Abstract
Purpose
Percutaneous reduction and periarticular screw implantation techniques have been successfully introduced in acetabular surgery. The advantages of this less invasive approach are attenuated by higher risks of screw misplacement. Anatomical landmarks are strongly needed to prevent malplacement. This cadaver study was designed to identify reliable anatomical osseous landmarks in the pelvic region for screw placement in acetabular surgery. Gender differences were specifically addressed.
Methods
Twenty-seven embalmed cadaveric hemipelvic specimens (13 male, 14 female) were used. After soft-tissue removal, anterior and posterior column acetabular screw placement was conducted by one orthopaedic trauma surgeon under direct vision. Each column was addressed by antegrade and retrograde screw insertion. Radiographic verification of ideal screw placement was followed by assessment of the distance from the different entry points to adjoining anatomical osseous structures.
Results
For anterior column screw positioning, the posterior superior iliac spine (PSIS), posterior inferior iliac spine (PIIS), iliopectineal eminence and centre of the symphysis were most reliable regarding gender differences. For posterior column screw positioning, the distance to the anterior superior iliac spine (ASIS) and the ischial tuberosity showed the lowest deviation between the different gender specimens. Highest gender differences were seen in relation to the cranial rim of the superior pubic ramus in retrograde anterior column screw positioning (p = 0.002). Most landmarks could be targeted within a 2.5-cm range in all specimens.
Conclusions
The findings emphasise the relevance of osseous landmarks in acetabular surgery. By adhering to easily identifiable structures, screw placement can be safely performed. Significant gender differences must be taken into consideration during preoperative planning.
Introduction
Most acetabular fractures result from high-energy trauma, or low-energy trauma in elderly people with osteoporotic bones. An open approach is usually needed for joint reconstruction and osteosynthesis. Depending on the involved bone structures, the iliofemoral approach for anterior column or the Kocher–Langenbeck approach for posterior column fractures are frequently used. Excellent exposure of the relevant anatomical structures is necessarily offset by extensive tissue damage. In special circumstances, such as the multimorbid elderly patient, or in minimally displaced fractures, percutaneous reduction and periarticular screw implantation has been successfully achieved [1, 2]. Accurate preoperative planning and solid intraoperative navigation or intraoperative computed tomography (CT) are essential to insert the implants in a safe osseous corridor [3]. It is mandatory that the surgeon has a general familiarity with the osseous anatomy of the pelvis. Navigation systems might be of benefit in this regard [4]. However, navigation systems in the pelvic region are costly and demand extensive experience in order to avoid disasters during surgery. Besides this cost, radiation exposure to the patient and the surgical team is highly relevant. Anatomical osseous landmarks can be easily assessed with intraoperative fluoroscopy.
The purpose of this study was to identify reliable anatomical osseous landmarks and determine gender-related variation of different entrance points for periarticular screw placement.
Methods
Twenty-seven embalmed cadaveric hemipelvic specimens (13 male, 14 female of indeterminate age) were obtained for the study in accordance with the rules and regulations of the University of Medicine, Regensburg. A standard embalming process with internal application of formaldehyde, phenol, glycerine and alcohol, followed by a nine month external application of glycerin and phenol, was conducted. Prior to the main experiments, specimens were dissected to remove overlying soft tissue, and the hip joints were disarticulated. The remaining bony and ligamentous structures were checked for integrity before each experiment. After soft-tissue dissection, all specimens showed intact bony and ligamentous structures. No signs of former fracture healing or obvious pathologies to the bone were seen.
Using a 2.5-mm drill bit, a hole was made and one cannulated 6.5-mm lag screw was placed under direct vision by one experienced orthopaedic trauma surgeon. Screw placement was possible in all pelvises. No iatrogenic fracture was induced. One screw each was placed for posterior and anterior columns (Fig. 1). Optimal screw placement was achieved using direct visualisation and then immediately afterwards validated using C-arm image-intensified fluoroscopic imaging. Each specimen was therefore positioned on a radiolucent table, and anteroposterior (AP), iliac oblique and obturator oblique views were obtained. No violation of articular joint surface was tolerated. The cortex was penetrated at the antegrade and retrograde entry points only. In the literature, antegrade and retrograde placements are described for each column [2, 5–9]. Therefore, we assessed the relationship of both entrance points of each screw to surrounding structures. A randomised order for the different entry points was used when placing anterior or posterior column screws (Figs. 2, 3, 4 and 5).
