Abstract
Purpose
Modular acetabular reconstructive cups have been introduced in an attempt to offer initial rigid fixation by iliac lag screws and ischial pegs, to support bone grafts with a flanged metal socket, and to restore original hip center in acetabular revision. The purpose of this study was to clarify minimum ten year follow-up results of this cup system with morsellised allografts in revision cases.
Methods
We retrospectively investigated 54 acetabular revisions at a mean of 11 years (range, ten to 14 years). The indications were Paprosky’s type 2B (eight hip), 2C (eight hips), 3A (23 hips), 3B (nine hips), and 4 (six hips).
Results
Using aseptic loosening as the endpoints, the survival rate was 89.3 % (95 % CI 81–98). Radiographically, one type 3A hip, three type 3B hips and one type 4 hip showed aseptic loosening while no type 2 hips or no cemented cups showed loosening.
Conclusions
The modular reconstructive cups for acetabular revision showed bone stock restoration and stable implantation.
Introduction
Acetabular bone deficiency due to osteolysis, infection, and/or aseptic loosening is a major problem in revision total hip arthroplasty (THA) [1–14]. Favourable long-term results of treatment for cases with Paprosky type 3A, 3B, and pelvic discontinuity is desirable [15]. In order to treat the massive acetabular bone deficiency, bone and bone substitutes including morsellised allografts [1–5, 8, 12, 13], massive allografts [4, 9] and hydroxyapatite granules [6, 7, 10, 11], have been grafted in revision THA. As for morsellised allografts, favourable mid-term or long-term results using cemented polyethylene components have been reported [2, 8].
Although modular acetabular implants have been introduced to overcome various bone deficiency, their results with morsellised allografts for revision cases were not so good, i.e. the survival of 43 % at 15 years in 21 hips [3] and 64.5 % at five years in 62 hips [16]. One of the reasons for poor results is mechanical failure [17] such as screw breakage [3] and hook and side plate breakage [16] of the uncemented non-porous metal-backed prosthesis with augmentation. On the other hand, an improved modular acetabular cup system including porous metal components [18] and components composed of a flanged metal socket, an iliac lag screw, and an ischial peg [7] has been reported; the latter modular acetabular reconstructive cup with hydroxyapatite granules grafting showed the survival of 74.2 % at 11 years with aseptic loosening as the endpoint [7]. There was no implant breakage. Thus, modular acetabular implants, if they had no mechanical failure, showed good mid-term results. The long-term outcome of the modular acetabular implant and morsellised allografts in revision THA has not been well documented. The hypothesis of this study is that modular acetabular implants and morsellised allografts show good long-term survival, bone stock restoration, and stable implantation if they had no mechanical failure.
The purpose of the present study is to clarify retrospectively the clinical and radiographic results of modular reconstructive cups and morsellised allografts at a minimum ten-year follow-up.
Patients and methods
Between July 1998 and January 2003, modular acetabular reconstructive cups and morsellised allografts were used in 58 hips of 52 patients for revision THA. Within five years after the index revision surgery, four patients (four hips) were diseased. Therefore 54 hips of 48 patients were investigated retrospectively. There were 43 women and five men. The mean age of the patients at the time of the acetabular revision surgery was 67 years (range, 49–81 years). The mean height was 149 cm (range, 135–171 cm), and the mean weight was 51.8 kg (range, 35–70 kg). The mean body mass index (BMI) was 23.2 (range, 15.6–32.6). The mean follow-up was 11 years (range, ten to 14 years). The reason for the revision THA was aseptic loosening of THA in 48 hips, aseptic loosening of bipolar endprostheses in five hips, and infection after THA in one hip. The cumulative number of operations prior to the index acetabular revision surgery was one in 33 hips, two in 16 hips, three in three hips, and four in two hips.
The classification system of Paprosky et al. [15] was used in order to evaluate the severity of the acetabular bone deficiency. Eight hips had a type 2B acetabulum (>2 cm superior migration), eight hips had type a 2C (medial wall defect), 23 hips had a type 3A (30–60 % rim defect), nine hips had a type 3B (>60 % rim defect), and six hips had a type 4 (pelvic discontinuity). Thus, the patients in the present study showed moderate to severe bone deficiency.
