Abstract
Purpose
The purpose of this study was to evaluate reconstruction of the medial patellofemoral ligament (MPFL) using the double-bundle anatomical or single-bundle isometric procedure with respect to the patients’ clinical outcomes.
Methods
In this retrospective study, we evaluated the clinical outcome of double-bundle anatomical versus single-bundle isometric reconstruction of the MPFL for patellar dislocation patients. Sixty-three patients were included in this study from August 2004 to January 2008. From August 2004 to September 2006, MPFL reconstruction using a single-bundle isometric technique was performed in 21 patients (26 knees). Since October 2006, the double-bundle anatomical reconstruction of the MPFL has been used as the routine surgical procedure. It was performed in 37 patients (44 knees). Fifty-eight patients (70 knees) could be followed up. According to the different techniques, we divided the patients into two groups: group D with double-bundle anatomical reconstruction (37 patients) and group S with single-bundle isometric reconstruction (21 patients). Clinical evaluation consisted of the number with a patellar re-dislocation, patellar apprehension sign, Kujala score, subjective questionnaire score, the patella lateral shift rate and patellar tilt angle measured by cross-sectional CT scan.
Results
According to the Kujala score and the subjective questionnaire score, the outcome of the double-bundle group was better than the outcome of the single-bundle group especially in the long-term. Patellar re-dislocation occurred in three patients in the group S, while no re-dislocation occurred in the group D. In total, 26.9 % of group S was considered to have patellar instability, compared to 4.54 % of the group D. After operation, the patellar tilt angle (PTA) and the patella lateral shift rate (PLSR) were restored to the normal range, with statistical significance (P < 0.05) compared to the preoperative state.
Conclusion
Single- and double-bundle reconstruction of the MPFL can both effectively restore patella stability and improve knee function. However, outcomes in the follow-up period showed that the double-bundle surgery procedure was much better than in single-bundle surgery.
Introduction
Patellar dislocation is a very common clinical condition and the previous treatment methods include plication of the medial patellar retinaculum, medial patella retinaculum plasty, lateral retinacular release, medial capsular reefing, anteromedial tibial tubercle transfer, vastus medialis advancement, etc. [1–5]. But the clinical effect is unsatisfactory and the recurrence rate of patella dislocation ranges from 10 % to 35 % with traditional surgical treatment [6]. Recent studies have indicated that patellar dislocation is associated with MPFL laxity, tear or dysfunction [7–10]. In recent years, biomechanical studies have confirmed that the MPFL is the most important soft tissue structure to prevent the patella lateral shift and control the patellar trajectory, providing about 53–60 % limit force [11, 12]. Kang et al. [13] pointed out the functional bundles’ concept, forming the ascending superior-oblique bundle and horizontalis inferior-straight bundle. The superior-oblique bundle together with the vastus medialis obliquus maintained the dynamic stability of the patellar, while the inferior-straight bundle provided the static strength of inhibition. This new concept had an important guidance for MPFL treatment which should not only focus on the anatomical reconstruction, but also on the biomechanical function of ligaments. Therefore, MPFL reconstruction to treat patellar dislocation becomes the focus of clinical research. Regaining the balance of patellar soft tissue and the movement trajectory are the prerequisites to obtain a satisfying long-term clinical outcome. Based on experiments and anatomical studies, researchers have proposed both isometric and anatomical reconstructions of the MPFL [14, 15]. We postulated that the double-bundle anatomical reconstruction of the MPFL was better for patellar stability and knee function than the single-bundle isometric reconstruction of the MPFL.
Methods
Retrospective analysis from August 2004 to January 2008 showed that 58 patients (70 knee) who suffered from patellar dislocation had undergone MPFL reconstruction, including 23 males and 35 females with an average age of 25 ± 8 years (ranging from 18 to 35 years). From August 2004 to September 2006, MPFL reconstruction was performed in seven male patients (nine knees) and 14 females (17 knees); 21 patients (26 knees) in total received single-bundle isometric reconstruction. In our early follow-up period, we found that the clinical results of the single-bundle isometric reconstruction of the MPFL for patellar dislocation were not satisfactory. Steensen et al. [9] found that the patellar side of the patellofemoral ligament attachment point was flexible, as a fan-shaped attachment over an extremely wide range from the superior patellar pole to the midpoint of the patella. We therefore began to use the double-bundle anatomical reconstruction of the MPFL to simulate its fan shape for patients with patellar dislocation. Since October 2006, the double-bundle anatomical reconstruction of the MPFL was used as the routine surgical procedure. Double-bundle anatomical reconstruction of the MPFL was performed in 37 patients (44 knees), including 16 male patients (18 knees) and 21 females (26 knees). General characteristics of these two groups are shown in Table 1 and there was no significant difference (P > 0.05). Recurrent patellar dislocation was defined as at least two or more incidences of patellar dislocation, or patellar instability symptoms which lasted for more than three months after the first dislocation [16].
