Abstract
Purpose
The purpose of this study was to examine retrospectively the effectiveness of Sugioka’s transtrochanteric valgus osteotomy (TVO) combined with the shelf procedure for patients who had advanced osteoarthritis (OA) of the hip with severe acetabular dysplasia.
Methods
Sixty-two hips in 61 patients were reviewed retrospectively between April 1993 and March 2009. Of these hips, 25 hips with the pre-operative acetabular head index (AHI) ≥ 60 % (single group) underwent a TVO, whereas the other 37 with AHI < 60 % (combined group) underwent a TVO combined with the shelf procedure.
Results
Using conversion to total hip arthroplasty as the endpoint, the Kaplan-Meier survival rates at ten years were calculated to be 85.5 % for the single group and 100 % for the combined group; there was a significant difference between the two groups (p < 0.05, log-rank test). Similarly, calculated using progressive OA as the endpoint, survival rates at ten years were 69.5 % and 89.3 % respectively; there was also a significant difference between the two groups (p < 0.05, log-rank test). In the single group, the latest radiographic evaluations of the patients with the pre-operative AHI ≥ 70 % were significantly better than those of the patients with the pre-operative AHI < 70 % (P < 0.05).
Conclusion
More satisfactory ten year results of TVO were obtained in cases that had a pre-operative AHI of ≥70 %, or where the shelf procedure was added. It is desirable that acetabuloplasty be added for patients with pre-operative AHI < 70 %.
There continues to be controversy surrounding the topic of optimal treatment for advanced osteoarthritis (OA) of the hip in young patients. From the viewpoint of pain relief and early recovery, total hip arthroplasty (THA) tends to be the chosen treatment for advanced OA. However, long-term results of THA for these patients, even though they have improved due to advances in the prosthesis and surgical techniques [1], are considered to be poorer due to the long lifespan: serious problems such as loosening and osteolysis with regard to limited durability remain unsolved, and these problems account for the need for revision of THA [2, 3]. To avoid frequent revision of THA for these patients, joint-preserving surgery should be indicated as much as possible.
Acetabular dysplasia is the most common cause of secondary OA [4], in which pelvic osteotomy, such as rotational acetabular osteotomy (RAO) or peri-acetabular osteotomy (PAO), may be carried out. However, these joint-preserving operations are rarely effective for advanced OA [5–7].
Since Pauwels reported the procedure of femoral valgus osteotomy as the best treatment for advanced OA, this procedure has been widely developed as Pauwels’ intertrochanteric valgus osteotomy [8]. Several modified procedures were also reported, including Bombelli’s intertrochanteric valgus-extension osteotomy [9–12], the intertrochanteric valgus-flexion osteotomy by Itoman et al. [13], and Sugioka’s transtrochanteric valgus osteotomy (TVO) [14, 15].
Many studies of the results of valgus osteotomies for advanced OA have been described with a mean follow-up of ten to 25 years [9–13, 15, 16]. Among these studies, for severe acetabular dysplasia, additional acetabuloplasty such as the shelf procedure or Chiari pelvic osteotomy is recommended [11–13, 15], because acetabular coverage remains insufficient after osteotomy, thereby allowing further lateralization of the head of OA [13, 17]. Nevertheless, to our knowledge, studies of the comparison between valgus osteotomy alone and the procedure combined with acetabuloplasty for the treatment of advanced OA have been limited [12, 13].
In this study, we performed Sugioka’s TVO for patients younger than 60 years old with advanced OA, and we added acetabuloplasty using the shelf procedure during TVO for patients with severe acetabular dysplasia.
The purpose of this study was to examine retrospectively the effectiveness of Sugioka’s TVO combined with the shelf procedure for patients who had advanced OA with severe acetabular dysplasia.
Patients and methods
Patients
We retrospectively reviewed 62 hips (61 patients) that had Sugioka’s TVO for advanced OA secondary to acetabular dysplasia between April 1993 and March 2009. The mean age of the patients at surgery was 46.3 years (27–58 years). There were nine men and 52 women. The mean duration of follow-up was 10.7 years (3–18.5 years). 23 patients had unilateral OA, and 38 patients had bilateral OA.