The modular reconstructive cup (ModuRec system, Zimmer, Warsaw, IN; Fig. 1) was composed of a flanged metal socket, an iliac lag screw, and an ischial peg. This system was intended to acquire ideal hip center and to restore bone stock in revision THA cases with several acetabular bone deficiency. We generally used this system not for primary cases, but for revision cases or some acetabular bone tumour cases with severe bone deficiency. It was made of titanium alloy (Ti-6Al-4 V) and the surface finish of the flanged socket was corundum-blasted. The flanged socket was 48, 52, 54, 56, or 60 mm in the external diameter. An iliac lag screw with a diameter of 20 mm, and an ischial peg were used to acquire the initial stability against rotational force. The iliac lag screw was 50, 55, 60, 65, 70, 75, or 80 mm in length. The ischial peg came in two types. Modular, gamma-sterilized, conventional ultra-high-molecular-weight polyethylene (UHMWPE) inserts were available with an internal diameter of 22, 26, 28 or 32 mm and either with a neutral liner (five hips) or an elevated liner (49 hips).
Fig. 1.
The modular reconstructive cup (ModuRec system, Zimmer, Warsaw, IN). Flanged metal socket with sleeve for an iliac lag screw as well as an iliac lag screw and ischial peg
The surgical technique is as follows: using a posterolateral approach to the hip, the loose components and fibrous tissues were removed to expose the host bone. The iliac lag screw was inserted through the posterior column of the iliac bone beside the sciatic notch; this bony region is usually intact even in severe acetabular deficiency, except pelvic discontinuity cases. For pelvic discontinuity cases, we added a fixation of the posterior column with reconstruction plates. A guide wire was passed into the posterior column of the iliac bone using a jig. An iliac lag screw of appropriate length was inserted beneath the iliosacral joint. Morsellised allografts of 7–10 mm in diameter, which were harvested under sterile conditions and additionally sterilized using Lobator sd-2 (Ai-medic Co, Ltd, Marburg, Germany), were prepared with a milling apparatus. In order to densely pack the entire bone defect area, morsellised allografts were impacted using a trial cup. A space was left for the cup, and impaction with the trial cup was performed to compress the allografts. After morsellised allografts packing, a flanged metal socket was connected with the lag screw through the sleeve and impacted. The modular cup was then located in the original hip centre level as high as possible. An ischial peg was inserted and fixed through the window of the flanged metal socket. The flanged metal socket has eight holes, through which additional bone and/or further morsellised allografts can be grafted into any remaining bone defect of the acetabulum and screws can be fixed. Of the 54 grafts, 31 components were fixed without cement, while 23 components were fixed with cement. We used cement at the interface between the flanged metal socket and morsellised allograft layer in case of small contact area between the flanged metal socket and the host bone.
On the femoral side, 32 hips had no femoral revision at the index acetabular revision THA, while the other 22 hips had femoral revision; 18 hips were revised using cementless stems and four hips were revised using cemented stems. Concerning the femoral head, 32-mm cobalt–chrome modular heads were used in seven hips, 28-mm cobalt-chrome modular heads were used in 16 hips, 28 mm alumina modular heads (Biolox, CeramTec, Plochingen, Germany) were used in 20 hips, 26-mm cobalt-chrome modular heads were used in eight hips, and 22-mm stainless heads were used in three hips.