Table 1.
Characteristics of patients in the single-bundle isometric group (group S) and double-bundle anatomical group (group D)
| Characteristic | Group S (n = 26) | Group D (n = 44) | P value |
|---|---|---|---|
| Case (knee) | 21 (26) | 37 (44) | |
| Gender (male/female) | 7/14 | 16/21 | 0.458 |
| Mean age (years) | 23 ± 10 | 26 ± 7 | 0.941 |
| Range | 18–33 | 19–35 | |
| Injury to operation time (months) | 28 ± 14 | 24 ± 12 | 0.225 |
| Range | 1–88 | 0.5–70 | |
| Injury reason, n (%) | 0.958 | ||
| Traffic accident injury | 5 (23.8) | 9 (24.3) | |
| Sprain | 7 (33.3) | 11 (29.7) | |
| Unknown | 9 (42.9) | 17 (46) | |
| Meniscus injury knee, n (%) | 0.897 | ||
| Medial | 9 (34.6) | 17 (38.6) | |
| Lateral | 6 (23.1) | 9 (20.5) | |
| Bilateral | 3 (11.5) | 4 (9.1) | |
| Cartilage injury (%) | 18 (69.2) | 35 (79.5) | 0.530 |
Inclusion criteria
The following four items were considered inclusion criteria for the study: (1) patellar dislocation occurred at least two times, or the patient had a history of patellar dislocation and patellar instability symptoms (pain, subluxation, or both) existed for more than three months after the first dislocation, (2) patellar apprehension sign was positive, (3) CT showed patella excessive external divergence indicating MPFL laxity, and (4) conservative treatment was unsuccessful.
Exclusion criteria
Exclusion criteria included: (1) a history of knee surgery, (2) patellar height: Insall index > 1.2, Q angle > 20°, (3) CT measurement of the knee-joint: femoral trochlear groove angle > 150°, TT-TG > 15 mm, (4) cruciate ligament damage complicated by lateral collateral ligament injury, (5) associated with rheumatoid arthritis, bone necrosis etc., and the level of articular cartilage defects above Outerbridge III.
Preoperative evaluation
Stability
The first step was to check the stability of the patella. If the patella mobility was over 1.5 cm by the lateral stress in 30° flexion, patella hypermobility was diagnosed. If patellar mobility is more than 1.5 cm, associated with a soft ending point or no stop point, this could be diagnosed as patellar dislocation [17]. If the patella mobility was less than 1/4 patella width under the medial force, this could be called lateral overstrain [18]. Patellar hypermobility and dislocation are defined as patellar instability. This standard had also been used to determine the tension of reconstruction of the MPFL during the operation, to determine whether to release the lateral patellar retinaculum, and to determine the stability of the patella during postoperative follow-up.
Imaging
Imaging examination was made using the standard lateral radiograph of the knee to evaluate the patella height. This was made using cross-sectional CT scan in 20° knee flexion to measure the patellar tilt angle [19] and patellar lateral shift rate [20, 21].
Surgical technique
Operations in all patients were performed by the same senior surgeon, using MPFL reconstruction combined with vastus medialis advancement. In group S, all the operations used autologous semitendinosus tendon to reconstruct the MPFL. In group D, all the operations used autologous semitendinosus tendon or autogenous semitendinosus tendon combined with the gracilis tendon. Anteromedial (AM), anterolateral (AL) and superolateral (SL) portals were routinely adopted. Arthroscopy exploration was used to assess patella articular contact, to deal with intra-articular lesions. If the patella mobility was less than 1/4 patella width under the medial force, this could be called lateral overstrain [18]. If the lateral structures were excessively tight (less than one quadrant medial shift), a lateral release was routinely performed.
