Abstract
People with chronic pain and comorbid posttraumatic stress disorder (PTSD) report more severe pain and poorer quality of life than those with chronic pain alone. This study evaluated the extent to which associations between PTSD and chronic pain interference and severity are mediated by pain-related coping strategies and depressive symptoms. Veterans with chronic pain were divided into two groups, those with (n=65) and those without (n=136) concurrent PTSD. All participants completed measures of pain severity, interference, emotional functioning, and coping strategies. Those with current PTSD reported significantly greater pain severity and pain interference, had more symptoms of depression, and were more likely to meet diagnostic criteria for a current alcohol or substance use disorder (all p-values ≤ 0.01). Participants with PTSD reported more use of several coping strategies, including guarding, resting, relaxation, exercise/stretching, and coping self-statements. Illness-focused pain coping (i.e., guarding, resting, and asking for assistance) and depressive symptoms jointly mediated the relationship between PTSD and both pain interference (total indirect effect = 0.194, p < 0.001) and pain severity (total indirect effect = 0.153, p = 0.004). Illness-focused pain coping also evidenced specific mediating effects, independent of depression. In summary, specific pain coping strategies and depressive symptoms partially mediated the relationship between PTSD and both pain interference and severity. Future research should examine whether changes in types of coping strategies following targeted treatments predict improvements in pain-related function for chronic pain patients with concurrent PTSD.
1. Introduction
A growing body of research has examined pain-related coping strategies on adaptation to chronic pain. Pain-related coping may be defined as individuals’ attempts to manage problems associated with their pain state [14]. Pain coping strategies have been characterized as adaptive or maladaptive based on their ability to impact symptoms. Adaptive coping responses (e.g., staying active, pacing, problem solving) are often considered active; whereas maladaptive coping responses tend to be passive (e.g., resting, avoidance of activity) [25]. Maladaptive coping strategies are hypothesized to play a more important role and are more strongly related to chronic pain outcomes than adaptive coping strategies [19]. Several studies have subsequently examined this hypothesis. For example, increased use of passive coping responses following multidisciplinary pain treatment has been associated with increased disability and depression [24]. In a study of 106 military veterans with chronic pain, maladaptive responses were most strongly associated with pain interference and depression, while adaptive coping styles were significantly related to pain intensity [51].
Recently, research has focused on the prevalence and role of posttraumatic stress disorder (PTSD) in chronic pain. Patients with PTSD have more risk factors for pain, including higher rates of psychiatric and substance use disorders [29,40], as well as general medical conditions [41]. Indeed, patients with PTSD have high rates of chronic pain [6,35,47] and patients with chronic pain also have disproportionately high rates of PTSD [7,15,21,44]. Relative to patients with chronic pain alone, patients with chronic pain and comorbid PTSD report greater pain severity [20] and pain-related impairment [39]. They are also more likely to be prescribed opioid medications for pain control [39] and to have high-risk opioid use [45].
The mutual maintenance and shared vulnerability models suggest that chronic pain and PTSD symptoms interact or that patients have shared vulnerability to both conditions [2,3,46]. For example, patients with chronic pain and PTSD report significantly higher levels of maladaptive coping strategies and beliefs about pain, relative to patients with chronic pain alone [1]. Individuals with PTSD also have high rates of comorbid depression, and the biopsychosocial model posits that depressive symptoms can exacerbate or lead to increased pain and impaired function [18,52]. No study to our knowledge has explored maladaptive coping and depression as mediators of the relationship between PTSD and chronic pain.
The purpose of this study was to build on prior research by examining whether pain-related coping mechanisms and depression mediate the relationship between PTSD and pain interference and severity. Given prior empirical research documenting the role of illness-focused pain coping and depressive symptoms on pain-related outcomes [4,13,24,51,53], we conducted a multiple mediation analysis that examined the combined roles of pain coping strategies and depressive symptoms on pain interference and pain severity in a veteran patient population. We hypothesized that illness-based coping strategies and depressive symptoms would jointly mediate the relationship between PTSD and both pain interference and pain severity. We also hypothesized that patients with comorbid PTSD would have more impaired function, severe pain intensity, and psychiatric and substance abuse comorbidity.
2. Methods
This study was approved by the local Institutional Review Board and all participants provided written informed consent.
2.1. Participants
Data were collected as part of a larger cross-sectional study examining the relationship between chronic pain, substance abuse, and hepatitis C virus infection at a Veterans Affairs (VA) Medical Center. To be included, participants must have been tested for hepatitis C (patients with both positive and negative hepatitis C test results were included). Additional inclusion criteria for this study were at least 18 years of age, current self-report of chronic pain confirmed with medical record diagnosis, and ability to read and write in English. Participants were excluded if they were older than 70 years of age, or they had pending litigation or disability compensation for pain, advanced liver disease, current suicidal ideation, or untreated bipolar disorder or schizophrenia. Participants were recruited by posted advertisements in the Medical Center, letters sent to patients who had pending appointments in primary care, announcements made in mental health classes, and referral from patients being treated in the hospital’s Hepatology Clinic.
All participants signed informed consent, completed study-related tasks, and received a $30 store gift card as compensation. A total of 284 participants were recruited into the larger study. In order to examine factors associated with chronic pain, we limited the current analyses to only those participants with chronic pain. To be included, participants self-reported current pain of greater than six months duration, had treatment for a pain condition within the last five years documented in the medical record, and completed relevant study measures (n = 205) between March 2009 and August 2011.
2.2. Data Collection
Demographic characteristics were gathered including participants’ age, gender, number of years of education, annual income, and marital status. Based on their responses to a question about race/ethnicity, we classified the sample as either Caucasian or Ethnic Minority (due to limited racial/ethnic diversity).
