Abstract
Purpose
The need for perioperative blood management measures aimed at improving patient outcomes and reducing allogenic blood transfusion (ABT) is increasingly recognised. Our study aim is to create an algorithm to predict and manage the need for blood transfusion in patients with hip fractures.
Methods
We retrospectively assessed 1,484 patients with hip fractures and analysed the probability of receiving an ABT within 72 hours of admission. Univariate, multiple logistic regression analysis and a probability algorithm for predicting the need for blood transfusion on the basis of independent multivariate predictors were used.
Results
Significant predictors for ABT were: older age; lower haemoglobin on admission; female gender; type of surgical implant (cephalomedullary nail and dynamic hip screw more than hemiarthroplasty); and a shorter wait time from admission to surgery. A regression model algorithm correctly predicted the need for an ABT in 73 % of the cases.
Conclusion
An algorithm and a simple clinical tool were devised to predict and manage the need for a blood transfusion within 72 hours of admission in patients with hip fractures.
Introduction
Hip fractures rate first among all orthopaedic procedures in terms of use of hospital resources, due to adverse events and excess hospital day stay [1]. The need for perioperative patient blood management measures aimed at improving patient outcomes and reducing allogenic blood transfusion (ABT) is increasingly recognised [2]. Studies suggest we are over cross-matching and over transfusing patients, and evidence-based medicine supports the adoption of restrictive transfusion policies [3–6]. Indeed, restrictive policies have been shown not to negatively influence morbidity, mortality or functional outcomes in patients with hip fractures [5–7]. Moreover, over transfusion influences patient health and has economic implications. Allogenic blood transfusion is a known risk factor for immunosupression and increases the risk of infection [8].
The purpose of this study was to assess the epidemiological characteristics of patients requiring allogenic blood transfusion admitted to hospital with a hip fracture. Using this data, an algorithm was built to predict the need for transfusion according to current hospital current transfusion guidelines. A train test statistical model was used to validate the algorithm. The study hypothesis was that we would be able to predict which patients admitted with a hip fracture would not need a blood transfusion in 70 % of the cases. By better managing this process, patients may receive optimal care without straining hospital resources, thus reducing the cost of care [9].
Materials and methods
This retrospective, single level I (1,400 bed) institution, database study was based on data gathered from the hospital electronic medical record (EMR) system and the blood bank database. One thousand four hundred eighty four patients admitted with a hip fracture that underwent surgical treatment between 2007 and 2010 were included. The average age was 82 years (SD 10.3). There were 1,024 females (69 %) and 460 males (31 %); only 40 (2 %) were younger than 55 years. The study excluded patients with non-displaced intracapsular fractures that were treated nonoperatively or with cannulated screws, and non-ambulatory, nursing home, demented patients that were treated nonoperatively. Risk factors for an ABT that were assessed included patient demographics (age, gender), fracture type, time from admission to surgery, laboratory values (haemoglobin [Hb], mean corpuscular volume [MCV], international normalised ratio [INR], creatinine), medications (aspirin, clopidogrel, proton pump inhibitors, diabetes medication, statins), and surgical details (procedure type, length of procedure).
Monitoring Hb and transfusion protocol
On admission to hospital, all patients had a full blood count (CBC), two samples of blood were taken for ABO Rh group type, antibody screen and two units of packed red blood cells (RBC) were cross-matched and ordered. Mean haemoglobin on admission for males was 12.7 g/dl (SD 1.8), 51 % of those were anaemic (Hb < 13 g/dl), and microcytic anaemia was prevalent in four percent of male anaemic patients. Mean haemoglobin for females was 12.1 g/dl (SD 1.5), 42 % of the females were anaemic (Hb < 12 g/dl), and microcytic anaemia was prevalent in ten percent of those anaemic patients. Two units of packed RBC were cross-matched for all hip fractures. An additional cross-match was carried out after 72 hours and 48 hours thereafter as needed, as blood bank safety regulations cause the previous sample to expire. A full blood count was taken on post-op days one and three, when patients presented signs of symptomatic anaemia (tachycardia, weakness, palpitations) and after blood transfusion.
Our institute currently adheres to the liberal blood transfusion approach. According to our transfusion protocol, patients were transfused to a haemoglobin of 10 g/dl pre-op. Patients were transfused post-operatively when their haemoglobin dropped below 8 g/dl. This “transfusion trigger” was raised to 10 g/dl in clinically symptomatic patients (extreme weakness, chest pain, extreme paleness or major bleeding); if vital signs were abnormal (tachycardica, heart rate [HR] > 100, and low blood pressures, systolic blood pressure [SBP] < 90); and in those with a history of heart disease (coronary, valvular, and arrhythmia) or cerebrovascular disease.
