk for BRCA1 mutation carriers for genotyped SNPs (diamond symbols ◊) and SNPs imputed from the 1000 genomes project data (square symbols □), by position (hg18) on chromosome 1. Missing genotypes were replaced by imputed results. Red gradient represents r2 value with the most significant genotyped SNP rs11196174. The blue peaks represent recombination rate in the region.
(PDF)
Linkage disequilibrium patterns between the SNPs in the novel (17q21.31) and previously identified regions on 17q21. SNPs in the novel region are uncorrelated with SNPs in the 43.3–44.3 Mb region (positions according to hg build 36.3).
(PDF)
4q32.3 regional association plot using BRCA1 stage 1 and stage 2 samples. P-values for association (−log10 scale) with ovarian cancer risk for BRCA1 mutation carriers for genotyped SNPs (diamond symbols ◊) and imputed SNPs from the 1000 genomes project data (square symbols □), by position (hg18) on chromosome 1. Red gradient represents r2 value with the most significant genotyped SNP rs4691139. Blue peaks represent recombination rate in the region.
(PDF)
Combined Hazard Ratios (HR) for breast and ovarian cancer for BRCA1 mutation carriers. (A) HR for Breast Cancer based on 10 loci associated with breast cancer risk for BRCA1 mutation carriers. (B) Ovarian Cancer based on 7 loci associated with ovarian cancer risk for BRCA1 mutation carriers. All HRs computed relative to the lowest risk category. The Y-axes translate the combined HRs into absolute risks of developing breast or ovarian cancer by age 80. The absolute risks and HRs at different percentiles of the combined genotype distribution are also marked. The combined HRs were obtained under the assumption that the loci interact multiplicatively.
(PDF)
Cis-eQTL and allelic expression (AE) analyses at MDM4 locus. A) Cis-eQTLs for SNPs at MDM4 locus using expression data from primary human osteoblasts (HOb). B) AE mapping for cis-regulatory variation in MDM4 locus using primary skin fibroblasts. Coordinates (hg18) for locus shown on top; blue tracks indicate the −log10(P value) of the association across all SNPs tested. The location of transcripts in this region is shown below.
(PDF)
Cis-eQTL and allelic expression (AE) analyses at chr17q21.31 locus. (Upper panel) Cis-eQTLs for SNPs at c17orf69 locus using expression data from primary human osteoblasts. Allelic expression mapping for cis-regulatory variation in KANSL1 (middle panel) and WNT3 loci (lower panel) using a CEU population panel of lymphoblastoid cells. Coordinates (hg18) for loci are shown on top; blue tracks indicate the −log10(P value) of the association across all SNPs tested. The location of transcripts in these regions are shown.
(PDF)
Affected and unaffected BRCA1 mutation carriers by study country in the breast and ovarian cancer analysis used in SNP selection for the iCOGS array.
(DOCX)
Origin of BRCA1 samples by Country and Stage used in the current analysis.
(DOCX)
Sample and SNP quality control summary.
(DOCX)
Associations with breast cancer risk for BRCA1 mutation carriers, for known breast cancer susceptibility variants.
(DOCX)
Associations with BRCA1 breast or ovarian cancer risk for SNPs genotyped at stages 1, 2, and 3.
(DOCX)
Analysis of breast cancer associations by BRCA1 mutation class.
(DOCX)
Associations with Breast Cancer ER status in BRCA1 carriers for SNPs genotyped in stages 1–3.
(DOCX)
Imputed SNPs at the novel 17q21 region with P-values less than the most significant genotyped SNP (rs169201).
(DOCX)
SNPs associated (P<1×10−5) with local expression and Allelic Imbalance.
(DOCX)
Supplementary Methods.
(DOCX)
Acknowledgments
Antonis C. Antoniou is a Cancer Research–UK Senior Cancer Research Fellow. Douglas F. Easton is a Cancer Research UK Principal Research Fellow. Georgia Chenevix-Trench is an NHMRC Senior Principal Research Fellow.
iCOGS: CIMBA acknowledges the contributions of Kyriaki Michailidou, Jonathan Tyrer, and Ali Amin Al Olama to the iCOGS statistical analyses; Shahana Ahmed, Melanie J. Maranian, and Catherine S. Healey for their contributions to the iCOGS genotyping quality control process; and the staff of the genotyping unit in the Medical Genomics Facility at the Mayo Clinic under the supervision of Dr. Julie Cunningham.
Breast Cancer Family Registry (BCFR) Studies: Samples from the NC-BCFR were processed and distributed by the Coriell Institute for Medical Research. We wish to thank members and participants in the Breast Cancer Family Registry for their contributions to the study. The ABCFS would like to also thank Maggie Angelakos, Judi Maskiell, and Gillian Dite. The content of this manuscript does not necessarily reflect the views or policies of the National Cancer Institute or any of the collaborating centers in the BCFR, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government or the BCFR.
Baltic Familial Breast Ovarian Cancer Consortium (BFBOCC): BFBOCC acknowledges Vilius Rudaitis and Laimonas Griškevičius. BFBOCC-LV acknowledges oncologists Janis Eglitis, Anna Krilova and Aivars Stengrevics.
BRCA-gene mutations and breast cancer in South African women (BMBSA): BMBSA thanks the families who contributed to the BMBSA study.
Beckman Research Institute of the City of Hope (BRICOH): BRICOH thanks Greg Wilhoite and Marie Pinto for their work in participant enrollment and biospecimen and data management.
Copenhagen Breast Cancer Study (CBCS): CBCS thanks the Danish Breast Cancer Cooperative Group (DBCG) for clinical data.
Spanish National Cancer Centre (CNIO): CNIO thanks Alicia Barroso, Rosario Alonso and Guillermo Pita for their assistance.
CONsorzio Studi ITaliani sui Tumori Ereditari Alla Mammella (CONSIT TEAM): CONSIT TEAM acknowledges Daniela Zaffaroni of the Fondazione IRCCS Istituto Nazionale Tumori (INT), Milan, Monica Barile of Istituto Europeo di Oncologia (IEO), Milan, Riccardo Dolcetti of the Centro di Riferimento Oncologico (CRO) IRCCS, Aviano (PN), Maurizio Genuardi of University of Florence, Florence, Giuseppe Giannini of “La Sapienza” University, Rome, Adele Patrini of the Ospedale di Circolo-Università dell'Insubria, Varese, Antonella Savarese and Aline Martayain of the Istituto Nazionale Tumori Regina Elena (IRE), Rome and Stefania Tommasi of the Istituto Nazionale Tumori “Giovanni Paolo II”, Bari and the personnel of the CGT-lab at IFOM-IEO Campus, Milan, Italy.
Dana-Farber Cancer Institute (DFCI): DFCI thanks the study staff and participants.