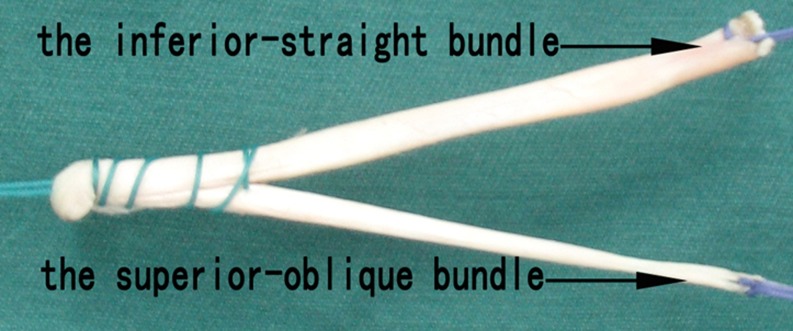
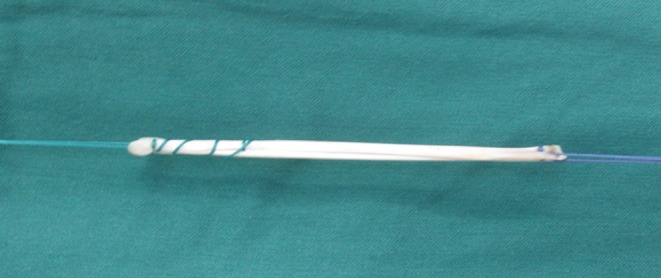
Single-bundle isometric reconstruction
A tendon stripper was used to harvest the semitendinosus tendon length of about 20 cm (if the semitendinosus tendon was too thin, we also took the gracilis tendon). The folded end of the graft was braided 2.5 cm with Ethibond No.2 non-absorbable suture. It was then fixed on the other end of the graft (Figs. 1 and 2) using the Ethicon No.2 non-absorbable suture as a traction line.
Fig. 1.
The graft preparation of single-bundle
Fig. 2.
The graft preparation of double-bundle
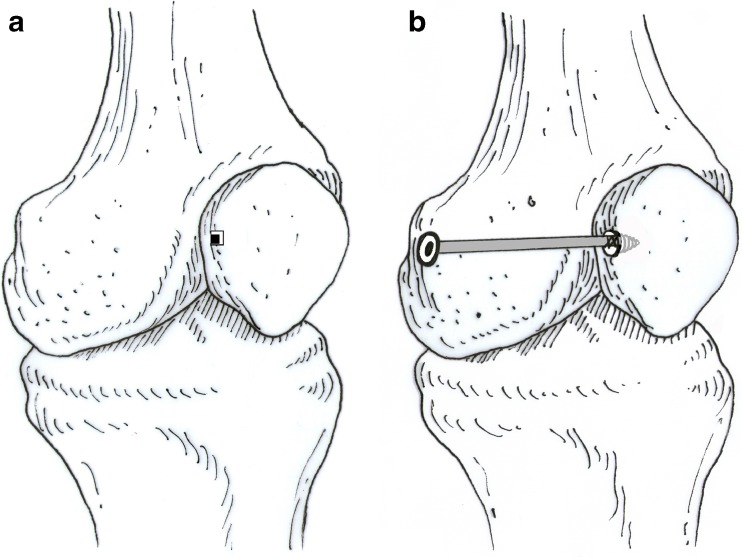
The midpoint between adductor tubercle and the highest point of the medial femoral condyle was selected as the initial insertion point on the femur, and the supermedial patellar medial edge was selected as the insertion point on the patella. The patella was maintained in the centre of the femoral trochlea and the location of the femoral insertion was selected in order to obtain the fixed distance between the insertion point of femur and patella in the process of knee extension and flexion. A 2.4-mm guide pin with an eyelet was then inserted into the femoral insertion site of the MPFL. The guide pin placement was monitored by a fluoroscopy machine in a straight lateral view to obtain the correct anatomical femoral insertion. Subsequently, a longitudinal skin incision of 1 cm was made over the femoral insertion site of the MPFL, and subcutaneous tissue was dissected to expose cortical bone. A femoral tunnel three centimetres deep was drilled using a seven millimetre diameter reamer. The sutured, folded end of the graft was inserted into the femoral tunnel and secured with a 7 × 23-mm absorbable screw.
An three centimetre incision was made over the patellar medial edge. A bony groove was made in the patellar medial edge half a centimetre long by half a centimetre wide and half a centimetre deep. A suture anchor with No.3 non-absorbable braided suture was placed into the bony groove. The graft tension was adjusted before the grafts were sutured to the anchors in the patella. The other end of the graft was fixed to the anchors by the No.3 non-absorbable braided suture at the patella. The tension was evaluated again during knee flexion from 0° to 90° so as to maintain the proper tracking of the patella. The knee flexion was 30° during the process of final fixation. A schematic diagram shows the process of single-bundle isometric reconstruction of the MPFL (Fig. 3). Finally, the vastus medialis oblique was imbricated by suturing it to the supermedial patellar edge.
Fig. 3.
