Abstract
Purpose
The aim of this study was to investigate the biomechanics of the pelvis reconstructed with a modular hemipelvic prosthesis using finite element (FE) analysis.
Methods
A three-dimensional FE model of the postoperative pelvis was developed and input into the Abaqus FEA software version 6.7.1. Mesh refinement tests were then performed and a force of 500 N was applied at the lamina terminalis of the fifth lumbar vertebra along the longitudinal axis of the normal pelvis and the postoperative pelvis for three positions: sitting, standing on two feet, and standing on the foot of the affected side. Stress distribution analysis was performed between the normal pelvis and postoperative pelvis at these three static positions.
Results
In the normal pelvis, stress distribution was concentrated on the superior area of the acetabulum, arcuate line, sacroiliac joint, sacral midline and, in particular, the superior area of the greater sciatic notch. In the affected postoperative hemipelvis, stress distribution was concentrated on the proximal area of the pubic plate, the top of the acetabular cup, the connection between the CS-fixator and acetabular cup and the fixation between the prosthesis and sacroiliac joint.
Conclusions
Stress distribution of the postoperative pelvis was similar to the normal pelvis at three different static positions. Reconstruction with a modular hemipelvic prosthesis yielded good biomechanical characteristics.
Introduction
In recent decades, limb salvage surgery has become more common than hemipelvectomy in the treatment of primary pelvic sarcomas. However, hemipelvic reconstruction after sarcoma resection is critical and many methods for the approach exist, such as massive allograft [1–4], autoclaved autograft [5, 6], custom-made endoprosthesis combined with hip arthroplasty [7–9], modular saddle prosthesis [9–12], and modular hemipelvic endoprosthesis [13, 14]. The modular hemipelvic prosthesis is a new design that can be easily used in surgery and features flexible sizes. We performed this surgery with satisfactory functional outcomes, as previously reported [14].
Finite element (FE) analysis, which can accommodate large inter-subject variations in bone geometry and material properties, has been widely used to analyse pelvic biomechanics [15–19]. An empirically validated FE model can provide information on the static and dynamic responses of joint structures under a variety of loading and boundary conditions that would be difficult or impossible to obtain experimentally [20–22].
The objective of this study was to analyse the biomechanical characteristics of a modular hemipelvic endoprosthesis using FE analysis at different static positions.
Materials and methods
Between 2004 and 2008, twelve patients underwent periacetabular resections and reconstruction with a modular hemipelvic prosthetic system in West China Hospital, Sichuan University. Postoperatively, five patients were able to walk without support, three patients required braces to walk, and four patients were able to walk using a crutch. We chose one patient (male, 63 years old, 176 cm in height, 57 kg in weight) who had a similar hip joint rotation centre reconstruction on the uninjured side and could walk without any support postoperatively. This patient underwent an Enneking Type I/II/III pelvic resection, with resection of part of the gluteus maximus, gluteus medius and tensor fasciae latae. The pelvis was reconstructed using a modular hemipelvic endoprosthesis, and the muscles were reconstructed by suturing the remaining gluteus maximus, gluteus medius and tensor fasciae latae to the iliopsoas. The following steps were carried out, as outlined below.
Three-dimensional reconstruction model of pelvis
A three-dimensional reconstruction model of the pelvis was developed from the chosen patient, 17 months after surgery (Fig. 1). The patient had a long axis body CT scan (Philips Brilliance 64CT, Philips Healthcare, The Netherlands; slice thickness = 0.7 mm, 947slices) while both lower extremities were kept in a neutral position. Because of the titanium prosthesis, the three-dimensional reconstruction model was accompanied by artifacts. We eliminated image artifacts through the difference of the gray value between the prosthesis and artifacts in the CT image. The data were then input into Mimics software (version 8.1, Materialise, Leuven, Belgium) and the three-dimensional reconstruction model of the postoperative pelvis was acquired. Because the patient’s normal pelvis could not be reconstructed directly, we obtained the normal pelvis through copying the uninjured side onto the affected side (Fig. 2).