The Hereditary Breast and Ovarian Cancer Research Group Netherlands (HEBON): HEBON recognizes Netherlands Cancer Institute, Amsterdam, NL: M.A. Rookus, F.B.L. Hogervorst, S. Verhoef, F.E. van Leeuwen, M.K. Schmidt, J. de Lange; Erasmus Medical Center, Rotterdam, NL: J.M. Collée, A.M.W. van den Ouweland, M.J. Hooning, C. Seynaeve; Leiden University Medical Center, NL: C.J. van Asperen, J.T. Wijnen, R.A. Tollenaar, P. Devilee, T.C.T.E.F. van Cronenburg; Radboud University Nijmegen Medical Center, NL: C.M. Kets, A.R. Mensenkamp; University Medical Center Utrecht, NL: M.G.E.M. Ausems, R.B. van der Luijt; Amsterdam Medical Center, NL: C.M. Aalfs, T.A.M. van Os; VU University Medical Center, Amsterdam, NL: J.J.P. Gille, Q. Waisfisz, H.E.J. Meijers-Heijboer; University Hospital Maastricht, NL: E.B. Gómez-Garcia, M.J. Blok; University Medical Center Groningen, NL: J.C. Oosterwijk, H. van der Hout, M.J. Mourits, G.H. de Bock.
Epidemiological study of BRCA1 & BRCA2 mutation carriers (EMBRACE): Douglas F. Easton is the PI of the study. EMBRACE acknowledges the Coordinating Centre, Cambridge: Susan Peock, Debra Frost, Steve Ellis, Elena Fineberg, Radka Platte. North of Scotland Regional Genetics Service, Aberdeen: Zosia Miedzybrodzka, Helen Gregory. Northern Ireland Regional Genetics Service, Belfast: Patrick Morrison, Lisa Jeffers. West Midlands Regional Clinical Genetics Service, Birmingham: Trevor Cole, Kai-ren Ong, Jonathan Hoffman. South West Regional Genetics Service, Bristol: Alan Donaldson, Margaret James. East Anglian Regional Genetics Service, Cambridge: Marc Tischkowitz, Joan Paterson, Amy Taylor. Medical Genetics Services for Wales, Cardiff: Alexandra Murray, Mark T. Rogers, Emma McCann. St James's Hospital, Dublin & National Centre for Medical Genetics, Dublin: M. John Kennedy, David Barton. South East of Scotland Regional Genetics Service, Edinburgh: Mary Porteous, Sarah Drummond. Peninsula Clinical Genetics Service, Exeter: Carole Brewer, Emma Kivuva, Anne Searle, Selina Goodman, Kathryn Hill. West of Scotland Regional Genetics Service, Glasgow: Rosemarie Davidson, Victoria Murday, Nicola Bradshaw, Lesley Snadden, Mark Longmuir, Catherine Watt, Sarah Gibson, Eshika Haque, Ed Tobias, Alexis Duncan. South East Thames Regional Genetics Service, Guy's Hospital London: Louise Izatt, Chris Jacobs, Caroline Langman. North West Thames Regional Genetics Service, Harrow: Huw Dorkins, Angela Brady, Athalie Melville, Kashmir Randhawa. Leicestershire Clinical Genetics Service, Leicester: Julian Barwell. Yorkshire Regional Genetics Service, Leeds: Julian Adlard, Gemma Serra-Feliu. Cheshire & Merseyside Clinical Genetics Service, Liverpool: Ian Ellis, Catherine Houghton. Manchester Regional Genetics Service, Manchester: D Gareth Evans, Fiona Lalloo, Jane Taylor. North East Thames Regional Genetics Service, NE Thames, London: Lucy Side, Alison Male, Cheryl Berlin. Nottingham Centre for Medical Genetics, Nottingham: Jacqueline Eason, Rebecca Collier. Northern Clinical Genetics Service, Newcastle: Fiona Douglas, Oonagh Claber, Irene Jobson. Oxford Regional Genetics Service, Oxford: Lisa Walker, Diane McLeod, Dorothy Halliday, Sarah Durell, Barbara Stayner. The Institute of Cancer Research and Royal Marsden NHS Foundation Trust: Rosalind A. Eeles, Susan Shanley, Nazneen Rahman, Richard Houlston, Astrid Stormorken, Elizabeth Bancroft, Elizabeth Page, Audrey Ardern-Jones, Kelly Kohut, Jennifer Wiggins, Elena Castro, Emma Killick, Sue Martin, Gillian Rea, Anjana Kulkarni. North Trent Clinical Genetics Service, Sheffield: Jackie Cook, Oliver Quarrell, Cathryn Bardsley. South West Thames Regional Genetics Service, London: Shirley Hodgson, Sheila Goff, Glen Brice, Lizzie Winchester, Charlotte Eddy, Vishakha Tripathi, Virginia Attard, Anna Lehmann. Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton: Diana Eccles, Anneke Lucassen, Gillian Crawford, Donna McBride, Sarah Smalley.
Fox Chase Cancer Canter (FCCC): FCCC thanks Dr. Betsy Bove for her technical support.
German Consortium of Hereditary Breast and Ovarian Cancer (GC-HBOC): GC-HBOC thanks all family members who participated in this study, Wolfram Heinritz, Center Leipzig, and Dieter Schäfer, Center Frankfurt, for providing DNA samples and Juliane Köhler for excellent technical assistance.