Surgical procedure
Five hundred and seventy nine patients underwent hemiarthroplasty, 730 patients underwent a dynamic hip screw fixation and 175 had a cephalomedullary nail inserted. Patients with an intracapsular fracture were treated with a hemiarthroplasty, most commonly an uncemented bipolar (428 patients, 29 %) (Taperloc, Biomet, Warsaw, USA) or a cemented Thompson prosthesis (151 patients, 10 %) (Biomet, Bridgend, South Wales, UK). Pertrochanteric fractures were treated with a dynamic hip screw plate (49 %). Subtrochanteric and reverse oblique fractures were fixed with a cephalomedullary nail, (12 %) (Gamma nail, Stryker, MI,USA; Fixion nail, CarboFix, IL). Preoperatively, patients were given low-dose (40 mg) enoxaparine until 12 hours before surgery. Postoperatively, enoxaparin (40 mg) was given once daily for 30 days.
Statistical analysis was conducted with SAS for windows version 9.2. Univariate analysis was used to compare the group which received an ABT within 72 hours and the group that did not with respect to 14 variables.
Continuous variables that follow a normal distribution were analysed using a two-sample Student t test, and variables that did not follow the normal distribution were analysed using the Wilcoxson two sample test. The Pearson chi-square test was used to compare the groups with respect to categorical variables.
A Multivariate logistic regression was applied to identify the significant independent predictors for blood transfusion. The full regression model included 13 risk factor candidates. Model selection methods such as backward elimination were used in order to identify important factors from the 12 explanatory variables. The final parsimonious model included five risk factors that have a statistical significant effect on receiving blood transfusion.
In addition, the train/test method was employed. The data set was randomly split into two sets: training set and test set (70 % and 30 % respectively). The final five risk factors predictive model was applied to the training set and the quality of the predictions was assessed by the root mean squared error (RMSE) of the test set.
Results
One thousand four hundred and eighty four patients with hip fractures were treated, and 581 patients (39 %) received an ABT within the first 72 hours from admission, which is the expiry time of the cross-match sample taken on admission. An additional 301 patients (20 %) who were treated with an ABT during their admission needed a new cross-match blood sample before transfusion (Table 1). The 30-day mortality rate was 5 % and the 90-day mortality was 9.8 %. In the perioperative period (ten days from admission) 604 patients (41 %) did not receive an allogenic blood transfusion (ABT), 402 (27 %) received one ABT, 314 (21 %) patients received two units, 164 (11 %) were treated with more than two units.
Table 1.
General characteristics of 1,484 patients with hip fracture treated between 2007 and 2010
| Patient characteristics | Means (SD) | |
|---|---|---|
| Age (years) | 81.76 (10.27) | |
| Gender (female/male) | 69 %/31 % | |
| Surgery time (minutes) | 107.4 (30) | |
| Time from admission to surgery (hours) | 57.42 (65.3) | |
| Haemoglobin at admission (g/dL) | 12.27 (1.64) | |
| MCV at admission (fl) | 88.99 (5.86) | |
| Creatinine at admission (mg/dL) | 1.22 (0.58) | |
