Abstract
Purpose
Dislocations of components, loosening of the stem, overstuffing and removal in up to 24 % of common radial head prostheses (RHP) after implantation in complex elbow injuries signal the need for improvement. The latest biomechanical evidence shows advantages for monopolar designs. Clinical results after primary and secondary implantation of the newly designed press-fit monobloc monopolar RHP in cases of complex elbow injury are evaluated.
Methods
Twenty-nine patients [median age 60 years (29–86)] were followed up retrospectively for a median of 25 months (7–54) post-operatively. Subjective parameters, the Mayo Elbow Performance Score (MEPS), the Broberg and Morrey score (BMS), latest radiographs and complications were evaluated.
Results
MEPS and BMS averaged 87.2 ± 12.9 and 81.1 ± 11.9 points, respectively. No case of implant loosening was observed; the RHP had to be removed in one case (3 %). The overall complication and revision rate was higher after secondary (53 %) than after primary (19 %) implantation.
Conclusions
Satisfactory clinical results and low short-term removal rates emphasise the practicality of monobloc monopolar RHP. Differentiated treatment of complex elbow fracture-dislocations is compulsory to avoid the need for secondary RHP implantation which carries a higher complication rate.
Introduction
Although it is a secondary stabiliser of the elbow, the radial head has a critical role when structural integrity of ligaments and the coronoid process are compromised [22]. Next to the medial collateral ligament the radial head is a major constraint to valgus loading; in the case of medial ligament disruption the radial head accounts for 60 % of valgus stability [7, 15]. Together with the coronoid process the radial head is an important posterolateral stabiliser of the elbow and furthermore plays a role in axial and varus stability [7, 20]. Comminuted radial head fractures are complex elbow injuries. Of Mason type III radial head fractures, 75 % are associated with further ligamentous and osseous damage [7, 12, 23] (Fig. 1). Unfortunately, associated injuries are often missed as they may not be visible on routine imaging or are not obvious on examination leading to subluxation or recurrent dislocation [7].
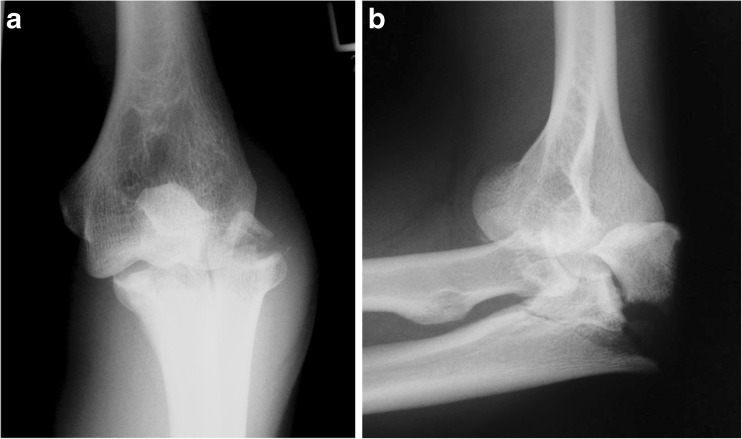
Fig. 1.
A 46-year-old man, left elbow; complex elbow fracture-dislocation, Monteggia-like lesion Bado type II with radial head fracture Mason type III and coronoid fracture Regan and Morrey type III (a anteroposterior view, b lateral view)
Treatment goals for radial head fractures are to restore elbow stability and forearm rotation, to preserve elbow motion and to maintain the length of the radius [25]. Common treatment options of Mason type III fractures are osteosynthesis, radial head resection and prosthetic replacement. Radial head resection leads to predominantly good results in stable elbows without further concomitant lesions [1]. An incorrect indication for resection will lead to persistent valgus, longitudinal forearm instability and other secondary symptoms [1, 12, 13, 25].
Restoring osseous, articular components converts a complex fracture-dislocation into a simple dislocation [22]. The radial head prosthesis (RHP) seems preferable to osteosynthesis in Mason type III fracture with more than three fragments [17]. Primary prosthetic radial head replacement is indicated in non-reconstructable three- or more fragment radial head fractures with valgus instability and further concomitant injuries. Remaining instability and pain after primary radial head resection and post-traumatic arthrosis, deformation and non-union may require secondary implantation. Modular monopolar and cemented bipolar metal RHP are the most frequently implanted types [7, 10]. Despite predominantly good clinical results, dislocation of components, implant loosening, overstuffing and radiocapitellar arthritis regularly lead to removal and revision. Recent biomechanical testing showed a higher instability in the bipolar design compared to the monopolar design and the uninjured radial head, especially in cases of severe soft tissue damage [6, 14].
