Abstract
Purpose
The purpose of this study was to present a retrospective comparative overview of the Ilizarov non-free bone plasty techniques of one-stage multilevel fragment lengthening and gradual tibilisation of the fibula used for extensive tibial defect management.
Methods
Extensive tibial defects in 83 patients were managed either by multilevel fragment lengthening (group I, n = 41, mean defect size 13.1 ± 0.9 cm) or gradual tibilisation of the fibula (group II, n = 42, mean defect size 12.5 ± 1.2 cm) using the Ilizarov apparatus. The initial findings, treatment protocols and outcomes of those patients treated within the period 1972–2011 were studied retrospectively by medical records and radiographs, and statistically assessed with Microsoft Excel and Attestat software.
Results
Group I had multilevel fragment lengthening over one stage that averaged 288.0 ± 14.4 days. The mean total period of gradual tibilisation of the fibula in group II was 316.0 ± 29.7 days. The patient’s age in the latter group had an effect on the completeness of leg-length equalisation.
Conclusions
The techniques can be used to manage extensive tibial defects as all the defects bridged, leg-length discrepancy and deformity were corrected and patients were able to load their limbs.
Introduction
Poor outcomes in the management of long-bone defects with free allografts or autografts were associated, first of all, with the lack of good intraosseous blood flow and prolonged bone tissue remodelling in cases of massive replants [1]. Infection, rejection, degradation, non-union and allograft or autograft fractures were the most observed complications with their rate in the range of eight to 60 % [2–4]. Therefore, the use of vascularised autografts for extensive tibial defects was considered to be the most effective method of reconstructive bone surgery [5–7]. Nowadays, the Ilizarov non-free bone plasty and free vascularised autografts have been universally acknowledged as two alternative ways for bone defect management [8, 9].
Ideally, the Ilizarov bone plasty implies a gradual transport of a vascularised osteotomised bone autograft that is enveloped into soft tissues and induces guided tubular bone formation in the defect gap both in length and shape. The system of Ilizarov bone reconstruction for defect management is based on two main techniques: lengthening of a defect fragment through an osteotomy with consolidation of the transported fragment at the docking site, and gradual tibiofibular synostosis or gradual tibilisation of the fibula. Each of them may include specific ways or technical solutions that are used according to a particular orthopaedic situation and clinical rehabilitation objectives. The technique of bone defect fragment lengthening is implemented by bifocal or polyfocal osteotomies and osteosynthesis when one or several distraction regenerates are formed followed by union at the docking site. The technique of tibilisation uses gradual transport of an osteotomised cylindrical fibular fragment or of a split fibular portion in the medial direction into a tibial defect for further union with the tibial fragments [10, 11].
It was believed that the most rational and efficient way of filling in long-bone defects would be lengthening of one tibial fragment in one stage to the amount in the range of five to ten centimetres as far as such a volume of a new regenerated bone could be provided by high level distraction osteogenesis and would result in the optimal treatment time and rehabilitation process [10–12].
However the reported outcomes and our clinical findings showed that hypoplastic bone formation could happen during defect filling when a single-level distraction regenerate was grown to more than five centimetres or to the length that exceeded 40 % of the original segment. Thus, osteogenesis was delayed in 1.6–13.8 % of the cases when one-stage defect fragment lengthening was used to the amount of eight to ten centimetres, and the distraction regenerate tended to assume the shape of an hour-glass [11]. It was also reported that in total nine to 18 months were necessary if one-fragment lengthening was used to manage tibial defects that ranged from six to 12 cm [11–14].
The aim of our retrospective comparative study was to present an overview of the two techniques of the Ilizarov non-free bone plasty used for extensive tibial defects in the cases when it was impossible or doubtful whether the deficiency of the tibial bone stock could be completely restored at one distraction osteogenesis level. We planned to analyse the completeness of defect filling, total treatment time, and the indications to use the techniques of multilevel fragment lengthening and fibula transport for tibial reconstruction in the studied groups.
