Abstract
Purpose
To address the question, compared to having hip replacement with latent revision, does Bernese periacetabular osteotomy (PAO) before primary hip replacement occupy a preferable treatment strategy for middle aged (aged 35–54 years) hip dysplasia patients? We assessed the mid-term functional outcome and survivorship of PAO in those patients.
Methods
Forty-one hips in 36 patients at middle age at the time of surgery (mean age, 39.5 years; range, 35–47 years) were retrospectively identified out of a total PAO cohort of 315 patients. Eleven of the 41 PAO hips also underwent osteochondroplasty at the femoral head-neck junction. Radiographic parameters of lateral centre edge angle, anterior centre edge angle and hip joint medialisation were investigated using the Harris Hip Score (HHS).
Results
The average follow-up was 5.1 years (range, two to ten years). Radiographic parameters postoperatively improved into the normal range, whereas no progression was found from preoperative Tonnis osteoarthritis score. Forty hips survived at the last follow-up, with HHS Score improved from 63.7 to 88.4. Compared to the sole PAO group, both postoperative alpha angle and range of joint motion improved in the PAO combined with osteochondroplasty group. However, no difference in HHS score was found.
Conclusions
Good survivorship and improved joint function were identified in middle-aged Chinese patients following PAO with or without osteochondroplasty. We prudently suggest PAO as an alternative strategy for treating DDH in those patients.
Introduction
Bernese periacetabular osteotomy (PAO) has been practised over the past 24 years [1]. As one of the joint preserving operations, PAO is usually suggested for the treatment of developmental dysplasia of hip (DDH) in adolescents and young adults. Old people with severe osteoarthritis are more suitable for hip replacement, since older age and higher preoperative osteoarthritis grade have been identified as two important predictors of PAO failure [1–5]. Debate has focussed on the treatment of middle aged DDH patients who usually have mild or moderate osteoarthritis at an age of 35–54 years, especially when the reported survival rate of hip prosthesis is much greater than it used to be [6, 7]. Based on data in the Norwegian Arthroplasty Register, only 11 % of 24,728 implants were revised after 18 years [7]. Listed by the United Nations, the average life expectancy of Chinese people was 73 years in 2010 [8]. Since middle aged patients would have a high possibility of hip revision surgery in their lifetime, either having hip replacement with latent revision or having PAO before primary hip replacement, presents us with a dilemma, because few studies have evaluated mid or long-term results in middle aged patients treated with PAO.
Millis et al. and Garbuz et al. both reported good outcome of PAO in patients over the age of 40 [2, 9]. Millis et al. also published a survival rate of 76 % after average 4.9 years follow-up [2]. However, the WOMAC pain and function score in PAO group was not as good as that of a similarly aged group of patients treated by primary total hip replacement [9]. In order to evaluate the priority between having hip replacement with latent revision and having PAO before primary hip replacement, we suggested that the results of hip revision, not primary hip replacement, should be compared with that of PAO in middle aged patients. Based on this premise we retrospectively assessed the mid-term functional outcome and survivorship of PAO in middle aged patients. Finally, the result of these patients was compared with that of revised hip in literature.
Patients and methods
Forty-one hips in 36 patients aged from 35 to 54 years (mean 39.5 years) at the time of surgery between March 2001 and December 2009 were retrospectively identified out of a total PAO cohort of 315 (341 hips) patients at our institution. The thirty-four female (39 hips) and two male patients were investigated according to the ethical standards of the committee on human experimentation of our institution. All of the patients were diagnosed as developmental dysplasia of the hip (DDH) with hip pain and mean 6.4° of lateral centre edge angle (LCEA) on the anteroposterior (AP) radiograph. The average body-mass index was 21.4 (range, 18.2 to 26.6). Fifteen hips (37 %) had a total of twenty surgical procedures prior to the index PAO, including open reduction, Salter osteotomy, trochanteric transfer and varus-producing proximal femoral osteotomy. All patients had hip flexion of 95° or more. Congruency was preoperatively confirmed on a functional radiograph with the hip in abduction and internal rotation. All hips had different grades of osteoarthritis: twelve grade 1, twenty-two grade 2, and seven grade 3 according to the Tönnis classification [10].