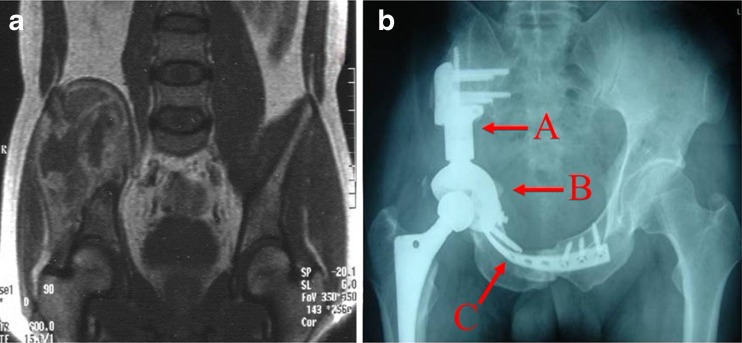
Fig. 1.
a MRI scan shows the tumour before surgery. b Radiographic image of the pelvis 12 months after surgery. A CS-fixator; B acetabular cup; C pubic plate
Fig. 2.
The three-dimensional reconstruction model of the pelvis before surgery (a) and after surgery (b)
Finite element (FE) model of pelvis
The model of three-dimensional reconstruction was input into the Abaqus software (version 6.7.1, Dassault Systemes, Vélizy-Villacoublay, France) and mesh refinement tests were performed. The final FE model consisted of 622,833 tetrahedral elements for the reconstructed pelvis, 728,432 tetrahedral elements for the normal pelvis and 106,103 shell elements for the prosthesis. We applied a force of 500 N to the lamina terminalis of the fifth lumbar vertebra along the longitudinal axis of the normal pelvis and the postoperative pelvis for three positions: sitting, standing on two feet, and standing on the foot of the affected side. The strength of the periacetabular muscles was not considered because it was greatly affected by the widespread resection and could not be calculated accurately.
All implant components were made of continuous isotropy elastomeric materials. Material property values of the implant components were provided by Chunli Zhengda Co. (Beijing, China) (Fig. 3). The CS-fixator and the connection between the CS-fixator and acetabular cup were made of TC4 titanium. The pubis plate was made of TA2 titanium. Values of cortical bone are reported in Table 1 [15, 20, 22–25].
Fig. 3.
a Acetabular cup. b CS-fixator. c Assembly of the acetabular cup and CS-fixator. d Pubic plate
Table 1.
Values of cortical bone and modular hemipelvic endoprosthesis components
| Material | Elasticity (GPa) | Poisson’s ratio | Fatigue resistance (MPa) |
|---|---|---|---|
| Cortical bone | 17 | 0.3 | Acetabulum 120 |
| TA2 Titanium | 105 | 0.33 | Tensile strength (σb) 500, Yield strength (σ0.2) 405 |
| TC4 Titanium | 115 | 0.33 | Tensile strength (σb) 965, Yield strength (σ0.2) 905 |
Results
Three-dimensional reconstruction model of the normal pelvis
Stress distribution was concentrated on the superior area of the acetabulum, arcuate line, sacroiliac joint, sacral midline and, in particular, the superior area of the greater sciatic notch (Table 2; Fig. 4).
Table 2.
Maximum stress in different places of the normal pelvis (MPa)
| Location | Two-legged stance | Single-legged stance | Sitting |
|---|---|---|---|
| Superior sacral midline | 0.8 | 1.2 | 1.0 |
| Sacroiliac joint | 0.9 | 2.5 | 1.1 |
| Superior area of greater sciatic notch | 1.7 | 4.0 | 1.6 |
Fig. 4.
Stress distribution of the normal pelvis during two-legged stance position (a), single-legged stance position (b), and sitting (c)
The three-dimensional reconstruction model of postoperative pelvis
Stress distribution of the affected hemipelvis was concentrated on the proximal area of the pubic plate, the top of the acetabular cup, the connection between the CS-fixator and acetabular cup and the fixation between the prosthesis and sacroiliac joint (Table 3; Fig. 5).
Table 3.
Maximum stress in different places of postoperative pelvis (MPa)
| Location | Two-legged stance | One-legged stance on affected leg | Sitting |
|---|---|---|---|
| Connection between CS-fixator and acetabular cup | 4.3 | 12.8 | 5.0 |
| Fixation between prosthesis and sacroiliac joint | 2.8 | 3.0 | 3.2 |
| Superior region of the arcuate line | 0.5 | 1.3 | 0.8 |
| Sacroiliac joint of the uninjured side | 1.5 | 1.1 | 1.4 |
| Superior area of greater sciatic notch of the uninjured side | 1.6 | 0.8 | 1.7 |
Fig. 5.