Few clinical results of modern press-fit metal RHP are described in the literature [10]. The purpose of this study was to evaluate the results after primary and secondary implantation of a newly designed monobloc monopolar type of RHP with a partially grit-blasted, roughened surface conical stem in complex elbow injuries. We postulated that good clinical results and a low removal rate can be achieved with a monopolar press-fit implant design.
Patients and methods
All patients with implantation of RHP type Corin® (Corin Group PLC, Cirencester, UK) after complex elbow injuries were identified in the hospital information system and reviewed retrospectively after approval of the local Institutional Review Board.
The Corin® (Corin Group PLC, Cirencester, UK) RHP is a monobloc all-metal prosthesis (cobalt-chrome-molybdenum) with a conical stem which allows press-fit implantation in the proximal radius. The proximal part of the stem has a hydroxyapatite-on-titanium porous coating to improve ingrowth.
Between 2007 and 2011 31 Corin® (Corin Group PLC, Cirencester, UK) RHP were implanted in 31 consecutive patients (23 female, eight male) in the authors’ institution in cases of complex elbow injury. The mean patient age at the time of radial head implantation was 59 years (28–85).
Sixteen primary prostheses were implanted in cases of non-reconstructable radial head fractures in elbows with valgus and/or posterolateral instability. All patients with primary implantation of the RHP had ligamentous/osseous concomitant injuries (Table 1); medial collateral disruption was observed (n = 15) and treated conservatively in all patients (Table 1).
Table 1.
Patients with primary radial head replacement: concomitant lesions, injury patterns and treatment besides RHP
| Pat. no. | Gender: M = male, F = female | Age (years) | Affected side: L = left, R = right | Radial head fracture (Mason) | Coronoid process fracture (Reagan & Morrey) | Monteggia-like lesion (Bado) | Lateral ulnar collateral ligament | Elbow dislocation | Primary surgery besides radial head replacement |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 44 | L | III | II | – | – | Yes | Refixation of the anterior capsule with 1 anchor after resection of the coronoid fragment |
| 2 | M | 48 | R | III | I | – | – | Yes | – |
| 3 | F | 53 | R | III | I | – | – | Yes | Refixation of the anterior capsule with 1 anchor after resection of the coronoid fragment |
| 4 | F | 75 | R | III | – | – | – | No | – |
| 6 | F | 75 | L | Radial neck | – | II | – | Yes | Locking plate osteosynthesis of proximal ulnar fracture |
| 8 | F | 70 | R | III | I | – | Disrupted | Yes | Refixation of the anterior capsule with 1 anchor after resection of the coronoid fragment, refixation of the lateral ligament complex with 2 anchors |
| 9 | F | 85 | L | III | I | – | Disrupted | Yes | Refixation of the anterior capsule with 1 anchor after resection of the coronoid fragment, refixation of the lateral ligament complex with 2 anchors |
| 11 | F | 69 | R | III | II | II | – | Yes | Refixation of the coronoid fragment and the anterior capsule with 1 screw and suture, locking plate osteosynthesis of proximal ulnar fracture |
| 12 | F | 52 | L | III | – | – | – | Yes | Refixation of the anterior capsule with 1 anchor |
| 19 | M | 40 | L | III | II | – | Disrupted | Yes | Refixation of the coronoid fragment, anterior capsule & lateral ligament complex with 1 anchor each |
| 20 | F | 78 | L | III | II | – | – | Yes | Refixation of the anterior capsule and coronoid fragment with 1 anchor |
| 22 | F | 83 | L | III | – | – | – | Yes | – |
| 23 | F | 71 | L | III | I | – | Disrupted | Yes | Resection of the coronoid fragment, refixation of the lateral ligament complex with 1 anchor |
| 25 | F | 28 | L | III | I | – | Disrupted | Yes | Refixation of the anterior capsule with 1 anchor & refixation of the lateral ligament complex with 2 anchors |
| 26 | F | 70 | L | III | – | II | – | Yes | Locking plate osteosynthesis of proximal ulnar fracture |
| 30a | F | 72 | L | III | – | – | Disrupted | Yes | Refixation of the lateral ligament complex with 1 anchor |
| Total | 3 M, 13 F | 63 ± 17.8 | 5 R, 11 L | 15× III, 1× radial neck | 6× I, 4× II (63 %) | 3× II (19 %) | n = 6 (38 %) disrupted | n = 14 (94 %) dislocated |
aNot followed up
Secondary implantation of the RHP was performed in 15 patients following failed primary surgery with persistent instability, osteonecrosis, pseudarthrosis or after primary conservative treatment (Table 2); 13 of those patients were referred to our institution from other trauma units.