Surgical technique
As previously described by Ganz and Siebenrock [10, 11], PAO through a modified Smith-Peterson approach was performed by one senior surgeon (X. Chen) in all of the patients. After four periacetabular osteotomies and a controlled fracture, the completely mobile acetabulum was reduced and fixed with three 4.5-mm cortical screws. The posterior column of the pelvis remained intact apart from one patient. Another fragment that was previously cut from the anterior superior iliac spine was fixed with a 3.5-mm cortical screw. Acetabular inclination, rotational centre, and femoral head coverage were intraoperatively assessed with fluoroscopic images. Concurrent proximal femoral varus-producing osteotomy was performed in four hips when there was a greater femoral neck-shaft angle (> 150°) or femoral neck anteversion angle (> 40°). Since 2008, anterior arthrotomy was almost routinely performed through the same incision, especially when anterior femoroacetabular impingement was positive. Angle α, which was described by Notzli et al. [12], was measured. From 2008 to 2009, osteochondroplasty of the femoral head-neck junction was performed to improve femoral head-neck offset in eleven hips that had a preoperative α angle of greater than 55° [12]. Acetabular labral tears were also found and debrided in three hips. Patients were hospitalised for an average of 9.6 days (range, eight to 15 days). Partial weight bearing was encouraged on the third postoperative day with two crutches. Twelve weeks later, full weight bearing was allowed if osseous healing was seen radiologically at the osteotomy sites.
Clinical and radiographic evaluation
Clinical results were evaluated using the range of motion (ROM) and Harris hip score (HHS) preoperatively, at six months and one year postoperatively, and then yearly until the last follow-up or hip replacement. Clinical failure was defined as the involved hip being recommended for hip replacement. Radiographic evaluation was performed by one surgeon (Y. Cui). Anteroposterior and false cross-table lateral radiographs were made at each follow-up. Preoperative and postoperative hip centre position, Angle α, LCEA and anterior centre-edge angle (ACEA) were measured and compared. Hip joint medialisation was determined by measuring the distance between the ilioischial line and the medial aspect of the femoral head. Provided consolidation appeared across the osteotomy sites, osseous healing was reported. Osteoarthritis (OA) progression was evaluated using the Tonnis classification system [10].
Statistical analysis
Preoperative and postoperative HHS scores and radiographic evidence were compared using t test. The eleven hips that had PAO combined with osteochondroplasty were compared with ten other hips of this cohort that had PAO surgery alone before 2008, but occupied a preoperative α angle of bigger than 55°. Significance was determined at a p value of < 0.05.
Results
The average follow-up was 5.1 years (range, two to ten years). Forty of the forty-one hips survived at the last follow-up. Only one lady who was 42 years old at PAO surgery converted to total hip replacement in the ninth postoperative year. The average HHS score and radiographic evaluation in these patients postoperatively improved, whereas no progression was found from preoperative Tonnis OA score (Fig.1 and Table 1). Only five hip Tonnis scores increased from grade 2 to grade 3, one from grade 2 to grade 4 and one from grade 3 to grade 4 at the last follow-up.