When the acetabular head index (AHI) of Heyman and Herndon [18] pre-operatively was less than 60 %, a shelf procedure was added. TVO alone was carried out for patients whose AHI was more than 60 %. When the AHI was measured, a roof osteophyte was included in the acetabulum. Twenty-five hips (24 patients) had TVO alone (single group), and 37 hips (37 patients) had TVO combined with the shelf procedure (combined group). The shelf procedure was carried out with the modified Spitzy-Katayama procedure [12].
The mean age of the patients at the time of surgery was 45.8 years (range, 27–56) in the single group, and 46.6 years (range, 37–58) in the combined group. There were six men and 18 women in the single group, and three men and 34 women in the combined group. The mean duration of follow-up was 10.7 years (range, three to 18.5) in the single group, and 10.8 years (range, 5.6–18.5) in the combined group. The Fisher exact test in the pre-operative period showed no statistical difference between the two groups in terms of patient profile (sex difference, p = 0.086; opposite side involvement, p =0.74). The Mann–Whitney U test also showed no significant difference between the two groups in terms of age (p = 0.92) and follow-up period (p = 0.90). The average osteotomy angles in the single group and combined group were 23.3° (range, 20°–30°) and 23.5° (range, 20°–30°) respectively. The Mann–Whitney U test also showed no significant difference between the two groups in terms of the osteotomy angle (p = 0.95).
Indication of transtrochanteric valgus osteotomy
Indications of TVO were as follows: Hinge abduction can be observed on a dynamic radiogram (with adduction, the lateral joint space can open wide); Full weight bearing of the contra-lateral side; Flexion > 60°; Patients < 60 years of age.
Postoperative and rehabilitation protocol
The postoperative management included active range of motion exercises a few days after surgery, and partial weight bearing at six weeks after surgery. Half weight bearing was allowed at three months after surgery, and full weight bearing at six months, after the patients had sufficient abductor strength and had demonstrated a negative or slight Trendelenburg sign.
Assessment
Clinical assessments pre-operatively and at the final follow-up were evaluated according to the scoring system of Merle d’Aubigné and Postel [19], with scoring for pain, mobility of the hip, and walking.
Before surgery, plain antero-posterior (AP) radiographs were obtained to measure acetabular coverage. The center-edge angle of Wiberg (CE angle) [20], the acetabular angle of Sharp [21], and AHI were measured. Furthermore, plain radiographs at the final follow-up were divided into two groups (improved or worsened), according to the presence or absence of progressive OA.
The improved group included hips with joint space of more than 2 mm and joint congruency without any increase of sclerosis or cystic change in the subchondral bone. The worsened group included hips with no improvement or worsening of OA with an increase of sclerosis or cystic change in the subchondral bone [16].
The survival rate analysis was performed using the Kaplan-Meier method, with the reduction of the joint space on radiographs at follow-up or conversion to THA as the end point.
Statistical analysis
The differences between the two means were calculated using the Mann–Whitney U test, the Wilcoxon signed-rank test, or Fisher’s exact probability test. The cumulative probabilities of conversion to THA, or the progression of the radiographic stage were estimated by using the Kaplan-Meier product-limit method. The survival curves for various subgroups were compared by using the log-rank test. Statistical differences were considered significant for p values < 0.05.
Results
Clinical evaluation
The mean preoperative clinical score was similar in the two groups: 10.9 points (range, 8–14) for the single group and 11.0 points (range, 8–14) for the combined group, with p = 0.17 (no statistical difference).
In the single group, the mean clinical score improved significantly from 10.9 to 12.2 points (range, 7–16) at the time of final follow up (p < 0.05). The pain score increased significantly from 2.3 to 3.2 points (p < 0.05), the mobility score remained unchanged from 5.1 to 5.1 points (p = 0.32), and the walking score slightly increased from 3.5 to 3.9 points (p = 0.16). At the final follow-up, four of 25 hips had THA.
In the combined group, the mean clinical score improved significantly from 11.0 points preoperatively to 13.7 points (range, 5–17) at the time of final follow-up (p < 0.01). The pain score significantly increased from 2.3 to 3.8 points (p < 0.01), the mobility score slightly decreased from 5.7 to 5.6 points (p = 0.15), and the walking score significantly increased from 3.3 to 4.3 points (p < 0.01). At final follow-up, only one of 37 hips had THA.