Table 2.
Patients with secondary RHP: primary injury patterns and treatment, indication for secondary radial head replacement and secondary surgery besides RHP
| Pat. no. | Gender: M = male, F = female | Age (years) | Affected side: R = right, L = left | Primary elbow injury | Primary surgery | Indication for secondary radial head replacement | Secondary surgery besides RHP |
|---|---|---|---|---|---|---|---|
| 5 | F | 66 | L | Secondary dislocated radial neck fracture | Elastic intramedullary nailing | Necrosis, pseudarthrosis, subluxation | Removal of the nail |
| 7 | F | 73 | R | Chronic posterior fixed elbow dislocation with radial neck fracture | Radial head resection + refixation of the coronoid fragment + anterior capsule | Chronic posterior fixed elbow dislocation due to persistent instability | Open arthrolysis, reposition, refixation of lateral ligaments, hinged external fixator |
| 10 | F | 48 | L | Elbow dislocation + Mason III + ligamentous instability | Open reposition, resection of radial head, transfixation with K-wire | Persistent valgus instability after removal of K-wire | Reconstruction of lateral ligament complex with 1 anchor |
| 13 | M | 60 | R | Elbow dislocation with Mason III fracture + coronoid fracture type II | None | Post-traumatic elbow stiffness, dislocated bone healing | Open arthrolysis, neurolysis of n. ulnaris, refixation of radial capsule |
| 14 | F | 33 | L | Mason III fracture | K-wire stabilisation | Radial head necrosis + elbow stiffness | Open arthrolysis |
| 15 | M | 46 | L | Monteggia-like lesion Bado type II + Mason III fracture | Plate osteosynthesis of ulna, hinged external fixator | Persistent dorsolateral instability | Removal of fixator, refixation of coronoid fragment with 1 screw, refixation of anterior capsule + lateral ligament complex with 1 anchor each |
| 16 | F | 60 | R | Elbow dislocation with Mason III fracture | Initially 3 weeks cast, after recurrent dislocation refixation of anterior capsule + hinged external fixator | Third dislocation after removal of hinged external fixator | Refixation of anterior capsule + lateral ligament complex |
| 17 | M | 45 | L | Monteggia-like lesion Bado type II + Mason III fracture | Open reposition, plate osteosynthesis of ulna, resection of radial head | Persistent valgus instability | – |
| 18 | F | 58 | R | Mason III fracture + Essex-Lopresti | None | Persistent pain, longitudinal instability and restricted range of motion | – |
| 21 | F | 53 | R | Mason III fracture | Screw osteosynthesis | Radial head deformity + persistent pain and restricted range of motion | Arthrolysis |
| 24 | M | 49 | L | Monteggia-like lesion Baso type II + Mason III fracture | Plate osteosynthesis of ulna, radial head resection, refixation of anterior capsule with 1 anchor | Persistent pain, valgus instability and restricted range of motion | Removal of a loose anchor, refixation of lateral ligament complex |
| 27 | F | 67 | L | Elbow dislocation + Mason III fracture | Open reposition, radial head resection, medial and lateral ligament reconstruction | Recurrent dislocation | Open reposition, neurolysis of n. ulnaris, refixation of the lateral ligament complex + hinged external fixator |
| 28 | M | 55 | R | Essex-Lopresti with distal radial fracture + dissociation of distal radioulnar joint + Mason III fracture | K-wire transfixation of distal radial fracture + external fixator on wrist | Secondary surgical treatment | Removal of K-wires, plate osteosynthesis of distal radius |
| 29 | F | 62 | R | Elbow dislocation with Mason III fracture | Screw osteosynthesis + reconstruction of the lateral and medial ligament complex | Restricted range of motion, radial head deformity, subluxation | Arthrolysis |
| 31a | F | 55 | L | Elbow dislocation + Mason III fracture | Screw osteosynthesis + reconstruction of lateral ligaments + anterior capsule | Recurrent dislocation | Refixation of lateral ligament complex and anterior capsule + hinged external fixator |
| Total | 5 M, 10 F | 55 ± 10.5 | 7 R, 8 L |
aNot followed up
At the time of follow-up clinical function including range of motion, pain and subjective results, neurological status, scars together with the Mayo Elbow Performance Score (MEPS) and Broberg and Morrey score (BMS) were assessed. Further treatment after radial head replacement, complications and revisions were assessed. The latest available radiographs were evaluated to determine possible overstuffing, implant loosening, ossifications (Ilahi classification [11]) and elbow osteoarthritis (Broberg and Morrey classification [2]) (Fig. 2).