Genetic Modifiers of Cancer Risk in BRCA1/2 Mutation Carriers (GEMO): GEMO thanks all the GEMO collaborating groups for their contribution to this study. GEMO Collaborating Centers are: Coordinating Centres, Unité Mixte de Génétique Constitutionnelle des Cancers Fréquents, Hospices Civils de Lyon - Centre Léon Bérard, & Equipe «Génétique du cancer du sein», Centre de Recherche en Cancérologie de Lyon: Olga Sinilnikova, Sylvie Mazoyer, Francesca Damiola, Laure Barjhoux, Carole Verny-Pierre, Sophie Giraud, Mélanie Léone; and Service de Génétique Oncologique, Institut Curie, Paris: Dominique Stoppa-Lyonnet, Marion Gauthier-Villars, Bruno Buecher, Claude Houdayer, Virginie Moncoutier, Muriel Belotti, Carole Tirapo, Antoine de Pauw. Institut Gustave Roussy, Villejuif: Brigitte Bressac-de-Paillerets, Olivier Caron. Centre Jean Perrin, Clermont–Ferrand: Yves-Jean Bignon, Nancy Uhrhammer. Centre Léon Bérard, Lyon: Christine Lasset, Valérie Bonadona, Sandrine Handallou. Centre François Baclesse, Caen: Agnès Hardouin, Pascaline Berthet. Institut Paoli Calmettes, Marseille: Hagay Sobol, Violaine Bourdon, Tetsuro Noguchi, Audrey Remenieras, François Eisinger. CHU Arnaud-de-Villeneuve, Montpellier: Isabelle Coupier, Pascal Pujol. Centre Oscar Lambret, Lille: Jean-Philippe Peyrat, Joëlle Fournier, Françoise Révillion, Philippe Vennin, Claude Adenis. Hôpital René Huguenin/Institut Curie, St Cloud: Etienne Rouleau, Rosette Lidereau, Liliane Demange, Catherine Nogues. Centre Paul Strauss, Strasbourg: Danièle Muller, Jean-Pierre Fricker. Institut Bergonié, Bordeaux: Emmanuelle Barouk-Simonet, Françoise Bonnet, Virginie Bubien, Nicolas Sevenet, Michel Longy. Institut Claudius Regaud, Toulouse: Christine Toulas, Rosine Guimbaud, Laurence Gladieff, Viviane Feillel. CHU Grenoble: Dominique Leroux, Hélène Dreyfus, Christine Rebischung, Magalie Peysselon. CHU Dijon: Fanny Coron, Laurence Faivre. CHU St-Etienne: Fabienne Prieur, Marine Lebrun, Caroline Kientz. Hôtel Dieu Centre Hospitalier, Chambéry: Sandra Fert Ferrer. Centre Antoine Lacassagne, Nice: Marc Frénay. CHU Limoges: Laurence Vénat-Bouvet. CHU Nantes: Capucine Delnatte. CHU Bretonneau, Tours: Isabelle Mortemousque. Groupe Hospitalier Pitié-Salpétrière, Paris: Florence Coulet, Chrystelle Colas, Florent Soubrier. CHU Vandoeuvre-les-Nancy : Johanna Sokolowska, Myriam Bronner. Creighton University, Omaha, USA: Henry T. Lynch, Carrie L. Snyder.
GFAST: G-FAST acknowledges the contribution of Bruce Poppe and Anne De Paepe and the technical support of Ilse Coene en Brecht Crombez.
Hospital Clinico San Carlos (HCSC): HCSC acknowledges Alicia Tosar for her technical assistance
Helsinki Breast Cancer Study (HEBCS): HEBCS thanks Carl Blomqvist, Kirsimari Aaltonen and RN Irja Erkkilä for their help with the HEBCS data and samples.
Study of Genetic Mutations in Breast and Ovarian Cancer patients in Hong Kong and Asia (HRBCP): HRBCP thanks Hong Kong Sanatoriuma and Hospital for their continual support.
Molecular Genetic Studies of Breast and Ovarian Cancer in Hungary (HUNBOCS): HUNBOCS thanks Hungarian Breast and Ovarian Cancer Study Group members (Janos Papp, Aniko Bozsik, Kristof Arvai, Judit Franko, Maria Balogh, Gabriella Varga, Judit Ferenczi, Department of Molecular Genetics, National Institute of Oncology, Budapest, Hungary) and the clinicians and patients for their contributions to this study.
INterdisciplinary HEalth Research Internal Team BReast CAncer susceptibility (INHERIT): INHERIT thanks Dr Martine Dumont, Martine Tranchant for sample management and skillful technical assistance. J.S. is Chairholder of the Canada Research Chair in Oncogenetics.
Kathleen Cuningham Consortium for Research into Familial Breast Cancer (kConFab): kConFab thanks Heather Thorne, Eveline Niedermayr, all the kConFab research nurses and staff, the heads and staff of the Family Cancer Clinics, and the Clinical Follow Up Study for their contributions to this resource, and the many families who contribute to kConFab.
Modifier Study of Quantitative Effects on Disease (MODSQUAD): MODSQUAD acknowledges ModSQuaD members Csilla Szabo and Zohra Ali-Kahn Catts (University of Delaware, Newark, USA); Lenka Foretova and Eva Machackova (Department of Cancer Epidemiology and Genetics, Masaryk Memorial Cancer Institute, Brno, Czech Republic); and Michal Zikan, Petr Pohlreich and Zdenek Kleibl (Oncogynecologic Center and Department of Biochemistry and Experimental Oncology, First Faculty of Medicine, Charles University, Prague, Czech Republic).
National Israeli Cancer Control Center (NICCC): NICCC thanks the NICCC National Familial Cancer Consultation Service team led by Sara Dishon, the laboratory team led by Dr. Flavio Lejbkowicz, and the research field operations team led by Dr. Mila Pinchev.
Ontario Cancer Genetics Network (OCGN): OCGN thanks the study staff and participants.
The Ohio State University Comprehensive Cancer Center (OSUCCG): OSU CCG acknowledges Kevin Sweet, Caroline Craven and Michelle O'Connor who were instrumental in accrual of study participants, ascertainment of medical records and database management. Samples were processed by the OSU Human Genetics Sample Bank.
South East Asian Breast Cancer Association Study (SEABASS): SEABASS thanks Yip Cheng Har, Nur Aishah Mohd Taib, Phuah Sze Yee, Norhashimah Hassan and all the research nurses, research assistants and doctors involved in the MyBrCa Study for assistance in patient recruitment, data collection and sample preparation. In addition, we thank Philip Iau, Sng Jen-Hwei and Sharifah Nor Akmal for contributing samples from the Singapore Breast Cancer Study and the HUKM-HKL Study respectively.
Sheba Medical Centre (SMC): SMC acknowledges the assistance of the Meirav Comprehensice breast cancer center team at the Sheba Medical Center for assistance in this study.
Swedish Breast Cancer Study (SWE-BRCA): SWE-BRCA Acknowledges SWE-BRCA collaborators from Lund University and University Hospital: Åke Borg, Håkan Olsson, Helena Jernström, Karin Henriksson, Katja Harbst, Maria Soller, Niklas Loman, Ulf Kristoffersson; Gothenburg Sahlgrenska University Hospital: Anna Öfverholm, Margareta Nordling, Per Karlsson, Zakaria Einbeigi; Stockholm and Karolinska University Hospital: Anna von Wachenfeldt, Annelie Liljegren, Annika Lindblom, Brita Arver, Gisela Barbany Bustinza, Johanna Rantala; Umeå University Hospital: Beatrice Melin, Christina Edwinsdotter Ardnor, Monica Emanuelsson; Uppsala University: Hans Ehrencrona, Maritta Hellström Pigg, Richard Rosenquist; Linköping University Hospital: Marie Stenmark-Askmalm, Sigrun Liedgren.
The University of Chicago Center for Clinical Cancer Genetics and Global Health (UCHICAGO): UCHICAGO thanks Cecilia Zvocec, Qun Niu, physicians, genetic counselors, research nurses and staff of the Cancer Risk Clinic for their contributions to this resource, and the many families who contribute to our program. OIO is an ACS Clinical Research Professor.