2.3. Measures
The 64-item self-report Chronic Pain Coping Inventory (CPCI) [26] assessed the ways in which participants cope with chronic pain. Respondents are asked on how many days in the past week they used each of 64 chronic pain coping strategies. The CPCI is comprised of eight scales: guarding (Cronbach’s alpha for the current study = 0.89), resting (alpha = 0.77), asking for assistance (Cronbach’s alpha = 0.85), relaxation (Cronbach’s alpha = 0.74), task persistence (Cronbach’s alpha = 0.81), exercise/stretching (Cronbach’s alpha = 0.92), use of coping self-statements (Cronbach’s alpha = 0.92), and seeking social support (Cronbach’s alpha = 0.85). Scale scores are derived by averaging items within a respective scale, with higher scores indicating greater use of the particular coping strategy. The developers of the CPCI posited that three scales (guarding, resting, and asking for assistance) comprise the construct of “illness-focused pain coping,” while four scales (relaxation, task persistence, exercise/stretching, and use of coping self-statements) comprise the construct of “wellness-focused pain coping” [26]. The seeking social support scale of the CPCI was hypothesized to be separate from the illness-focused and wellness-focused pain coping constructs [26], has been inconsistently related to pain interference and pain severity in prior studies [23,24,43,50], and was thus excluded from the current study.
PTSD was assessed with the Posttraumatic Stress Disorders Checklist – Civilian (PCL-C) [55]. The PCL-C is a 17-item self-report measure which corresponds to diagnostic symptoms of PTSD. Participants were asked to indicate how much they have been bothered by each symptom in the past month using a 5-point (1 = Not at all, to 5 = Extremely) scale. The PCL-C has evidenced strong psychometric characteristics and reliably predicts diagnoses of PTSD [10,54]. PCL-C Cronbach’s alpha for the current study = 0.95. Participants were operationalized as having PTSD if they met three specific criteria: (1) their response to a stem question about trauma was affirmative, (2) their total score on the PCL-C was ≥ 50, and (3) consistent with diagnostic criteria, they endorsed one or more re-experiencing symptoms (PCL-C items 1 to 5), three or more avoidance symptoms (PCL-C items 6 to 12), and two or more arousal symptoms (PCL-C items 13–17) as “moderate” to “extreme” (i.e., PCL-C scores of 3 to 5).
Pain severity and pain interference were assessed with the respective subscales of Multidimensional Pain Inventory (MPI) [28]. Symptoms of depression were assessed with the Beck Depression Inventory – Second Edition (BDI-II) [5]. Each of these self-report measures has been used in numerous studies with chronic pain samples and has demonstrated good to excellent psychometric characteristics. Internal consistency for each of these measures in the current study was excellent: Cronbach’s alpha for MPI severity = 0.90, MPI interference = 0.91, BDI-II = 0.95.
Substance use disorders (SUD) were assessed with the Structured Clinical Interview for DSM-IV (SCID) [17], a semi-structured clinical interview that assesses diagnostic symptoms. A SUD was considered current if the participant met criteria for abuse or dependence to the substance within the past month. SCID interviews were conducted by masters-level research clinicians or students in graduate-level clinical psychology or social work programs. All interviewers received extensive training by a licensed psychologist. Regular supervision of SCID interviews was conducted to reduce likelihood of coder drift.
Self-reported use of prescription opioid medications in the past 30 days was assessed with the TimeLine Follow-Back (TLFB) [48]. The TLFB is a reliable and valid tool that uses calendar prompts to track the frequency of use of alcohol, illicit substances, and prescription medications.
Pain diagnoses were extracted from the electronic medical record using the Veterans Integrated Service Network-20 (VISN-20) Data Warehouse. The VISN-20 Data Warehouse contains extracts of data from the clinical records of regional VA facilities and two national VA databases. Pain diagnoses were obtained using ICD-9-CM codes listed in medical encounter records for the five years prior to the study assessment.
2.4. Statistical Analyses
Independent samples t-tests and chi-square tests of association compared demographic variables, as well as pain diagnoses, pain coping, depressive symptom severity, current substance use, pain interference, and pain severity between participants with and without a PTSD diagnosis. Bivariate correlations evaluated the associations of PTSD, illness-focused pain coping scales, wellness-focused pain coping scales, and depressive symptom severity with study outcome variables pain interference and pain severity.
Because coping was one construct hypothesized to mediate the relationship between PTSD and pain interference and pain severity, we first wanted to confirm the construct validity of illness-focused and wellness-focused pain coping in our sample. The factor structure of these constructs was assessed with two 2nd-order confirmatory factor analysis (CFA) models. The first CFA model examined model fit of the hypothesized illness-focused pain coping construct. Individual items of the guarding, resting, and asking for assistance scales were constrained to load only on the hypothesized latent construct. The three 1st-order latent constructs were then loaded on a 2nd-order “illness-focused pain coping” latent construct. A second CFA model evaluated the “wellness-focused pain coping” latent construct using similar procedures and items from the relaxation, task persistence, exercise/stretching, and coping self-statements scales of the CPCI. Model fit was assessed with Comparative Fit Index (CFI) > 0.90, Tucker Lewis Index (TLI) > 0.90, Root Mean Square Error of Approximation (RMSEA) < 0.08, and Standardized Root Mean Square Residual (SRMR) < 0.08 [12,22,31,33].