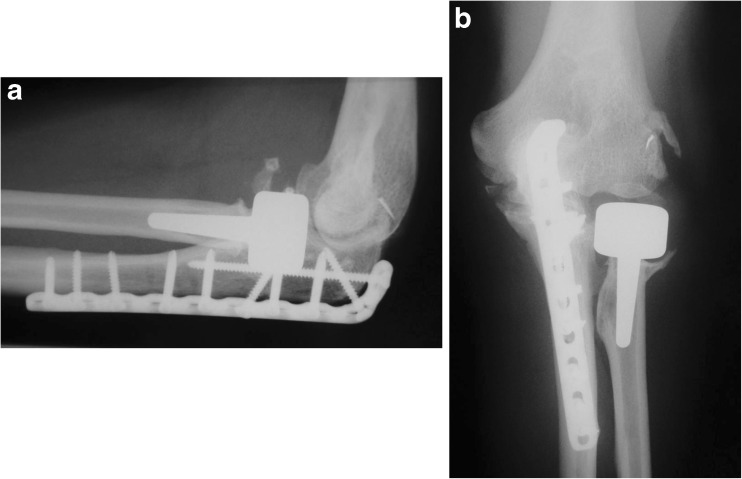
Fig. 2.
A 49 year-old man, left elbow; radiographic result 3 years after plate osteosynthesis of the ulna, screw refixation of the coronoid process and radial head replacement (a anteroposterior view, b lateral view). No bone resorption, implant loosening or radial head overstuffing. Type I ossifications, type I humeroulnar osteoarthritis
Twenty-nine patients (94 %; 21 female, eight male) were followed up at a median of 25 months (7–54). The median age at the time of follow-up was 60 years (29–86). Two patients were lost to follow-up; one of them was the only patient requiring explantation of the prosthesis in the post-operative course (patient 31, Table 2).
Statistical analysis
All statistical analyses were performed using SPSS Statistics Students version 18.0® (SPSS Inc.®, Chicago, IL, USA). Differences in clinical results were compared using the Mann–Whitney U and Wilcoxon matched-pair tests. In all cases, a p value of 0.05 was assumed to denote statistical significance.
Results
Entire cohort
At the time of follow-up the mean extension deficit of the injured side was 14.7 ± 13.4° and the mean flexion range of the affected side was 123.6 ± 26.6°. The mean extension/flexion arc of the injured elbow (108.9 ± 17.4°) was significantly (p < 0.001) restricted compared to the unaffected contralateral side (139.3 ± 5.8°). The mean forearm pronation of the affected arm was 76.3 ± 19.0° and supination was 74.3 ± 20.7°. The arc of forearm rotation of the affected side (150.3 ± 34.8°) was significantly (p < 0.001) lower than on the contralateral side (177.4 ± 5.8°).
The MEPS averaged 87.2 ± 12.9 points, which corresponded to an overall good result (Fig. 3). The MEPS outcomes were excellent in 13, good in 13, fair in two and poor in one. The BMS averaged 81.1 ± 11.9 points, which also corresponded to an overall good result. The BMS outcomes were excellent in three, good in 12, fair in 12 and poor in one. No clinically relevant elbow instabilities were observed.