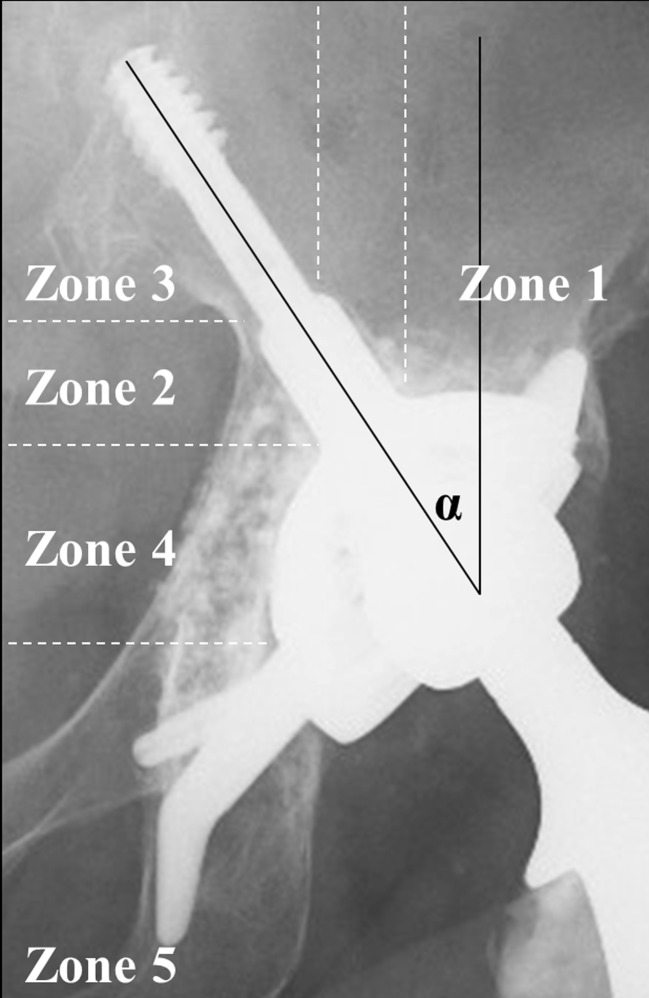
The clinical and radiographic data were evaluated by two independent authors (TS and NS) with no prior knowledge of the results. Kaplan-Meier survival analysis was performed with two end-points: radiologic aseptic loosening and re-operation for any reason including loosening. The 95 % confidence interval (95 % CI) was also calculated. The clinical results were evaluated pre-operatively and at the latest follow-up using the Harris hip score (HHS) [19]. Anteroposterior and oblique radiographs were taken pre-operatively and at each follow-up. On the anteroposterior radiographs taken just after surgery, the location of the hip centre was evaluated as the vertical distance from the teardrop line [20] and the horizontal distance from the vertical line through the ipsilateral teardrop. We measured the angle of the iliac lag screw in order to evaluate the cup positioning (Fig. 2). Because the modular cup had a unique shape, we defined five zones and measured the presence of radiolucent lines in each zone as follows: Zone 1, the weight bearing zone; Zone 2, around the sleeve; Zone 3, around the iliac lag screw; Zone 4, the medial wall; and Zone 5, around the ischial peg (Fig. 2). We also checked the consolidation of morsellised allograft and the interface between the bone and allograft layer on the anteroposterior plain radiographs [6]. Migration of the component, both horizontally and vertically, was measured according to the method of Nunn et al. [21]. Acetabular loosening was established if the sum of acetabular migration in the horizontal and vertical planes was >5 mm [22], if the change in the acetabular component was >5°, or if there was a progressive radiolucent line >1 mm in all zones, as described by DeLee and Charnley [23].
Fig. 2.
Radiological zones and angle of the iliac lag screw. Five zones were defined. Zone 1, the weight bearing zone; Zone 2, around the sleeve; Zone 3, around the iliac lag screw; Zone 4, the medial wall; and Zone 5, around the ischial peg. The iliac lag screw angle was defined as the angle composed of the perpendicular line and the lag screw line
Statistical analysis
With an anticipated effect size of 0.8 and a statistical power of 0.8, we estimated our minimum sample size required was 54 hips, which was consistent with the patients number in the present study. We evaluated post hoc power according to the method by Hoenig and Heisey [24]. Comparison between the radiographically defined loosening hips and hips without loosening was carried out using the Mann–Whitney U test, the chi-square test or Fisher’s exact probability test. All calculations were performed using SPSS software for Microsoft Windows ver 21.0 (IBM, Armonk NY). A p-value <0.05 was considered significant.