Stress distribution of the postoperative pelvis during two-legged stance position (a), one-legged stance position on the affected leg (b) and sitting (c)
Discussion
There are many methods to reconstruct the hemipelvis after sarcoma resection, but each method has its own limitations, such as high complication rate or poor functional outcome [26]. The modular hemipelvic endoprosthesis has been applied recently with good results [13, 14]. It is difficult to assess the stress and strain distributions throughout the entire pelvis using simplified mathematical models, implanted prostheses, or via experiments with cadaveric tissue [20]. However, FE analysis, which can accommodate large inter-subject variations in bone geometry and material properties, provides an attractive approach to analysing pelvic mechanics.
The present study has inherent limitations. First, the FE model was based on the anatomy of a single patient. Second, the role of muscles or ligaments was not examined because of difficulty assessing the soft tissue changes after excision and reconstruction of the pelvis. Of course, anatomical variations of the pelvis and the extent of the excision may affect the results. We hope to address these limitations in a future study.
When comparing the contralateral side of the postoperative pelvis with the normal pelvis, we found that the stress distribution profiles were similar. Stresses were mostly concentrated along the inside and top of the acetabular cup, similar to the distribution of stresses along the acetabular contact surface of the normal pelvis. This implies the affected side of the postoperative pelvis had little change in stress distribution and approached the physiological condition.
We compared the stress distributions of the affected side of the postoperative pelvis with the contralateral side and the normal pelvis at different positions: standing on two feet, standing on the foot of the affected side, and sitting. While standing on two feet and standing on the affected foot, stress concentration of the normal pelvis was on the superior area of the acetabulum, arcuate line, the greater sciatic notch, sacroiliac joint and the sacral midline. The maximum stress appeared on the inside and top of the acetabulum and the superior area of the greater sciatic notch. Stress concentration of the postoperative pelvis was on the proximal end of the pubic plate, the top of the acetabular cup, the connection between the CS-fixator and acetabular cup and the fixation between the prosthesis and sacroiliac joint. The maximum stress appeared on the top of the acetabular cup and the connection between the CS-fixator and acetabular cup. During sitting, stress concentration of the normal pelvis was on the ischial tuberosity, superior area of the greater sciatic notch, sacroiliac joint and the sacral midline. The maximum stress appeared on the ischial tuberosity. Stress concentration of the postoperative pelvis was on the proximal end of the pubic plate, the top of the acetabular cup, the connection between CS-fixator and acetabular cup and the fixation between the prosthesis and sacroiliac joint. The maximum stress appeared on the sacroiliac joint. All of the above demonstrates that stress distribution on the affected side of the postoperative pelvis was similar to the contralateral side and the normal pelvis. Although the distribution of stresses on the affected side of the postoperative pelvis varied at different positions, the magnitude of stresses was obviously greater than for the contralateral side and the normal pelvis, which may be because of the smaller volume of the modular hemipelvic endoprosthesis.
For all three static positions, the modular hemipelvic endoprosthesis was safe and fatigue was unlikely to occur because the maximum stress was much lower than the implant’s tensile strength and yield strength. However, the stresses incurred during static positions are not the biggest stresses borne by the pelvis [27]. Stress borne by the pelvis is only 81 % of body weight when standing on one foot. However, stress on the pelvis increases to four to seven times body weight when walking steadily, and even ten times body weight when running and jumping [28, 29]. In order to analyse the biomechanics of the modular hemipelvic endoprosthesis more accurately, stresses on the pelvis while walking steadily should be investigated. That is the next study to be addressed.
The proximal end of the pubic plate endured a high stress distribution in all three positions, especially while standing on the affected foot and during sitting (Fig. 6). However, the pubic plate (TA2 titanium) only had a tensile strength of 500 MPa and a yield strength of 405 MPa, much lower than that of TC4 titanium (965 MPa tensile strength, 905 MPa yield strength). That may be a reason for the breakage of the proximal pubic plate reported in two cases by Guo et al. [13]. The pubic fixation may require some improvements.
Fig. 6.
