Abstract
Objectives
The main objectives of this study were to assess personality traits and levels of anxiety in Foundation Year 2 (F2) doctors during the foundation doctor training programme in the Northern Ireland Deanery (NIMDTA).
Methods
A prospective survey-based study was conducted for all F2 doctors attending the mandatory generic skills programme at NIMDTA. Anxiety was measured using the State-Trait Anxiety Inventory (STAI) while personality was assessed using the IPIP-NEO questionnaire. These previously validated questionnaires were completed at the start and again at the end of the F2 year.
Results
147 (M=65, F=82) and 106 (M=55, F=51) F2 doctors completed questionnaires at both time points. STAI scores suggested a moderate level of anxiety amongst both male and female doctors at baseline and at the end of the academic year. There was no difference between gender for either parameter (Baseline-State: 34.0 vs. 36.0, p=0.48 and Trait: 39.0 vs. 40.5, p=0.33) (End-State: 41.0 vs. 36.0, p=0.14 and Trait: 42.0 vs. 40.5, p=0.78). IPIP-NEO scores for F2 doctors were consistently higher in the Accommodation (93.9 & 92.3) and Consolidation (88.8 & 87.6) personality factors and lower in the Neuroticism factor (66.3 & 65.9) at both assessment time-points. Female F2 doctors scored significantly higher in the accommodation factor at the end of the academic year when compared to their male counterparts (88.0 vs. 94.0, p<0.001). There was no difference between the genders for the other personality factors at the end of the year (p>0.09).
Conclusion
This first cohort of F2 doctors were exposed to many emerging changes in their training which did not appear to have any detrimental effect on their anxiety levels or personality profiles and suggests that junior doctors may not be affected by external influences or changing educational environments.
Keywords>: Anxiety, Doctor, Foundation, Personality, Programme
INTRODUCTION
A high level of stress and depressive symptomatology has been reported amongst male and female junior doctors in both Britain and the United States particularly during the transition from medical school to junior doctor 1–4. Females were reported to be more severely affected with a 1.5 times higher risk of depression and an 8 times higher likelihood of severe depression2,4. Newbury-Birch and Kamali (2001) identified that 37.5% of female and 24% of male pre-registration house officers suffered from possible psychological stress 3. More recently, Tyssen et al (2007) have also described a higher level of stress amongst female medical students 5. This gender difference in symptomatology is destined to become a more important phenomenon as many medical schools now report a higher proportion of females to males (70:30) in the medical student population6,7.
Numerous factors for anxiety and stress have been documented such as overwork and its impact on sleep and personal life, talking to distressed relatives and serious treatment failures 2. These high levels of fatigue and distress have also been independently associated with self-perceived medical errors in internal medical residents8. Despite the introduction of numerous steps to reduce working hours, improve education and clinical supervision, the incidence of psychological morbidity amongst house officers remains high 9–11.
It was hoped that modern amendments to postgraduate training through the combined auspices of Foundation Training Programmes, Modernising Medical Careers (MMC) and Regional Post-Graduate Medical Training Agencies may lead to reductions in overall anxiety and stress amongst junior doctors. However, in a profession that is occupied with the treatment of patients, elements of psychological disturbance can never be completely avoided. The assessment of anxiety in the modern junior doctor is therefore an extremely important factor to determine whether newly implemented strategies to improve the quality of junior doctor experiences, training and quality of life are working.
Medical doctors have been shown to represent a homogenous group of individuals in terms of intellectual and cognitive ability. They appear to share common personality traits based on their initial choice of the medical profession as a career 12,13. However, personality differences within this group do still exist during the early stages of a medical career. Maron et al (2007) reported a significantly higher degree of neuroticism and openness in medical students selecting psychiatry residencies compared to a lower degree of neuroticism in medical students selecting family practice. These authors concluded that these personality profiles may only predict medical student selection of some but not all medical specialities14.
During medical school, trainee doctors often experience a uniform core curriculum which provides a similar range of experiences and perceptions of future career choices. However, environmental differences can still be introduced at an undergraduate level through variances in individually selected special study modules or may only become evident after graduation from medical school where the junior doctor experiences a variety of medical specialties with different work settings, job duties, requisite skills and vocational interests 13. Despite the influence of a medical environment on an individual’s choice of future career, it is also important to consider an individual’s personality trait as a major factor in determining their future occupational requirements 15,16. Medical educators and career counsellors therefore attempt to explore and match such personality traits to occupational requirements. However, these efforts often rely on anecdotal evidence about the incumbents of different medical specialties to direct the junior doctor towards a specialty that best fits their personality 13.