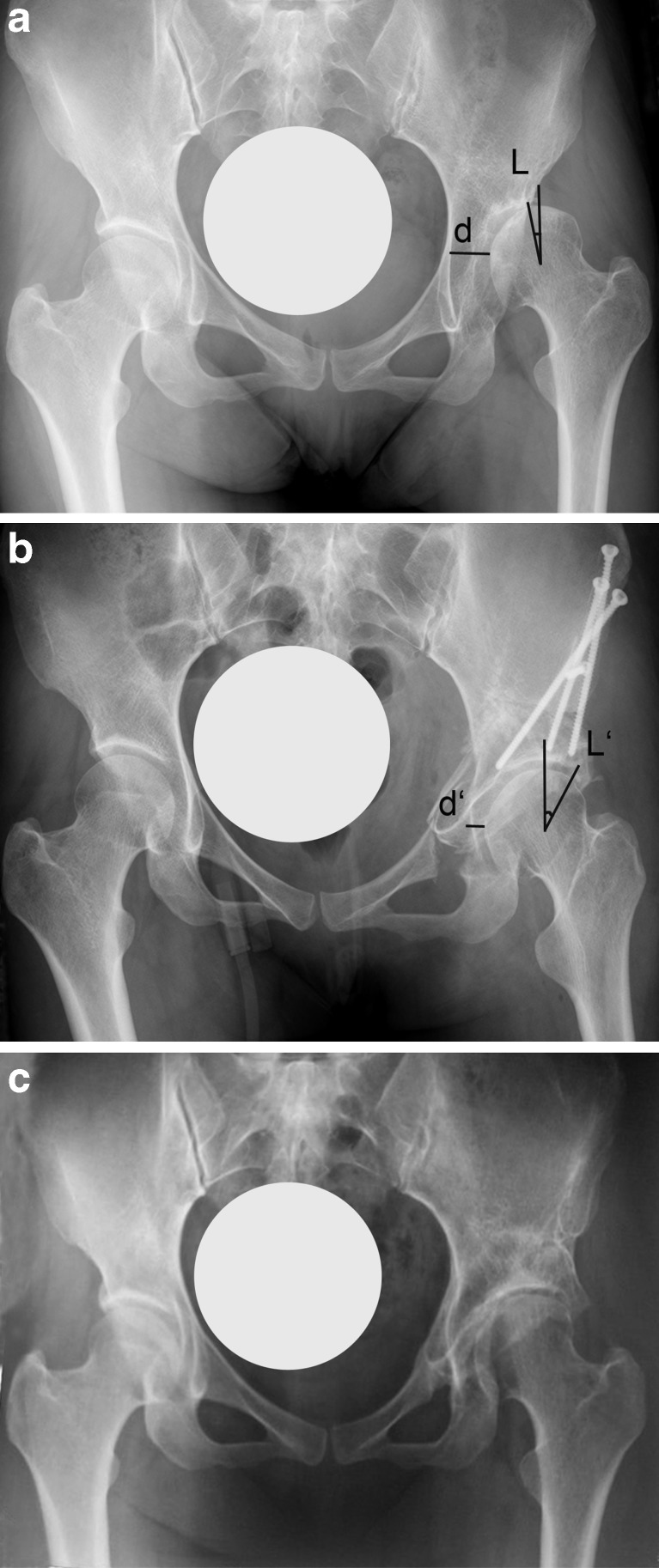
Fig. 1.
Radiographs are shown of a 38-year-old woman with left dysplastic hip. a The preoperative LCEA was -7° and the preoperative hip joint medialisation was 22 mm. The preoperative Harris hip score was 64. b The postoperative LCEA was 27° and the postoperative hip joint medialisation was 8 mm. c At the 5-year follow-up, the Harris hip score was 90 and no progression was found on osteoarthitic change. Letter L and L’ refer to LCEA, which means lateral centre edge angle. Letter d and d’ refer to hip joint medialisation, which was determined by measuring the distance between the ilioischial line and the medial aspect of the femoral head. The postoperative hip joint medialisation decreased from 22 mm to 8 mm, which indicated that the hip joint was translated medially 14 mm in this case
Table 1.