Materials and methods
Our series were one-stage approaches for managing extensive tibial defects of more than ten centimetres in 83 patients who were treated either by multilevel lengthening or gradual fibula tibilisation at our specialised clinic and who were followed up for not less than one year (range one to ten years).
Group 1
Group 1 comprised 41 patients who were treated from 1992 till the end of 2011 by multilevel distraction osteogenesis that was produced on one or both tibial fragments (Table 1). They had had a total of 129 unsuccessful previous interventions, including 32 operations using Ilizarov techniques at other clinics. Thirty-one patients (75.6 %) had scarred soft tissues that adhered internally to tibial fragments. In group 1, we used two technical solutions for tibial defect management: lengthening of one fragment by bifocal proximal fragment distraction in 21 cases and by bifocal distal fragment distraction in six cases, or lengthening of both fragments in 14 cases (Fig. 1), including four cases of combining lengthening of one fragment at one level while the other was lengthened bifocally.
Table 1.
Initial findings and outcomes in two groups of non-free Ilizarov bone plasty
| Parameters | Group 1 | Group 2 |
|---|---|---|
| Male/female | 29/12 | 25/17 |
| Mean age (years) | 20.7 ± 11.1 | 19.9 ± 9.3 |
| Children | 15 | 14 |
| Adults 18–40 years old | 21 | 20 |
| Adults older than 40 years | 5 | 8 |
| Defect origin | ||
| Injuries including consequences | 21 | 17 |
| Haematogenous osteomyelitis | 4 | 25 |
| Congenital | 9 | – |
| Tumour resection | 7 | – |
| Mean anatomical shortening (cm) | 6.6 ± 0.7 | 4.6 ± 2.8 |
| Bone defect | 13.1 ± 0.9 | 12.5 ± 1.2 |
| Fragment ends shape, congruent/incongruent | 7/34 | 13/29 |
| Contractures | ||
| Knee joint | 7 | 14 |
| Ankle joint | 3 | 9 |
| Both joints | 34 | 6 |
| Ankle ankylosis | 4 | 13 |
| Knee ankylosis | – | 1 |
| Weight-bearing | 0 | 0 |
| Condition duration (years) | 5.8 ± 1.9 | 11.8 ± 8.4 |
| Number of metaphyseal osteotomiesa | 55 | |
| Number of diaphyseal osteotomies | 31 | 84 |
| Total treatment time with the frame on (days) | 288.0 ± 14.4 | 316.0 ± 29.7 |
| Mean gradual bone transport (days) | 97.7 ± 5.9 | 98.1 ± 14.0 |
| Distraction for tibial fragment separation/correction (days) | – | 84.7 ± 22.7 |
| Tibiofibular synostosis (days) | – | 88.6 ± 14.7 |
| Mean fixation time (days) | 170.3 ± 12.4 | 166.3 ± 22.7 |
| Bone defect filling (cm) | 11.4 ± 0.8 | 12.5 ± 1.2 |
| Restoration of lower leg length (%) | 88.4 ± 2.4 | 64.3 ± 1.1 |
| Cases of residual anatomical leg discrepancy (≥ 3 cm) | 4 | 19 |
| Contractures at follow-ups | ||
| Knee joint | – | 7 |
| Ankle joint | 3 | 4 |