Two multiple mediation analyses evaluated the indirect effects of the independent variable, PTSD, on the dependent variables pain interference and pain severity, respectively, through the mediators pain coping and depression. Multiple mediation is an extension of simple mediation analyses and allows for the evaluation of two or more mediators simultaneously in a model [42]. Path analysis is typically used for multiple mediation models that contain only measured variables; however, structural equation models can also be used when the independent, mediating, and/or dependent variables are latent constructs [32]. We have labeled the paths in the figures depicting the mediation model a, b, and c’ to be consistent with the mediation literature, where a is the effect of the independent variable on the mediator, b is the effect of the mediator on the dependent variable, and c′ is the effect of the independent variable on the dependent variable after accounting for mediation (i.e., the “direct effect”). For mediation analyses, the independent variable PTSD, mediator depressive symptom severity, and dependent variables pain interference and pain severity were manifest/observed variables. Pain coping mediators were treated as a latent constructs derived from CPCI scale scores.
We followed recommendations by Preacher and Hayes [42] and assessed the total (i.e., combined) mediating effect of pain coping and depressive symptom severity and the individual (i.e., specific) mediating effect of each putative mediator. To evaluate the magnitude of the indirect effects, we used the product-of-coefficients approach [8] to calculate standard errors of the indirect effects. In this approach, the indirect effect is divided by its standard error and compared to a critical value using a Z-test. We employed bootstrapping procedures [42] with a total of n = 5,000 bootstrapped samples to corroborate findings from the product-of-coefficients tests.
Finally, within a structural equation modeling framework, we examined the relationship between pain coping and specific PTSD symptom clusters (i.e., re-experiencing, avoidance, and arousal) among the full study sample and among the subset of participants diagnosed with PTSD. Specifically, we computed PTSD symptom cluster scores by summing PCL-C items (re-experiencing symptoms = items 1 through 5; avoidance symptoms = items 6 through 12; arousal symptoms = items 13 through 17). Each symptom cluster was correlated with pain coping latent constructs.
Descriptive and bivariate analyses were conducted using SPSS version 18, while CFA models, multiple mediation analyses, and correlations between PTSD symptom clusters and pain coping latent constructs were conducted using Mplus version 6. An α-level of 0.05 and two-tailed tests of significance were used for all statistical analyses.
3. Results
We were unable to determine PTSD diagnosis for 4 of 205 participants due to non-response to one or more PTSD questions. We excluded these four participants from all analyses, resulting in our final analytic sample of n = 201 participants with chronic pain.
Tables 1 and 2 provide descriptive statistics for demographic variables, pain diagnoses, mental health functioning, pain coping, pain interference, and pain severity for the full sample and the subsamples of participants with and without concurrent PTSD, as well as bivariate statistical comparisons between the subsamples. Sixty-five participants (32%) met study criteria for PTSD and chronic pain. Participants with and without PTSD did not significantly differ on any demographic characteristic. Participants with PTSD reported significantly greater pain severity, pain interference, and had more symptoms of depression relative to participants without PTSD (all p-values ≤ 0.001). In addition, a greater proportion of participants with PTSD met diagnostic criteria for a current alcohol or substance use disorder (28% versus 11%, p = 0.003).
Table 1.
Comparison of demographic characteristics and pain diagnoses.
| Full Sample (n=201) | Pain and PTSD (n=65) | Pain Only (n=136) | p-value | |
|---|---|---|---|---|
| Demographic Characteristics | ||||
| Age | 54.9 (7.6) | 53.8 (7.5) | 55.5 (7.7) | 0.159 |
| Male gender | 92.0% (185) | 92.3% (60) | 91.9% (125) | 0.923 |
| White race | 77.6% (156) | 76.9% (50) | 77.9% (106) | 0.871 |
| Marital status | 0.561 | |||
| Single | 22.0% (44) | 26.2% (17) | 20.0% (27) | |
| Married | 23.5% (47) | 18.5% (12) | 25.9% (35) | |
| Separated/Divorced | 49.5% (99) | 49.2% (32) | 49.6% (67) | |
| Widowed | 5.0% (10) | 6.2% (4) | 4.4% (6) | |
| Greater than 12 years of education | 77.1% (155) | 76.9% (50) | 77.2% (105) | 0.964 |
| Annual income less than $15,000 | 58.7% (118) | 56.9% (37) | 59.6% (81) | 0.723 |
| Pain Diagnoses | ||||
| Neck or Joint Pain | 82.6% (166) | 83.1% (54) | 82.4% (112) | 0.899 |
| Low Back Pain | 62.7% (126) | 78.5% (51) | 55.1% (7475 | 0.001 |
| Rheumatism/Arthritis | 58.7% (118) | 63.1% (41) | 56.6% (77) | 0.384 |
| Headache | 20.9% (42) | 27.7% (18) | 17.6% (24) | 0.101 |
| Neuropathy | 10.9% (22) | 7.7% (5) | 12.5% (17) | 0.307 |
| Fibromyalgia | 10.4% (21) | 12.3% (8) | 9.6% (13) | 0.551 |
Note. Column values indicate % (n) for categorical variables or Mean (Standard Deviation) for continuous variables.
Table 2.
Comparison of mental health functioning, pain coping, pain interference, and pain severity.