Preoperative and postoperative radiographic and clinical results
| n=41 | Preoperative value | Postoperative value | p Value |
|---|---|---|---|
| Lateral centre edge angle (°) | 6.4 ± 5.0 (−4.6–14.8) | 29.1 ± 4.2 (20.5–35.5) | < 0.001 |
| Anterior centre edge angle (°) | 7.6 ± 4.4 (−2.2–16.4) | 27.4 ± 4.5 (16.8–35.7) | < 0.001 |
| Hip joint medialisation (mm) | 15.4 ± 3.8 (8.6–20.8) | 8.9 ± 2.9 (5.1–14.3) | < 0.001 |
| Harris hip score | 63.7 ± 8.6 (50–78) | 88.4 ± 7.8 (45–96) | < 0.001 |
| Tonnis grade | 1.9 ± 0.7 (1–3) | 2.0 ± 0.9 (1–4) | 0.323 |
Values are expressed as mean ± standard deviation with range in parentheses
In comparison to the PAO only group, the mean preoperative α angle, ROM and HHS score were similar in the PAO combined with osteochondroplasty group, whereas postoperative α angle decreased (Fig. 2 and Table 2). At two year follow-up, postoperative ROM was significantly better (p < 0.001) in the PAO combined with osteochondroplasty group. The improved HHS score was also slightly better in this group; however, the difference was not significant. Finally, the survival rate was similar since, no hip failed in the two years of follow-up.
Fig. 2.
Radiographs are shown of a 42-year-old woman with dysplastic right hip. a She preoperatively presented with a negative impingement test, even if the alpha angle was 60°. b During the operation, the impingement test converted to positive following the rotation and fixation of the acetabular fragment. However, the impingement test returned to negative after osteochondroplasty of the femoral head-neck junction by which the postoperative alpha angle was improved to 41°. Letters α and α’ refer to alpha angle, which was described by Notzli et al. [12]
Table 2.
Comparision between solo periacetabular osteotomy (PAO) group and PAO combined with osteochondroplasty group
| PAO | PAO combined with osteochondroplasty | p Value | |
|---|---|---|---|
| n | 10 | 11 | |
| α angle (°) | 62.3 ± 6.8 (55.8–73.8) | 64.1 ± 7.6 (54.6–76.8) | 0.563 |
| α angle (°) | 62.3 ± 6.8 (55.8–73.8) | 33.3 ± 3.6 (29.8–41) | < 0.001 |
| Range of motion (°) | 177.5 ± 16.7 (155–205) | 179.1 ± 13.6 (160 –200) | 0.812 |
| Range of motion (°) | 129.5 ± 9.6 (120–145) | 170.5 ± 10.4 (150–180) | < 0.001 |
| Harris hip score | 61.6 ± 9.5 (50–78) | 63.5 ± 7.8 (53–76) | 0.631 |
| Harris hip score | 90.5 ± 3.6 (84–95) | 91.5 ± 2.8 (88–96) | 0.506 |
Preoperative data bold. Postoperative Harris hip scores were evaluated at 2 year follow-up. Range of motion referred to the sum of flexion, internal and external rotation. Values are expressed as mean ± standard deviation with range in parentheses
The complications in this cohort were recorded as follows: Posterior column fracture of the pelvis occurred in one hip and healed after six months. There were nine cases of lateral femoral cutaneous nerve injury, four of which completely resolved at the last follow-up. Six patients had delayed union at the site of pubic osteotomy. Neither femoral neck fracture nor avascular femoral head necrosis was found following the surgery in this cohort.
Discussion
Because of clinically and sonographically deficient screening for DDH in neonates and infants, most of the middle aged DDH patients did not obtain early diagnosis and treatment over the past 30 years. They consequently suffer from painful hips with different grades of OA and struggle to make a choice between hip replacement and joint preserving surgery. Two different strategies for treating symptomatic DDH were suggested to middle aged patients in China. One strategy was to have primary hip replacement in middle age and hip revision in older age. The alternative was to have PAO in middle age, and then primary hip replacement in older age. Due to their higher level of physical activity, primary hip replacement in younger people results in a relatively worse survivorship in literature than that in older people [13, 14]. Provided a primary hip replacement was performed in DDH patients, the survivorship, which ranged from 60 % to 78 % at 14 year follow-up, significantly decreased [15, 16]. Loosening of the acetabular component accounted for most of the failure. Several surgical techniques, such as shelf graft, have been suggested for increasing the acetabular coverage in DDH patients. Failed pelvic osteotomies might have compromised the subsequent hip replacement; however, a properly performed PAO procedure or other pelvic osteotomy would contribute to the success of a later hip replacement by making the stability of the acetabular component more reliable [15, 17, 18], since both LCEA and ACEA postoperatively improved to the normal range in this study. How about the comparison between PAO in middle aged and hip revision in old people? Provided both have comparable long-term results may mean that primary hip replacement following PAO is an alternative strategy for middle aged patients.