| Both joints | – | |
| Foot equinus | – | 3 |
| Ankle ankylosis | 4 | 13 |
| Knee ankylosis | – | – |
| Weight-bearing | 41 | 42 |
a Group I—tibial metaphysis; group II—fibular metaphysis
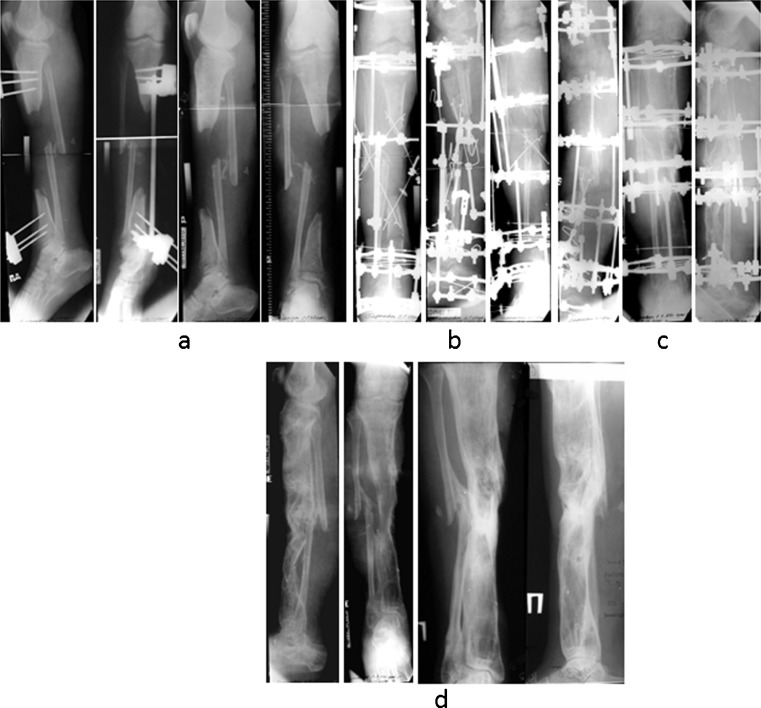
Fig. 1.
a A 15-cm post-traumatic defect of the right tibia associated with soft and vascular disorders in a 37-year-old patient due to explosion was fixed with the Wagner device on admission. He had thermal burns, partial free skin grafting of the extensive wound with necrosis and granulation on the anteromedial side of the leg, absent pulsation of the tibialis аnterior and dorsalis pedis, reduced arterial tone and marked asymmetry of blood filling, as well as impaired venous outflow according to ultrasound Doppler reovasography. b Both tibial fragments had corticotomies and were transported with distraction guiding wires at a rate of 0.25 mm three to four times a day for 68 days at the proximal distraction level and 90 days at the distal one. c Bone transport of the third fragment followed after an additional corticotomy of the proximal fragment at a rate of 0.5–0.75 mm a day for 67 days; adaptation at the docking site was open. Fixation with the frame on was 165 days. The wound closed by the end of fixation. d Outcome at a 1.5-years follow-up
Group 2
Group 2 included 42 patients who were treated using the technique of gradual tibilisation of the fibula to reconstruct tibial defects in the period between 1972 and 2011 (Table 1). Thirty-two cases (76.2 %) were subtotal defects. Nine patients had associated diaphyseal defects in the fibula. The fibula was hypertrophic and mimicked the deformity in the tibia in 33 cases. All the patients had marked blood supply disorders in the lower leg. Arteriography and Doppler radiography revealed main stream circulation disorders in the pools of the posterior and anterior tibial arteries in 39 patients (92.8 %). All the patients had soft tissue scarring in the area of non-unions, and the scars were internally adherent to the adjacent ends of the tibial fragments in 14 patients. Each patient had undergone four or more surgical procedures prior to admission to our department. In group II, the fibula was osteotomised at two levels that corresponded to the levels of the tibial fragments ends in the defect, and the fibular fragment was gradually transported in a medial direction to the tibial gap in three to four steps a day, 0.25 mm each (Fig. 2). Compression was produced at the docking sites with the tibial fragments for tibiofibular synostosis. Moreover, we simultaneously performed longitudinal stretching on the fixator rods to reduce anatomical shortening when it was possible.