| Full Sample (n=201) | Pain and PTSD (n=65) | Pain Only (n=136) | p-value | |
|---|---|---|---|---|
| Mental Health Functioning | ||||
| Beck Depression Inventory–II | 17.3 (12.6) | 26.6 (12.2) | 12.9(10.2) | < 0.001 |
| Current Substance Use Disorder | 16.4% (33) | 27.7% (18) | 11.0% (15) | 0.003 |
| Chronic Pain Coping | ||||
| Guarding | 3.3 (2.0) | 3.8 (1.9) | 3.1 (2.0) | 0.015 |
| Resting | 3.6 (1.7) | 4.0 (1.5) | 3.4 (1.8) | 0.020 |
| Asking for assistance | 1.7 (1.9) | 2.0 (2.0) | 1.6 (1.8) | 0.100 |
| Relaxation | 1.9 (1.4) | 2.3 (1.5) | 1.8 (1.4) | 0.022 |
| Task persistence | 3.7 (1.8) | 3.9 (1.7) | 3.6 (1.9) | 0.233 |
| Exercise/Stretching | 2.3 (1.9) | 2.7 (2.1) | 2.1 (1.8) | 0.048 |
| Coping self-statements | 3.2 (2.0) | 3.7 (1.9) | 2.9 (2.0) | 0.009 |
| Pain Outcome Variables | ||||
| MPI Pain Interference | 3.5 (1.7) | 4.3 (1.5) | 3.1 (1.7) | < 0.001 |
| MPI Pain Severity | 3.1 (1.6) | 3.7 (1.4) | 2.9 (1.6) | 0.001 |
Note. Column values indicate Mean (Standard Deviation) for continuous variables or % (n) for categorical variables. MPI = Multidimensional Pain Inventory.
The most common pain diagnoses in the full sample were chronic neck or joint pain (83%), chronic low back pain (63%), and rheumatism/arthritis (59%). Participants, on average, were diagnosed with a pain problem 14.1 years ago (SD = 11.9 years). Participants with PTSD were more likely to be diagnosed with chronic back pain (79% versus 55%, p = 0.001) but did not differ from participants without PTSD on other pain diagnoses. Participants with PTSD were more likely to report having taken prescription opioid medications in the past month, compared to participants without PTSD (51% versus 29%, p = 0.003). Participants with PTSD used a variety of both illness-focused (i.e., guarding, resting) and wellness-focused (i.e., relaxation, exercise/stretching, coping self-statements) pain coping strategies to a greater extent than participants without PTSD (Table 2).
3.1. Mediation Analyses
The 2nd-order CFA model for illness-focused pain coping fit the data well (CFI = 0.91, TLI = 0.90, RMSEA = 0.07 [95% CI = 0.06–0.08], SRMR = 0.07). All individual CPCI items in the guarding, resting, and asking for assistance scales significantly loaded on the hypothesized latent construct (all p’s < 0.001, path coefficients not reported). In addition, 1st-order latent constructs significantly loaded on the hypothesized 2nd-order latent construct of illness-focused pain coping (all p’s < 0.001, path coefficients not reported). The 2nd-order CFA model of wellness-focused pain coping evidenced significant 1st- and 2nd-order loadings (all p’s < 0.001, path coefficients not reported). However, the model did not meet minimum fit criteria (CFI = 0.85, TLI = 0.84, RMSEA = 0.07 [95% CI = 0.06–0.08], SRMR = 0.07). Because the hypothesized construct of wellness-focused pain coping was not supported by the 2nd-order CFA model, this latent variable was not included as a potential mediator in subsequent analyses or in analyses examining the relationship between PTSD symptom clusters and pain coping. As can be seen in Table 3, PTSD and purported mediating variables depressive symptom severity and illness-focused pain coping strategies (i.e., guarding, resting, and asking for assistance scales of the CPCI) were all positively correlated with the dependent variables pain interference and pain severity.
Table 3.
Bivariate correlation matrix for PTSD diagnosis, PTSD symptom clusters, hypothesized mediators, and pain-related dependent variables (n = 201).a
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Independent Variable | ||||||||||
| 1. PTSD Diagnosis | 1 | |||||||||
| 2. PTSD Re-Experiencing | 0.770** | 1 | ||||||||
| 3. PTSD Avoidance | 0.766** | 0.783** | 1 | |||||||
| 4. PTSD Arousal | 0.776** | 0.780** | 0.775** | 1 | ||||||
| Mediators | ||||||||||
| 5. Depressive Symptom Severity | 0.510** | 0.580** | 0.709** | 0.648** | 1 | |||||
| 6. CPCI Guarding | 0.172* | 0.179* | 0.320** | 0.217** | 0.346** | 1 | ||||
| 7. CPCI Resting | 0.164* | 0.176* | 0.235** | 0.250** | 0.262** | 0.561** | 1 | |||
| 8. CPCI Asking for Assistance | 0.116 | 0.154* | 0.227** | 0.181* | 0.182** | 0.467** | 0.383** | 1 | ||
| Dependent Variables | ||||||||||
| 9. MPI Pain Interference | 0.334** | 0.347** | 0.452** | 0.393** | 0.447** | 0.664** | 0.402** | 0.383** | 1 | |
| 10. MPI Pain Severity | 0.243* | 0.267** | 0.268** | 0.296** | 0.340** | 0.578** | 0.355** | 0.343** | 0.805** | 1 |
= p < 0.05,
= p < 0.01.
Thirty-one participants did not endorse prior trauma and thus did not respond to PCL-C items.
Correlations between PTSD symptom clusters (i.e., PTSD re-experiencing, avoidance, and arousal) and other variables thus represent a sample size of n = 170. CPCI = Chronic Pain Coping Inventory; MPI = Multidimensional Pain Inventory.
Figure 1 displays the mediation model for the dependent variable pain interference. PTSD had a significant total effect on pain interference (c = 0.334, p < 0.001). A significant proportion of this effect occurred indirectly through illness-focused pain coping and depressive symptom severity (total indirect effect = 0.194, p < 0.001). In addition, significant indirect effects occurred for both illness-focused pain coping (specific indirect effect = 0.126, p = 0.011) and depressive symptom severity (specific indirect effect = 0.068, p = 0.021). A direct effect of PTSD on pain interference remained statistically significant after accounting for indirect mediation effects (c′ = 0.140, p = 0.016).
Figure 1.