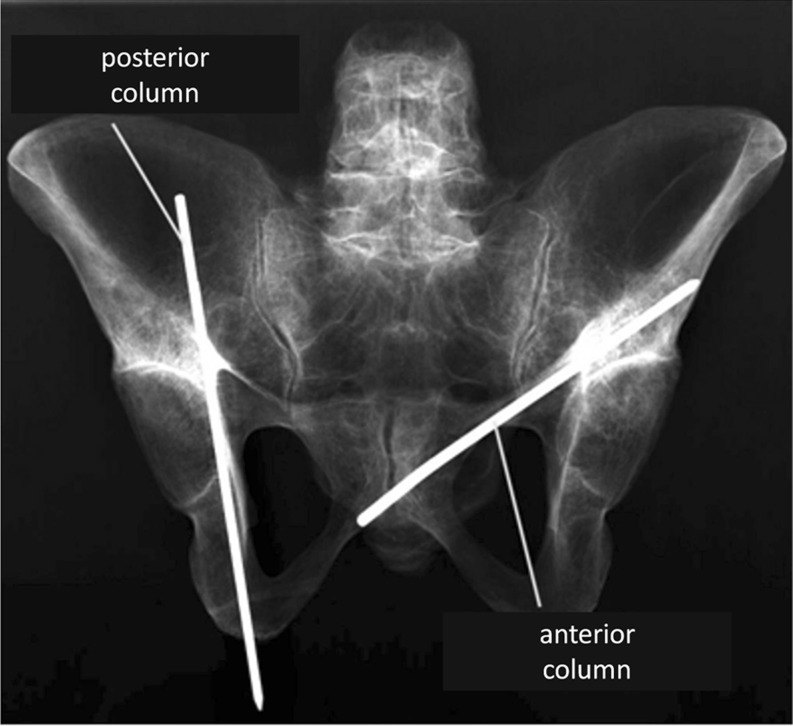
Fig. 1.
Anteroposterior (AP) radiograph of a full pelvis specimen with both anterior and posterior columns addressed by one wire each for demonstration purposes
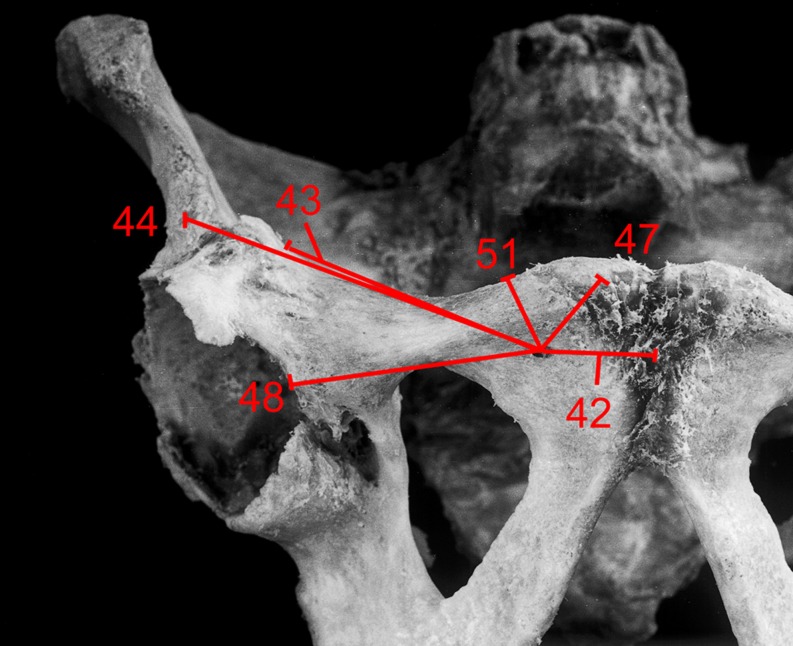
Fig. 2.