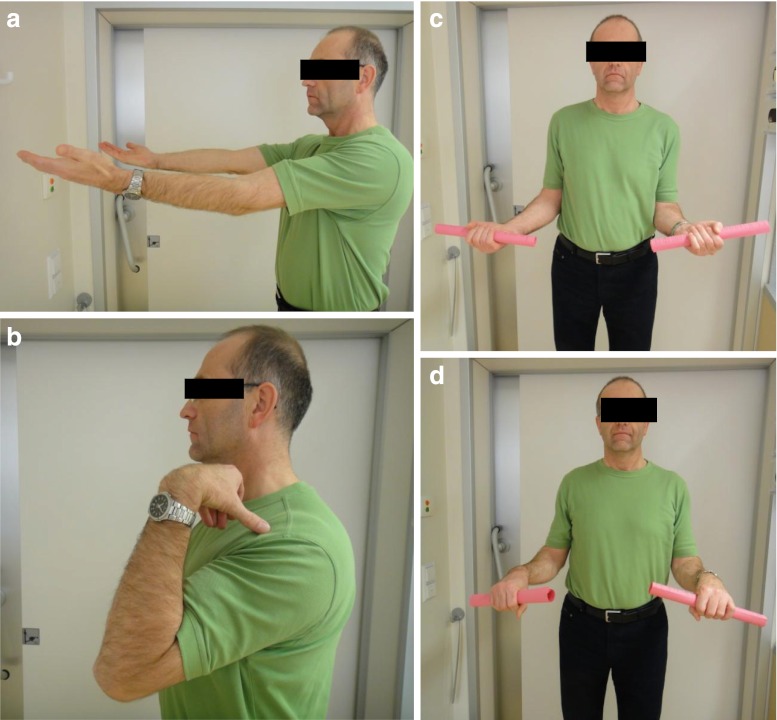
Fig. 3.
A 49-year-old man left elbow; clinical result 3 years after plate osteosynthesis of the ulna, screw refixation of the coronoid process and radial head replacement (a extension, b flexion, c supination, d pronation)
There were 11/29 (35 %) complications. In 5/29 (16 %) cases revision surgery with ulnar implant removal and open arthrolysis was necessary due to discomfort (n = 3) or persistent elbow stiffness (n = 2). In one case (3 %) a screw had to be shortened due to an intra-articular screw penetration (patient 11). The RHP was removed in one patient (3 %, patient 31) due to overstuffing and elbow stiffness. One patient (patient 5) developed a complex regional pain syndrome (CRPS) of the wrist and forearm, and another patient (patient 13) had a superficial wound infection; both complications were treated conservatively. Three patients (10 %) had slight persistent sensory deficits of the ulnar nerve.
All patients but one (97 %) were satisfied with the post-operative result. Five of six patients needing revision surgery after radial head replacement experienced subjectively improved elbow function. Ten patients reported slight pain under heavy load of the affected elbow.
Post-operative radiographs were available in 27/29 (93 %) patients with a mean interval of 7.2 ± 9.9 months post-operatively. Five patients (19 %) showed an osteoarthritis of the affected elbow (4× grade 1, 1× grade 2 [2]). Although all patients received prophylaxis with indomethacin or ibuprofen for six weeks slight ossifications around the elbow were observed in 10/29 (37 %) patients. In five patients these ossifications were located in the medial and lateral capsule at the origin of the collateral ligaments and were probably caused by bony avulsion of the ligaments at the time of injury. The remaining ossifications (n = 5) were located in the ventral aspect of the elbow and could be classified as grade 1 [11]. There was no implant loosening, no bone resorption and no evident radiocapitellar overstuffing [9].
Primary versus secondary RHP
Results after primary and secondary RHP were compared as both groups differed completely regarding conditions under which the prosthesis was implanted. In the primary group the injury pattern was identified and the osseous columns were restored. The secondary group consisted of elbows with instability after the previous surgery or conservative treatment with subluxation and post-traumatic lesions.
Regarding the flexion arc of the affected arm there was no significant (p > 0.05) difference between patients with primary (113.3 ± 22.7°) or secondary (104.3 ± 21.1°) RHP. The forearm rotation arc also showed no significant (p > 0.05) difference between patients with primary (141.3 ± 44.2°) or secondary (160 ± 17.5°) radial head replacement.
In the group of primary RHP the MEPS averaged 90.7 ± 11.5 points, which corresponded to an excellent overall result. After secondary RHP the overall result was good. The MEPS averaged 83.6 ± 13.8 points. No significance (p > 0.05) but a tendency in favour of primary RHP was observed. Also the BMS tended to be in favour of the primary group (84.5 ± 12.9) compared to the secondary group (77.1 ± 9.7) without significance (p > 0.05).