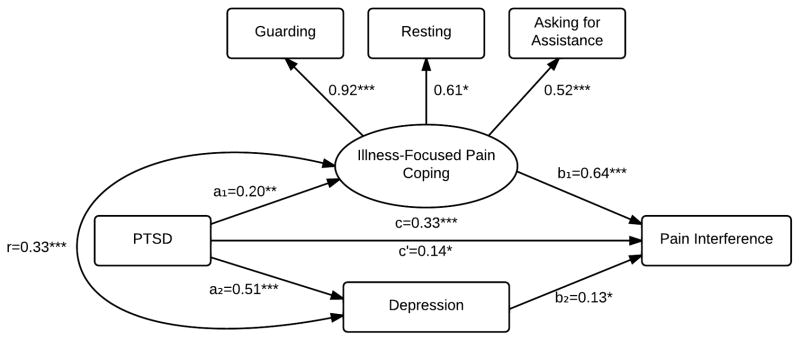
Mediation model for PTSD and pain interference.
Note. * = p < 0.05. ** = p < 0.01. *** = p < 0.001.
Figure 2 depicts the mediation model for the dependent variable pain severity. PTSD had a significant total effect on pain severity (c = 0.243, p < 0.001), and combined illness-focused pain coping and depressive symptom severity accounted for a significant indirect effect (total indirect effect = 0.153, p = 0.004). An examination of specific indirect effects indicated that illness-focused pain coping significantly mediated the effect of PTSD on pain severity (specific indirect effect = 0.119, p = 0.012); however, depressive symptom severity did not (specific indirect effect = 0.034, p = 0.319). The direct effect of PTSD on pain severity after accounting for the total indirect mediating effects was no longer statistically significant (c′ = 0.090, p = 0.174).
Figure 2.
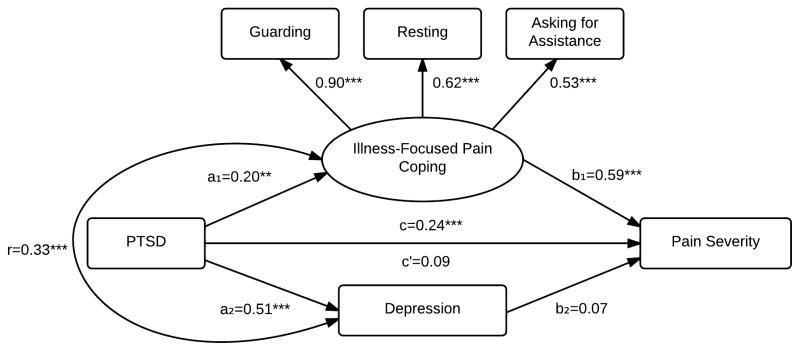
Mediation model for PTSD and pain severity.
Note. * = p < 0.05. ** = p < 0.01. *** = p < 0.001.
Table 4 provides sample statistics for indirect effects of both mediation models computed through product-of-coefficient and bootstrapping procedures. Bootstrapping procedures corroborated the findings of product-of-coefficient analyses. All 95% confidence intervals of the indirect effect point estimates excluded zero, with the exception of the indirect effect of depressive symptom severity, on the relationship between PTSD and pain severity, which was also non-significant in product-of-coefficient analyses.
Table 4.
Indirect effects of PTSD on (a) pain interference and (b) pain severity via illness-focused pain coping and depressive symptom severity.
| Point Estimate | Product-of-Coefficients | Bootstrapping
|
|||
|---|---|---|---|---|---|
| 95% Confidence Interval | |||||
|
| |||||
| SE | Z | Lower 2.5% | Upper 2.5% | ||
| a. Pain Interference | |||||
| Total indirect effects | 0.194 | 0.051 | 3.801 | 0.094 | 0.294 |
| Illness-focused coping | 0.126 | 0.049 | 2.556 | 0.029 | 0.222 |
| Depressive symptom severity | 0.068 | 0.029 | 2.314 | 0.010 | 0.125 |
|
| |||||
| b. Pain Severity | |||||
| Total indirect effects | 0.153 | 0.053 | 2.890 | 0.049 | 0.257 |
| Illness-focused coping | 0.119 | 0.048 | 2.512 | 0.026 | 0.212 |
| Depressive symptom severity | 0.034 | 0.034 | 0.996 | −0.033 | 0.101 |
3.2. Association between Illness-Focused Pain Coping and PTSD Symptom Clusters
Thirty-one participants did not endorse any prior trauma and thus did not respond to PCL-C items. Of the n = 170 participants who completed the PCL-C, PTSD re-experiencing, avoidance, and arousal symptoms were all significantly related to illness-focused pain coping (r = 0.244, p = 0.004 for re-experiencing; r = 0.382, p < 0.001 for avoidance; r = 0.311, p < 0.001 for arousal). Among the 65 participants who met criteria for PTSD, avoidance symptoms were significantly related to illness-focused pain coping (r = 0.304, p = 0.020). However, PTSD re-experiencing and arousal symptoms were unrelated to illness-focused pain coping (r = 0.014, p = 0.931 for re-experiencing symptoms; r = 0.113, p = 0.461 for arousal symptoms).
4. Discussion
Maladaptive coping strategies have been hypothesized to lead to poorer pain-related outcomes [19], and past research has indicated that patients with PTSD and chronic pain employ greater use of maladaptive pain coping strategies than patients with chronic pain alone [1]. The present results build on prior research by indicating that the use of maladaptive pain coping styles in patients with PTSD and chronic pain contribute to more pain interference and greater pain severity. This finding is consistent with previous research that has implicated maladaptive coping styles in the exacerbation of pain-related dysfunction in patients with a variety of chronic pain conditions [24,27,37,43].