The schematic diagram of the single-bundle isometric reconstruction of the MPFL. a A bony groove was made in the patellar medial edge 0.5 cm long, 0.5 cm wide and 0.5 cm deep. b The two ends of the graft were fixed by a 7 × 23-mm absorbable screw and an anchor
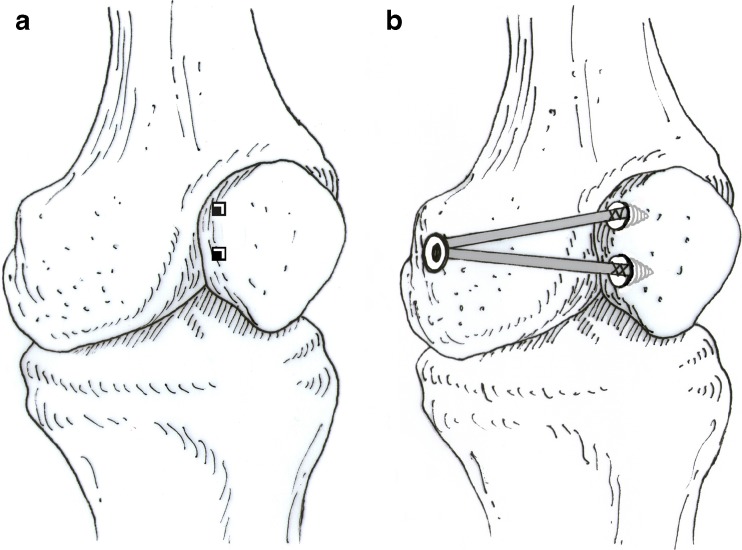
Double-bundle anatomical reconstruction
In group S, two bony grooves were made in the group D in the patellar medial edge, which were in the centre and the upper inner corner of the patellar medial edge. Two suture anchors carrying No. 3 non-absorbable braided suture were inserted into the two bony grooves. The graft tension was adjusted before the grafts were sutured to the anchors in the patella. The fixation method of the femoral side was the same as the single-bundle isometric reconstruction. The inferior-straight bundle was fixed to the suture anchor that was in the centre of the patellar medial edge. The superior-oblique bundle was fixed to another suture anchor. The tension was evaluated again during knee flexion from 0° to 90° so as to maintain theproper tracking of the patella. The knee flexion degree was 30° during the process of final fixation. The schematic diagram of the double-bundle anatomical reconstruction of the MPFL is shown in Fig. 4. Finally, the vastus medialis obliquus was imbricated by suturing it to the superior-obliquus bundle of the MPFL.
Fig. 4.
The schematic diagram of the double-bundle anatomical reconstruction of the MPFL. a Two bony grooves were made in the group S in the patellar medial edge, which were in the centre and the upper inner corner of the patellar medial edge. b The three ends of the graft were fixed by a 7 × 23-mm absorbable screw and two anchors
Postoperative rehabilitation program
The rehabilitation program was the same for single and double bundle cases. After the MPFL reconstruction patients wore a brace for one week. The patients began moderate exercise such as isometric contraction of quadriceps femoris muscle, straight leg raising, patella traction and mild genuflection two days after the operation. Flexion of 10° was allowed from the third day after the operation and the angle was increased gradually to 90° in a month. Two weeks after operation, the patients could start CPM exercises, and active or assisted knee-joint ROM exercises; three weeks after operation, the affected limb could withstand partial weight-bearing and full weight-bearing five weeks after operation or later. The patient could jog three months after operation and participate in normal sports activities six months after operation.
Evaluation methods
Postoperative follow-up recorded complications and prognosis of MPFL reconstruction, a manual check on patella stability, and any patella re-dislocation. The CT scan was used to examine patellar tilt angle (PTA) and patellar lateral shift rate (PLSR) in 20° flexion. The knee-joint function was assessed by the Kujala score [22] and subjective questionnaire score [23]. In the subjective questionnaire score, a score of 95–100 is graded excellent, 90–94 is excellent, 80–89 is good, 70–79 is fair, and less than 70 is poor.
Statistical analysis
The SPSS 13.0 software was used for data processing. Preoperative and postoperative indices for each group were compared by paired t test. Independent-samples t test and Mann-Whitney U test were used for group comparison. Chi-square was used on ratio comparison. P < 0.05 was defined as a significant difference.
Results
In group S, all patients were treated with autologous semitendinosus tendon for patellofemoral ligament reconstruction surgery. In group D, 14 patients (19 knees) were treated with autogenous semitendinosus tendon and gracilis tendon for patellofemoral ligament reconstruction surgery. Twenty-five cases (32 knees) underwent patellar lateral retinacular release surgery. Thirteen patients (15 knees) received single-bundle isometric reconstruction (group S), while 12 patients (17 knees) underwent double-bundle anatomical reconstruction (group D). During postoperative follow-up, superficial wound infection occurred in one patient of each group. The wound healed over time and had no effect on recovery of joint function. Patellar re-dislocation occurred in three patients of group S but none in group D. There was no deep vein thrombosis or joint flexion-extension limitation in either group. Five patients (three patients of group S, two patients of group D) were lost due to the loss of their contact number. The follow-up data is shown in Tables 2 and 3.
Table 2.