As previously noted, both postoperative LCEA and ACEA in this study were comparable to others [1, 2]. The improved acetabular version increased femoral head coverage, and decreased the stress on hip joint surface, which prevented further cartilage injury. It was consistent with the unchanged average Tonnis grade in this study. Hip joint medialisation decreased from 15.4 mm preoperatively to 8.9 mm postoperatively in this cohort, which resulted in smaller medial translation of hip centre than others [19]. The difference could result from the smaller pelvis in the Chinese and the conservative technique in the early stage of our learning curve. However, the hip survivorship in this study exceeded the 76 % in Millis’s report [2], even if we had higher grade of preoperative OA. The following aspects could account for the advantage. First, both the average age (39.5 years) at the time of surgery and the BMI (21.4) in this study differed from those of Millis who had a bigger BMI in patients older than 40 years [2]. Second, fewer cases of preoperative surgery in our cohort could improve the postoperative results. Additionally, Chinese patients usually had relatively low level of physical activity, which decreased the risk of aggravating cartilage injury. Good outcome of periacetabular osteotomy has also been reported in patients older than 50 years by our Japanese colleagues [20, 21]. During a minimum two-year follow-up, Teratani et al. noted a mean HHS score that improved from 69.6 preoperatively to 90.9 postoperatively [20]. Compared to the result of hip revision in literature, which was not encouraging in the past [22] but clinically and radiographically improved in recent studies [23, 24], the functional outcome and survivorship of PAO in this cohort and others [2, 9, 20, 21] were comparable. Therefore, we prudently suggest PAO as an alternative strategy for treating DDH in middle aged Chinese patients.
Osteochondroplasty for treating hip impingement following PAO was introduced by Ganz et al. in 1999 [11]. Cam and pincer, two different types of femoroacetabular impingement, have been recognised in previous reports [25]. Pincer deformity was rarely found in our department. On the contrary, cam deformity, which refers to deformity of femoral head-neck junction, has been frequently identified in middle aged DDH patients. The preoperative impingement test was mostly negative in these patients, due to the lack of anterior acetabular coverage. Unfortunately, it usually converted to positive following a great correction of the ACEA. In our previous publication, the range of hip motion in DDH patients with PAO alone, decreased postoperatively at a level of more than 20° [26]. Similar results were indicated in other studies [1, 11]. In this study, osteochondroplasty really improved postoperative ROM; however, no difference of HHS score was found between the two groups at two year follow-up. This could result from the short duration of follow-up. We presume that the outcome of PAO combined with osteochondroplasty group would have an advantage over that of solo PAO group in long-term follow-up, since impingement has been identified as a major aetiological factor in the pathogenesis of hip osteoarthritis [1, 25].
This study has several limitations. First, there was no broad consensus on the definition of middle aged adults. The US Census defined middle age as the age from 35 to 54 [27]. The average life expectancy was 73 years for Chinese and 78 years for Americans in 2010 [8, 27]. Therefore, it made sense to determine the middle age in Chinese as age of over 35 years. Second, no control group of hip revision could be matched to this study. So, the outcome and survivorship of PAO was directly compared with those in literature. Third is the relatively small number of patients. At the early stage of our practice, we were limited by both the learning curve and conservative patient selection. Nowadays, we undertake more than one hundred cases of PAO surgery every year. Fourth, seven of forty-one patients did not return to our clinic at the last follow-up. We thought, however, it was reasonable to include the seven patients, since they were interviewed by telephone and were still satisfied with the involved hips. Finally, the outcome of sole PAO was compared with that of PAO combined with osteochondroplasty. The comparison could be affected by the learning curve of PAO, since osteochondroplasty was only performed after 2008.