Results
Kaplan-Meier survival analysis with radiologic and aseptic loosening as the endpoint showed a 89.3 % probability (95 % CI 81–98). That with re-operations for any reason as the endpoint, including three cases of cup loosening and two femoral fractures without cup loosening, showed an 86.7 % probability (95 % CI 71–98) of retaining the modular cup at a mean of ten years postoperatively. The mean pain HHS improved from 19.6 (range, 0–35) to 36.0 points (range, 10–40), and the mean total HHS improved from 49.2 (range, 26–78) to 78.9 points (range, 41–97) at the latest follow-up. There was no breakage of the flanged cup or iliac lag screw. Although there were no infections, there were three dislocations and three femoral fractures.
Concerning the location of the hip centre, the vertical distance from the inter-teardrop line was 25.2 ± 9.2 mm (range, 7.5–49.8 mm) while the horizontal distance from the ipsilateral teardrop was 33.2 ± 4.9 mm (range, 22.0–46.7 mm). The mean angle of the iliac lag screw was 27.1° (range, 8–40°). A radiolucent line around the modular cup was seen in ten hips for Zone 1, ten hips for Zone 2, 12 hips for Zone 3, ten hips for Zone 4, and four hips for Zone 5. Consolidation of the allograft layer was detected in 45 hips (83 %, Fig. 3). Radiolucent lines between the allograft layer and the host bone were detected in three hips (5.6 %).
Fig. 3.
An anteroposterior radiograph of a 59-year-old woman who had acetabular revision for Paprosky type3A hip. a Before the revision surgery. b Just after the surgery. c Six years postoperatively. d Ten years postoperatively, morsellised allograft layer showed consolidation without loosening
A total of 49 hips showed no aseptic loosening radiographically (Fig. 3) while five hips showed aseptic loosening and progressive migration with collapse of the allograft layer at the weight bearing area. Loosening was detected in four out of 31 hips without cement and one out of 23 hips with cement. In Paprosky’s classification, one out of 23 type 3A hips, three out of nine type 3B hips, and one out of six type 4 hips showed radiologic loosening, while none of 16 type 2 hips showed loosening. Three loosening hips underwent additional revision at 36 months, 82 months, and 96 months postoperatively respectively, using new modular reconstructive cups with a metal plate and/or fibular graft for the rim defect. At the additional revision surgery, all three hips were evaluated as Paprosky type 3B and morsellised allografts did not show binding directly onto the surface of the loosened cup. However, the interface between the host bone and morsellised allografts showed rigid fixation, and morsellised allografts themselves showed partial incorporation. Between the hips that loosened and those that did not, there were significant differences in the horizontal distance of the head center from the vertical line through the ipsilateral teardrop (p = 0.005) and consolidation of morsellised allograft (p = 0.002) (Table 1).
Table 1.
Comparison between non-aseptic loosening hips and loosening hips
| Parameters | Non-aseptic loosening (49 hips) | Aseptic loosening (5 hips) | p value |
|---|---|---|---|
| Age in years (SD) | 67.0 (7.4) | 62.0 (2.6) | 0.08b |
| Gender (men : women, hips) | 4:45 | 1:4 | 0.397c |
| Height in cm (SD) | 149.7 (7.6) | 147.1 (1.9) | 0.491b |
| Weight in kg (SD) | 51.8 (9.1) | 52.0 (8.0) | 0.881b |
| Body mass index | 23.1 (3.6) | 24.0 (3.1) | 0.549b |
| Operation times before the index revision (hips) | |||
| 1/2/3/4 | 30/14/3/2 | 3/2/0/0 | 0.871d |
| Paprosky’s classificationa (hips) | |||
| Type 2B/2C/3A/3B/4 | 8/8/22/6/5 | 0/0/1/3/1 | 0.064d |
| Head center in mm (SD) | |||
| Vertical distance from the teardrop line | 25.3 (9.3) | 25.0 (9.3) | 0.834b |
| Horizontal distance from the vertical line through the ipsilateral teardrop | 32.5 (4.5) | 39.8 (4.1) | 0.005b |
| Angle of the iliac lag screw in degrees (SD) | 26.8 (7.0) | 30.4 (7.6) | 0.288b |
| Consolidation of morsellised allograft (+/−, hips) | 44/5 | 1/4 | 0.002c |
| Cement use (+/−, hips) | 22/27 | 1/4 | 0.38c |
A p value of <0.05 indicates a statistical significant difference
a Type2: superior migration/medial wall defect; Type 3A: 30–60 % rim defect; Type 3B: >60 % rim defect; Type 4: pelvic discontinuity
b Mann Whitney U test
c Fisher’s exact probability test
d Chi-square test
Discussion
The aim of this study was to clarify the clinical and radiographic results of modular reconstructive cups and morsellised allografts at a minimum ten-year follow-up. Our hypothesis was that the system provides adequate bone stock restoration and stable implantation.