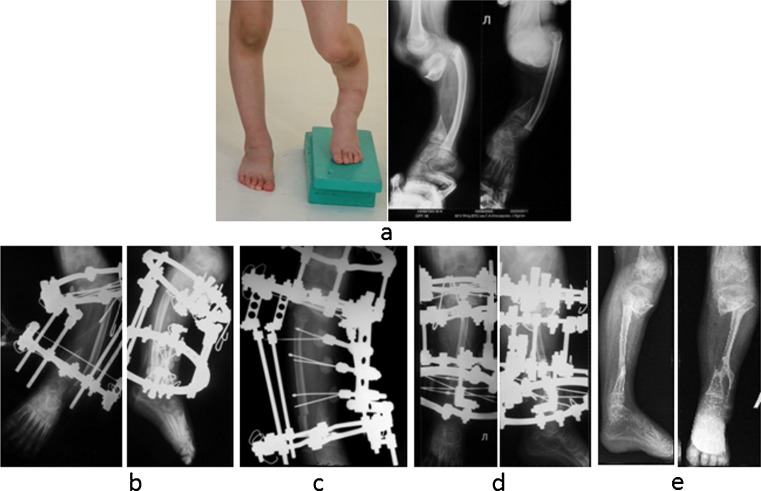
Fig. 2.
a X-rays of a 6-year-old patient treated in 2010 who had a 7-cm diaphyseal defect of the left tibia with icicle-like fragment ends, varus and recurvation deformity (165/165°), proximal fibular head dislocation, and anteromedial rigid skin scars adhered to the fragment ends as a consequence of umbilical sepsis. Thick fibula mimicked the deformity of the tibia. b Ilizarov frame was applied for 70 days to correct the deformity and bring the fibula head down. c Double osteotomy of the fibula followed. d The cylinder-like fibular fragment was transported for 29 days to be docked to the tibial fragments, and fixation was 113 days. e Total treatment was 217 days. Residual discrepancy was 3 cm on Ilizarov frame removal
Preoperative data, operative data, duration of treatment, functional outcomes, and complications were studied in both groups.
Microsoft Excel and version 1.0 of the AtteStat software were used for statistical processing [15].
The study was approved by the institutional ethics committee and was conducted in accordance with the ethical standards laid down in the Declaration of Helsinki. The study of human subjects followed the rules of clinical practice in the Russian Federation (RF Ministry of health order # 266 from 19.06.03).
Results
In group 1, all the defects bridged either by simultaneous distraction regeneration at the osteotomised levels, or an additional corticotomy was used during the distraction period for consecutive trifocal lengthening (Fig. 1). Distraction osteogenesis was complicated in four cases as the guiding olive wires cut out of the elongated fragments due to osteoporosis, and those wires were replaced. The tibial artery was injured during the performance of an additional corticotomy in a nine-year-old patient that resulted in post-traumatic aneurism that was resected and sutured. That complication did not affect the outcome or treatment time. Axial alignment and consolidation were achieved in all cases. No age to outcome relationship was observed in this group, and the residual shortening in four cases was functionally useful due to ankle ankylosis or contracture. At follow-up, all patients walked without additional aids (Table 1).
We used gradual medial fibular fragment transport alongside simultaneous deformity correction in group 2 patients (Fig. 2). All the defects bridged, but it was not possible to restore limb-length completely in six adults older than 40 years of age and growing children in one stage. All the patients could bear weight after the reconstruction, and the treatment was limb-salvage (Table 1).
Ten patients developed superficial peroneal nerve neuritis and two had peroneal nerve paresis. We reduced the transport rate or stopped distraction for two to three days, and administered analgesics until the signs were relieved. Seven patients had soft tissue infection around the wires treated by both local injections and general administration of antibiotics. One patient who had wire osteomyelitis required an additional debridement surgery (sequestrectomy).
Deformities due to full loading immediately after apparatus removal occurred in six patients, and they had re-operations. In 13 cases limb discrepancy did not exceed three centimetres and was functional due to ankle ankylosis.