University of California Los Angeles (UCLA): UCLA thanks Joyce Seldon MSGC and Lorna Kwan, MPH for assembling the data for this study.
University of California San Francisco (UCSF): UCSF thanks Ms. Salina Chan for her data management and the following genetic counselors for participant recruitment: Beth Crawford, Nicola Stewart, Julie Mak, and Kate Lamvik.
United Kingdom Familial Ovarian Cancer Registries (UKFOCR): UKFOCR thanks Paul Pharoah, Simon Gayther, Carole Pye, Patricia Harrington and Eva Wozniak for their contributions towards the UKFOCR.
Victorian Familial Cancer Trials Group (VFCTG): VFCTG thanks Sarah Sawyer and Rebecca Driessen for assembling this data and Ella Thompson for performing all DNA amplification.
Funding Statement
The study was supported by NIH grant CA128978, an NCI Specialized Program of Research Excellence (SPORE) in Breast Cancer (CA116201), a U.S. Department of Defense Ovarian Cancer Idea award (W81XWH-10-1-0341), grants from the Breast Cancer Research Foundation and the Komen Foundation for the Cure; Cancer Research UK grants C12292/A11174 and C1287/A10118; the European Commission's Seventh Framework Programme grant agreement 223175 (HEALTH-F2-2009-223175). Breast Cancer Family Registry Studies (BCFR): supported by the National Cancer Institute, National Institutes of Health under RFA # CA-06-503 and through cooperative agreements with members of the Breast Cancer Family Registry (BCFR) and Principal Investigators, including Cancer Care Ontario (U01 CA69467), Cancer Prevention Institute of California (U01 CA69417), Columbia University (U01 CA69398), Fox Chase Cancer Center (U01 CA69631), Huntsman Cancer Institute (U01 CA69446), and University of Melbourne (U01 CA69638). The Australian BCFR was also supported by the National Health and Medical Research Council of Australia, the New South Wales Cancer Council, the Victorian Health Promotion Foundation (Australia), and the Victorian Breast Cancer Research Consortium. Melissa C. Southey is a NHMRC Senior Research Fellow and a Victorian Breast Cancer Research Consortium Group Leader. Carriers at FCCC were also identified with support from National Institutes of Health grants P01 CA16094 and R01 CA22435. The New York BCFR was also supported by National Institutes of Health grants P30 CA13696 and P30 ES009089. The Utah BCFR was also supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, NIH grant UL1 RR025764, and by Award Number P30 CA042014 from the National Cancer Institute. Baltic Familial Breast Ovarian Cancer Consortium (BFBOCC): BFBOCC is partly supported by Lithuania (BFBOCC-LT), Research Council of Lithuania grant LIG-19/2010, and Hereditary Cancer Association (Paveldimo vėžio asociacija). Latvia (BFBOCC-LV) is partly supported by LSC grant 10.0010.08 and in part by a grant from the ESF Nr.2009/0220/1DP/1.1.1.2.0/09/APIA/VIAA/016. BRCA-gene mutations and breast cancer in South African women (BMBSA): BMBSA was supported by grants from the Cancer Association of South Africa (CANSA) to Elizabeth J. van Rensburg. Beckman Research Institute of the City of Hope (BRICOH): Susan L. Neuhausen was partially supported by the Morris and Horowitz Families Endowed Professorship. BRICOH was supported by NIH R01CA74415 and NIH P30 CA033752. Copenhagen Breast Cancer Study (CBCS): The CBCS study was supported by the NEYE Foundation. Spanish National Cancer Centre (CNIO): This work was partially supported by Spanish Association against Cancer (AECC08), RTICC 06/0020/1060, FISPI08/1120, Mutua Madrileña Foundation (FMMA) and SAF2010-20493. City of Hope Cancer Center (COH): The City of Hope Clinical Cancer Genetics Community Research Network is supported by Award Number RC4A153828 (PI: Jeffrey N. Weitzel) from the National Cancer Institute and the Office of the Director, National Institutes of Health. CONsorzio Studi ITaliani sui Tumori Ereditari Alla Mammella (CONSIT TEAM): CONSIT TEAM was funded by grants from Fondazione Italiana per la Ricerca sul Cancro (Special Project “Hereditary tumors”), Italian Association for Cancer Research (AIRC, IG 8713), Italian Minitry of Health (Extraordinary National Cancer Program 2006, “Alleanza contro il Cancro” and “Progetto Tumori Femminili), Italian Ministry of Education, University and Research (Prin 2008) Centro di Ascolto Donne Operate al Seno (CAOS) association and by funds from Italian citizens who allocated the 5×1000 share of their tax payment in support of the Fondazione IRCCS Istituto Nazionale Tumori, according to Italian laws (INT-Institutional strategic projects ‘5×1000’). German Cancer Research Center (DKFZ): The DKFZ study was supported by the DKFZ. The Hereditary Breast and Ovarian Cancer Research Group Netherlands (HEBON): HEBON is supported by the Dutch Cancer Society grants NKI1998-1854, NKI2004-3088, NKI2007-3756, the NWO grant 91109024, the Pink Ribbon grant 110005, and the BBMRI grant CP46/NWO. Epidemiological study of BRCA1 & BRCA2 mutation carriers (EMBRACE): EMBRACE is supported by Cancer Research UK Grants C1287/A10118 and C1287/A11990. D. Gareth Evans and Fiona Lalloo are supported by an NIHR grant to the Biomedical Research Centre, Manchester. The Investigators at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust are supported by an NIHR grant to the Biomedical Research Centre at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust. Rosalind A. Eeles and Elizabeth Bancroft are supported by Cancer Research UK Grant C5047/A8385. Fox Chase Cancer Canter (FCCC): The authors acknowledge support from The University of Kansas Cancer Center and the Kansas Bioscience Authority Eminent Scholar Program. Andrew K. Godwin was funded by 5U01CA113916, R01CA140323, and by the Chancellors Distinguished Chair in Biomedical Sciences Professorship. German Consortium of Hereditary Breast and Ovarian Cancer (GC-HBOC): The German Consortium of Hereditary Breast and Ovarian Cancer (GC-HBOC) is supported by the German Cancer Aid (grant no 109076, Rita K. Schmutzler) and by the Center for Molecular Medicine Cologne (CMMC). Genetic Modifiers of cancer risk in BRCA1/2 mutation carriers (GEMO): The GEMO study was supported by the Ligue National Contre le Cancer; the Association “Le cancer du sein, parlons-en!” Award and the Canadian Institutes of Health Research for the “CIHR Team in Familial Risks of Breast Cancer” program. Gynecologic Oncology Group (GOG): This study was supported by National Cancer Institute grants to the Gynecologic Oncology Group (GOG) Administrative Office and Tissue Bank (CA 27469), Statistical and Data Center (CA 37517), and