In summary, good survivorship and improved joint function were identified in middle aged Chinese patients following PAO. Based on the following aspects, we prudently suggest PAO as an alternative strategy for treating DDH in middle aged Chinese patients. First, the outcome of hip preserving surgery was comparable to that of hip revision in mid-term follow-up. Due to superior BMI and relatively low level of physical activity, hip preserving surgery such as the Bernese PAO seems to have greater potential in Asian patients. Second, due to the higher level of physical activity, primary hip replacement is supposed to have higher risk of failure in younger people than older people. Third, a prior PAO would restore the acetabular version to a relatively normal anatomy, which would have beneficial effects on subsequent acetabular cup fixation and survivorship [19]. Finally, the medical costs for PAO were less than those associated with hip replacement, whereas, the costs for hip revisions were 4.8 folds higher than primary hip replacement [28]. Further investigation is needed to determine the long-term outcome of PAO combined osteochondroplasty in middle aged patients.
Acknowledgments
The study was financially supported by National Natural Science Foundation of China (NO. 81171705 and 81101381) and Research Foundation of Shanghai Jiaotong University Medical School (NO. YZ1002).
Conflict of interest
We declare that we have no conflicts of interest in the authorship or publication of this contribution.
References
- 1.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Millis MB, Kain M, Sierra R, Trousdale R, Taunton MJ, Kim YJ, Rosenfeld SB, Kamath G, Schoenecker P, Clohisy JC. Periacetabular osteotomy for acetabular dysplasia in patients older than 40 Years. Clin Orthop Relat Res. 2009;467:2228–2234. doi: 10.1007/s11999-009-0824-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sambandam SN, Hull J, Jiranek WA. Factors predicting the failure of Bernese periacetabular osteotomy: a meta-regression analysis. Int Orthop. 2009;33(6):1483–1488. doi: 10.1007/s00264-008-0643-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shinoda T, Naito M, Nakamura Y, Kiyama T. Periacetabular osteotomy for the treatment of dysplastic hip with Perthes-like deformities. Int Orthop. 2009;33(1):71–75. doi: 10.1007/s00264-007-0476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biedermann R, Donnan L, Gabriel A, Wachter R, Krismer M, Behensky H. Complications and patient satisfaction after periacetabular pelvic osteotomy. Int Orthop. 2008;32(5):611–617. doi: 10.1007/s00264-007-0372-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petsatodis GE, Papadopoulos PP, Papavasiliou KA, Hatzokos IG, Agathangelidis FG, Christodoulou AG. Primary cementless total hip arthroplasty with an alumina ceramic-on-ceramic bearing: results after a minimum of 20 years offollow-up. J Bone Joint Surg Am. 2010;92(3):639–644. doi: 10.2106/JBJS.H.01829. [DOI] [PubMed] [Google Scholar]
- 7.Espehaug B, Furnes O, Engesaeter LB, Havelin LI. 18 years of results with cemented primary hip prostheses in the Norwegian Arthroplasty Register: concerns about some newer implants. Acta Orthop. 2009;80(4):402–412. doi: 10.3109/17453670903161124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zheng XY, Chen SJ. Life expectancy of people with physical disabilities in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(7):693–696. [PubMed] [Google Scholar]