We found that the modular reconstructive cups for revision hips, including Paprosky types 2, 3, and 4, showed bone stock restoration and stable implantation. Morsellised allograft with modular reconstructive cups demonstrated comparable clinical and radiographic results, i.e., 89.3 % survival with loosening as the endpoint, to other acetabular revisions at a minimum ten-year follow-up [8]. The longevity of morsellised allograft with a modular cup depends on the bone deficiency of the acetabulum as the previous report [12]. There was no breakage of the iliac lag screw or ischial peg of the modular cup at a minimum ten year follow-up in the present study since the diameter of the screw was larger than another modular acetabular cup system [3, 16].
The position of the hip centre could be maintained using the modular acetabular cups with morselised allografts compared with the position of the hip centre in general primary THA cases [24]. The vertical distance from the inter-teardrop line and the horizontal distance from the ipsilateral teardrop was 25.2 ± 9.2 mm and 33.2 ± 4.9 mm in the present study, and 23.3 ± 5.9 mm and 29.7 ± 5.9 mm in general primary THA cases, respectively [25]. However, hips with longer horizontal distance (mean 39.8 ± 4.1 mm) significantly showed aseptic loosening (Table 1).
The size of the morsellised allograft or the shape of the allograft including the block may influence the longevity of the allograft layer and the acetabular components. Morsellised allograft with 7–10 mm in diameter were used in the present study and the same size morsellised allograft have shown survival of 75 % at 20 years in 58 hips with the endpoint as revision for any reason using cemented cup [8]. Block or larger morsellised allograft may be more useful bone defect fillers. In the use of allograft, Kawanabe et al. [4] have reported that a monoblock had better results than a morsellised graft. Okano et al. [5] have also claimed that a structural allograft should be considered in the weight-bearing area of the support ring in addition to the morsellised bone graft.
Morsellised allograft did not show binding directly onto the corundum-blasted surface of the loosened modular cup components when re-operation was performed. Acetabular biopsy specimens have also shown that fibrous tissues existed at the interface between the implants and the morsellised bone graft [26]. Although there were no significant differences in radiologic loosening between hips with and without cement in the present study, aseptic loosening was detected in four out of 31 hips without cement and in one out of 23 hips with cement. Cemented revision with morsellised allograft may be better in order to bind morsellised allografts onto the cup surface [8, 27].
There were some limitations to the present study. First, it was a small number of hips with minimum follow-up of ten years, as in many other acetabular revision studies [3, 8]. However, power analysis confirmed that number of hips fulfilled the minimum sample size, and this modular reconstructive cup showed a good longevity over ten years. Second, the Asian patients were very light in terms of weight (mean 51.8 kg, range 35–70 kg) and may not translate to a typical Western population. Although the mean BMI was 23.2 and maximum BMI was 32.6, further study of this modular cup for heavy patients is needed.
In conclusion, the modular reconstructive cup and morsellised allograft for acetabular revision, including Paprosky types 2, 3, and 4, showed bone stock restoration and stable implantation at a minimum ten-year follow-up. For pelvic discontinuity (Paprosky type 4) cases, we added reconstruction acetabular rim by fixation of the posterior column with reconstruction plates.
Acknowledgments
We thank Prof Hideki Yoshikawa for technical support.