GOG's Cancer Prevention and Control Committtee (CA 101165). Drs. Mark H. Greene and Phuong L. Mai were supported by funding from the Intramural Research Program, NCI, NIH. Hospital Clinico San Carlos (HCSC): HCSC was supported by RETICC 06/0020/0021, FIS research grant 09/00859, Instituto de Salud Carlos III, Spanish Ministry of Economy and Competitivity, and the European Regional Development Fund (ERDF). Helsinki Breast Cancer Study (HEBCS): The HEBCS was financially supported by the Helsinki University Central Hospital Research Fund, Academy of Finland (132473), the Finnish Cancer Society, the Nordic Cancer Union, and the Sigrid Juselius Foundation. Study of Genetic Mutations in Breast and Ovarian Cancer patients in Hong Kong and Asia (HRBCP): HRBCP is supported by The Hong Kong Hereditary Breast Cancer Family Registry and the Dr. Ellen Li Charitable Foundation, Hong Kong. Molecular Genetic Studies of Breast and Ovarian Cancer in Hungary (HUNBOCS): HUNBOCS was supported by Hungarian Research Grant KTIA-OTKA CK-80745 and the Norwegian EEA Financial Mechanism HU0115/NA/2008-3/ÖP-9. Institut Català d'Oncologia (ICO): The ICO study was supported by the Asociación Española Contra el Cáncer, Spanish Health Research Foundation, Ramón Areces Foundation, Carlos III Health Institute, Catalan Health Institute, and Autonomous Government of Catalonia and contract grant numbers: ISCIIIRETIC RD06/0020/1051, PI09/02483, PI10/01422, PI10/00748, 2009SGR290, and 2009SGR283. International Hereditary Cancer Centre (IHCC): Supported by the Polish Foundation of Science. Katarzyna Jaworska is a fellow of International PhD program, Postgraduate School of Molecular Medicine, Warsaw Medical University. Iceland Landspitali–University Hospital (ILUH): The ILUH group was supported by the Icelandic Association “Walking for Breast Cancer Research” and by the Landspitali University Hospital Research Fund. INterdisciplinary HEalth Research Internal Team BReast CAncer susceptibility (INHERIT): INHERIT work was supported by the Canadian Institutes of Health Research for the “CIHR Team in Familial Risks of Breast Cancer” program, the Canadian Breast Cancer Research Alliance grant 019511 and the Ministry of Economic Development, Innovation and Export Trade grant PSR-SIIRI-701. Jacques Simard is Chairholder of the Canada Research Chair in Oncogenetics. Istituto Oncologico Veneto (IOVHBOCS): The IOVHBOCS study was supported by Ministero dell'Istruzione, dell'Università e della Ricerca and Ministero della Salute (“Progetto Tumori Femminili” and RFPS 2006-5-341353,ACC2/R6.9”). Kathleen Cuningham Consortium for Research into Familial Breast Cancer (kConFab): kConFab is supported by grants from the National Breast Cancer Foundation and the National Health and Medical Research Council (NHMRC) and by the Queensland Cancer Fund; the Cancer Councils of New South Wales, Victoria, Tasmania, and South Australia; and the Cancer Foundation of Western Australia. Amanda B. Spurdle is an NHMRC Senior Research Fellow. The Clinical Follow Up Study was funded from 2001–2009 by NHMRC and currently by the National Breast Cancer Foundation and Cancer Australia #628333. Mayo Clinic (MAYO): MAYO is supported by NIH grant CA128978, an NCI Specialized Program of Research Excellence (SPORE) in Breast Cancer (CA116201), a U.S. Department of Defence Ovarian Cancer Idea award (W81XWH-10-1-0341) and grants from the Breast Cancer Research Foundation and the Komen Foundation for the Cure. McGill University (MCGILL): The McGill Study was supported by Jewish General Hospital Weekend to End Breast Cancer, Quebec Ministry of Economic Development, Innovation, and Export Trade. Memorial Sloan-Kettering Cancer Center (MSKCC): The MSKCC study was supported by Breast Cancer Research Foundation, Niehaus Clinical Cancer Genetics Initiative, Andrew Sabin Family Foundation, and Lymphoma Foundation. Modifier Study of Quantitative Effects on Disease (MODSQUAD): MODSQUAD was supported by the European Regional Development Fund and the State Budget of the Czech Republic (RECAMO, CZ.1.05/2.1.00/03.0101). Women's College Research Institute, Toronto (NAROD): NAROD was supported by NIH grant: 1R01 CA149429-01. National Cancer Institute (NCI): Drs. Mark H. Greene and Phuong L. Mai were supported by the Intramural Research Program of the US National Cancer Institute, NIH, and by support services contracts NO2-CP-11019-50 and N02-CP-65504 with Westat, Rockville, MD. National Israeli Cancer Control Center (NICCC): NICCC is supported by Clalit Health Services in Israel. Some of its activities are supported by the Israel Cancer Association and the Breast Cancer Research Foundation (BCRF), NY. N. N. Petrov Institute of Oncology (NNPIO): The NNPIO study has been supported by the Russian Foundation for Basic Research (grants 11-04-00227, 12-04-00928, and 12-04-01490), the Federal Agency for Science and Innovations, Russia (contract 02.740.11.0780), and through a Royal Society International Joint grant (JP090615). The Ohio State University Comprehensive Cancer Center (OSU-CCG): OSUCCG is supported by the Ohio State University Comprehensive Cancer Center. South East Asian Breast Cancer Association Study (SEABASS): SEABASS is supported by the Ministry of Science, Technology and Innovation, Ministry of Higher Education (UM.C/HlR/MOHE/06) and Cancer Research Initiatives Foundation. Sheba Medical Centre (SMC): The SMC study was partially funded through a grant by the Israel Cancer Association and the funding for the Israeli Inherited Breast Cancer Consortium. Swedish Breast Cancer Study (SWE-BRCA): SWE-BRCA collaborators are supported by the Swedish Cancer Society. The University of Chicago Center for Clinical Cancer Genetics and Global Health (UCHICAGO): UCHICAGO is supported by grants from the US National Cancer Institute (NIH/NCI) and by the Ralph and Marion Falk Medical Research Trust, the Entertainment Industry Fund National Women's Cancer Research Alliance, and the Breast Cancer Research Foundation. University of California Los Angeles (UCLA): The UCLA study was supported by the Jonsson Comprehensive Cancer Center Foundation and the Breast Cancer Research Foundation. University of California San Francisco (UCSF): The UCSF study was supported by the UCSF Cancer Risk Program and the Helen Diller Family Comprehensive Cancer Center. United Kingdom Familial Ovarian Cancer Registries (UKFOCR): UKFOCR was supported by a project grant from CRUK to Paul Pharoah. University of Pennsylvania (UPENN): The UPENN study was supported by the National Institutes of Health (NIH) (R01-CA102776 and R01-CA083855), Breast Cancer Research Foundation, Rooney Family Foundation, Susan G. Komen Foundation for the Cure, and the Macdonald Family Foundation. Victorian Familial Cancer Trials Group (VFCTG): The VFCTG study was supported by the Victorian Cancer Agency, Cancer Australia, and National Breast Cancer Foundation. Women's Cancer Research Initiative (WCRI): The WCRI at the Samuel Oschin Comprehensive Cancer Institute, Cedars Sinai Medical Center, Los Angeles, is funded by the American Cancer Society Early Detection Professorship (SIOP-06-258-01-COUN). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Antoniou A, Pharoah PD, Narod S, Risch HA, Eyfjord JE, et al. (2003) Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 72: 1117–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Antoniou AC, Chenevix-Trench G (2010) Common genetic variants and cancer risk in Mendelian cancer syndromes. Curr Opin Genet Dev 20: 299–307 S0959-437X(10)00044-4 [pii];10.1016/j.gde.2010.03.010 [doi]. [DOI] [PubMed] [Google Scholar]
- 3. Begg CB, Haile RW, Borg A, Malone KE, Concannon P, et al. (2008) Variation of breast cancer risk among BRCA1/2 carriers. JAMA 299: 194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Simchoni S, Friedman E, Kaufman B, Gershoni-Baruch R, Orr-Urtreger A, et al. (2006) Familial clustering of site-specific cancer risks associated with BRCA1 and BRCA2 mutations in the Ashkenazi Jewish population. Proc Natl Acad Sci U S A 103: 3770–3774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Couch FJ, Gaudet MM, Antoniou AC, Ramus SJ, Kuchenbaecker KB, et al. (2012) Common cariants at the 19p13.1 and ZNF365 loci are associated with ER subtypes of breast cancer and ovarian cancer risk in BRCA1 and BRCA2 mutation carriers. Cancer Epidemiol Biomarkers Prev 21: 645–657 1055-9965.EPI-11-0888 [pii];10.1158/1055-9965.EPI-11-0888 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ramus SJ, Kartsonaki C, Gayther SA, Pharoah PD, Sinilnikova OM, et al. (2010) Genetic variation at 9p22.2 and ovarian cancer risk for BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst 103: 105–116 djq494 [pii];10.1093/jnci/djq494 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ramus SJ, Antoniou AC, Kuchenbaecker KB, Soucy P, Beesley J, et al. (2012) Ovarian cancer susceptibility alleles and risk of ovarian cancer in BRCA1 and BRCA2 mutation carriers. Hum Mutat 33: 690–702 10.1002/humu.22025 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Antoniou AC, Spurdle AB, Sinilnikova OM, Healey S, Pooley KA, et al. (2008) Common breast cancer-predisposition alleles are associated with breast cancer risk in BRCA1 and BRCA2 mutation carriers. Am J Hum Genet 82: 937–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Antoniou AC, Sinilnikova OM, McGuffog L, Healey S, Nevanlinna H, et al. (2009) Common variants in LSP1, 2q35 and 8q24 and breast cancer risk for BRCA1 and BRCA2 mutation carriers. Hum Mol Genet 18: 4442–4456 ddp372 [pii];10.1093/hmg/ddp372 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Antoniou AC, Kartsonaki C, Sinilnikova OM, Soucy P, McGuffog L, et al. (2011) Common alleles at 6q25.1 and 1p11.2 are associated with breast cancer risk for BRCA1 and BRCA2 mutation carriers. Hum Mol Genet 20: 3304–3321 ddr226 [pii];10.1093/hmg/ddr226 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Antoniou AC, Kuchenbaecker KB, Soucy P, Beesley J, Chen X, et al. (2012) Common variants at 12p11, 12q24, 9p21, 9q31.2 and in ZNF365 are associated with breast cancer risk for BRCA1 and/or BRCA2 mutation carriers. Breast Cancer Res 14: R33 bcr3121 [pii];10.1186/bcr3121 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Antoniou AC, Wang X, Fredericksen ZS, McGuffog L, Tarrell R, et al. (2010) A locus on 19p13 modifies risk of breast cancer in BRCA1 mutation carriers and is associated with hormone receptor-negative breast cancer in the general population. Nat Genet 42: 885–892 ng.669 [pii];10.1038/ng.669 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stevens KN, Vachon CM, Lee AM, Slager S, Lesnick T, et al. (2011) Common breast cancer susceptibility loci are associated with triple negative breast cancer. Cancer Res 0008-5472.CAN-11-1266 [pii];10.1158/0008-5472.CAN-11-1266 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gaudet MM, Kuchenbaecker KB, Vijai J, Klein RJ, Kirchhoff T, et al. (2013) Identification of a BRCA2-specific Modifier Locus at 6p24 Related to Breast Cancer Risk. PLoS Genet 9: e1003173 doi:10.1371/journal.pgen.1003173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Robertson A, Hill WG (1984) Deviations from Hardy-Weinberg proportions: sampling variances and use in estimation of inbreeding coefficients. Genetics 107: 703–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Antoniou AC, Goldgar DE, Andrieu N, Chang-Claude J, Brohet R, et al. (2005) A weighted cohort approach for analysing factors modifying disease risks in carriers of high-risk susceptibility genes. Genet Epidemiol 29: 1–11. [DOI] [PubMed] [Google Scholar]
- 17. Barnes DR, Lee A, Easton DF, Antoniou AC (2012) Evaluation of association methods for analysing modifiers of disease risk in carriers of high-risk mutations. Genet Epidemiol 36: 274–291 10.1002/gepi.21620 [doi]. [DOI] [PubMed] [Google Scholar]
- 18. Antoniou AC, Sinilnikova OM, Simard J, Leone M, Dumont M, et al. (2007) RAD51 135G→C modifies breast cancer risk among BRCA2 mutation carriers: results from a combined analysis of 19 studies. Am J Hum Genet 81: 1186–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Amin N, van Duijn CM, Aulchenko YS (2007) A genomic background based method for association analysis in related individuals. PLoS ONE 2: e1274 doi:10.1371/journal.pone.0001274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Leutenegger AL, Prum B, Genin E, Verny C, Lemainque A, et al. (2003) Estimation of the inbreeding coefficient through use of genomic data. Am J Hum Genet 73: 516–523 10.1086/378207 [doi];S0002-9297(07)62015-1 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Boos DD (1992) On generalised score tests. American Statistician 46: 327–333. [Google Scholar]
- 22. Wellcome Trust Case Control Consortium (2007) Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature 447: 661–678 nature05911 [pii];10.1038/nature05911 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aulchenko YS, Ripke S, Isaacs A, van Duijn CM (2007) GenABEL: an R library for genome-wide association analysis. Bioinformatics 23: 1294–1296 btm108 [pii];10.1093/bioinformatics/btm108 [doi]. [DOI] [PubMed] [Google Scholar]