The comparison of initial findings showed that the groups were different in several parameters at the onset of treatment though the mean bone defect size was similar. Group 1 tibial fragments were of bigger sizes, the aetiology was mostly post-traumatic and the location was mainly in the middle or lower diaphysis in 33 cases. In group 2, lengthening procedures and consolidation of the atrophic tibial fragments mostly after necrotic bone resection were technically impossible due to subtotal defects, fragments’ small sizes and incongruent shape, disturbed major blood flow in the involved segment, low potential of bone tissue to regeneration, and soft tissue degeneration due to rough scars. Therefore, the fibula was used to reconstruct the tibia in such conditions.
Discussion
Extensive bone defects remain a challenge for orthopaedic surgeons in so far as the number of high energy injuries has been constantly growing. The Ilizarov method has been universally accepted as a method of choice among the orthopaedic community [12–14]. But the practical application of the Ilizarov single level transport to bridge the defect gap in the range of six–12 cm required prolonged fixation in the frame or featured delayed regeneration [11–14]. Our results in group 1 show the possibility of bone stock gain at the expense of multilevel lengthening for a shorter total osteosynthesis period and prove our reported experimental findings of sufficient regeneration by multilevel distraction for defect filling [16].
Several studies have shown that the degree of regenerated bone maturation should be considered during defect management. It was shown that the docking site union was the main factor for Ilizarov frame removal as the time of regenerated bone remodelling during fixation would also be sufficient for the contacting regenerate remodelling to provide union at the docking site, independent of open or closed variants [10, 11, 16, 17]. Therefore, the decision about the Ilizarov frame removal time should be one of the key moments during extensive defect management [11, 16, 17]. Nevertheless, failure to achieve docking site union has been reported in one fragment transport [2, 4, 13, 14]. According to our findings, failures occur due to the fact that the remodelling and continuous cortex in the regenerate peripheral areas develops earlier than the docking site union [11]. Therefore, the quality of the docking site union was considered first before Ilizarov frame removal, and resulted in consolidation in all our cases.
According to the literature, the techniques of acute non-vascularised contralateral or ipsilateral fibula transfer have resulted in limb weight-bearing in the majority of cases, and those techniques were considered technically easier than microvascular and Ilizarov techniques [18, 19]. However, their chances for success in the conditions of poor blood supply would be very low. Therefore, experienced surgeons prefer vascularised fibula grafts for extensive tibial defect management but their harvesting is either frequently technically difficult, or the transplantation itself is not possible. Clinical practice has also shown that the treatment time was longer when vascularised fibula transposition technique was used in the conditions of poor blood supply [20]. Having acknowledged the advantages of using free vascularised fibular grafts, some authors noted that the main problem was fatigue fractures of the fibula grafts that required additional interventions [5–7, 20, 21]. A free vascularised fibular graft reorganises slowly or frequently features secondary resorption as the transcortical blood outflow and blood recirculation in the transplanted fragment impede the donor bone acquisition of the required size. Therefore, the patients were advised not to bear weight on the operated limb until the graft hypertrophy developed. Moreover, free bone plasty with arteriovenous shunting results in a prolonged and traumatic intervention followed by administrations of medication [4, 9].
The Ilizarov non-free bone plasty made it possible to manage defects without free bone and skin grafts. The fibula seems to be a good biological graft when used for the Ilizarov tibiofibular synostosis that is less traumatic and costly as there is no need to intervene on the contralateral segment. Gradual transport of the fibular fragment does not affect the nutrient vessels and results in regeneration and consolidation [6, 11, 22–24].
To date, the reported series of fibula tibilisation, though not large, have been encouraging for avoiding amputation [6, 11, 22–24]. Ours is the largest historical series of patients, and demonstrates that the technique can be carefully carried out at a specific transporting rate thus reducing the incidence of peroneal neuropathy or paresis which could happen by acute fibula transfer in the conditions of scarred soft tissue.
In our view, gradual transport of the fibula should be considered as an alternative method to free bone plasty. Nevertheless, we should point out that the best anatomical outcomes were obtained when bone defects were compensated using the transported massive fibula fragment after double osteotomy and simultaneous stretching of the tibial gap. This contributed to the leg axial alignment and length correction. Also, this type of tibial reconstruction enables correction of associated foot deformities and avoids using preliminary skin plasty for soft tissue scars.