After primary RHP two patients needed ulnar implant removal for discomfort. Another one required screw shortening in the post-operative course. The other named complications and revisions occurred in the group of secondary implantation (n = 8, 53 %).
Discussion
The necessity for radial head replacement in selected cases is unquestioned. Nevertheless, reconstruction of radial head fractures should be the primary goal, which can be impossible when there is severe comminution. The first type of RHP that became established for regular clinical use with good long-term results was a modular monopolar metal prosthesis [10]. However, the “loose stem” design of the shaft was suspected of provoking surrounding osteolysis and bone resorption with subsequent capitellar arthritis. Later bipolar prostheses were designed to articulate with the capitulum humeri in a more anatomical fashion [7]. Short- and midterm results of bipolar prostheses show predominantly good results [3, 4, 19, 25]. Dislocation of components and subluxation of the prosthetic head in up to 12 % must be considered as possible disadvantages as must the fact that most prostheses with a bipolar design are cemented in the radial shaft [3, 4, 13, 24]. The alleged disadvantages of monopolar metallic prostheses led to some further developments such as variations in stem design and surface coating to improve ingrowth [5, 21].
At an average of two years follow-up 90 % of the patients in our study had excellent and good results in the MEPS (overall 87.2 ± 12.9 points). Our results are comparable to those after implantation of other modern types of prostheses [8, 18, 25]. In 30 patients with implantation of a newly designed bipolar RHP with a mean follow-up of 34 months the MEPS averaged 92.1 points [25]. As in our study clinical function was significantly reduced compared to the uninjured contralateral side. Results were significantly better in cases of implantation in the acute trauma situation (n = 23) than in chronic cases (n = 7) [25]. Results also tended to favour primary implantation in our study.
In the secondary setting cases might be regarded as being chronic as problems remain after previous surgical or conservative treatment. If the radial column is not restored and in cases of unstable radial head fractures, persistent instability, subluxation of the elbow and post-traumatic lesions arise, leading the affected elbow to develop a severe condition which is difficult to treat. The differences in results between primary and secondary RHP are not caused at the time of implantation but rather by the condition the elbow at the time of surgery.
Currently, the longest follow-up results exist for metallic monopolar RHP [10]. After a mean of 12.1 years the MEPS averaged 88 points in 20 patients [10]. Prostheses had to be removed in four cases. However, implant removal did not correlate with the patient’s elbow score at later follow-up [10]. Of 20 patients, nine (45 %) showed degenerative changes at the humeroulnar joint; no arthritis could be observed at the humeral capitellum [10]. Disruptions of medial collateral ligaments were treated surgically [10]. In our series there were no persistent instabilities at the time of follow-up, although all medial collateral disruptions (n = 14) in patients with primary RHP were managed non-operatively. The rate of osteoarthritis was comparably low (19 %), probably due to the short follow-up period of the post-operative radiographs. Periarticular ossifications around the elbow joint remain an issue as one third of our patients (n = 10) developed slight ossifications (grade 1).
Midterm results (follow-up nine years) of 17 patients with implantation of bipolar RHP showed excellent and good results in 95 % [3]. Dislocation of components requiring revision was observed in two patients (12 %). The overall arthritis rate was higher compared to long-term results after monopolar prostheses as 47 % showed arthritic changes of the humeral capitellum and 70 % at the humeroulnar joint [3].
Recently, results of 31 patients with press-fit implantation of metallic RHP showed good clinical results with an average of 86 points in MEPS at a mean follow-up of 53 months [8]. The prosthesis had to be removed in nine cases (24 %) due to loosening and associated pain [8]. Proximal forearm pain after cementless press-fit prostheses has been discussed as a strong indicator for symptomatic loosening [16]. Other results demonstrated that radiographic loosening around loose stem monobloc prostheses did not correlate with poorer clinical results [13]. BMS includes strength and pain under strain as outcome measures. The fact that ten patients in our series described pain under heavy loading fits the poorer results in the BMS. All patients with discomfort under heavy loading showed no clinical (as described by O’Driscoll and Herald [16]) or radiographic signs of implant loosening at the time of follow-up. The removal rate in our study was low (n = 1, 3 %); longer follow-up must be awaited to achieve better comparability to other studies. A possible reason for the high removal rate in the study of Flinkkilä et al. might be that bone was rasped until cortical contact could be achieved leaving no cancellous bone for better ingrowth [8].