The attendance of Foundation Year 2 (F2) doctors at the Generic Skills course as part of the Northern Ireland Foundation Programme afforded an opportunity to assess anxiety responses and personality traits amongst doctors in a non-clinical setting removed from the hospital environment (*The generic skills course includes guidance and teaching on clinical audit, career management advice, team working, patient safety with emphasis on risk management allied to clinical governance. All F2 doctors must complete the generic skills course as part of their two-year Foundation Programme). We have previously reported on the effects of MMC on Foundation doctor career orientation in the Northern Ireland Foundation School 17. The main objectives of this study were to assess personality traits and levels of anxiety in Foundation Year 2 doctors during the F2 training programme.
METHODS
This was a prospective survey-based cohort study assessing all F2 doctors enrolled in the F2 Training Programme in the Northern Ireland Deanery Foundation School for the academic year 2006-2007. A presentation explaining the study aims and objectives combined with written information was provided for each F2 doctor. The F2 doctors choose to participate while attending compulsory training modules of the Northern Ireland Foundation Programme Generic Skills course at the Northern Ireland Medical and Dental Training Agency (NIMDTA). Due to the assessment of a specific cohort of doctors in a single deanery, there was no comparator or control group assessed. Questionnaires were administered at 2 data capture points; at the start of the academic year (August – September 2006) and at the end of the academic year (June – July 2007). Basic demographical data was incorporated into the questionnaire followed by the assessment of anxiety and personality traits. To minimise inter-individual bias between data capture points, F2 doctors did not receive their questionnaire scores at either the start or end of the academic year.
STATE AND TRAIT ANXIETY INDEX
F2 doctor anxiety was measured using the State-Trait Anxiety Inventory (STAI) 18,19. The State-Anxiety scale (STAI Form X-1) consists of twenty statements that evaluate how the respondent feels “right now, at this moment” corresponding to the level of anxiety experienced in a particular situation. The Trait-Anxiety scale (STAI Form X-2) consists of a further twenty statements that evaluate how the respondent feels “generally” corresponding to the general level of anxiety independent of any particular anxiety-provoking event. The total scores for both the State-Anxiety and the Trait-Anxiety scales range from 20 to 80 with mean state scores of 35.7 and 35.2 and trait scores of 34.9 and 34.8 for male and female adults respectively 18. The internal consistency of the STAI scales remains high with reported Cronbach’s α co-efficient 0.93 and 0.92 for the State and Trait subscales respectively 19,20.
PERSONALITY TRAIT
Study of personality was based on the Five-Factor Model (FFM) which included the assessment of affective, experiental and motivational traits using the five factors of Neuroticism, Extraversion, Originality (Openness), Accommodation (Agreeableness) and Consolidation (Conscientiousness) 21–23. This study used the Short Form International Personality Item Pool Representation of the NEO PI-R™ personality inventory (IPIP-NEO) to assess personality traits 24,25. Each of the main personality domains were divided into thirty sub-domains which had a total of four different components giving 120 items in total. Each component was then keyed as a positive or negative item which was then collated to obtain a total scale score. The reported mean Cronbach’s α co-efficient for the Short Form IPIP-NEO is 0.75.
Statistical analysis was completed using the SPSS statistical package (Version 13 SPSS® inc. Chicago, USA). Descriptive data was presented as mean (standard error of the mean - SEM) or median (interquartile range - IQR). Differences in scores between genders were completed separately for doctors at each time-point and then for doctors who completed both questionnaires using the independent sample t-test. The mean percentage change for questionnaire indices at the end of the year was then compared to the baseline value at the start of the year [(End of Year Questionnaire – Start of Year Questionnaire) / Start of Year Questionnaire]. For doctors who completed both questionnaires, each parameter was also analysed independently for differences between both time points using the paired samples t-test. Pearson’s rank correlation co-efficient was calculated for state and trait anxiety scores. All statistical tests were 2-tailed with the differences considered significant if the p-value was <0.05.
RESULTS
There were 231 F2 doctors enrolled in the Northern Ireland Foundation Programme during 2006-2007. 147 (63.6%, M=65) and 106 (45.9%, M=55) completed questionnaires 1 and 2 at the start and end of the academic year, while 69 (29.9%, M=33) doctors completed the questionnaires at both time-points. Therefore, 46.9% (69/147) and 65.1% (69/106) of F2 doctors completed both questionnaires when compared to the total number of questionnaires completed for each time point. The study population was representative of the total year group with a mean age of 26 years with the majority graduating from Queen’s University Belfast in July 2005 (Male: 26.9 years, SEM 0.40 and Female: 26.1 years, SEM 0.28, p=0.09).