The follow-up data of single-bundle (group S) and double-bundle (group D) reconstruction of the MPFL (mean ± standard deviation)
| Follow-up index | Knee | A | B | C | P(B:A) | P(C:A) | P(C:B) |
|---|---|---|---|---|---|---|---|
| PTA (°) | |||||||
| Group S | 26 | 12.06 ± 2.76 | 8.34 ± 1.78 | 9.22 ± 1.62 | 0.000 | 0.000 | 0.000 |
| Group D | 44 | 12.79 ± 3.65 | 7.62 ± 1.71 | 7.76 ± 1.38 | 0.000 | 0.000 | 0.301 |
| PLSR (%) | |||||||
| Group S | 26 | 18.79 ± 4.93 | 10.65 ± 2.63 | 11.30 ± 2.12 | 0.000 | 0.000 | 0.007 |
| Group D | 44 | 19.75 ± 4.45 | 10.04 ± 1.52 | 10.24 ± 1.48 | 0.000 | 0.000 | 0.135 |
| Kujala Score | |||||||
| Group S | 26 | 57.35 ± 7.14 | 87.77 ± 3.99 | 80.46 ± 3.59 | 0.000 | 0.000 | 0.000 |
| Group D | 44 | 61.00 ± 5.17 | 92.34 ± 4.32 | 92.86 ± 2.47 | 0.000 | 0.000 | 0.404 |
Group S single-bundle isometric group, Group D double-bundle anatomical group, A preoperative, B postoperative 12 month, C postoperative 48 month, T T-value, P P-value, PTA patellar tilt angle, PLSR patella lateral shift rate
Table 3.
Group comparison data between single-bundle (group S) and double-bundle (group D) at 12 and 48 months
| Group comparison | B | C | ||
|---|---|---|---|---|
| T | P | T | P | |
| Kujala score | −4.399 | 0.000 | −15.561 | 0.000 |
| PTA | 1.679 | 0.098 | −3.994 | 0.000 |
| PLSR | −0.760 | 0.447 | 2.242 | 0.031 |
B postoperative 12 month, C postoperative 48 month, T T-value, P P-value, PTA patellar tilt angle, PLSR patella lateral shift rate
Patellar stability
The patellar instability rates at 12 months and 54 months were 19.2 % and 26.9 % in group S and 2.27 % and 4.54 % in group D, respectively. There was a significant difference between 12 months and 48 months in group S. However, no significant difference was found between 12 months and 48 months in group D. There was no significant difference between group D and group S at 12 months after operation. However, the statistical difference was significant in group comparison at 48 months.
CT evaluation
CT scan evaluation was made of the patellofemoral joint in 20° of flexion. A significant difference could be found between 12 and 48 months in group S, while there was no statistical difference in group D. The difference between group D and group S was not statistically significant at 12 months, but the difference was obvious at 48 months.
Kujala score
There was a significant difference of Kujala score between 12 and 48-months in group S, while there was no statistical difference of Kujala score in group D. The differences between the group D and group S were statistically significant at both 12 and 48 months after operation.
Subjective questionnaire score
For group S, 18 cases were graded excellent, five were good, three fair and the excellent and good rate was 88.5 % at 12 months postoperation. At 48 months, 17 cases were graded excellent, four good, two fair, three poor and the excellent and good rate was 80.8 %. For group D, 37 cases were graded excellent, six good, one fair and the excellent and good rate was 97.7 % at the 12th month; 37 cases were graded excellent, five good, two fair and the excellent and good rate was 95.5 % at 48 months.
Discussion
Sallay et al. [10] reported that 94 % of patients with patellar dislocation were accompanied by MPFL tear. Amis et al. [24] pointed out that the MPFL played a predominant role in maintaining the patella stability. Therefore, MPFL repair or reconstruction has been universally believed to be the primary surgical treatment for patellar dislocation. In recent years, based on experimental and anatomical study, scholars [14, 15] believed that the non-isometric and non-anatomical patellofemoral ligament reconstruction operations, which led to abnormal patella dynamic changes, were the key factors that affected the short- and long-term clinical outcomes. Satterfield and Johnson [25] adopted single-bundle isometric MPFL reconstruction for patients with patellar dislocation and the follow-up results showed the Kujala score increased from 55.0 to 85.7, but three patients still suffered patellar re-dislocation and three knees had a positive patella apprehension sign. Similar reports were published from other researchers who adopted single-bundle isometric reconstruction [26–28]. Toritsuka et al. [29] treated 20 patients with double-bundle anatomical MPFL reconstruction, and no patella re-dislocation occurred in the following 30 months, while the Kujala score rose to 96 ± 5 and patient satisfaction rate was 100 % by the Crosby and Insall rating system. Some scholars [30–32] reported similar results to Toritsuka et al. It could be clearly shown in our research that the incidence of patella instability remarkably increased over time prolongation after single-bundle isometric reconstruction. Kujala score and subjective questionnaire scores significantly decreased, while there was no significant change for the double-bundle anatomical reconstruction group. The long-term clinical results of double-bundle anatomical reconstruction was highly superior to single-bundle isometric reconstruction.