The Ilizarov tibilisation technique requires meticulous planning adapted to each surgical case. The differentiated and individual approach allowed us to equalise leg length in 29 cases of group 2 in one stage. Patients’ age had an effect on the lower leg-length correction. Thus, the reconstructive tibilisation of the fibula provided a complete elimination of leg discrepancy in 18–30-year old patients. In patients older than 40, it was fully corrected in two cases while all the defects bridged.
Conclusions
The two techniques of non-free Ilizarov bone plasty to manage extensive tibial defects can be used when it is impossible or doubtful whether the deficiency of the tibial bone stock can be completely achieved with a single level transport. The multilevel lengthening was possible in a better initial tibial bone condition while tibilisation can be used for subtotal tibial defects with satisfactory outcomes. Non-free vascularised bone grafts represent a useful biological treatment for surgical repair of extensive tibial defects. Patients have a good chance for limb salvage and acceptable function. However, because of the delicate operative techniques the operations should be performed by skilled surgeons in specialised departments.
Acknowledgments
We greatly appreciate the contributions of Prof. V.I. Shevtsov and Prof. V.D. Makushin in the development of the techniques described.
Conflict of interest
None
References
- 1.Kanczler JM, Oreffo RO. Osteogenesis and angiogenesis: the potential for engineering bone. Eur Cell Mater. 2008;15:100–114. doi: 10.22203/ecm.v015a08. [DOI] [PubMed] [Google Scholar]
- 2.Green SA. Skeletal defects. A comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop. 1994;301:111–117. [PubMed] [Google Scholar]
- 3.Rose RE. The Ilizarov technique in the treatment of tibial bone defects. Case reports and review of the literature. West Indian Med J. 2002;51(4):263–267. [PubMed] [Google Scholar]
- 4.Cierny G, Zorn KE. Segmental tibial defects. Comparing conventional and Ilizarov methodologies. Clin Orthop. 1994;301:118–123. [PubMed] [Google Scholar]
- 5.Judet H, Gilbert A, Mathoulin C, Judet J, Judet T, Siguier M, Brumpt B. Reconstruction of loss of bony substance in limbs by free vascularized fibula transplant. Chirurgie. 1991;117(5–6):469–476. [PubMed] [Google Scholar]
- 6.Atkins RM, Madhavan P, Sudhakar J, Whitwell D. Ipsilateral vascularised fibular transport for massive defects of the tibia. J Bone Joint Surg Br. 1999;81(6):1035–1040. doi: 10.1302/0301-620X.81B6.10001. [DOI] [PubMed] [Google Scholar]
- 7.Kühner C, Simon R, Bernd L. Vascularized fibula transplantation in orthopedic oncology. Personal experience and review of the literature. Orthopade. 2001;30(9):658–665. doi: 10.1007/s001320170054. [DOI] [PubMed] [Google Scholar]
- 8.Yokoyama K, Itoman M, Nakamura K, Tsukamoto T, Saita Y, Aoki S. Free vascularized fibular graft vs. Ilizarov method for post-traumatic tibial bone defect. J Reconstr Microsurg. 2001;17(1):17–25. doi: 10.1055/s-2001-12684. [DOI] [PubMed] [Google Scholar]
- 9.El-Gammal TA, Shiha AE, El-Deen MA, El-Sayed A, Kotb MM, Addosooki AI, Ragheb YF, Saleh WR. Management of traumatic tibial defects using free vascularized fibula or Ilizarov bone transport: a comparative study. Microsurgery. 2008;28(5):339–346. doi: 10.1002/micr.20501. [DOI] [PubMed] [Google Scholar]
- 10.Ilizarov GA. Transosseous osteosynthsis. Berlin Heidelberg: Springer; 1992. Pseudoarthrosis and defects of long tubular bones; pp. 453–494. [Google Scholar]