Specimen with retrograde entry point of anterior column screw. Distances to the different bony landmarks are marked in straight lines. Numbers are for identification use
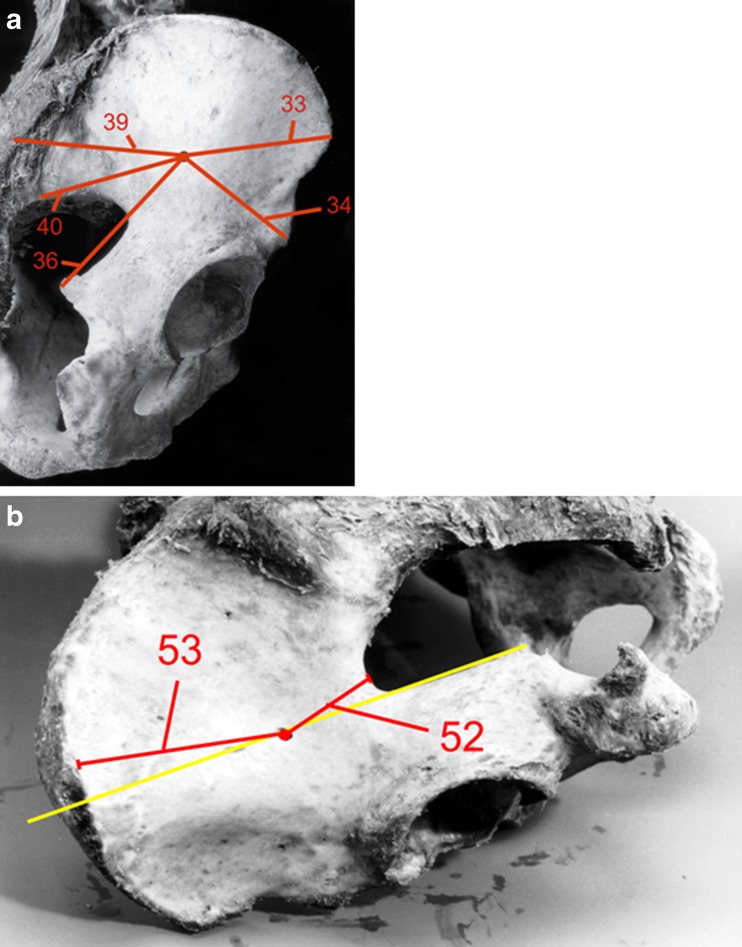
Fig. 3.
a, b Specimen with antegrade entry point of anterior column screw. Distances to the different bony landmarks are marked in straight lines. Numbers are for identification use
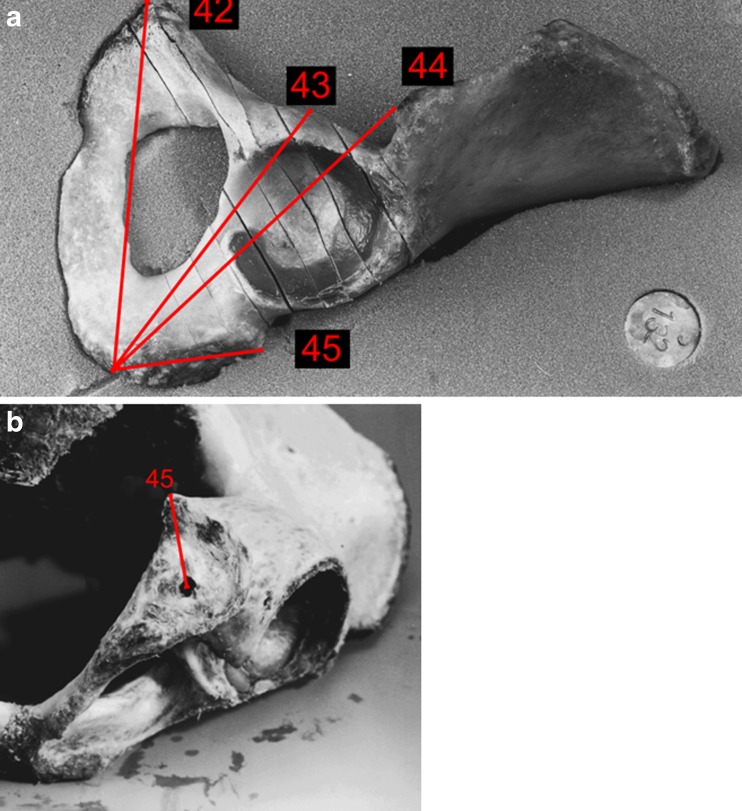
Fig. 4.