Based on anatomical research, Smirk and Morris [33] confirmed that the femoral patellofemoral ligament attachment point was located between the near posterior side of the medial femoral condyle and the distal end of the adductor tubercle. Aragāo et al. [34] and Steensen et al. [9] found that the patellar side of the patellofemoral ligament attachment point was flexible, as a fan-shaped attachment over an extremely wide range from the superior patellar pole to the midpoint of the patella. Single-bundle reconstruction of the MPFL lost the normal patello-femoral ligament anatomy shape, while the double-bundle anatomical reconstruction was the maximum morphological imitation of the fan-shaped structure of the original patellofemoral ligament. Therefore, it was generally acknowledged that double-bundle anatomical reconstruction was consistent with the anatomical characteristics of the patellofemoral ligament. Clinical follow-up results showed that the postoperative Kujala score was significantly higher than the preoperative. The group comparison illustrated that group D was much more successful than group S in both short- and long-term clinical results. There was no occurrence of patellar re-dislocation in either group at the 12-month follow-up, and the incidence of patella instability was 19.2 % and 2.27 % for groups S and D, respectively. The significant statistical difference in patella instability between groups D and S obviously indicates that double-bundle anatomical reconstruction was superior to single-bundle isometric reconstruction. Double-bundle anatomical reconstruction provides stable function, improved grades of joint function, and more satisfying clinical results.
Panagiotopoulos et al. [35] demonstrated that the MPFL and the vastus medialis obliquus together form a dynamic and static knee stability system. The patella could reach the femoral trochlear groove by contraction of the vastus medialis obliquus during the early stage of knee-joint flexion. This strengthened the MPFL protection on patella stability during movement rather than static condition. Kang et al. [13], studying MPFL anatomy, pointed out a double functional bundles concept that MPFL fibres grow into two major different shapes: an ascending superior-oblique bundle and a horizontalis inferior-straight bundle. The ascending bundle combined with the vastus medialis obliquus was to maintain the dynamic stability of the patellar structure, while the horizontal bundle formed the static strength. If double-bundle anatomical reconstruction was applied, the inferior-straight bundle reconstruction helps to restore the stabilising effect of the lower fibre in the patellofemoral ligament and the superior-oblique bundle combined with vastus medialis oblique transfer reconstruction strengthens both the static and dynamic knee-joint stabilisation device. Therefore, from a biomechanical viewpoint, double-bundle anatomical reconstruction should restore the MPFL biomechanical function to the maximum extent. The single-bundle isometric reconstruction would probably lead to ligament laxity or failure with the passage of time and this, in turn, could cause abnormal stress on the patellofemoral joint, resulting in patellar arthritis. However, double-bundle anatomical reconstruction should restore both anatomical structure and biomechanical characteristics of the MPFL, which should prevent lateral patellar tilt or re-dislocation. Subjective questionnaire score at the 48th month showed the excellent and good rate of group S to be 80.8 % and group D was 95.5 %. Kujala score at 48 months indicated that group S was 80.46 ± 3.59 and group D was 92.86 ± 2.47. Again, we found that double-bundle anatomical reconstruction significantly surpassed single-bundle isometric reconstruction in maintenance of knee-joint stability and long-term quality of life.
From the clinical follow-up results at 12 months, we found that the patellar tilt angle (PTA) and patellar lateral shift rate (PLSR) remained normal from both groups and there was no statistical difference between two groups. However, at the 48th month, single, there was a significant difference between two groups, and group D was markedly superior to group S. The incidence of patellar instability in the 48th month followed the same trend: 26.9 % and 4.54 % for groups S and D respectively. Mountney et al. [36] found that there were some differences in the length, width and thickness of the MPFL and it could reach 208 N in in vitro tensile strength test. Panagiotopoulos et al. [35] considered that the MPFL force in vivo should be far larger than that in vitro. Hamner et al. [37] found single-bundle semitendinosus tendon strength was 1,060 ± 227 N and single-bundle gracilis tendon strength was 837 ± 138 N. Moreover, the double-bundle semitendinosus and gracilis tendon strengths were 2,640 ± 320 N and 1,550 ± 369 N, respectively. Animal experiments show that the strength of a graft declines with time and the strength could only achieve 10–50 % of the normal ligament after three years [38]. Reconstructed tendon will undergo three processes: necrosis, vascularisation and remodelling. During these processes, the ligament strength decreased. Therefore, the single-bundle isometric MPFL reconstruction may not provide sufficient traction in the early rehabilitation, resulting in ligament dysfunction. However, double-bundle anatomical reconstruction can provide double the traction force compared to the single-bundle isometric reconstruction. Consequently, the ligament was not easily stretched in the early rehabilitation period. Thus, group D surpassed group S in the incidence of patellar instability, Kajala score and subjective questionnaire score.