ANXIETY ASSESSMENT
The median state anxiety scores for male and female doctors were not significantly different for those doctors who completed the questionnaire at the start of the year only (34.0 vs. 36.0, p=0.48) and at the end of the year (41.0 vs. 36.0, p=0.14). There was no difference between gender for those doctors who completed the questionnaires at both time-points; Start of Year (33.0 vs. 36.0, p=0.16) and End of Year (41.0 vs. 37.0, p=0.31) (Table 1). There was also no difference identified in state anxiety scores for those who completed both questionnaires when the start and end of year scores were compared (36.3 vs. 39.5, p=0.06) (Figure 1).
Table 1.
State and Trait Anxiety scores for F2 Doctors who completed the questionnaire at the start, the end and for those who completed both questionnaires (Median, IQR).
| QUESTIONNAIRE | STATE | TRAIT | |||||
|---|---|---|---|---|---|---|---|
| Male | Female | p-value | Male | Female | p-value | ||
| Start of Year (n=147) | 34.0 (30.0-41.0) | 36.0 (32.0-42.0) | 0.48 | 39.0 (35.0-46.5) | 40.5 (36.0-47.0) | 0.33 | |
| End of Year (n=106) | 41.0 (41.0-45.3) | 36.0 (31.3-45.0) | 0.14 | 42.0 (36.8-47.0) | 40.5 (37.0-50.5) | 0.78 | |
| Both (n=69) | 1 | 33.0 (29.0-39.0) | 36.0 (32.0-41.8) | 0.16 | 40.0 (35.5-46.0) | 41.0 (36.3-47.0) | 0.21 |
| 2 | 41.0 (33.0-44.8) | 37.0 (30.0-43.0) | 0.31 | 42.5 (37.5-47.0) | 39.0 (36.0-51.0) | 0.84 | |
Fig. 1.
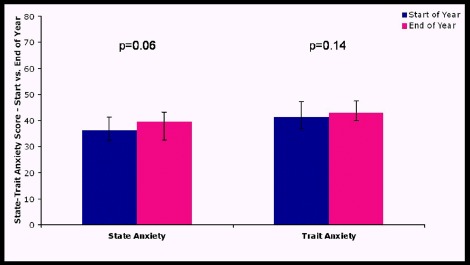
State and Trait Anxiety scores for F2 doctors who completed both questionnaires at the start and at the end of the year (median, IQR).
The median trait anxiety scores for male and female doctors were not significantly different for those doctors who only completed the questionnaire at the start of the year (39.0 vs. 40.5, p=0.33) and at the end of the year (42.0 vs. 40.5, p=0.78). When trait anxiety scores were assessed for those doctors who completed the questionnaire at both time-points, there was also no difference between the male and females; Start of Year (40.0 vs. 41.0, p=0.21) and End of Year (42.5 vs. 39.0, p=0.84) (Table 1). There was also no difference identified in trait anxiety scores for F2 doctors who completed both questionnaires when the start and end of year scores were assessed (41.3 vs. 42.9, p=0.14) (Figure 1).
Although there was no difference in state and trait anxiety scores for doctors who completed both questionnaires, there appeared to be a trend for a larger percentage increase in both state and trait anxiety scores for males compared to females when the mean percentage change for the end of year scores were compared to baseline (State: 27.2% vs. 4.5%, p=0.06 and Trait: 12.6% vs. 1.0%, p=0.09). There was a high correlation between the scores of state-anxiety and trait-anxiety for all the groups of F2 doctors (r=0.57, p<0.001).
PERSONALITY ASSESSMENT
At the start of the academic year, F2 doctors scored higher in the Accommodation and Consolidation factors and lower in the Neuroticism factor. There was no difference between genders for any of these five factors at the start of the academic year (Table 2). At the end of the academic year, F2 doctors continued to score higher in the Accommodation and Consolidation factors with lower scores for the Neuroticism factor. Similar to the start of the year, there was again no difference between genders for any of these five factors at the end of the academic year except for the accommodation factor which was significantly higher in the females (Table 2).
Table 2.