Specimen with antegrade entry point of posterior column screw. Distances to the different bony landmarks are marked in straight lines. Numbers are for identification use
Fig. 5.
a, b Specimen with retrograde entry point of posterior column screw. Distances to the different bony landmarks are marked in straight lines. Numbers are for identification use
The screw for the posterior column was inserted antegrade from the inner aspect of the ilium towards the ischium. The anterior column screw was directed retrograde from the outer superior pubic ramus to the outer surface of the ilium, as described by Stöckle et al. [7]. The distance to numerous osseous landmarks were assessed by drawing a direct line, mimicking information gathered by 2D fluoroscopic visualisation. Statistical analysis was performed using the descriptive methods of SPSS v.19 for Windows (SPSS Inc., Chicago, IL, USA). The Mann–Whitney U test was used to evaluate gender-specific differences in measured parameters. Results were considered to be significant when p value was <0.05.
Results
At the entry point of the retrograde anterior column screw, there was a significant difference in the distance to the cranial rim of the superior pubic ramus (p = 0.002), with a shorter distance for female specimens (Table 1). The distance to the iliopectineal eminence, the anterior inferior iliac spine and the pubic tubercle showed low interspecimen deviation, with no distance exceeding 2.5 cm above the mean values.
Table 1.
Distance of screw entry point to various landmarks. Identification number in brackets (see Fig. 2)
| Distance of retrograde entry point anterior column screw to various landmarks | Male specimen | Female specimen | P value |
|---|---|---|---|
| Mean [cm; (range) standard deviation] | |||
| Centre of symphysis (42)a | 2.7 (2.0–3.1) 0.34 | 2.8 (1.4–4.2) 0.98 | 0.653 |
| Iliopectineal eminence (43)a | 5.4 (4.6–6.4) 0.60 | 5.3 (4.2–6.4) 0.82 | 0.749 |
| Anterior inferior iliac spine (44)a | 9.3 (8.5–9.8) 0.46 | 9.0 (8.1–10.0) 0.71 | 0.370 |
| Pubic tubercle (47)a | 1.7 (1.2–2.1) 0.28 | 1.4 (0.3–2.4) 0.70 | 0.368 |
| Medial acetabular rim (48)a | 5.0 (3.5–6.0) 0.88 | 4.8 (4.2–6.7) 0.98 | 0.847 |
| Cranial rim of superior pubic ramus (51)a | 1.5 (1.2–1.7) 0.20 | 0.9 (0.3–1.3) 0.38 | 0.002 |
asee Fig. 2
When placing the anterior column screw in the antegrade direction (Table 2), the distance to the anterior inferior iliac spine was significantly different between sexes (p = 0.007). The distance to the posterior superior and inferior iliac spine was the most consistent distance between sexes, with differences in mean values <0.5 cm.
Table 2.