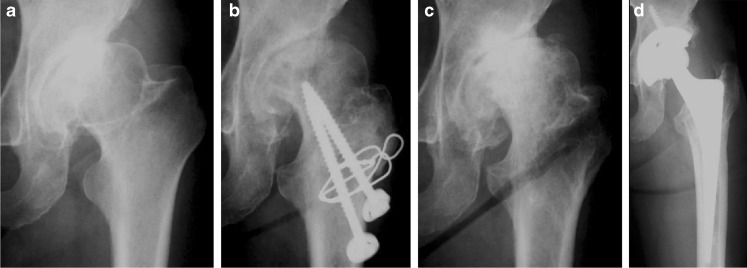
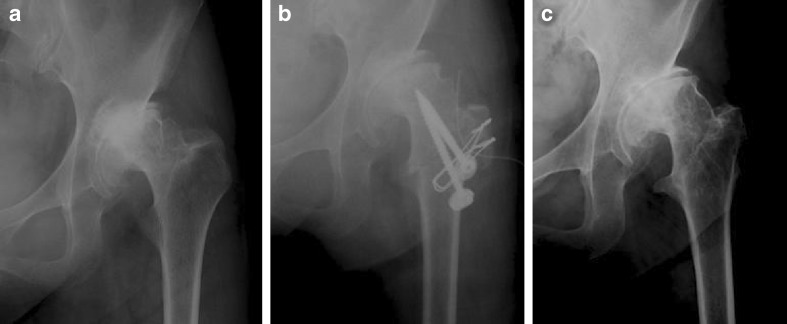
With the end point defined as the time of conversion to THA, the Kaplan-Meier survival rates were 85.5 % at 10 years and 77.7 % at 15 years in the single group, and 100 % at ten years and 92.3 % at 15 years in the combined group; there was a significant difference between the two groups (p < 0.05, log-rank test) (Table 1) (Figs. 1 and 3).
Table 1.
Survival probability for transtrochanteric valgus osteotomy (TVO) from the time of the operation until the end point of conversion to total hip arthroplasty (THA)
| Years after operation | ||||
|---|---|---|---|---|
| Surgical procedure | 5 | 10 | 15 | p Value |
| Single group (N = 25 hips)a | 0.957 (0.873 to 1.000) | 0.855 (0.703 to 1.000) | 0.777 (0.577 to 0.978) | p < 0.05b |
| Combined group (N = 37 hips)a | 1.000 (1.000 to 1.000) | 1.000 (1.000 to 1.000) | 0.923 (0.778 to 1.000) | |
aThe values are given as the probability, with 95 % confidence interval in parentheses
bLog rank test
Statistical differences were considered significant for p values < 0.05
Fig. 1.
A 50-year-old woman had a transtrochanteric valgus osteotomy alone of the left hip. a The preoperative radiograph shows advanced osteoarthritis with 64 % in AHI, b the radiograph obtained after surgery shows improved joint space, but c the radiograph obtained six years after osteotomy shows joint space narrowing, and d THA was carried out seven years after osteotomy. AHI acetabular head index; THA total hip arthroplasty
Fig. 3.
A 47-year-old woman had a transtrochanteric valgus osteotomy combined with a shelf procedure of the left hip. a The pre-operative radiograph shows advanced osteoarthritis with 52 % in AHI, b the radiograph obtained after surgery shows improved joint space with 87 % in AHI, and c the radiograph obtained 12 years after osteotomy shows good congruency and joint space. AHI acetabular head index
No patients in either of the two groups suffered from intra-operative or postoperative complications such as non-union or infection.
Radiographical evaluation
In the evaluations of the latest radiographs, 48 hips (77.4 %) were categorized into the improved group, and 14 hips (22.6 %) into the worsened group. The improved group had 16 out of 25 hips in the single group, and 32 out of 37 hips in the combined group. Meanwhile, the worsened group had nine hips in the single group and five hips in the combined group. The Fisher’s exact probability test showed a significant relationship between the method of surgical treatment and the evaluations from the latest radiographs (p < 0.05) (Figs. 1 and 3).
In the single group, the preoperative mean CE angle, Sharp angle and AHI of the improved group were 11.5°(range, 5–16), 43.6° (range, 41–49) and 79.3 % (range, 67–95) respectively, and those of the worsened group were 7.4° (range, −5 –19), 42.9° (range, 39–48) and 67.6 % (range, 61–81) respectively.