IPIP-NEO Personality Factor scores for F2 doctors at the start and at the end of the academic year (median, IQR).
| start of year n=147 | end of year n=106 | |||||
|---|---|---|---|---|---|---|
| PERSONALITY FACTOR | Male | Female | p-value | Male | Female | p-value |
| Neuroticism | 63.0 (56.0-73.0) | 66.0 (59.0-73.0 ) | 0.17 | 63.0 (57.0-70.0) | 64.0 (58.0-72.5) | 0.17 |
| Extraversion | 83.0 (77.0-88.0) | 82.0 (75.0-89.0) | 0.81 | 85.0 (76.0-89.3) | 81.0 (72.5-87.0) | 0.09 |
| Originality | 78.0 (72.0-83.5) | 80.0 (71.0-85.0) | 0.94 | 76.0 (72.0-83.3) | 78.0 (70.5-84.0) | 0.64 |
| Accommodation | 90.0 (85.0-96.5) | 95.0 (89.0-101.3) | 0.07 | 88.0 (80.8-95.5) | 94.0 (90.5-100.5) | <0.001 |
| Consolidation | 90.0 (80.5-95.5) | 90.0 (83.8-95.3) | 0.89 | 88.0 (80.8-94.3) | 90.0 (82.5-95.0) | 0.78 |
When the IPIP-NEO scores were compared for those doctors who completed both questionnaires, there was no significant difference for any of the personality factors between the start and end of the academic year (Figure 2). However, when the mean percentage change from baseline was assessed between genders for F2 doctors who completed both questionnaires, a significantly higher score was identified in the female doctors for the Accommodation Factor compared to male doctors (Figure 3). There was no difference in the mean percentage change from baseline between genders for the other factors.
Fig. 2.
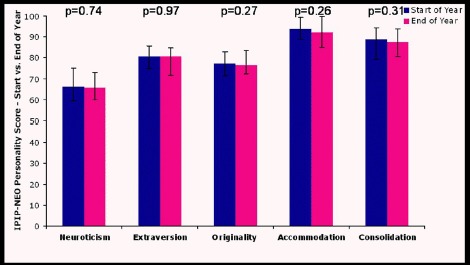
IPIP-NEO Personality Factors scores for F2 doctors who completed both questionnaires at the start and at the end of the academic year (median, IQR).
Fig. 3.
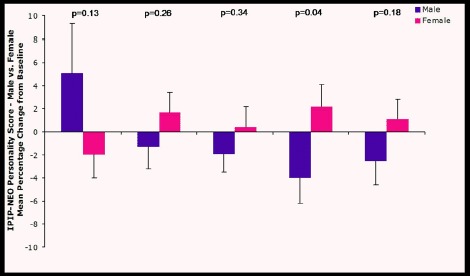
Mean percentage change from baseline in IPIP-NEO Personality Factor scores for male and female F2 doctors who completed both questionnaires at the start and at the end of the academic year (mean, SEM). From left to right, personality factors analysed include Neuroticism, Extraversion, Originality, Accommodation and Consolidation.
DISCUSSION
Identifying what one is suited to do and securing an opportunity to do it, is imperative in achieving life goals 26. Anxiety is known to influence many of these types of judgments and decisions with both state- and trait-anxiety shown to be significantly related to career decidedness 27–29. Previous researchers have emphasised the importance of career decision within an individual’s development and personal happiness 30,31 Campagna et al (2007) also identified, through regression analyses, that state anxiety was the strongest predictor of career certainty and indecision rather than the trait anxiety indices 29.
Unfortunately psychological morbidity among junior doctors still remains high 9,10. Despite Foundation Programmes providing an increased level of pastoral support for new doctors combined with improvements in educational and clinical supervision, it has been suggested that such educational bodies may also act as stress risk factors through increased scrutiny and monitoring of junior doctor professional performance. Mizuguchi et al (1991) defined STAI parameters for state-anxiety as; very low <22, low 23–31, normal 32–40, high 41–49 and very high >50 and trait-anxiety as; very low <23, low 24–32, normal 33–43, high 44–52 and very high >53 32. Other researchers have also documented mean adult state-anxiety scores of 34.4 whilst trait anxiety levels have been divided into low (<33), medium (33-49) and high (>49) 33,34. It is important to realise that these extrapolations may only apply to certain demographic groups who have recognisable pathologies.