The stress distribution of the implant components during two-legged stance (a), one-legged stance on the affected leg (b), and sitting (c). The red arrows indicate the proximal pubic plate bears high stresses
We conclude that the FE model well analysed the stress distribution of the pelvis reconstructed with modular hemipelvic endoprosthesis in three static positions. The concentration of stress in the pelvis reconstructed with the modular hemipelvic endoprosthesis resembles that of the normal pelvis during static positions.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Bell RS, Davis AM, Wunder JS, Buconjic T, McGoveran B, Gross AE. Allograft reconstruction of the acetabulum after resection of grade II B sarcoma. Intermediate term results. J Bone Joint Surg. 1997;79A:1663–1674. doi: 10.2106/00004623-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Kohler R, Lorge F, Brunat-Mentigny M, Noyer D, Patricot L. Massive bone allografts in children. Int Orthop. 1990;14:249–253. doi: 10.1007/BF00178754. [DOI] [PubMed] [Google Scholar]
- 3.Matejovsky Z, Jr, Matejovsky Z, Kofranek I. Massive allografts in tumour surgery. Int Orthop. 2006;30:478–483. doi: 10.1007/s00264-006-0223-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ozaki T, Hillmann A, Bettin D, Wuisman P, Winkelmann W. High complication rates with pelvic allografts: Experience of 22 sarcoma resections. Acta Orthop Scand. 1996;67:333–338. doi: 10.3109/17453679609002326. [DOI] [PubMed] [Google Scholar]
- 5.Harrington KD. The use of hemipelvis allografts or autoclaved grafts for reconstruction after wide resection of malignant tumors of the pelvis. J Bone Joint Surg. 1992;74:331–341. [PubMed] [Google Scholar]
- 6.Campanacci D, Chacon S, Mondanelli N, Beltrami G, Scoccianti G, Caff G, Frenos F, Capanna R (2012) Pelvic massive allograft reconstruction after bone tumour resection. Int Orthop 36:2529–2536 [DOI] [PMC free article] [PubMed]
- 7.Abudu A, Grimer RJ, Cannon SR, Carter SR, Sneath RS. Reconstruction of the hemipelvis after excision of malignant tumors. J Bone Joint Surg. 1997;79:773–779. doi: 10.1302/0301-620X.79B5.6749. [DOI] [PubMed] [Google Scholar]
- 8.Gradinger R, Rechl H, Hipp E. Pelvic osteosarcoma. Clin Orthop Relat Res. 1991;270:149–157. [PubMed] [Google Scholar]
- 9.Windhager R, Karner J, Kutschera HP, Polterauer P, Salzer-Kuntschik M, Kotz R. Limb salvage in periacetabular sarcomas: review of 21 consecutive cases. Clin Orthop Relat Res. 1996;331:265–276. doi: 10.1097/00003086-199610000-00038. [DOI] [PubMed] [Google Scholar]
- 10.Aboulafia AJ, Buch R, Mathews J, Li W, Malawer MM. Reconstruction using the saddle prosthesis following excision of primary and metastatic periacetabular tumors. Clin Orthop Relat Res. 1995;314:203–213. [PubMed] [Google Scholar]
- 11.Aljassir F, Beadel GP, Turcotte RE, Griffin AM, Bell RS, Wunder JS, Isler MH. Outcome after pelvic sarcoma resection reconstructed with saddle prosthesis. Clin Orthop Relat Res. 2005;438:36–41. doi: 10.1097/00003086-200509000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Benevenia J, Cyran FP, Biermann JS, Patterson FR, Leeson MC. Treatment of advanced metastatic lesions of the acetabulum using the saddle prosthesis. Clin Orthop Relat Res. 2004;426:23–31. doi: 10.1097/01.blo.0000141387.03035.3e. [DOI] [PubMed] [Google Scholar]
- 13.Guo W, Li D, Tang X. Reconstruction with modular hemipelvic prostheses for periacetabular tumor. Clin Orthop Relat Res. 2007;461:180–188. doi: 10.1097/BLO.0b013e31806165d5. [DOI] [PubMed] [Google Scholar]