| INR at admission | 1.13 (0.47) | |
| Use of statins | 490 (33 %) | |
| Use of diabetes mellitus drugs | 208 (14 %) | |
| Use of aspirin | 312 (21 %) | |
| Use of clopidogral | 74 (5 %) | |
| Type of implant | Hemiarthroplasty | 579 (39 %) |
| Cephalomedullary nail | 175 (12 %) | |
| Dynamic hip screw | 730 (49 %) | |
| Packed Cells issued within 72 hours of admission | 581 (39 %) | |
| Packed Cells issued intra-operatively | 126 (8.4 %) | |
| Packed Cells issued within 10 days of admission | 880 (59 %) | |
MCV mean corpuscular volume, INR international normalised ratio
The values are given as the mean and the standard deviation for continuous variables and as the number of patients, with the percentage in parentheses, for categorical variables
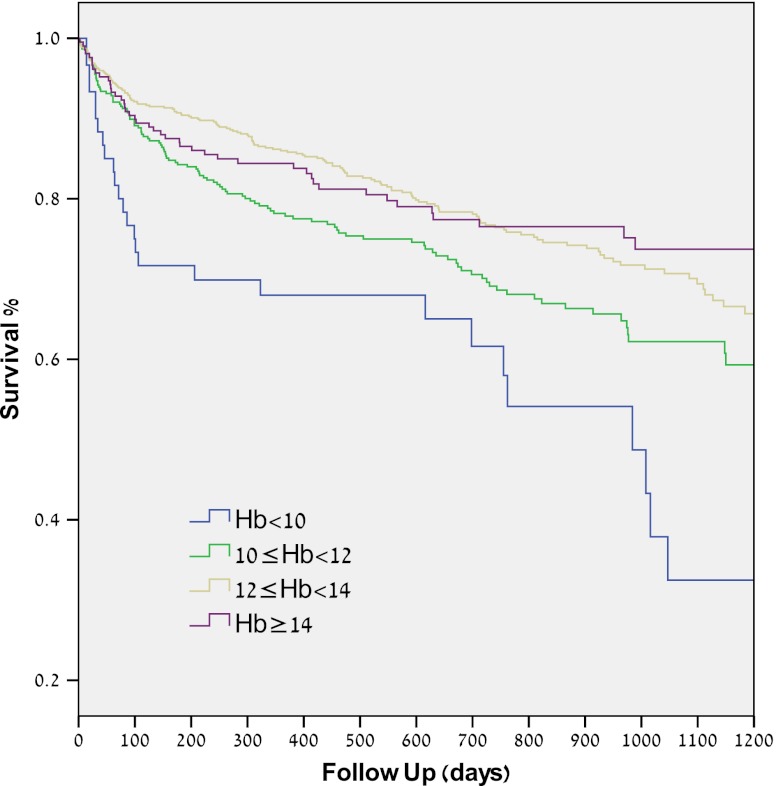
Risk factors for ABT within 72 hours from admission were assessed with univariate analysis (Table 2). Significant risk factors (p < 0.001) were age (83.4 ± 9.3 years vs. 80.6 ± 10.6 years), haemoglobin at admission (11.39 ± 1.57 g/dl compared with 12.83 ± 1.4 g/dl), INR at admission (1.08 ± 0.37 compared with 1.15 ± 0.52), female gender, type of surgical implant (cephalomedullary nail and dynamic hip screw), a shorter wait time from admission to surgery (40 ± 34.9 hours compared with 68 ± 76.7 hours). Similar same risk factors were significant on univariate analysis for ABT within ten days from admission (Table 3). Additional analysis demonstrated that higher presurgical haemoglobin level was associated with better patients’ survival. Haemoglobin level was not associated with post-operative complications, such as infections, cardiac, thromboembolic or cerebrovascular events (see Table 5 and Fig. 4 in the appendix).
Table 2.
Univariate analysis of risk factors for allogenic blood transfusion (ABT) within 72 hours from admission in 1,484 patients with hip fractures
| Variable | No ABT within 72 hours | ABT within 72 hours | P value | |
|---|---|---|---|---|
| Age at Admission (years) | 80.6 (10.6) | 83.4 (9.3) | < 0.001* | |
| Gender (Female/Male) | 64 %/36 % | 78 %/22 % | < 0.001§ | |
| Surgery time (minutes) | 102 (24) | 108 (34) | < 0.001* | |
| Time admission to surgery (hours) | 68.91 (76.78) | 39.55 (34.9) | ||
| Log | 3.8 (0.86) | 3.4 (0.71) | < 0.001* | |
| Haemoglobin at admission (g/dL) | 12.83 (1.4) | 11.39 (1.57) | < 0.001 * | |
| MCV at admission (fl) | 82.22 (5.4) | 88.62 (6.37) | 0.06* | |
| Creatinine at admission (mg/dL) | 1.21 (0.6) | 1.25 (0.56) | ||
| Log | 0.12 (0.32) | 0.15 (0.33) | 0.06* | |
| INR at admission | 1.15 (0.52) | 1.08 (0.37) | 0.04¥ | |
| Type of implant | Hemiarthroplasty | 48 % | 24.6 % | < 0.001 § |
| Cephalomedullary nail | 7.3 % | 18.7 % | ||
| Dynamic hip screw | 44.4 % | 56.6 % | ||
| Statins used (%) | 34 % | 31 % | 0.32§ | |
| Proton pump inhibitors used (%) | 38 % | 35 % | 0.23§ | |
| Diabetes mellitus drugs used (%) | 14 % | 14 % | 0.69§ | |
| Aspirin used (%) | 22 % | 20 % | 0.27§ | |
| Clopidogral used (%) | 5 % | 5 % | 0.99§ | |
MCV mean corpuscular volume, INR international normalised ratio
*Two sample t-test
¥Two sample wilcoxon test
§Chi-square test
The values are given as the mean and the standard deviation for continuous variables and as the number of patients, with the percentage in parentheses, for categorical variables
Table 3.