Depending on the criterion used to define anxiety states, our study reports normal or medium state (36.3 and 39.5) and trait (41.3 and 42.9) scores for all junior doctors at the start and end of year respectively. Although there was no difference in scores between the genders, there was a trend for an increase in state anxiety score for male doctors compared to female doctors when the mean percentage change for the end of year scores compared to baseline was assessed (27.2% vs. 4.5%, p=0.06). Even with this increase, this would still imply a normal or medium amount of stress for these doctors at the time of their end of year assessment.
As trait-anxiety reflects a personality dimension, trait-anxiety scores would not be expected to change over short periods of time as has been demonstrated in this study (p=0.14). This lack of change combined with the high level of correlation between state and trait anxiety scores (r>0.57, p<0.001) has served to validate our study results and can be taken as an indicator of reliability in the use of the STAI-trait scale 35. The STAI-scores from our study do however contrast with other published reports. Peterlini et al (2002) reported a mean state-anxiety score of 42.5 and 49.3 for male and female first year residents in Brazil where female doctors had a significantly higher state-anxiety score (p<0.001) 35. They concluded that female doctors may have higher actual anxiety levels but that such a variance could also be attributed to higher reporting rates amongst this group.
Within NIMDTA, there have been numerous factors deployed and integrated into the Foundation Programme to improve the quality of work life balance for new foundation doctors. The majority of foundation doctor rotas are now fully compliant with the European Working Time Directive (EWTD)36. Allied to this reduction in overall working hours, there has been a reduction in the actual length of doctor’s shifts and an increase in off-duty during the working week ranging from single days up to a full week of leave. Further beneficial effects of the Foundation Programme have included an increase in both clinical and educational support particularly designed to support the mandatory completion of each individual’s e-portfolio. The introduction of the Generic Skills Course has afforded the opportunity for foundation doctors to discuss clinical scenarios away from the workplace in an environment with educational tutors and to avail of peer support.
In addition to such exogenous training tools, F2 doctor ability and maturity should also increase as the year progresses leading to an improved ability to deal with clinical scenarios and typical acute hospital workloads. It remains unclear whether the influence of NIMDTA’s numerous programmes to improve the Foundation Programme in our study has had an advantageous influence amongst foundation doctor anxiety in Northern Ireland. Furthermore the development and implementation of MMC combined with the Medical Training Application System (MTAS) may also have created both positive and negative experiences for this group of doctors.
From their review of personality and medical specialty choice, Borges et al (2002) comment extensively on difficulties associated with defining specific personality types in different specialties due to the multiplicity of factors such as the use of different personality inventories, recruitment criteria, the presence of small sample sizes and the effect of individual assessments at different stages of a medical career (graduates, residents and attending) (Table 3) 13. Other authors have reported specialty choices with other personality traits such as a higher degree of neuroticism and openness with psychiatry and a lower degree of neuroticism in family practice 14. Hojat and Zuckerman (2008) reported higher “impulsive sensation seeking” and lower “neuroticism” personality scores with surgical specialties whilst higher and lower “sociability” scores were attributed to primary care and hospital based specialties respectively with the Zuckerman-Kuhlman personality questionnaire (ZKPQ)15.
Table 3.
Personality traits for different medical specialties (data collated from review by Borges et al – 2002).
| specialty | scoring higher | scoring lower | Character |
|---|---|---|---|
| Anaesthesia | Extraversion, Originality | Neuroticism, Accommodation, Consolidation | Ability to experience negative affect, less sociable and dominating |
| General Medicine | Consolidation | Extraversion | Tendency to be stiff, cool, sceptical and aloof. Prefer working with things rather than people. |
| General Practice | Accommodation, Consolidation | Originality | Sympathetic, trusting, co-operative, and altruistic |
| Obstetrics and Gynaecology | Consolidation | Originality, Accommodation | Highly conscientious, organised, persistent, scrupulous and achievement orientated. |
| Paediatrics | Neuroticism, Extraversion, Accommodation | Consolidation | N / A |
| Pathology | Originality | Neuroticism | Able to experience negative effect, less socialable and dominating |
| Psychiatrists | Neuroticism, Originality, Accommodation | Extraversion, Vary with respect to Consolidation | Imaginative, curious, needing variety, experience feelings deeply, sympathetic, trusting, co-operative, altruistic |
| Rehabilitation | Neuroticism, Originality | Extraversion | N / A |
| Surgeons | Extraversion, Originality | Accommodation | Sociable, active, dominant, more antagonistic, less agreeable |
Our study is one of the first to prospectively assess a cohort of junior doctors at the same level who were in the process of considering future career choices. We have demonstrated that these foundation doctors scored higher on accommodation and consolidation but lower in neuroticism at the start of the academic year. Higher scores in accommodation and consolidation suggest a sympathetic, trusting, co-operative, and altruistic personality often attributed to doctors working within general practice. A lower score in neuroticism implies an ability to experience negative effect, whilst being less socialable and dominating often identified in laboratory specialties particularly pathology 13. The consolidation (conscientiousness) personality trait has also been reported as a significant predictor of performance in medical school where such relationships between personality and performance become increasingly significant as learners advance through medical training 37.