Conflict of interest
No competing interests declared. Each author certifies that he or she, or a member of their immediate family, has no commercial associations that might pose a conflict of interest in connection with the submitted article.
References
- 1.Comba F, Buttaro M, Pusso R, Piccaluga F. Acetabular reconstruction with impacted bone allografts and cemented acetabular components. A 2- to 13-year follow-up study of 142 aseptic revisions. J Bone Joint Surg Br. 2006;88:865–869. doi: 10.1302/0301-620X.88B7.17227. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Cimbrelo E, Cruz-Pardos A, Garcia-Rey E, Ortega-Chamarro J. The survival and fate of acetabular reconstruction with impaction grafting for large defects. Clin Orthop Relat Res. 2010;468:3304–3313. doi: 10.1007/s11999-010-1395-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeffery M, Scott G, Freeman M. Failure of an uncemented non-porous metal-backed prosthesis with augmentation using impacted allograft for acetabular revision. 12- to 17-year results. J Bone Joint Surg Br. 2003;85:182–186. doi: 10.1302/0301-620X.85B2.13249. [DOI] [PubMed] [Google Scholar]
- 4.Kawanabe K, Akiyama H, Onishi E, Nakamura T. Revision total hip replacement using the Kerboull acetabular reinforcement device with morsellised or bulk graft. J Bone Joint Surg Br. 2007;89:26–31. doi: 10.1302/0301-620X.89B1.18037. [DOI] [PubMed] [Google Scholar]
- 5.Okano K, Miyata N, Enomoto H, Osaki M, Shindo H. Revision with impacted bone allografts and the Kerboull cross plate for massive bone defect of the acetabulum. J Arthroplasty. 2010;25:594–599. doi: 10.1016/j.arth.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Oonishi H, Iwaki Y, Kin N, Kushitani S, Murata N, Wakitani S, Imoto K. Hydroxyapatite in revision of total hip replacements with massive acetabular defects. J Bone Joint Surg Br. 1997;79:87–92. doi: 10.1302/0301-620X.79B1.1290. [DOI] [PubMed] [Google Scholar]
- 7.Sakai T, Ohzono K, Nishii T, Miki H, Takao M, Sugano N. Grafting with hydroxyapatite grannules for defects of acetabular bone at revision total hip replacement. A minimum ten-year follow-up. J Bone Joint Surg Br. 2010;92:1215–1221. doi: 10.1302/0301-620X.92B9.24555. [DOI] [PubMed] [Google Scholar]
- 8.Schreurs BW, Keurentjes JC, Gardeniers JWM, Verdonschot N, Slooff TJJH, Veth RPH. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented acetabular component. A 20-to 25-year follow-up. J Bone Joint Surg Br. 2009;91:1148–1153. doi: 10.2106/JBJS.G.01701. [DOI] [PubMed] [Google Scholar]
- 9.Sporer SM, O’Rourke M, Chong P, Paprosky WG. The use of structural distal femoral allografts for acetabular reconstruction. Average 10-year follow-up. J Bone Joint Surg Am. 2005;87:760–765. doi: 10.2106/JBJS.D.02099. [DOI] [PubMed] [Google Scholar]
- 10.Sudo A, Hasegawa M, Fukuda A, Kawamura G, Muraki M, Uchida A. Acetabular reconstruction using a cementless cup and hydroxyapatite granules. J Arthroplasty. 2007;22:828–832. doi: 10.1016/j.arth.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka C, Shikata J, Ikenaga M, Takahashi M. Acetabular reconstruction using a Kerboull-type acetabular reinforcement device and hydroxyapatite granules. A 3- to 8- year follow-up study. J Arthroplasty. 2003;18:719–725. doi: 10.1016/S0883-5403(03)00149-9. [DOI] [PubMed] [Google Scholar]
- 12.van Haaren EH, Heyligers IC, Alexander FGM, Wuisman PIJM. High rate of failure of impaction grafting in large acetabular defects. J Bone Joint Surg Br. 2007;89:296–300. doi: 10.1302/0301-620X.89B3.18080. [DOI] [PubMed] [Google Scholar]