The Mann–Whitney U test showed no statistical difference between the improved and worsened group in the preoperative CE angle (p = 0.34) or Sharp angle (p = 0.68), while it did show a statistical difference in the preoperative AHI (p < 0.05) (Table 2).
Table 2.
Pre-operative radiographical data and latest radiographical evaluation
| Single group | Combined group | |||
|---|---|---|---|---|
| Improved group (N = 16 hips) | Worsened group (N = 9 hips) | Improved group (N = 32 hips) | Worsened group (N = 5 hips) | |
| CE angle* | 11.5° (5–16) | 7.4° (−5–19) | 3.7° (−6–12) | 2.6° (−17–23) |
| Sharp angle* | 43.6° (41–49) | 42.9° (39–48) | 46.3° (38–53) | 47.4° (44–51) |
| AHI* | 79.3 % (67–95) † | 67.6 % (61–81) | 54.6 % (42–59) | 52.5 % (49–59) |
*The values are given as the mean, with the range in parentheses
†p < 0.05 (Mann–Whitney U test) compared with the worsened group in the single group
AHI acetabular head indexAHI acetabular head index, CE angle center-edge angle of Wiberg
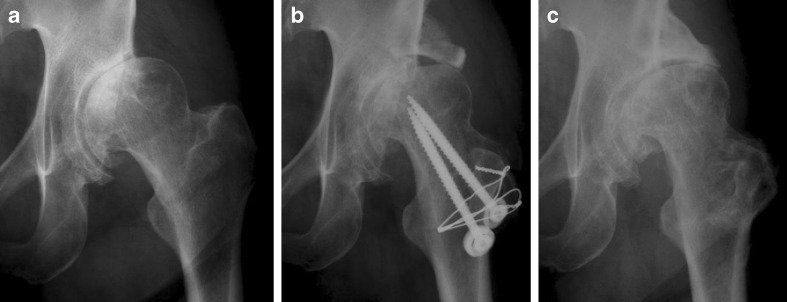
In the single group, 15 of 17 hips with the pre-operative AHI ≥ 70 % were included in the improved group, and seven of eight hips with the pre-operative AHI < 70 % were included in the worsened group. The proportion of hips with the pre-operative AHI ≥ 70 % in the improved group was larger than that in the worsened group. When the Fisher’s exact probability test was used for statistical analysis, the evaluations of patients with the pre-operative AHI≥ 70 % were significantly better than those of patients with the pre-operative AHI < 70 % from the Fisher exact test (p < 0.05) (Figs. 1 and 2).
Fig. 2.
A 52-year-old woman had a transtrochanteric valgus osteotomy of just the left hip. a The preoperative radiograph shows advanced osteoarthritis with 78 % in AHI, b the radiograph obtained after surgery shows improved joint space, and c the radiograph obtained 10 years after osteotomy shows no progressive osteoarthritis. AHI acetabular head index
In the combined group, the pre-operative mean CE angle, Sharp angle and AHI of the improved group were 3.7° (range, −6–12), 46.3° (range, 38–53) and 54.6 % (range, 42–59) respectively, and those of the worsened group were 2.6° (range, −17–23), 47.4° (range, 44–51) and 52.5 % (range, 45–59) respectively. The Mann–Whitney U test showed no statistical difference between the improved and worsened group in the preoperative CE angle (p = 0.88), Sharp angle (p = 0.54) or AHI (p = 0.93) (Table 2).
With the end point defined as the time of OA progression, the Kaplan-Meier survival rates were 69.5 % at ten years and 42.9 % at 15 years after osteotomy in the single group, and 89.3 % at ten years and 83.0 % at 15 years after osteotomy in the combined group; there was a significant difference between the two groups (p < 0.05, log-rank test) (Table 3) (Figs. 1 and 3).
Table 3.