Similar to our study, Buddenberg-Fischer et al (2006) assessed specialty choices amongst fourth year Swiss residents and reported that gender had the greatest impact on specialty and career choice whilst career motivation and life goals were two other relevant influencing factors 38. In contrast, we only identified a minimal gender difference in the accommodation trait and no change in the other personality factors or STAI anxiety scores. These personality trends continued through to the end of the academic year which suggests that our personality testing instrument remained valid as an individual’s personality trait should remain fixed over time. We did not assess other attributes such as motivation or aspired life goals.
Although our study assessed the same cohort of doctors over one year, Borges et al (2002) commented that differences in personality trait may occur if such assessments are performed at different parts of a junior doctor’s career. Bland et al (1995) further reported that personality assessment should still be included as one of the many factors that students consider when choosing a specialty. The UK Strategy Group Reforms from 2004 suggested that both personality and aptitude of students and junior doctors should be taken into account during job selection processes 39. However, it should be understood that personality type testing is not an exact process as there is a greater variation within medical specialties than between them 13.
Similar to Borges et al (2002), we accept the limitations of our study whereby it remains difficult to compare these personality traits of foundation year doctors with those already in a specialty and who have already made a career choice. However, our study does provide early indicators of personality types for this group of doctors. Borges et al (2002) acknowledged inconsistencies regarding data recording probably due to measurement error and sampling idiosyncrasies. They further accepted that their review did not include any evidence of randomisation and may therefore be biased by an under- or over-representation of certain population subsets. A selection bias could also have been introduced because the individuals who chose to participate in the study may have had personality traits at the outset that attract them to particular psychological interventions. Although our data was not randomised, a true representation of the foundation year 2 doctors for the period of the study was obtained. However, similar to previous studies with varying response rates between 45.7% and 67.5%, it is unclear as to the influence of a potential selection bias in this selected group of doctors as only 63.6% of the total cohort chose to complete the questionnaires whilst a gender bias may also have been introduced due to differences in completion demographics between the two time points 5,8,40.
Despite recruitment from a single deanery, one of the major strengths of this study was the assessment of a fixed cohort of doctors who were exposed to a uniform Foundation Programme Generic Skills course. Although it would be impractical to attempt to initiate randomisation of foundation doctors to receive or abstain from generic skills tuition, a cross-sectional study incorporating a different deanery would be very useful to investigate the actual effect of the Foundation school on this group of doctors when compared to different foundation methodologies. However, this may also have ethical ramifications as it is important for optimisation of junior doctor training and development particularly within the first few years following qualification. It would also be useful to conduct this study at the very beginning of medical school with annual assessments rather than completion on multiple occasions in a single year. These assessments could then continue throughout medical school, the foundation programme and into the junior doctor’s career.
CONCLUSION
Studying this group of inaugural foundation doctors proved a challenging task. Despite the implementation of MMC with a coordinated UK wide specialty application process (MTAS) on the first cohort (2005-2007) of Foundation doctors, a detrimental effect on their anxiety levels and personality profiles was not evident. The resilience of new medical graduates is the most striking outcome demonstrated. However, the role of rota compliance, improved clinical and educational supervision as well as the generic skills course at the Northern Ireland Foundation School must not be discounted.
Acknowledgments
The authors acknowledge Mr Niall O’Donnell for his assistance with data entry and Dr Donncha Hanna and Dr Colin Cooper from the Department of Psychology, Queen’s University Belfast for their assistance with the personality and anxiety assessment tools.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest. We certify that we have participated sufficiently in the work of this paper. We have reviewed the final version of the manuscript and approve it for publication. To the best of our knowledge and belief, this manuscript has not been published in whole or in part nor is it being considered for publication elsewhere. No research funding or external financial support has been provided for this study.