- 11.Shevtsov VI, Makushin VD, Kuftyrev LM (2000) Defects of the lower limb bones. Treatment based on Ilizarov techniques. Chapters 8–12, pp 329–661. Zauralie, Kurgan http://www.ilizarov.ru/en/index.php?option=com_content&view=article&id=304&Itemid=328. Accessed 24 January 2013
- 12.Cattaneo R, Catagni M, Johnson EE. The treatment of infected nonunions and segmental defects of the tibia by the methods of Ilizarov. Clin Orthop. 1992;280:143–152. [PubMed] [Google Scholar]
- 13.Green SA, Jackson JM, Wall DM, Marinow H, Ishkanian J. Management of segmental defects by the Ilizarov intercalary bone transport method. Clin Orthop Relat Res. 1992;280:136–142. [PubMed] [Google Scholar]
- 14.Lenoble E, Lewertowski JM, Goutallier D. Reconstruction of compound tibial and soft tissue loss using a traction histogenesis technique. J Trauma. 1995;39(2):356–360. doi: 10.1097/00005373-199508000-00028. [DOI] [PubMed] [Google Scholar]
- 15.Gaidyshev IP (2004) Solutions for scientific and engineering tasks using Excel, VBA and C/C++. BHV-Peterburg, St. Petersburg (in Russian) http://www.ozon.ru/context/detail/id/1677525/. Accessed 24 January 2013
- 16.Borzunov DY. Long bone reconstruction using multilevel lengthening of bone defect fragments. Int Orthop. 2012;36(8):1695–1700. doi: 10.1007/s00264-012-1562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lovisetti G, Sala AN, Miller AM, Thabed V, Zotolla D, Capitani F. Clinical reliability of closed techniques and comparison with open strategies to achieve union at the docking site. Int Orthop. 2012;36(4):817–825. doi: 10.1007/s00264-011-1260-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kassab M, Samaha C, Saillant G. Ipsilateral fibular transposition in tibial nonunion using Huntington procedure: a 12-year follow-up study. Injury. 2003;34(10):770–775. doi: 10.1016/S0020-1383(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 19.Morsi E. Tibial reconstruction using a non-vascularised fibular transfer. Int Orthop. 2002;26(6):377–380. doi: 10.1007/s00264-002-0378-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laffosse JM, Accadbled F, Abid A, Kany J, Darodes P, Sales De Gauzy J. Reconstruction of long bone defects with a vascularized fibular graft after tumor resection in children and adolescents: thirteen cases with 50-month follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2007;93(6):555–563. doi: 10.1016/S0035-1040(07)92677-X. [DOI] [PubMed] [Google Scholar]
- 21.Yazar S, Lin CH, Wei FC. One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg. 2004;114(6):1457–1466. doi: 10.1097/01.prs.0000138811.88807.65. [DOI] [PubMed] [Google Scholar]
- 22.Catagni MA, Camagni M, Combi A, Ottaviani G. Medial fibula transport with the Ilizarov frame to treat massive tibial bone loss. Clin Orthop Relat Res. 2006;448:208–216. doi: 10.1097/01.blo.0000205878.43211.44. [DOI] [PubMed] [Google Scholar]
- 23.Shiha AE, Khalifa AR, Assaghir YM, Kenawey MO. Medial transport of the fibula using the Ilizarov device for reconstruction of a massive defect of the tibia in two children. J Bone Joint Surg Br. 2008;90(12):1627–1630. doi: 10.1302/0301-620X.90B12.21378. [DOI] [PubMed] [Google Scholar]
- 24.Shafi R, Fragomen AT, Rozbruch SR. Ipsilateral fibular transport using Ilizarov-Taylor spatial frame for a limb salvage reconstruction: a case report. HSS J. 2009;5(1):31–39. doi: 10.1007/s11420-008-9102-7. [DOI] [PMC free article] [PubMed] [Google Scholar]