- 24. Lange K, Weeks D, Boehnke M (1988) Programs for pedigree analysis: MENDEL, FISHER, and dGENE. Genet Epidemiol 5: 471–472. [DOI] [PubMed] [Google Scholar]
- 25. Antoniou AC, Cunningham AP, Peto J, Evans DG, Lalloo F, et al. (2008) The BOADICEA model of genetic susceptibility to breast and ovarian cancers: updates and extensions. Br J Cancer 98: 1457–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mulligan AM, Couch FJ, Barrowdale D, Domchek SM, Eccles D, et al. (2011) Common breast cancer susceptibility alleles are associated with tumor subtypes in BRCA1 and BRCA2 mutation carriers: results from the Consortium of Investigators of Modifiers of BRCA1/2. Breast Cancer Res 13: R110 bcr3052 [pii];10.1186/bcr3052 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Howie B, Marchini J, Stephens M (2011) Genotype imputation with thousands of genomes. G3 (Bethesda) 1: 457–470 10.1534/g3.111.001198 [doi];GGG_001198 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Antoniou AC, Beesley J, McGuffog L, Sinilnikova OM, Healey S, et al. (2010) Common Breast Cancer Susceptibility Alleles and the Risk of Breast Cancer for BRCA1 and BRCA2 Mutation Carriers: Implications for Risk Prediction. Cancer Res 70: 9742–9754 0008-5472.CAN-10-1907 [pii];10.1158/0008-5472.CAN-10-1907 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mavaddat N, Barrowdale D, Andrulis IL, Domchek SM, Eccles D, et al. (2012) Pathology of breast and ovarian cancers among BRCA1 and BRCA2 mutation carriers: results from the Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA). Cancer Epidemiol Biomarkers Prev 21: 134–147 1055-9965.EPI-11-0775 [pii];10.1158/1055-9965.EPI-11-0775 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Goode EL, Chenevix-Trench G, Song H, Ramus SJ, Notaridou M, et al. (2010) A genome-wide association study identifies susceptibility loci for ovarian cancer at 2q31 and 8q24. Nat Genet 42: 874–879 ng.668 [pii];10.1038/ng.668 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bojesen S, Pooley KA, Johnatty SE, Beesley J, Michailidou K, et al. (2012) Multiple independent TERT variants associated with telomere length and risks of breast and ovarian cancer. Nat Genet In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Michailidou K, Hall P, Gonzalez-Neira A, Ghoussaini M, Dennis J, et al. (2012) Large-scale genotyping identifies 41 new loci associated with breast cancer risk. Nat Genet In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sladek R, Rocheleau G, Rung J, Dina C, Shen L, et al. (2007) A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 445: 881–885 nature05616 [pii];10.1038/nature05616 [doi]. [DOI] [PubMed] [Google Scholar]
- 34. Garcia-Closas M, Couch FJ, Lindstrom S, Michailidou K, Schmidt MK, et al. (2012) Genome-wide association studies identify four ER-negative specific breast cancer risk loci. Nat Genet In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Atwal GS, Kirchhoff T, Bond EE, Montagna M, Menin C, et al. (2009) Altered tumor formation and evolutionary selection of genetic variants in the human MDM4 oncogene. Proc Natl Acad Sci U S A 106: 10236–10241 0901298106 [pii];10.1073/pnas.0901298106 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Curtis C, Shah SP, Chin SF, Turashvili G, Rueda OM, et al. (2012) The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 486: 346–352 nature10983 [pii];10.1038/nature10983 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Laurie NA, Donovan SL, Shih CS, Zhang J, Mills N, et al. (2006) Inactivation of the p53 pathway in retinoblastoma. Nature 444: 61–66 nature05194 [pii];10.1038/nature05194 [doi]. [DOI] [PubMed] [Google Scholar]
- 38. Wade M, Wahl GM (2009) Targeting Mdm2 and Mdmx in cancer therapy: better living through medicinal chemistry? Mol Cancer Res 7: 1–11 7/1/1 [pii];10.1158/1541-7786.MCR-08-0423 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fairfax BP, Makino S, Radhakrishnan J, Plant K, Leslie S, et al. (2012) Genetics of gene expression in primary immune cells identifies cell type-specific master regulators and roles of HLA alleles. Nat Genet 44: 501–510 ng.2205 [pii];10.1038/ng.2205 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ge B, Pokholok DK, Kwan T, Grundberg E, Morcos L, et al. (2009) Global patterns of cis variation in human cells revealed by high-density allelic expression analysis. Nat Genet 41: 1216–1222 ng.473 [pii];10.1038/ng.473 [doi]. [DOI] [PubMed] [Google Scholar]
- 41. Grundberg E, Adoue V, Kwan T, Ge B, Duan QL, et al. (2011) Global analysis of the impact of environmental perturbation on cis-regulation of gene expression. PLoS Genet 7: e1001279 doi:10.1371/journal.pgen.1001279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Stefansson H, Helgason A, Thorleifsson G, Steinthorsdottir V, Masson G, et al. (2005) A common inversion under selection in Europeans. Nat Genet 37: 129–137 ng1508 [pii];10.1038/ng1508 [doi]. [DOI] [PubMed] [Google Scholar]
- 43. Bowen NJ, Walker LD, Matyunina LV, Logani S, Totten KA, et al. (2009) Gene expression profiling supports the hypothesis that human ovarian surface epithelia are multipotent and capable of serving as ovarian cancer initiating cells. BMC Med Genomics 2: 71 1755-8794-2-71 [pii];10.1186/1755-8794-2-71 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ikram MA, Fornage M, Smith AV, Seshadri S, Schmidt R, et al. (2012) Common variants at 6q22 and 17q21 are associated with intracranial volume. Nat Genet 44: 539–544 ng.2245 [pii];10.1038/ng.2245 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Simon-Sanchez J, Schulte C, Bras JM, Sharma M, Gibbs JR, et al. (2009) Genome-wide association study reveals genetic risk underlying Parkinson's disease. Nat Genet 41: 1308–1312 ng.487 [pii];10.1038/ng.487 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pharoah P, Tsai YY, Ramus S, Phelan C, Goode EL, et al. (2012) GWAS meta-analysis and replication identifies three new susceptibility loci for ovarian cancer. Nat Genet In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multidimensional scaling of stage 1 and stage 2 (genotyped on iCOGS) samples. Panel A: Graphical representation of the first two components, for the BRCA1 carriers, for subgroups defined by the common 185delAG (c.68_69delAG) BRCA1 Jewish founder mutation, the 5382insC (c.5266dupC) Eastern European founder mutation and Hapap individuals (CEU: European; ASI: Includes CHB and JPT populations; YRI: African). Panel B: Red dots represent the samples with >22% non-European ancestry, excluded from the analysis.