- 13.Wang JW, Fong CY, Su YS, Yu HN. Acetabular revision with morsellised allogenic bone graft and a cemented metal-backed component. J Bone Joint Surg Br. 2006;88:586–591. doi: 10.1302/0301-620X.88B5.17275. [DOI] [PubMed] [Google Scholar]
- 14.Sadoghi P, Schröder C, Fottner A, Steinbrück A, Betz O, Müller PE, Jansson V, Hölzer A. Application and survival curve of total hip arthroplasties: a systematic comparative analysis using worldwide hip arthroplasty registers. Int Orthop. 2012;36:2197–2203. doi: 10.1007/s00264-012-1614-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty: a six year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 16.Babis GC, Sakellariou VI, Chatziantoniou AN, Soucacos PN, Megas P. High complication rate in reconstruction of Paprosky type IIIa acetabular defects using an oblong implant with modular side plates and a hook. J Bone Joint Surg Br. 2011;93:1592–1596. doi: 10.1302/0301-620X.93B12.27299. [DOI] [PubMed] [Google Scholar]
- 17.Friesenbichler J, Schwarzkopf R, Sadoghi P, Marwin SE, Glehr M, Maurer-Ertl W, Leithner A. Failure rate of a rotating hinge knee design due to yoke fracture of the hinged tibial insert: a retrospective data analysis and review of the literature. Int Orthop. 2012;36:993–998. doi: 10.1007/s00264-011-1462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lingaraj K, Teo YH, Bergman N. The management of severe acetabular bone defects in revision hip arthroplasty using modular porous metal components. J Bone Joint Surg Br. 2009;91:1555–1560. doi: 10.1302/0301-620X.91B12.22517. [DOI] [PubMed] [Google Scholar]
- 19.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 20.Asayama I, Chamnongkich S, Simpson KJ, Kinsey TL, Mahoney OM. Reconstructed hip joints position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005;20:414–420. doi: 10.1016/j.arth.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 21.Nunn D, Freeman MAR, Hill PF, Evans SJW. The measurement of migration of the acetabular component of hip prostheses. J Bone Joint Surg Br. 1989;71:629–631. doi: 10.1302/0301-620X.71B4.2768311. [DOI] [PubMed] [Google Scholar]
- 22.Ochs BG, Schmid U, Rieth J, Ateschrang A, Weise K, Ochs U. Acetabular bone reconstruction in revision arthroplasty. A comparison of freeze-dried, irradiated and chemically-treated allograft vitalized with autologous marrow versus frozen non-irradiated allograft. J Bone Joint Surg Br. 2008;90:1164–1171. doi: 10.1302/0301-620X.90B9.20425. [DOI] [PubMed] [Google Scholar]
- 23.DeLee JG, Charnley J. Radiographic demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 24.Hoenig JM, Heisey DM. The abuse of power: the pervasive fallacy of power calculations for data analysis. Am Stat. 2001;55:19–24. doi: 10.1198/000313001300339897. [DOI] [Google Scholar]
- 25.Takao M, Nakamura N, Ohzono K, Sakai T, Nishii T, Sugano N. The results of a press-fit-only technique for acetabular fixation in hip dysplasia. J Arthroplasty. 2011;26:562–568. doi: 10.1016/j.arth.2010.05.025. [DOI] [PubMed] [Google Scholar]
- 26.van der Donk S, Buma P, Slooff TJJH, Gardeniers JWM, Schreurs BW. Incorporation of morsellised bone grafts: a study of 24 acetabular biopsy specimens. Clin Orthop Relat Res. 2002;396:131–141. doi: 10.1097/00003086-200203000-00022. [DOI] [PubMed] [Google Scholar]
- 27.Winter E, Piert M, Volkmann R, Maurer F, Eingartner C, Weise K, Weller S. Allogeneic cancellous bone graft and a Burch-Schneider ring for acetabular reconstruction in revision hip arthroplasty. J Bone Joint Surg Am. 2001;83:862–867. doi: 10.2106/00004623-200106000-00007. [DOI] [PubMed] [Google Scholar]