Distance of screw entry point to various landmarks. Identification number in brackets (see Fig. 3a,b)
| Distance of antergrade entry point anterior column screw to various landmarks | Male specimen | Female specimen | P value |
|---|---|---|---|
| Mean [cm; (range) standard deviation] | |||
| Anterior superior iliac spine (33)a | 7.1 (6.2–8.0) 0.61 | 6.6 (5.5–7.7) 0.86 | 0.224 |
| Anterior inferior iliac spine (34)a | 6.5 (5.0–8.5) 1.23 | 4.7 (4.0–5.3) 0.46 | 0.007 |
| Iliac crest (36)a | 9.3 (8.5–10.7) 0.76 | 7.8 (6.0–9.0) 1.21 | 0.025 |
| Posterior superior iliac spine (39)a | 10.3 (8.4–11.6) 1.38 | 10.5 (9.5–12.0) 0.86 | 0.949 |
| Posterior inferior iliac spine (40)a | 7.4 (6.6–8.9) 0.93 | 7.3 (5.8–8.5) 0.96 | 0.949 |
| Vertex of greater sciatic notch (52)a | 4.2 (3.4–5.4) 0.70 | 3.7 (2.5–4.9) 0.96 | 0.276 |
| External lip of iliac crest (53)a | 6.6 (5.0–7.9) 1.09 | 6.9 (5.8–7.7) 0.67 | 0.607 |
asee Fig. 3a, b
There were no gender differences in measurements around the antegrade entry point of the posterior column screw (Table 3). The mean distance to the ischial spine, linea terminalis and anterior inferior iliac spine was similar in both sexes. In the retrograde approach (Table 4), distances to the iliopectineal eminence and anterior inferior iliac spine were different between genders (p = 0.003 and p = 0.006, respectively).
Table 3.
Distance of screw entry point to various landmarks. Identification number in brackets (see Fig. 4)
| Distance of antegrade entry point posterior column screw to various landmarks | Male specimen | Female specimen | P value |
|---|---|---|---|
| Mean [cm; (range) standard deviation] | |||
| Anterior superior iliac spine (33)a | 7.4 (6.6–8.9) 0.86 | 7.3 (6.1–8.0) 0.62 | 0.830 |
| Anterior inferior iliac spine (34)a | 5.3 (5.0–5.6) 0.22 | 5.3 (4.0–6.1) 0.75 | 0.519 |
| Iliopectineal eminence (35)a | 5.1 (3.9–6.3) 0.97 | 5.7 (3.5–7.8) 1.48 | 0.390 |
| Ischial spine (36)a | 8.0 (6.2–10.1) 1.38 | 8.0 (6.9–9.5) 0.93 | 0.886 |
| Sacroiliac joint on height linea terminalis (37)a | 3.5 (3.0–4.2) 0.49 | 3.2 (2.1–4.5) 0.76 | 0.281 |
| Linea terminalis (56)a | 1.5 (0.8–3.4) 0.99 | 1.5 (0.5–2.5) 0.86 | 0.885 |
asee Fig. 4
Table 4.
Distance of screw entry point to various landmarks. Identification number in brackets (see Fig. 5a,b)
| Distance of retrograde entry point posterior column screw to various landmarks | Male specimen | Female specimen | P value |
|---|---|---|---|
| Mean [cm; (range) standard deviation] | |||
| Centre of symphysis (42)a | 12.7 (11.6–13.4) 0.74 | 12.0 (11.5–12.4) 0.36 | 0.073 |
| Iliopectineal eminence (43)a | 11.5 (10.9–12.0) 0.42 | 9.8 (9.3–10.4) 0.42 | 0.003 |
| Anterior inferior iliac spine (44)a | 13.7 (12.8–14.3) 0.54 | 12.1 (11.2–13.6) 0.75 | 0.006 |
| Ischial tuberosity (45)a | 2.6 (1.5–3.3) 0.71 | 2.7 (1.1–4.1) 1.09 | 0.830 |
asee Fig. 5a, b
Discussion
Apart from standard surgical approaches in acetabular surgery, there are indications for minimally invasive techniques [2, 9]. These methods are indicated when soft-tissue damage needs to be limited—as in the elderly or polytraumatised patient in whom recovery from extensive surgical intervention is at risk [1, 10, 11]. In the presence of large fracture fragments, screw fixation alone proved satisfactory [7], and in biomechanical testing, lag-screw fixation in transverse or T-shaped fractures was at least comparably effective with plate fixation [12]. In minimally displaced fractures, single screw implantation allowed faster patient mobilisation and accelerated recovery [13]. For these situations, percutaneous screw implantation can be successful. In our study, we identified reliable anatomical osseous landmarks for this procedure and indicated gender-derived variations.