An evaluation of failure of RHP showed a significant correlation between time of implantation and removal. The later the prosthesis was implanted after the injury, the higher was the likelihood of removal [24]. The only prosthesis removed in our study had been implanted in a secondary setting. Of 15 patients with secondary implantation in our study, 11 (73 %) had persistent instability and recurrent dislocations after primary treatment due to overlooked concomitant lesions; 87 % were referred to us from other trauma units. Furthermore, the overall complication rate after secondary implantation was high (53 %). Knowledge of these facts alongside better results after primary implantation has to lead to a stringent pre- and post-operative evaluation of the elbow and the correct diagnosis of concomitant lesions.
The monobloc monopolar prosthesis is easy to implant and remove compared to cemented bipolar designs. The simple surgical technique allows a broad application in the acute trauma situation. Furthermore, the prosthesis can act as a spacer until the elbow has become stable through soft tissue healing.
Limitations of our study included the retrospective study design and the small cohort size, which was however comparable to other recent studies [8, 18, 25]. Radiological results have a short-term follow-up. Further evaluation will be necessary to confirm low removal rates and an ingrowth without loosening.
Conclusion
First results after implantation of the Corin® RHP in complex elbow injuries with comminuted radial head fractures are good with low short-term removal rates. No observed instabilities indicate that the medial collateral ligament need not be reconstructed in the acute trauma situation when the radial column is restored. Regarding results in the literature, different types of RHP seem to lead to similar short-term results with different pros and cons and without clear recommendation of a specific prosthetic type. Monobloc metallic prostheses allow an easy implantation and removal when needed as a temporary spacer. Correct diagnosis and treatment of concomitant ligamentous and osseous injuries are essential for successful primary treatment. Secondary implantations are accompanied by a higher complication rate and a poorer clinical outcome.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Antuña SA, Sánchez-Márquez JM, Barco R. Long-term results of radial head resection following isolated radial head fractures in patients younger than forty years old. J Bone Joint Surg Am. 2010;92:558–566. doi: 10.2106/JBJS.I.00332. [DOI] [PubMed] [Google Scholar]
- 2.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–674. [PubMed] [Google Scholar]
- 3.Burkhart KJ, Mattyasovszky SG, Runkel M, Schwarz C, Küchle R, Hessmann MH, Rommens PM, Lars MP. Mid- to long-term results after bipolar radial head arthroplasty. J Shoulder Elbow Surg. 2010;19:965–972. doi: 10.1016/j.jse.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 4.Burkhart KJ, Mattyasvszky SG, Runkel M, Schwarz C, Rump A, Kuechle R, Hessmann MH, Rommens PM, Müller LP. Clinical and radiological results after Judet’s bipolar radial head prosthesis: long term effects. Ob Ex. 2011;6(2):108–114. [Google Scholar]
- 5.Chanlalit C, Fitzsimmons JS, Moon JG, Berglund LJ, An KN, O’Driscoll SW. Radial head prosthesis micromotion characteristics: partial versus fully grit-blasted stems. J Shoulder Elbow Surg. 2011;20:27–32. doi: 10.1016/j.jse.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 6.Chanlalit C, Shukla DR, Fitzsimmons JS, Thoreson AR, An KN, O’Driscoll SW. Radiocapitellar stability: the effect of soft tissue integrity on bipolar versus monopolar radial head prostheses. J Shoulder Elbow Surg. 2011;20:219–225. doi: 10.1016/j.jse.2010.10.033. [DOI] [PubMed] [Google Scholar]
- 7.Charalambous CP, Stanley JK, Mills SP, Hayton MJ, Hearnden A, Trail I, Gagey O. Comminuted radial head fractures: aspects of current management. J Shoulder Elbow Surg. 2011;20:996–1007. doi: 10.1016/j.jse.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 8.Flinkkilä T, Kaisto T, Sirinö K, Hyvönen P, Leppilahti J. Short- to mid-term results of metallic press-fit radial head arthroplasty in unstable injuries of the elbow. J Bone Joint Surg Br. 2012;94-B(6):805–810. doi: 10.1302/0301-620X.94B6.28176. [DOI] [PubMed] [Google Scholar]