An important indication of patellar instability lies in the abnormal patellar trajectory. Based on the theory that MPFL length changes only 1.1 mm during knee flection from 0° to 90°, Steensen et al. [39] undertook single-bundle isometric MPFL reconstruction and the follow-up results turned out to be satisfactory; whereas Parker’s [15] research showed single-bundle isometric reconstruction could not restore normal patellar trajectory in any angle of knee-joint flexion. Single-bundle reconstruction could not reconstruct the normal patellofemoral ligament anatomical shape. Although double-bundle anatomical reconstruction does not fully restore the normal patellar trajectory, it can ensure the normal patellar trajectory in the centre of the femoral trochlear groove. The patellar trajectory had quite essential clinical significance. Abnormal patellar trajectory leads to abnormal stress distribution which causes articular cartilage injury and patella pain [40]. If the normal patellar trajectory is not restored, the incidence of patellar arthritis will be remarkably increased. Kujala score at the 48th month indicates that group S was 80.46 ± 3.59 and group D was 92.86 ± 2.47. Subjective questionnaire score at 48 months showed the excellent and good rate of group S was 80.8 % and group D was 95.5 %. The double bundle anatomical MPFL reconstruction surgery procedure had a higher knee assessment score and better clinical results.
Limitations
This research is a retrospective study rather than a prospective randomised controlled trial. Hence, selection bias cannot be avoided. More accurate evaluation could be obtained between single-bundle isometric and double-bundle anatomical reconstruction for the patellar dislocation patients under a further prospective randomised controlled trial.
Conclusion
Single, double-bundle reconstruction of the MPFL could both effectively restore patella stability and improve knee function. However, the clinical outcomes showed that the double-bundle surgery procedure was far better than the single-bundle technique.
Footnotes
Level of evidence: Therapeutic studies, level III.
Contributor Information
Cheng-hai Wang, Email: 9112qwa@163.com.
Fei Wang, Email: doctorwf@yeah.net.
References
- 1.Haspl M, Cicak N, Klobucar H, Pecina M. Fully arthroscopic stabilization of the patella. Arthroscopy. 2002;18(1):E2. doi: 10.1053/jars.2002.29868. [DOI] [PubMed] [Google Scholar]
- 2.Rhee SJ, Pavlou G, Oakley J, et al. Modern management of patellar instability. Int Orthop. 2012;36(12):2447–2456. doi: 10.1007/s00264-012-1669-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ji G, Wang F, Zhang Y, et al. Medial patella retinaculum plasty for treatment of habitual patellar dislocation in adolescents. Int Orthop. 2012;36(9):1819–1825. doi: 10.1007/s00264-012-1544-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freitag S, Lill H, Hepp P, et al. Locked lateral patella dislocation with generalized ligamentous laxity after arthroscopic lateral release of the knee. Arthroscopy. 2005;21(5):628.e1–628.e4. doi: 10.1016/j.arthro.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 5.Sillanpää P, Mattila VM, Visuri T, et al. Ligament reconstruction versus distal realignment for patellar dislocation. Clin Orthop Relat Res. 2008;466(6):1475–1484. doi: 10.1007/s11999-008-0207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davis DK, Fithian DC. Techniques of medial retinacular repair and reconstruction. Clin Orthop Relat Res. 2002;402:38–52. doi: 10.1097/00003086-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Ahmad CS, Stein BE, Matuz D, et al. Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation: a review of eight cases. Am J Sports Med. 2000;28:804–810. doi: 10.1177/03635465000280060701. [DOI] [PubMed] [Google Scholar]
- 8.Andrikoula S, Tokis A, Vasiliadis HS, et al. The extensor mechanism of the knee joint: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):214–220. doi: 10.1007/s00167-005-0680-3. [DOI] [PubMed] [Google Scholar]
- 9.Steensen RN, Dopirak RM, McDonald WG. The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction: implications for reconstruction. Am J Sports Med. 2004;32:1509–1513. doi: 10.1177/0363546503261505. [DOI] [PubMed] [Google Scholar]
- 10.Sallay PI, Poggi J, Speer KP, et al. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24(1):52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 11.Conlan T, Garth WP, Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 13.Kang HJ, Wang F, Chen BC, et al. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1511–1516. doi: 10.1007/s00167-010-1090-8. [DOI] [PubMed] [Google Scholar]
- 14.Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34(8):1254–1261. doi: 10.1177/0363546505285584. [DOI] [PubMed] [Google Scholar]
- 15.Parker DA, Alexander JW, Conditt MA, et al. Comparison of isometric and anatomic reconstruction of the medial patellofemoral ligament: a cadaveric study. Orthopedics. 2008;31(4):339–343. doi: 10.3928/01477447-20080401-28. [DOI] [PubMed] [Google Scholar]