Mu et al. [14] described optimal entry points for antegrade screw placement in the posterior column in the hemipelvis of 30 dried specimens. Findings in their study for the optimal entry point in relation to the iliosacral joint and linea terminalis were comparable with findings in our study. However, those authors did not distinguish between male and female specimens. Benedetti et al. [15] performed an analysis of the thickness of the anterior column in relation to the acetabular margin. Although there was a balanced quotient of male and female specimens, they found no statistically significant differences. They described their safe zone in relation to the acetabular boundaries [15], whereas we used various osseous landmarks. A similar setting was used by Xian-quan et al., who evaluated the maximum possible screw lengths in the anterior column without differentiating between gender [16]. They also performed their investigation assuming an anterior approach to the acetabulum, whereas our study imitates a closed technique with long periarticular screws. We evaluated statistically significant different findings between genders in the retrograde entry point of dorsal column screws and in both entry points of anterior column screws. Puchwein et al.’s study from 2012 substantiated our findings by demonstrating gender differences in most of the assessed landmarks [11]. A safe zone was defined by Guy for an anterior approach [3] with 93 CT scans evaluated. However, they drew their findings from CT evaluation with a known limitation of reliability resulting from a calculation based on a defined slice thickness. They emphasised that the safe corridors are narrow, and percutaneous screw placement remains a challenging procedure. Hong showed in 30 acetabular screws (21 placed in the anterior column and nine in the posterior column) that percutaneous placement was possible not only in undisplaced but also in mildly displaced fracture situations [9]. Routt presented retrograde screw placement through the medullary superior pubic ramus [6]. In 24 out of 26 patients, this method could be achieved, thus avoiding extensile surgical exposure. An ideal starting point just inferior to the pubic tubercle and lateral to the symphyseal meniscus was described. However, in two patients, inaccurate screw placement was observed. Simonian demonstrated a biomechanically comparable fixation using a retrograde medullary superior pubis ramus screw with standard plating techniques [17]. Interestingly, shorter screws medial to the hip joint demonstrated comparable strength to longer periarticular screws. Additionally, Routt [6] reported that only a few screws had to pass beyond the acetabular borders because superior pubic ramus fractures were primarily addressed. In our study, the columns of the acetabulum were addressed, and therefore, longer screw paths through the osseous canal were used. Furthermore, we defined our entry points with exact measurements. Kazemi et al. [13] placed screws in 28 patients with fluoroscopy guidance. They used the anterior inferior iliac spine and a supra-acetabular direction perpendicular to the anterior column fracture line as landmarks. Moushine et al. [18] used the pubic tubercle as the osseous entry point in 18 patients. However, it remains unclear in those studies whether the length of the osseous canal was used to full capacity. In another study with complex acetabular fractures, the posterior column screw (7.0 mm) was inserted with the starting point descripition being “ischial bone” [8]. This reflects our impression that the starting point might not be considered critical by most surgeons and that screw placement is guided by other factors. With the help data we present here, a standardised starting point might be an additional safety factor.
The significance of our study lies in its reliable osseous landmarks. Using navigation systems can be technically challenging, and financial considerations might hinder a widespread acceptance. We present values that might help experienced surgeons manage percutaneous screw placement with fluoroscopy guidance only. Crowl described percutaneous fixation in 23 patients with the aid of fluoroscopy, CT guidance or computer assistance [5]. The authors claim these assistance techniques to be safe for anterior column acetabular fractures. On the other hand, Carmack found no differences in detecting screw penetration in acetabulum surgery when comparing intraoperative fluoroscopy and postoperative CT [19]. This data was supported by Norris [20], who demonstrated sufficient efficacy in evaluating acetabulum fracture reduction and hardware placement with the help of fluoroscopy. With the gold standard yet to be defined, we present reliable and easily assessable structures with special regard to gender differences.