Our results suggest that illness-focused pain coping styles mediate the relationship of PTSD with pain interference and pain severity. Our findings are consistent with mutual maintenance and shared vulnerability models of PTSD and chronic pain. The possibility of mutual maintenance has been supported by data indicating that pain has a mediating influence on re-experience and hyperarousal symptoms in PTSD, and PTSD-related hyperarousal mediates pain symptoms [30]. Shared emotional and physiological responses to stress, including hyperarousal, may predispose individuals to maladaptive coping and avoidance behaviors [3]. For example, anxiety sensitivity, which encompasses fear of anxiety reactions and fear of somatic sensations, is elevated in people with PTSD and some patients with chronic pain [2,3]. Our data indicate that PTSD symptoms, particularly avoidance symptoms, may predispose individuals to use analogous chronic pain coping strategies, such as guarding and resting. This finding is consistent with prior research, which found that PTSD avoidance symptoms predicted pain disability [34]. Prospective studies are needed, however, to determine causal directions between PTSD symptoms, chronic pain, and coping strategies.
Participants with PTSD and chronic pain in this study reported more frequent use of both illness-focused and wellness-focused pain coping styles. The increased use of both types of coping strategies by patients with PTSD may indicate general help-seeking behaviors [11], increased distress, or may have been acquired coping skills learned through specialty PTSD treatment (though past PTSD treatment utilization was not assessed in the current study). Our results suggest that illness-focused pain coping is significantly associated with pain interference and pain severity. Although wellness-focused coping is hypothesized to be associated with improved adjustment to pain, we did not include wellness-focused pain coping as a potential mediator in these analyses because the latent variable was not supported by the confirmatory factors analysis, indicating that in this sample the effects of wellness-focused pain coping could not be assessed. Prior findings on relationships between wellness-focused pain coping and pain-related outcomes have been inconsistent [16,23,24,27,37,43,49,50,51], suggesting that further research on the definition and components of this construct is needed to confirm its clinical relevance. Future clinical investigations may also emphasize competence and self-control, or self-efficacy for managing pain, with less focus on the specific coping strategies.
In addition to pain coping, we also examined the impact of depressive symptoms on both pain interference and pain severity. Depressive symptoms had an independent mediating effect on pain interference, but contrary to our hypotheses, not on pain severity. Symptoms of depression such as anhedonia and fatigue may lead to disengagement from activities of daily living, and patients with PTSD and chronic pain who experience these symptoms may perceive greater pain interference that is related, at least in part, to depressive symptoms. Thus, depression may be an active contributor to pain-related interference in patients with PTSD and comorbid chronic pain. Although prospective studies would be needed to verify the temporal relationships between these variables, our findings suggest that the treatment of depression may improve pain-related functioning, despite having modest to little impact on perceived severity of pain. This is consistent with a psychological treatment approach within a biopsychosocial model of pain management [18].
In this sample of U.S. military veterans with chronic pain, 32% had comorbid PTSD. Participants with PTSD reported more severe pain, poorer pain-related function, had more symptoms of depression, and were more likely to meet diagnostic criteria for a current alcohol or substance use disorder. Participants with PTSD were also more likely to have taken prescription opioid medications for pain in the past month. These data are consistent with prior research [39,45,47] and indicate that patients with chronic pain and comorbid PTSD present with a constellation of clinical concerns.
Cognitive-behavior therapy (CBT) based interventions have independently been shown to be effective for chronic pain [52] and for PTSD [9]. Integrated cognitive and behavioral techniques that simultaneously address symptoms of PTSD and chronic pain may help maximize effectiveness. A program that combines cognitive processing therapy, a cognitive-behavioral evidence-based treatment for PTSD, with CBT for chronic pain has some preliminary support [38]. The U.S. military is testing an integrated treatment that combines functional restoration for chronic pain with prolonged exposure, another evidence-based cognitive-behavioral approach for PTSD [36]. Additional research is needed to determine the overall impact of a combined intervention, relative to an active control, and to evaluate its essential components.
There are several limitations that should be considered in the interpretation of study results. The cross-sectional design prevents causal inference and prospective research is needed to confirm our findings. In addition, sample characteristics may limit generalizability of the results. In particular, all participants had a history of being tested for the hepatitis C virus and likely have higher rates of current and past risky alcohol and substance use behaviors than samples of patients recruited from primary care or specialty pain clinics. Substance use may be a maladaptive coping mechanism for pain, which we did not assess. We also did not obtain data on characteristics or etiology of PTSD-related trauma (such as duration or cause), which could have an impact on the presentation of PTSD symptoms. Our sample was comprised of U.S. military veterans and was predominately male. Replication of the results in other samples would add confidence in study findings.
In summary, we found evidence that patients with PTSD and chronic pain had more severe pain and poorer pain-related functioning than patients with chronic pain alone. We also found evidence that illness-focused pain coping styles mediate the effect of PTSD on both pain interference and pain severity among patients with PTSD and chronic pain. Depressive symptoms mediated the effect of PTSD on pain interference, but not pain severity. Illness-focused coping styles and depressive symptoms in patients with chronic pain and comorbid PTSD may be a useful target for treatment through multimodal PTSD symptom and pain management approaches.
Summary.
We found that illness-focused pain coping mediated the relationship between posttraumatic stress disorder and both pain interference and pain severity.
Acknowledgments
This study was supported in part by award K23DA023467 from the National Institute on Drug Abuse to Dr. Morasco. The work was supported with resources and the use of facilities at the Portland VA Medical Center. During the past 12 months, Dr. Turk has received research support from Endo, Johnson & Johnson, Philips Respironics, and the National Institutes of Health, and consulting fees from Eli Lilly, Empi, Johnson & Johnson, Pfizer, Philips Respironics, and SK LifeScience. He is also a Special Government Employee of the U.S. Food and Drug Administration.
Footnotes
No other author reports having any potential conflict of interest with this study.