(PDF)
Genotyping cluster plots in the BRCA1 samples for the key associated SNPs.
(PDF)
Quantile-quantile plot for the kinship adjusted score test statistic for stage 2 samples (1 degree of freedom χ2 trend test) for the associations with breast cancer (panel A) and ovarian cancer (panel B) risk for BRCA1 mutation carriers. The y = x line corresponds to the expected distribution, under the hypothesis of no inflation. Inflation was estimated using the values of the lowest 90% test statistics.
(PDF)
P-values (on −log10 scale) by chromosomal position, for the associations of 31,812 BRCA1 GWAS SNPs with breast (panel A) and ovarian (panel B) cancer risk for BRCA1 mutation carriers in the combined stage 1 and stage 2 samples. Blue lines correspond to a P-value of 10−5; red lines correspond to P-value 5×10−8.
(PDF)
Forest plots of the associations by country of residence of BRCA1 mutation carriers in the combined stage 1, stage 2 and stage 3 samples for SNPs found to be associated with breast and ovarian cancer risk for BRCA1 mutation carriers. Squares indicate the country specific, per-allele HR estimates for the SNPs. The area of the square is proportional to the inverse of the variance of the estimate. Horizontal lines indicate 95% confidence intervals. There was some evidence of heterogeneity in country-specific HR estimates for the rs2290854 and rs6682208 SNP (P = 0.04 and 0.02 respectively, Figure S3), but after accounting for opposite effects of these SNPs in Finland/Denmark, there was no evidence of heterogeneity. There was some evidence of heterogeneity in the country-specific HRs for rs17631303 (P-het = 0.004, df = 19) but this was no longer present after excluding one country (Poland, P-het = 0.12, df = 18), or when restricting analyses to Stage 1 and 2 samples only (P-het = 0.09, df = 19). There was no evidence of heterogeneity for correlated SNP rs183211 (P-het = 0.10). There was no evidence of hereterogeneity in the country-specific HRs for any of the other SNPs (P>0.68).
(PDF)
MDM4 regional association plot using BRCA1 stage 1 and stage 2 samples. P-values for association (−log10 scale) with breast cancer risk for BRCA1 mutation carriers for genotyped SNPs (diamond symbols ◊) and SNPs imputed from the 1000 genomes project data (square symbols □), by position (hg18) on chromosome 1. Red gradient represents r2 value with the most significant genotyped SNP rs4951407. The blue peaks represent recombination rate in the region.
(PDF)
TCF7L2 regional association plot using BRCA1 stage 1 and stage 2 samples. P-values for association (−log10 scale) with breast cancer risk for BRCA1 mutation carriers for genotyped SNPs (diamond symbols ◊) and SNPs imputed from the 1000 genomes project data (square symbols □), by position (hg18) on chromosome 1. Missing genotypes were replaced by imputed results. Red gradient represents r2 value with the most significant genotyped SNP rs11196174. The blue peaks represent recombination rate in the region.
(PDF)
Linkage disequilibrium patterns between the SNPs in the novel (17q21.31) and previously identified regions on 17q21. SNPs in the novel region are uncorrelated with SNPs in the 43.3–44.3 Mb region (positions according to hg build 36.3).
(PDF)
4q32.3 regional association plot using BRCA1 stage 1 and stage 2 samples. P-values for association (−log10 scale) with ovarian cancer risk for BRCA1 mutation carriers for genotyped SNPs (diamond symbols ◊) and imputed SNPs from the 1000 genomes project data (square symbols □), by position (hg18) on chromosome 1. Red gradient represents r2 value with the most significant genotyped SNP rs4691139. Blue peaks represent recombination rate in the region.
(PDF)
Combined Hazard Ratios (HR) for breast and ovarian cancer for BRCA1 mutation carriers. (A) HR for Breast Cancer based on 10 loci associated with breast cancer risk for BRCA1 mutation carriers. (B) Ovarian Cancer based on 7 loci associated with ovarian cancer risk for BRCA1 mutation carriers. All HRs computed relative to the lowest risk category. The Y-axes translate the combined HRs into absolute risks of developing breast or ovarian cancer by age 80. The absolute risks and HRs at different percentiles of the combined genotype distribution are also marked. The combined HRs were obtained under the assumption that the loci interact multiplicatively.
(PDF)
Cis-eQTL and allelic expression (AE) analyses at MDM4 locus. A) Cis-eQTLs for SNPs at MDM4 locus using expression data from primary human osteoblasts (HOb). B) AE mapping for cis-regulatory variation in MDM4 locus using primary skin fibroblasts. Coordinates (hg18) for locus shown on top; blue tracks indicate the −log10(P value) of the association across all SNPs tested. The location of transcripts in this region is shown below.
(PDF)
Cis-eQTL and allelic expression (AE) analyses at chr17q21.31 locus. (Upper panel) Cis-eQTLs for SNPs at c17orf69 locus using expression data from primary human osteoblasts. Allelic expression mapping for cis-regulatory variation in KANSL1 (middle panel) and WNT3 loci (lower panel) using a CEU population panel of lymphoblastoid cells. Coordinates (hg18) for loci are shown on top; blue tracks indicate the −log10(P value) of the association across all SNPs tested. The location of transcripts in these regions are shown.
(PDF)
Affected and unaffected BRCA1 mutation carriers by study country in the breast and ovarian cancer analysis used in SNP selection for the iCOGS array.
(DOCX)
Origin of BRCA1 samples by Country and Stage used in the current analysis.
(DOCX)
Sample and SNP quality control summary.
(DOCX)
Associations with breast cancer risk for BRCA1 mutation carriers, for known breast cancer susceptibility variants.
(DOCX)
Associations with BRCA1 breast or ovarian cancer risk for SNPs genotyped at stages 1, 2, and 3.
(DOCX)
Analysis of breast cancer associations by BRCA1 mutation class.
(DOCX)
Associations with Breast Cancer ER status in BRCA1 carriers for SNPs genotyped in stages 1–3.
(DOCX)
Imputed SNPs at the novel 17q21 region with P-values less than the most significant genotyped SNP (rs169201).
(DOCX)
SNPs associated (P<1×10−5) with local expression and Allelic Imbalance.
(DOCX)
Supplementary Methods.
(DOCX)