Survival probability for transtrochanteric valgus osteotomy (TVO) from the time of the operation until the end point of progressive osteoarthritis (OA)
| Years after operation | ||||
|---|---|---|---|---|
| Surgical procedure | 5 | 10 | 15 | p Value |
| Single group (N = 25 hips) * | 0.871 (0.734 to 1.000) | 0.695 (0.485 to 0.904) | 0.429 (0.152 to 0.706) | p < 0.05† |
| Combined group (N = 37 hips) * | 0.946 (0.873 to 1.000) | 0.893 (0.772 to 1.000) | 0.830 (0.665 to 0.995) | |
*The values are given as the probability, with 95 % confidence interval in parentheses
†Log rank test
Statistical differences were considered significant for p values < 0.05
Discussion
The previous studies of valgus osteotomy combined with acetabuloplasty have been limited [12, 13]. Toyama et al. [12] reported 67 hips with advanced OA that had been treated by a valgus-extension femoral osteotomy. Thirty-one procedures were combined with the shelf operation. They reported that patients who had the additional shelf procedure experienced a longer-lasting relief from pain compared with osteotomy alone. When the endpoints were defined as conversion to THA, the survival rate at ten years for the whole group, including those with a valgus osteotomy without a shelf procedure, was 79 %, but the survival rate for the group without a shelf procedure was not indicated. On the other hand, Takasaki et al. [13] reported 256 hips treated by a valgus-extension or flexion osteotomy, and 88 procedures were combined with Chiari’s pelvic osteotomy. They reported that the survival rate at ten years for the group with and without Chiari’s pelvic osteotomy was 93 % and 87 %, respectively, when the endpoint was defined as the subsequent operation, and there was no statistically difference in survival rates.
In the present study, when the endpoint was defined as conversion to THA, the survival rate at ten years for the group with and without shelf procedure was 85.5 % and 100 %, respectively, and there was a significant difference (Table 1). Similarly, when the endpoint was defined as progression of OA, the survival rate at ten years was 69.5 % and 89.3 %, respectively, and there was a significant difference (Table 3).
Moreover, in this study, the main factor that influenced the postoperative result was AHI obtained by a pre-operative radiograph: Preoperative AHI less than 70 % in the single group was a risk factor (Figs. 1 and 2). Morita et al. [11] reported 31 hips treated by a valgus-extension femoral osteotomy for advanced OA, and most hips with a postoperative AHI in the range of 60 % to 70 % showed loss or narrowing of the joint space on radiographs within ten years. They recommended that an acetabuloplasty should be added for these patients.
Previous studies have been reported about the survival rates of valgus osteotomy at follow-up intervals of ten and 25 years [10, 12, 13, 15, 16]. According to these reports, the survival rates with a further operation as the end point were 80–90 % at ten years and 60–90 % at 15 years. In the present study, the survival rate of TVO with or without combined shelf procedure was similar to those of previous reports. Moreover, the average age of five patients who underwent THA was 60.4 years (range, 52–71 years). These results indicated that TVO is a more desirable procedure as time-saving surgery for patients of the fifth to sixth decade with advanced OA, and can prevent frequent revision of THA.
A standard THA after TVO can be done easily, because it causes no deformity in the subtrochanteric region of the femur [15]. In fact, we have always inserted a standard stem without corrective osteotomy (Fig. 1). The shelf procedure also has an advantage of bone stock for THA as a further operation: if THA is carried out, bone grafting at the acetabular side will not be required.
In summary, more satisfactory ten year results of TVO were observed in patients who had pre-operative AHI ≥ 70 % or who also underwent the shelf procedure. It is desirable that the shelf procedure be added for patients whose pre-operative AHI is less than 70 %.