The authors appreciate the assistance of Susan Gritzner, Renee Cavanagh, and Aysha Crain with data collection, and Jonathan Duckart, MPS, for extracting data from the electronic medical record. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Veterans Affairs or the National Institute on Drug Abuse.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Alschuler KN, Otis JD. Coping strategies and beliefs about pain in veterans with comorbid chronic pain and significant levels of posttraumatic stress disorder symptoms. Eur J Pain. 2012;16:312–319. doi: 10.1016/j.ejpain.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 2.Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47:930–937. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- 3.Asmundson GJ, Katz J. Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depress Anxiety. 2009;26:888–901. doi: 10.1002/da.20600. [DOI] [PubMed] [Google Scholar]
- 4.Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TQ, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004;66:17–22. doi: 10.1097/01.psy.0000106883.94059.c5. [DOI] [PubMed] [Google Scholar]
- 5.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 6.Beckham JC, Crawford AL, Feldman ME, Kirby AC, Hertzberg MA, Davidson JR, Moore SD. Chronic posttraumatic stress disorder and chronic pain in Vietnam combat veterans. J Psychosom Res. 1997;43:379–389. doi: 10.1016/s0022-3999(97)00129-3. [DOI] [PubMed] [Google Scholar]
- 7.Benedikt RA, Kolb LC. Preliminary findings on chronic pain and posttraumatic stress disorder. Am J Psychiatry. 1986;143:908–910. doi: 10.1176/ajp.143.7.908. [DOI] [PubMed] [Google Scholar]
- 8.Bishop YMM, Fienberg SE, Holland PW. Discrete multivariate analysis: theory and practice. Cambridge, MA: MIT Press; 1975. [Google Scholar]
- 9.Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2007;190:97–104. doi: 10.1192/bjp.bp.106.021402. [DOI] [PubMed] [Google Scholar]
- 10.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behavioral Res Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 11.Calhoun PS, Bosworth HB, Grambow SC, Dudley TC, Beckham JC. Medical service utilization by veterans seeking help for posttraumatic stress disorder. Am J Psychiatry. 2002;159:2081–2086. doi: 10.1176/appi.ajp.159.12.2081. [DOI] [PubMed] [Google Scholar]
- 12.Cheung GW, Rensvold RB. The effects of model parsimony and sampling error on the fit of structural equation models. Organ Res Methods. 2001;4:236–264. [Google Scholar]
- 13.Currie SR, Wang JL. Chronic back pain and major depression in the general Canadian population. Pain. 2004;107:54–60. doi: 10.1016/j.pain.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 14.DeGood D, Tait R. Assessment of pain beliefs and pain coping. In: Turk DC, Melzack R, editors. Handbook of Pain Assessment. New York, NY: Guilford Press; 2011. pp. 320–334. [Google Scholar]
- 15.Dunn AS, Julian T, Formolo LR, Green BN, Chicoine DR. Preliminary analysis of posttraumatic stress disorder screening within specialty clinic setting for OIF/OEF veterans seeking care for neck or back pain. J Rehabil Res Dev. 2011;48:493–502. doi: 10.1682/jrrd.2010.05.0104. [DOI] [PubMed] [Google Scholar]
- 16.Ersek M, Turner JA, Kemp CA. Use of the Chronic Pain Coping Inventory to assess older adults’ pain coping strategies. J Pain. 2006;7:833–842. doi: 10.1016/j.jpain.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 17.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for the DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; Nov, 2002. [Google Scholar]
- 18.Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133:581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- 19.Geisser M, Robinson M, Riley J., III Pain beliefs, coping, and adjustment to chronic pain: let’s focus more on the negative. Pain Forum. 1999;8:161–168. [Google Scholar]
- 20.Geisser ME, Roth RS, Bachman JE, Eckert TA. The relationship between symptoms of post-traumatic stress disorder and pain, affective disturbance and disability among patients with accident and non-accident related pain. Pain. 1996;66:207–214. doi: 10.1016/0304-3959(96)03038-2. [DOI] [PubMed] [Google Scholar]
- 21.Hickling EJ, Blanchard EB, Silverman DJ, Schwarz SP. Motor vehicle accidents, headaches and post-traumatic stress disorder: assessment findings in a consecutive series. Headache. 1992;32:147–151. doi: 10.1111/j.1526-4610.1992.hed3203147.x. [DOI] [PubMed] [Google Scholar]
- 22.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Eq Modeling. 1999;6:1–55. [Google Scholar]
- 23.Jensen MP, Engel JM, Schwartz L. Coping with cerebral palsy pain: a preliminary longitudinal study. Pain Med. 2006;7:30–37. doi: 10.1111/j.1526-4637.2006.00086.x. [DOI] [PubMed] [Google Scholar]
- 24.Jensen MP, Turner JA, Romano JM. Changes after multidisciplinary pain treatment in patient pain beliefs and coping are associated with concurrent changes in patient functioning. Pain. 2007;131:38–47. doi: 10.1016/j.pain.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jensen MP, Turner JA, Romano JM, Nielson WR. Chronic Pain Coping Inventory: Professional Manual. Lutz, FL: Psychological Assessment Resources; 2008. [Google Scholar]
- 26.Jensen MP, Turner JA, Romano JM, Strom SE. The Chronic Pain Coping Inventory: development and preliminary validation. Pain. 1995;60:203–216. doi: 10.1016/0304-3959(94)00118-X. [DOI] [PubMed] [Google Scholar]