- 9.Frank SG, Grewal R, Johnson J, Faber KJ, King GJW, Athwal GS. Determination of correct implant size in radial head arthroplasty to avoid overlengthening. J Bone Joint Surg Am. 2009;91:1738–1746. doi: 10.2106/JBJS.H.01161. [DOI] [PubMed] [Google Scholar]
- 10.Harrington IJ, Sekyi-Otu A, Barrington TW, Evans DC, Tuli V. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: a long-term review. J Trauma. 2001;50(1):46–52. doi: 10.1097/00005373-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Ilahi OA, Bennett JB, Gabel GT, Mehlhoff TL, Kohl HW., 3rd Classification of heterotopic ossification about the elbow. Orthopedics. 2001;24(11):1075–1078. doi: 10.3928/0147-7447-20011101-20. [DOI] [PubMed] [Google Scholar]
- 12.Kiene J, Wäldchen J, Schulz AP, Jürgens C, Paech A. Midterm results of 19 fractures of the coronoid process of the ulna and concomitant injuries. Ob Ex. 2012;7(3):166–173. doi: 10.2174/1874325001307010086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moghaddam A, Lennert A, Studier-Fischer S, Wentzensen A, Zimmermann G. Prosthesis after comminuted radial head fractures: midterm results. Unfallchirurg. 2008;111:997–1004. doi: 10.1007/s00113-008-1514-9. [DOI] [PubMed] [Google Scholar]
- 14.Moon JG, Berglund LJ, Zachary D, An KN, O’Driscoll SW. Radiocapitellar joint stability with bipolar versus monopolar radial head prostheses. J Shoulder Elbow Surg. 2009;18:779–784. doi: 10.1016/j.jse.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 15.Morrey BF, Tanaka S, An KA. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res. 1991;265:187–195. [PubMed] [Google Scholar]
- 16.O’Driscoll SW, Herald JA. Forearm pain associated with loose radial head prostheses. J Shoulder Elbow Surg. 2012;21:92–97. doi: 10.1016/j.jse.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 17.Ruan HJ, Fan CY, Liu JJ, Zeng BF. A comparative study of internal fixation and prosthesis replacement for radial head fractures of Mason type II. Int Orthop. 2009;33:249–253. doi: 10.1007/s00264-007-0453-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sarris IK, Kyrkos MJ, Galanis NN, Papavasiliou KA, Sayegh FE, Kapetanos GA. Radial head replacement with the MoPyC pyrocarbon prosthesis. J Shoulder Elbow Surg. 2012;21(9):1222–1228. doi: 10.1016/j.jse.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Schofer MD, Peterlein CD, Kortmann HR. Radial head prosthesis – treatment of comminuted radial head fractures combined with elbow instability. Z Orthop Unfall. 2008;146:760–767. doi: 10.1055/s-2008-1038976. [DOI] [PubMed] [Google Scholar]
- 20.Schneeberger AG, Sadowski MM, Jacob HAC. Coronoid process and radial head as posterolateral rotator stabilizers of the elbow. J Bone Joint Surg Am. 2004;86:975–982. doi: 10.2106/00004623-200405000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Shukla DR, Fitzsimmons JS, An KN, O’Driscoll SW. Effect of stem length on prosthetic radial head micromotion. J Shoulder Elbow Surg. 2012;21(11):1559–1564. doi: 10.1016/j.jse.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 22.Turner RG, Rispoli D, Lopez-Gonzalez FM, O’Driscoll SW. Partial allograft replacement of the radial head in the management of complex fracture-dislocations of the elbow. J Shoulder Elbow Surg. 2012;21:396–404. doi: 10.1016/j.jse.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 23.van Riet RP, Morrey BF. Documentation of associated injuries occurring with radial head fractures. Clin Orthop Relat Res. 2008;466:130–134. doi: 10.1007/s11999-007-0064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Riet RP, Sanchez-Soleto J, Morrey BF. Failure of metal radial head replacement. J Bone Joint Surg Br. 2010;92-B:661–667. doi: 10.1302/0301-620X.92B5.23067. [DOI] [PubMed] [Google Scholar]
- 25.Zunkiewicz MR, Clemente JS, Miller MC, Baratz ME, Wysocki RW, Cohen MS. Radial head replacement with a bipolar system: a minimum 2-year follow-up. J Shoulder Elbow Surg. 2012;21:98–104. doi: 10.1016/j.jse.2011.05.012. [DOI] [PubMed] [Google Scholar]