References
- 1.Caton J, Prudhon JL. Over 25 years survival after Charnley’s total hip arthroplasty. Int Orthop. 2011;35:185–188. doi: 10.1007/s00264-010-1197-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duffy GP, Berry DJ, Rowland C, Cabanela ME. Primary uncemented total hip arthroplasty in patients less than 40 years old: 10- to 14-year results using first-generation proximally porous coated implants. J Arthroplasty. 2001;16:140–144. doi: 10.1054/arth.2001.28716. [DOI] [PubMed] [Google Scholar]
- 3.Mcaulley JP, Szuszczewicz ES, Yong A, Engh CA., Sr Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004;418:119–125. doi: 10.1097/00003086-200401000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Aronson J. Osteoarthritis of the young adult hip: etiology and treatment. Instr Course Lect. 1986;35:119–128. [PubMed] [Google Scholar]
- 5.Hasegawa Y, Iwase T, Kitamura S, Yamauchi Ki K, Sakano S, Iwata H. Eccentric rotational acetabular osteotomy for acetabular dysplasia: follow-up of one hundred and thirty-two hips for five to ten years. J Bone Joint Surg Am. 2002;84:404–410. [PubMed] [Google Scholar]
- 6.Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg Am. 2006;88:1915–1919. doi: 10.2106/JBJS.E.00715. [DOI] [PubMed] [Google Scholar]
- 7.Sambandam SN, Hull J, Jiranek WA. Factors predicting the failure of Bernese periacetabular osteotomy: a meta-regression analysis. Int Orthop. 2009;33:1483–1488. doi: 10.1007/s00264-008-0643-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pauwels F. The place of osteotomy in the operative management of osteoarthritis of the hip. Triangle. 1968;8:196–210. [PubMed] [Google Scholar]
- 9.Maistrelli GL, Gerundini M, Fusco U, Bombelli R, Bombelli M, Avai A. Valgus-extension osteotomy for osteoarthritis of the hip: Indications and long term results. J Bone Joint Surg Br. 1990;72:653–657. doi: 10.1302/0301-620X.72B4.2380222. [DOI] [PubMed] [Google Scholar]
- 10.Gotoh E, Inao S, Okamoto T, Ando M. Valgus-extension osteotomy for advanced osteoarthritis in dysplastic hips: results at 12 to 18 years. J Bone Joint Surg Br. 1997;79:609–615. doi: 10.1302/0301-620X.79B4.7218. [DOI] [PubMed] [Google Scholar]
- 11.Morita S, Yamamoto H, Hasegawa S, Kawachi S, Shinomiya K. Long-term results of valgus-extension femoral osteotomy for advanced osteoarthritis of the hip. J Bone Joint Surg Br. 2000;82:824–829. doi: 10.1302/0301-620X.82B6.10609. [DOI] [PubMed] [Google Scholar]
- 12.Toyama H, Endo N, Sofue M, Dohmae Y, Takahashi HE. Relief from pain after Bombelli’s valgus extension osteotomy, and effectiveness of the combined shelf operation. J Orthop Sci. 2000;5:114–123. doi: 10.1007/s007760050138. [DOI] [PubMed] [Google Scholar]
- 13.Takasaki S, Uchiyama K, Takahira N, Itoman M. Results and prognostic factors of valgus osteotomy in middle-aged patients with advanced or terminal osteoarthritis of the hip. J Orthop Sci. 2010;15:20–29. doi: 10.1007/s00776-009-1415-y. [DOI] [PubMed] [Google Scholar]
- 14.Sugioka Y. Transtrochanteric valgus osteotomy. Cent Jap J Orthop Surg Traumatol (Japanese) 1984;27:1506–1509. [Google Scholar]
- 15.Jingushi S, Sugioka Y, Noguchi Y, Miura H, Iwamoto Y. Transtrochanteric valgus osteotomy for the treatment of osteoarthritis of the hip secondary to acetabular dysplasia. J Bone Joint Surg Br. 2002;84:535–539. doi: 10.1302/0301-620X.84B4.11869. [DOI] [PubMed] [Google Scholar]
- 16.Kawate K, Tanaka Y, Ohmura T, Hiyoshi N, Yajima H, Tomita Y, Takakura Y. Twenty-five years followup of patients who had valgus osteotomy for arthritic hips. Clin Orthop Relat Res. 2004;426:151–158. doi: 10.1097/01.blo.0000136737.23447.da. [DOI] [PubMed] [Google Scholar]
- 17.Haverkamp D, Marti RK. Intertrochanteric osteotomy combined with acetabular shelfplasty in young patients with severe deformity of the femoral head and secondary osteoarthritis. A long-term follow-up study. J Bone Joint Surg Br. 2005;87:25–31. [PubMed] [Google Scholar]
- 18.Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767–768. [PubMed] [Google Scholar]
- 19.Merle D’Aubigné R, Postel M. Functional result of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed] [Google Scholar]
- 20.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83:58. [Google Scholar]
- 21.Sharp IK. Acetabular dysplasia. The acetabular angle. J Bone Joint Surg Br. 1961;43:268–272. [Google Scholar]