- 9.Garbuz DS, Awwad MA, Duncan CP. Periacetabular osteotomy and total hip arthroplasty in patients older than 40 years. J Arthroplast. 2008;23:960–963. doi: 10.1016/j.arth.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 10.Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20. doi: 10.1097/00003086-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. doi: 10.1097/00003086-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Nötzli HP, Wyss TF, Stocklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 13.Makela KT, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V. Cementless total hip arthroplasty for primary osteoarthritis in patients aged 55 years and older. Acta Orthop. 2010;81:42–52. doi: 10.3109/17453671003635900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop. 2006;77:57–70. doi: 10.1080/17453670610045704. [DOI] [PubMed] [Google Scholar]
- 15.Parvizi J, Burmeister H, Ganz R. Previous Bernese periacetabular osteotomy does not compromise the results of total hip arthroplasty. Clin Orthop Relat Res. 2004;423:118–122. doi: 10.1097/01.blo.0000128287.98083.63. [DOI] [PubMed] [Google Scholar]
- 16.Berry DJ, Harmsen WS, Ilstrup D, Lewallen DG, Cabanela ME. Survivorship of uncemented proximally porous-coated femoral components. Clin Orthop Relat Res. 1995;319:168–177. [PubMed] [Google Scholar]
- 17.Peters CL, Beck M, Dunn HK. Total hip arthroplasty in young adults after failed triple innominate osteotomy. J Arthroplast. 2001;16:188–195. doi: 10.1054/arth.2001.20903. [DOI] [PubMed] [Google Scholar]
- 18.Tokunaga K, Aslam N, Zdero R, Schemitsch EH, Waddell JP. Effect of prior Salter or Chiari osteotomy on THA with developmental hip dysplasia. Clin Orthop Relat Res. 2011;469(1):237–243. doi: 10.1007/s11999-010-1375-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Medial translation of the hip joint center associated with the Bernese periacetabular osteotomy. Iowa Orthop J. 2004;24:43–48. [PMC free article] [PubMed] [Google Scholar]
- 20.Teratani T, Naito M, Kiyama T, Maeyama A. Periacetabular osteotomy in patients 50 years of age or older: surgical technique. J Bone Joint Surg Am. 2011;93:30–39. doi: 10.2106/JBJS.J.01126. [DOI] [PubMed] [Google Scholar]
- 21.Ito H, Tanino H, Yamanaka Y, Minami A, Matsuno T. Intermediate to long-term results of periacetabular osteotomy in patients younger and older than 40 years of age. J Bone Joint Surg Am. 2011;93:1347–1354. doi: 10.2106/JBJS.J.01059. [DOI] [PubMed] [Google Scholar]
- 22.Howie DW, Wimhurst JA, McGee MA, Carbone TA, Badaruddin BS. Revision total hip replacement using cemented collarless double-taper femoral components. J Bone Joint Surg Br. 2007;89(7):879–886. doi: 10.1302/0301-620X.89B7.18981. [DOI] [PubMed] [Google Scholar]
- 23.Randhawa K, Hossain FS, Smith B, Mauffrey C, Lawrence T. A prospective study of hip revision surgery using the Exeter long-stem prosthesis: function, subsidence, and complications for 57 patients. J Orthop Traumatol. 2009;10:159–165. doi: 10.1007/s10195-009-0068-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adolphson PY, Salemyr MOF, Sköldenberg OG, Bodén HSG. Large femoral bone loss after hip revision using the uncemented proximally porous-coated Bi-Metric prosthesis. Acta Orthop. 2009;80(1):14–19. doi: 10.1080/17453670902804802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beck M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 26.Chen XD, Cui YM, Shen C, Zhang X, Wang YR, Zhu JF, Zhou ZD. Treatment of developmental dysplash of the hip with periacetalmlar osteotomy. Chin J Orthop. 2010;30(2):143–147. [Google Scholar]
- 27.Arias E, Rostron BL, Tejada-Vera B. United States life tables, 2005. Natl Vital Stat Rep. 2010;58(10):1–132. [PubMed] [Google Scholar]
- 28.Bozic KJ, Ries MD. The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg Am. 2005;87:1746–1751. doi: 10.2106/JBJS.D.02937. [DOI] [PubMed] [Google Scholar]