REFERENCES
- 1.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354–73. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Firth-Cozens J. Emotional distress in junior house officers. BMJ (Clin Res Ed.) 1987;295(6597):533–6. doi: 10.1136/bmj.295.6597.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Newbury-Birch D, Kamali F. Psychological stress, anxiety, depression, job satisfaction, and personality characteristics in preregistration house officers. Postgrad Med J. 2001;77(904):109–11. doi: 10.1136/pmj.77.904.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsu K, Marshall V. Prevalence of depression and distress in a large sample of Canadian residents, interns, and fellows. Am J Psychiatr. 1987;144(12):1561–6. doi: 10.1176/ajp.144.12.1561. [DOI] [PubMed] [Google Scholar]
- 5.Tyssen R, Dolatowski FC, Rovik JO, Thorkildsen RF, Ekeberg O, Hem E, et al. Personality traits and types predict medical school stress: a six-year longitudinal and nationwide study. Med Educ. 2007;41(8):781–7. doi: 10.1111/j.1365-2923.2007.02802.x. [DOI] [PubMed] [Google Scholar]
- 6.McKinstry B. Are there too many female medical graduates? Yes. BMJ. 2008;336(7647):748. doi: 10.1136/bmj.39505.491065.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lempp H, Seale C. Medical students’ perceptions in relation to ethnicity and gender: a qualitative study. BMC Med Educ. 2006;6:17. doi: 10.1186/1472-6920-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294–300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 9.Birch D, Ashton H, Kamali F. Alcohol, drinking, illicit drug use, and stress in junior house officers in north-east England. Lancet. 1998;352(9130):785–6. doi: 10.1016/S0140-6736(05)60679-4. [DOI] [PubMed] [Google Scholar]
- 10.Bogg J, Gibbs T, Bundred P. Training, job demands and mental health of pre-registration house officers. Med Educ. 2001;35(6):590–5. doi: 10.1046/j.1365-2923.2001.00951.x. [DOI] [PubMed] [Google Scholar]
- 11.West R, Goldberg I, Harrigan P, Paice E. Pre-registration house officer training: implementing change. London: COPMeD; 1993. [Google Scholar]
- 12.Schwartz RW, Barclay JR, Harrell PL, Murphy AE, Jarecky RK, Donnelly MB. Defining the surgical personality: a preliminary study. Surgery. 1994;115(1):62–8. [PubMed] [Google Scholar]
- 13.Borges N, Savickas M. Personality and Medical Specialty Choice: A Literature Review and Integration. J Career Assess. 2002;10(3):362–80. [Google Scholar]
- 14.Maron BA, Fein S, Maron BJ, Hillel AT El, Baghdadi MM, Rodenhauser P. Ability of prospective assessment of personality profiles to predict the practice specialty of medical students. Proc (Bay Univ Med Cent). 2007;20(1):22–6. doi: 10.1080/08998280.2007.11928228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hojat M, Zuckerman M. Personality and specialty interest in medical students. Medical teacher. 2008;30(4):400–406. doi: 10.1080/01421590802043835. [DOI] [PubMed] [Google Scholar]
- 16.Walton HJ. Personality assessment of future doctors: discussion paper. J R Soc Med. 1987;80(1):27–30. doi: 10.1177/014107688708000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Donnell ME, Noad R, Boohan M, Carragher A. The Effect of Modernising Medical Careers on Foundation Doctor Career Orientation in the Northern Ireland Foundation School. Ulster Med J. 2010;79(2):62–9. [PMC free article] [PubMed] [Google Scholar]
- 18.Spielberger CD, Gorush RL, Lushene RE. State Trait Anxiety Inventory Manual. Palo Alto, CA: Consuling Psychologists Press; 1970. [Google Scholar]
- 19.Fountoulakis KN, Papadopoulou M, Kleanthous S, Papadopoulou A, Bizeli V, Nimatoudis I, Iacovides A, Kaprinis GS. Reliability and psychometric properties of the Greek translation of the State-Trait Anxiety Inventory form Y: preliminary data. Ann Gen Psychiatr. 2006;5:2. doi: 10.1186/1744-859X-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spielberger CD, Gonzalez HP, Taylor CJ, Anton WD, Algaze B, Ross GR, et al. Test Anxiety Inventory: preliminary professional manual. Palo Alta, CA: Consulting Psychologist Press; 1980. [Google Scholar]
- 21.McCrae RR. The Five-Factor Model: issues and applications. [Special issue] J Pers. 1992; 60. [PubMed]
- 22.McCrae RR, Costa PT., Jr. Reinterpreting the Myers-Briggs Type Indicator from the perspective of the Five-Factor Model of Personality. J Pers. 1989;57(1):17–40. doi: 10.1111/j.1467-6494.1989.tb00759.x. [DOI] [PubMed] [Google Scholar]
- 23.Goldberg LR. The structure of phenotypic personality traits. Am Psychol. 1993;48(1):26–34. doi: 10.1037//0003-066x.48.1.26. [DOI] [PubMed] [Google Scholar]
- 24.International Personality Item Pool: A Scientific collaboratory for the development of advanced measures of personality traits and other individual differences. Available online at: http://ipip.ori.org/ Last accessed October 2011.