- 16.Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23(5):260–263. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deie M, Ochi M, Sumen Y, et al. A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):522–528. doi: 10.1007/s00167-005-0641-x. [DOI] [PubMed] [Google Scholar]
- 18.Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7(2):121–127. doi: 10.1016/S0968-0160(00)00038-7. [DOI] [PubMed] [Google Scholar]
- 19.Schutzer SF, Ramsby GR, Fulkerson JP. The evaluation of patellofemoral pain using computerized tomography. A preliminary study. Clin Orthop. 1986;204:286–293. [PubMed] [Google Scholar]
- 20.Sasaki T, Yagi T. Subluxation of the patella. Investigation by computerized tomography. Int Orthop. 1986;10:115–120. doi: 10.1007/BF00267752. [DOI] [PubMed] [Google Scholar]
- 21.Delgado-Martínez AD, Estrada C, Rodríguez-Merchán EC, et al. CT scanning of the patello-femoral joint. The quadriceps relaxed or contracted? Int Orthop. 1996;20:159–162. doi: 10.1007/s002640050054. [DOI] [PubMed] [Google Scholar]
- 22.Kujala UM, Jaakkola LH, Koskinen SK, et al. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi: 10.1016/S0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 23.Drez D, Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17(3):298–306. doi: 10.1053/jars.2001.21490. [DOI] [PubMed] [Google Scholar]
- 24.Amis AA, Firer P, Mountney J, et al. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215–220. doi: 10.1016/S0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 25.Satterfield WH, Johnson DL. Arthroscopic patellar “bankart” repair after acute dislocation. Arthroscopy. 2005;21(5):627.e1–627.e5. doi: 10.1016/j.arthro.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 26.Marteau E, Burdin P, Brilhault JM. Gracilis tendon transfer associated with distal alignment for patella alta with recurrent dislocations: an original surgical technique. Orthop Traumatol Surg Res. 2011;97(4):S5–S11. doi: 10.1016/j.otsr.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 27.Mikashima Y, Kimura M, Kobayashi Y, et al. Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. Acta Orthop Belg. 2006;72(1):65–71. [PubMed] [Google Scholar]
- 28.Schöttle PB, Fucentese SF, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):516–521. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 29.Toritsuka Y, Amano H, Uchida R, et al. Dual tunnel medial patellofemoral ligament reconstruction for patients with patellar dislocation using a semitendinosus tendon autograft. Knee. 2011;18(4):214–219. doi: 10.1016/j.knee.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 30.Matthews JJ, Schranz P. Reconstruction of the medial patellofemoral ligament using a longitudinal patellar tunnel technique. Int Orthop. 2010;34(8):1321–1325. doi: 10.1007/s00264-009-0918-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Christiansen SE, Jacobsen BW, Lund B, et al. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24(1):82–87. doi: 10.1016/j.arthro.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Ahmad CS, Brown GD, Stein BS. The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med. 2009;37(10):2021–2027. doi: 10.1177/0363546509336261. [DOI] [PubMed] [Google Scholar]
- 33.Smirk C, Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10(3):221–227. doi: 10.1016/S0968-0160(03)00038-3. [DOI] [PubMed] [Google Scholar]
- 34.Aragão JA, Reis FP, de Vasconcelos DP, et al. Metric measurements and attachments levels of the medial patellofemoral ligament: an anatomical study in cadavers. Clinics. 2008;63(4):541–544. doi: 10.1590/S1807-59322008000400021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Panagiotopoulos E, Strzelczyk P, Herrmann M, et al. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Tarumatol Arthrosc. 2006;14(1):7–12. doi: 10.1007/s00167-005-0631-z. [DOI] [PubMed] [Google Scholar]
- 36.Mountney J, Senavongse W, Amis AA, et al. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87(1):36–40. [PubMed] [Google Scholar]
- 37.Hamner DL, Brown CH, Jr, Steiner ME, et al. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999;81(4):549–557. doi: 10.2106/00004623-199904000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Clancy WG, Jr, Nelson DA, Reider B, et al. Anterior cruciate ligament reconstruction using one-third of the patellar ligament augmented by extra-articular tendon transfers. J Bone Joint Surg Am. 1982;64(3):352–359. [PubMed] [Google Scholar]
- 39.Steensen RN, Dopirak RM, Maurus PB. A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy. 2005;21(3):365–370. doi: 10.1016/j.arthro.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 40.Heegaard J, Leyvraz PF, Van Kampen A, et al. Influence of soft structures on patellar three- dimensional tracking. Clin Orthop Relat Res. 1994;299:235–243. [PubMed] [Google Scholar]