- 14.Zhou Y, Duan H, Liu Y, Min L, Kong Q, Tu C. Outcome after pelvic sarcoma resection and reconstruction with a modular hemipelvic prostheses. Int Orthop. 2011;35(12):1839–1846. doi: 10.1007/s00264-011-1222-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim JE, Li Z, Ito Y, Huber CD, Shih AM, Eberhardt AW, Yang KH, King AI, Soni BK. Finite element model development of a child pelvis with optimization-based material identification. J Biomech. 2009;42:2191–2195. doi: 10.1016/j.jbiomech.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 16.Kaku N, Tsumura H, Taira H, Sawatari T, Torisu T. Biomechanical study of load transfer of the pubic ramus due to pelvic inclination after hip joint surgery using a three-dimensional finite element model. J Orthop Sci. 2004;9:264–269. doi: 10.1007/s00776-004-0772-9. [DOI] [PubMed] [Google Scholar]
- 17.Levine DL, Dharia MA, Siggelkow E, Crowninshield RD, Degroff DA, Wentz DH. Repair of periprosthetic pelvis defects with porous metal implants: a finite element study. J Biomech Eng. 2010;132:021006. doi: 10.1115/1.4000853. [DOI] [PubMed] [Google Scholar]
- 18.Majumder S, Roychowdhury A, Pal S. Effects of body configuration on pelvic injury in backward fall simulation using 3D finite element models of pelvis-femur-soft tissue complex. J Biomech. 2009;42:1475–1482. doi: 10.1016/j.jbiomech.2009.03.044. [DOI] [PubMed] [Google Scholar]
- 19.Ivanov AA, Kiapour A, Ebraheim NA, Goel V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine. 2009;34:E162–169. doi: 10.1097/BRS.0b013e3181978ea3. [DOI] [PubMed] [Google Scholar]
- 20.Anderson AE, Peters CL, Tuttle BD, Weiss JA. Subject-specific finite element model of the pelvis: development, validation and sensitivity studies. J Biomech Eng. 2005;127:364–373. doi: 10.1115/1.1894148. [DOI] [PubMed] [Google Scholar]
- 21.Dalstra M, Huiskes R. Load transfer across the pelvic bone. J Biomech. 1995;28:715–724. doi: 10.1016/0021-9290(94)00125-N. [DOI] [PubMed] [Google Scholar]
- 22.Li Z, Alonso JE, Kim JE, Davidson JS, Etheridge BS, Eberhardt AW. Three-dimensional finite element models of the human pubic symphysis with viscohyperelastic soft tissues. Ann Biomed Eng. 2006;34:1452–62. doi: 10.1007/s10439-006-9145-1. [DOI] [PubMed] [Google Scholar]
- 23.Davy DT, Connolly JF. The biomechanical behaviour of healing canine radii and ribs. J Biomech. 1982;15:235–247. doi: 10.1016/0021-9290(82)90170-1. [DOI] [PubMed] [Google Scholar]
- 24.Li Z, Kim JE, Davidson JS, Etheridge BS, Alonso JE, Eberhardt AW. Biomechanical response of the pubic symphysis in lateral pelvic impacts: a finite element study. J Biomech. 2007;40:2758–2766. doi: 10.1016/j.jbiomech.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 25.Tanino H, Ito H, Higa M, Omizu N, Nishimura I, Matsuda K, Mitamura Y, Matsuno T. Three-dimensional computer-aided design based design sensitivity analysis and shape optimization of the stem using adaptive p-method. J Biomech. 2006;39:1948–1953. doi: 10.1016/j.jbiomech.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 26.Ozaki T, Hoffmann C, Hillmann A, Gosheger G, Lindner N, Winkelmann W. Implantation of hemipelvic prosthesis after resection of sarcoma. Clin Orthop Relat Res. 2002;396:197–205. doi: 10.1097/00003086-200203000-00030. [DOI] [PubMed] [Google Scholar]
- 27.Pedersen DR, Brand RA, Davy DT. Pelvic muscle and acetabular contact forces during gait. J Biomech. 1997;30:959–965. doi: 10.1016/S0021-9290(97)00041-9. [DOI] [PubMed] [Google Scholar]
- 28.Bergmann G, Graichen F, Rohlmann A. Hip joint loading during walking and running, measured in two patients. J Biomech. 1993;26:969–990. doi: 10.1016/0021-9290(93)90058-M. [DOI] [PubMed] [Google Scholar]
- 29.Bergmann G, Deuretzbacher G, Heller M, Graichen F, Rohlmann A, Strauss J, Duda GN. Hip contact forces and gait patterns from routine activities. J Biomech. 2001;34:859–871. doi: 10.1016/S0021-9290(01)00040-9. [DOI] [PubMed] [Google Scholar]