Our study has several limitations: Results are based solely on osseous structures in a 2D model. No CT scan evaluation for 3D analysis was conducted. Therefore, caution should be exercised when extrapolating these findings to the operating theatre. Soft-tissue coverage and adjoining nerves and vessels must be respected when placing implants, especially in percutaneous approaches. However, through the wide-spread of 2D fluoroscopy, the landmarks presented in this report are easily and reliably visualised. However, it is not always possible to achieve anatomical reduction, and therefore, intraoperative clinical findings might differ from our results, which were assessed on nonfractured specimens. This technique is mainly indicated in less displaced fractures, which may justify our conclusions.
Conclusions
This study describes reliable osseous landmarks for entry points of antegrade and retrograde periarticular screw implantation in the anterior or posterior acetabulum column. Our findings may be of help to the pelvic surgeon when placing long screws in the safe osseous corridors. Future clinical studies are needed to verify the benefit of our findings for patient safety.
Acknowledgements
We thank Annette Weiss for her excellent assistance in collecting data for this study.
Competing interests
The authors declare that they have no competing interest.
Authors’ contributions
All authors were involved in the research project and approved the final version of the manuscript. TD, BF, RS, MM, FM, AB collected data, analysed and interpreted these data and were involved in drafting and revising the manuscript. MN contributed substantially to study conception and design and gave critical and final approval. All authors read and approved the final manuscript.
References
- 1.Culemann U, Holstein JH, Kohler D, Tzioupis CC, Pizanis A, Tosounidis G, Burkhardt M, Pohlemann T. Different stabilisation techniques for typical acetabular fractures in the elderly–a biomechanical assessment. Injury. 2010;41(4):405–410. doi: 10.1016/j.injury.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Gary JL, VanHal M, Gibbons SD, Reinert CM, Starr AJ. Functional outcomes in elderly patients with acetabular fractures treated with minimally invasive reduction and percutaneous fixation. J Orthop Trauma. 2011;26(5):278–283. doi: 10.1097/BOT.0b013e31823836d2. [DOI] [PubMed] [Google Scholar]
- 3.Guy P, Al-Otaibi M, Harvey EJ, Helmy N. The ‘safe zone’ for extra-articular screw placement during intra-pelvic acetabular surgery. J Orthop Trauma. 2010;24(5):279–283. doi: 10.1097/BOT.0b013e3181bfcebf. [DOI] [PubMed] [Google Scholar]
- 4.Kendoff D, Citak M, Gardner MJ, Stubig T, Krettek C, Hufner T. Intraoperative 3D imaging: value and consequences in 248 cases. J Trauma. 2009;66(1):232–238. doi: 10.1097/TA.0b013e31815ede5d. [DOI] [PubMed] [Google Scholar]
- 5.Crowl AC, Kahler DM. Closed reduction and percutaneous fixation of anterior column acetabular fractures. Comput Aided Surg. 2002;7(3):169–178. doi: 10.3109/10929080209146027. [DOI] [PubMed] [Google Scholar]
- 6.Routt ML, Jr, Simonian PT, Grujic L. The retrograde medullary superior pubic ramus screw for the treatment of anterior pelvic ring disruptions: a new technique. J Orthop Trauma. 1995;9(1):35–44. doi: 10.1097/00005131-199502000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Stockle U, Hoffmann R, Nittinger M, Sudkamp NP, Haas NP. Screw fixation of acetabular fractures. Int Orthop. 2000;24(3):143–147. doi: 10.1007/s002640000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu YH, Tseng IC, Su CY, Huang JW, Wu CC. Modified technique of percutaneous posterior columnar screw insertion and neutralization plate for complex acetabular fractures. J Trauma. 2012;71(1):198–203. doi: 10.1097/TA.0b013e3181f2d50f. [DOI] [PubMed] [Google Scholar]