- 27.Karsdop PA, Vlaeyen JWS. Active avoidance but not activity pacing is associated with disability in fibromyalgia. Pain. 2009;147:29–235. doi: 10.1016/j.pain.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 28.Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 29.Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- 30.Liedl A, O’Donnell M, Creamer M, Silove D, McFarlane A, Knaevelsrud C, Bryant RA. Support for the mutual maintenance of pain and post-traumatic stress disorder symptoms. Psychol Med. 2010;40:1215–1223. doi: 10.1017/S0033291709991310. [DOI] [PubMed] [Google Scholar]
- 31.MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psych Methods. 1996;1:130–149. [Google Scholar]
- 32.MacKinnon DP. Introduction to statistical mediation. New York, NY: Taylor & Francis; 2008. [Google Scholar]
- 33.Marsh HW, Hau K, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Struct Eq Modeling. 2004;11:320–341. [Google Scholar]
- 34.Martin AL, Halket E, Asmundson GJG, Flora DB, Katz J. Posttraumatic stress symptoms and the diathesis-stress model of chronic pain and disability in patients undergoing major surgery. Clin J Pain. 2010;26:518–527. doi: 10.1097/AJP.0b013e3181e15b98. [DOI] [PubMed] [Google Scholar]
- 35.McFarlane AC, Atchison M, Rafalowicz E, Papay P. Physical symptoms in post-traumatic stress disorder. J Psychosom Res. 1994;38:715–26. doi: 10.1016/0022-3999(94)90024-8. [DOI] [PubMed] [Google Scholar]
- 36.McGeary D, Moore M, Vriend CA, Peterson AL, Gatchel RJ. The evaluation and treatment of comorbid pain and PTSD in a military setting: an overview. J Clin Psychol Med Settings. 2011;18:155–163. doi: 10.1007/s10880-011-9236-5. [DOI] [PubMed] [Google Scholar]
- 37.Miro J, Raichle KA, Carter GT, O’Brien SA, Abresch RT, McDonald CM, Jensen MP. Impact of biopsychosocial factors on chronic pain in persons with myotonic and facioscapulohumeral muscular dystrophy. Rehabilitation Medicine and Palliative Care. 2009;26:308–319. doi: 10.1177/1049909109335146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Otis JD, Keane TM, Kerns RD, Monson C, Scioli E. The development of an integrated treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Med. 2009;10:1300–1311. doi: 10.1111/j.1526-4637.2009.00715.x. [DOI] [PubMed] [Google Scholar]
- 39.Phifer J, Skelton K, Weiss T, Schwartz AC, Wingo A, Gillespie CF, Sands LA, Sayyar S, Bradley B, Jovanovic T, Ressler KJ. Pain symptomatology and pain medication use in civilian PTSD. Pain. 2011;152:2233–2240. doi: 10.1016/j.pain.2011.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25:456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Medical comorbidity of full and partial posttraumatic stress disorder in US adults: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom Med. 2011;73:697–707. doi: 10.1097/PSY.0b013e3182303775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 43.Raichle KA, Hanley M, Jensen MP, Cardenas DD. Cognitions, coping, and social environment predict adjustment to pain in spinal cord injury. J Pain. 2007;8:718–729. doi: 10.1016/j.jpain.2007.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44:4–19. doi: 10.3109/00048670903393597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Seal KH, Shi Y, Cohen G, Cohen BE, Maguen S, Krebs EE, Neylan TC. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307:940–947. doi: 10.1001/jama.2012.234. [DOI] [PubMed] [Google Scholar]
- 46.Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin Psychol Rev. 2001;21:857–877. doi: 10.1016/s0272-7358(00)00071-4. [DOI] [PubMed] [Google Scholar]
- 47.Shipherd JC, Keyes M, Jovanovic T, Ready DJ, Baltzell D, Worley V, Gordon-Brown V, Hayslett C, Duncan E. Veterans seeking treatment for posttraumatic stress disorder: what about comorbid chronic pain? J Rehabil Res Dev. 2007;44:153–166. doi: 10.1682/jrrd.2006.06.0065. [DOI] [PubMed] [Google Scholar]
- 48.Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Litton RZ, Allen JP, editors. Measuring alcohol consumption: psychosocial and biochemical methods. New Jersey: Human Press; 1992. pp. 41–72. [Google Scholar]
- 49.Tan G, Jensen MP, Robinson-Whelen S, Thornby JI, Monga TN. Coping with pain: a comparison of two measures. Pain. 2001;90:127–133. doi: 10.1016/s0304-3959(00)00395-x. [DOI] [PubMed] [Google Scholar]
- 50.Tan G, Nguyen Q, Anderson KO, Jensen M, Thornby J. Further validation of the Chronic Pain Coping Inventory. J Pain. 2005;6:29–41. doi: 10.1016/j.jpain.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 51.Tan G, Teo I, Anderson KO, Jensen MP. Adaptive versus maladaptive coping and beliefs and their relation to chronic pain adjustment. Clin J Pain. 2011;27:769–774. doi: 10.1097/AJP.0b013e31821d8f5a. [DOI] [PubMed] [Google Scholar]
- 52.Turk DC, Wilson HD, Cahana A. Treatment of chronic non-cancer pain. Lancet. 2011;377:2226–2235. doi: 10.1016/S0140-6736(11)60402-9. [DOI] [PubMed] [Google Scholar]
- 53.Von Korff M, Le Resche L, Dworkin SF. First onset of common pain symptoms: a prospective study of depression as a risk factor. Pain. 1993;55:251–258. doi: 10.1016/0304-3959(93)90154-H. [DOI] [PubMed] [Google Scholar]
- 54.Weathers FW, Ford J. Psychometric properties of the PTSD Checklist (PCL–C, PCL–S, PCL–M, PCL–PR) In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Foundation & Press; 1996. pp. 250–252. [Google Scholar]
- 55.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. Paper presented at the Annual Meeting of International Society for Traumatic Stress Studies; San Antonio, TX. October, 1993. [Google Scholar]