- 25.Goldberg LR. A broad-bandwidth, public domain, personality inventory measuring the lower-level facets of several five-factor models. In: Mervielde I Deary I De Fruyt F, Ostendorf F editors. Personality Psychology in Europe, Vol 7. Tilburg, The Netherlands: Tilburg University Press; 1999. p. 7-28.
- 26.Mandeville MY. The effects of communication on career decision making anxiety. In: The 79th Annual meeting of the Speech Communication Association. Nov. 18 - 1. Florida; 1993.
- 27.Fuqua DR, Newman JL, Seaworth TB. Relation of state and trait anxiety to different components of career indecision. J Couns Psychol. 1988;35(2):154–8. [Google Scholar]
- 28.Jones LK. Measuring a three-dimensional construct of career indecision among college students: A revision of the Vocational Decision Scale: The Career Decision Profile. J Couns Psychol. 1989;36:477–86. [Google Scholar]
- 29.Campagna CG, Curtis GJ. So worried I don’t know what to be: Anxiety is associated with increased career indecision and reduced career certainty. Aust J Guidance Counsel. 2007;17(1):91–6. [Google Scholar]
- 30.Krumboltz JD, Worthington RL. The school-to-work transition from a learning theory perspective. Career Development Quarterly. 1999;47:312–325. [Google Scholar]
- 31.Sharf RS. Applying career development theory to counseling. 2nd ed. Pacific Grove, CA: Brooks/Cole; 1997. [Google Scholar]
- 32.Mizuguchi T, Shimonaka J, Nakazato K. The Japanese Version of STAI Kyoto. Japan: Sankyoubou; 1991. [Google Scholar]
- 33.Gorenstein C, Andrade L. Validation of a Portuguese version of the Beck Depression Inventory and the State-Trait Anxiety Inventory in Brazilian subjects. Braz J Med Biol Res. 1996;29(4):453–7. [PubMed] [Google Scholar]
- 34.Colt HG, Powers A, Shanks TG. Effect of music on state anxiety scores in patients undergoing fiberoptic bronchoscopy. Chest. 1999;116(3):819–24. doi: 10.1378/chest.116.3.819. [DOI] [PubMed] [Google Scholar]
- 35.Peterlini M, Tiberio IFLC, Saadeh A, Pereira JCR, Martins MA. Anxiety and depression in the first year of medical residency training. Med Educ. 2002;36(1):66–72. doi: 10.1046/j.1365-2923.2002.01104.x. [DOI] [PubMed] [Google Scholar]
- 36.Kelly BD, Curtin PD, Corcoran M. The effects of the European Working Time Directive on surgical training: the basic surgical trainee’s perspective. Ir J Med Sci. 2011;180(2):435–7. doi: 10.1007/s11845-010-0670-4. [DOI] [PubMed] [Google Scholar]
- 37.Doherty EM, Nugent E. Personality factors and medical training: a review of the literature. Med Educ. 2011;45(2):132–40. doi: 10.1111/j.1365-2923.2010.03760.x. [DOI] [PubMed] [Google Scholar]
- 38.Buddeberg-Fischer B, Klaghofer R, Abel T, Buddeberg C. Swiss residents’ speciality choices--impact of gender, personality traits, career motivation and life goals. BMC Health Serv Res. 2006;6:137. doi: 10.1186/1472-6963-6-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.UK-Strategy-Group. Modernising medical careers: the next steps. The future shape of foundation, specialist and general practice training programmes. London: Department of Health; 2004. Available online from: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4079530. Last accessed October 2011.
- 40.Nash L, Daly M, Johnson M, Coulston C, Tennant C, van Ekert E, Walter G, Willcock S, Walton M. Personality, gender and medico-legal matters in medical practice. Australas Psychiatry. 2009;17(1):19–24. doi: 10.1080/10398560802085359. [DOI] [PubMed] [Google Scholar]