- 9.Hong G, Cong-Feng L, Cheng-Fang H, Chang-Qing Z, Bing-Fang Z. Percutaneous screw fixation of acetabular fractures with 2D fluoroscopy-based computerized navigation. Arch Orthop Trauma Surg. 2011;130(9):1177–1183. doi: 10.1007/s00402-010-1095-2. [DOI] [PubMed] [Google Scholar]
- 10.Vioreanu MH, Mulhall KJ. Intra-operative imaging technique to aid safe placement of screws in percutaneous fixation of pelvic and acetabular fractures. Acta Orthop Belg. 2011;77(3):398–401. [PubMed] [Google Scholar]
- 11.Puchwein P, Enninghorst N, Sisak K, Ortner T, Schildhauer TA, Balogh ZJ, Pichler W. Percutaneous fixation of acetabular fractures: computer-assisted determination of safe zones, angles and lengths for screw insertion. Arch Orthop Trauma Surg. 2012;132(6):805–811. doi: 10.1007/s00402-012-1486-7. [DOI] [PubMed] [Google Scholar]
- 12.Chang JK, Gill SS, Zura RD, Krause WR, Wang GJ. Comparative strength of three methods of fixation of transverse acetabular fractures. Clin Orthop Relat Res. 2001;392:433–441. doi: 10.1097/00003086-200111000-00057. [DOI] [PubMed] [Google Scholar]
- 13.Kazemi N, Archdeacon MT. Immediate full weightbearing after percutaneous fixation of anterior column acetabulum fractures. J Orthop Trauma. 2011;26(2):73–79. doi: 10.1097/BOT.0b013e318216b3e3. [DOI] [PubMed] [Google Scholar]
- 14.Mu WD, Wang XQ, Jia TH, Zhou DS, Cheng AX. Quantitative anatomic basis of antegrade lag screw placement in posterior column of acetabulum. Arch Orthop Trauma Surg. 2009;129(11):1531–1537. doi: 10.1007/s00402-009-0836-6. [DOI] [PubMed] [Google Scholar]
- 15.Benedetti JA, Ebraheim NA, Xu R, Yeasting RA. Anatomic considerations of plate-screw fixation of the anterior column of the acetabulum. J Orthop Trauma. 1996;10(4):264–272. doi: 10.1097/00005131-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Xian-quan W, Jin-fang C, Xue-cheng C, Wei-dong M, Wei Z, Shui S, Jin-lu Z, Jian W, Wei L. A quantitative anatomic study of plate-screw fixation of the acetabular anterior column through an anterior approach. Arch Orthop Trauma Surg. 2010;130(2):257–262. doi: 10.1007/s00402-009-0960-3. [DOI] [PubMed] [Google Scholar]
- 17.Simonian PT, Routt ML, Jr, Harrington RM, Tencer AF. Internal fixation of the unstable anterior pelvic ring: a biomechanical comparison of standard plating techniques and the retrograde medullary superior pubic ramus screw. J Orthop Trauma. 1994;8(6):476–482. [PubMed] [Google Scholar]
- 18.Mouhsine E, Garofalo R, Borens O, Wettstein M, Blanc CH, Fischer JF, Moretti B, Leyvraz PF. Percutaneous retrograde screwing for stabilisation of acetabular fractures. Injury. 2005;36(11):1330–1336. doi: 10.1016/j.injury.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 19.Carmack DB, Moed BR, McCarroll K, Freccero D. Accuracy of detecting screw penetration of the acetabulum with intraoperative fluoroscopy and computed tomography. J Bone Joint Surg Am. 2001;83-A(9):1370–1375. doi: 10.2106/00004623-200109000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Norris BL, Hahn DH, Bosse MJ, Kellam JF, Sims SH. Intraoperative fluoroscopy to evaluate fracture reduction and hardware placement during acetabular surgery. J Orthop Trauma. 1999;13(6):414–417. doi: 10.1097/00005131-199908000-00004. [DOI] [PubMed] [Google Scholar]