Univariate analysis of risk factors for allogenic blood transfusion (ABT) within 10 days from admission in 1,484 patients with hip fractures
| Variable | No ABT within 10 days | ABT within 10 days | P value | |
|---|---|---|---|---|
| Age at Admission (years) | 79.42 (11.4) | 83.36 (9.04) | <0.001* * | |
| Gender (Female/Male) | 59 %/41 % | 77 %/23 % | <0.001 § | |
| Surgery time (minutes) | 103.2 (25) | 109.8 (33) | <0.001* | |
| Time admission to surgery (hours) | 62.15 (77.65) | 54.17 (55.12) | ||
| Log | 3.74 (0.86) | 3.65 (0.81) | 0.038* | |
| Haemoglobin at admission (g/dL) | 13.17 (1.33) | 11.64 (1.52) | <0.001 * | |
| MCV at admission (fl) | 89.13 (5.2) | 88.88 (6.2) | 0.4* | |
| Creatinine at admission (mg/dL) | 1.19 (0.64) | 1.25 (0.54) | ||
| Log | 0.1 (0.32) | 0.15 (0.33) | 0.0026* | |
| INR at admission | 1.11 (0.47) | 1.14 (0.48) | 0.52¥ | |
| Type of implant | Hemiarthroplasty | 20.82 % | 18.19 % | <0.001 § |
| Cephalomedullary nail | 2.7 % | 9.1 % | ||
| Dynamic hip screw | 17.18 % | 32.01 % | ||
| Statins used (%) | 13.61 % | 19.74 % | 0.95§ | |
| Proton pump inhibitors used (%) | 14.62 % | 22.51 % | 0.42§ | |
| Diabetes mellitus drugs used (%) | 5.46 % | 8.89 % | 0.39§ | |
| Aspirin used (%) | 8.63 % | 12.8 % | 0.85§ | |
| Clopidogral used (%) | 1.62 % | 3.37 % | 0.13§ | |
MCV mean corpuscular volume, INR international normalised ratio
*Two sample t-test
¥Two sample wilcoxon test
§Chi-square test
The values are given as the mean and the standard deviation for continuous variables and as the number of patients, with the percentage in parentheses, for categorical variables
Table 5.
Comparison of haemoglobin level between patients with hip fracture who sustained a post operative complication and those who did not
| Post-operative complication | Mean Haemoglobin (g/dL) of patients with post-operative complications (SD) | Mean Haemoglobin (g/dL) of patients without post-operative complications (SD) | p value* |
|---|---|---|---|
| Pneumonia | 12.06 (1.4) n = 44 | 11.86 (1.3) n = 619 | 0.36 |
| Urinary Tract Infection | 11.89 (1.8) n = 44 | 11.88 (1.3) n = 619 | 0.95 |
| Bacteraemia | 12.11 (1.4) n = 51 | 11.86 (1.3) n = 612 | 0.23 |
| Surgical Site Infection | 12.12 (1.2) n = 39 | 11.86 (1.4) n = 624 | 0.28 |
| Cardiac Related complications | 12.1 (1.7) n = 23 | 11.87 (1.38) n = 640 | 0.47 |
| Respiratory insufficiency | 11.85 (1.5) n = 57 | 11.88 (1.38) n = 606 | 0.86 |
| Renal Failure | 11.85 (1.2) n = 23 | 11.88 (1.4) n = 640 | 0.92 |
| Cerebro-vascular accident | 12.24 (1.5) n = 13 | 11.87 (1.39) n = 640 | 0.38 |
*Two sample t-test
Fig. 4.
Kaplan-Meier survival curve for patients with hip fractures, divided to four groups according to Haemoglobin levels. A significant difference (P = 0.000) exists between the groups. Hb haemoglobin (g/dl) * Compared with LogRank test
Multivariate logistic regression was performed using variables available to the physician when admitting a patient with a hip fracture, in order to simulate a decision analysis situation. Five out of 13 independent variables were found to have a statistically significant effect on the rate of blood transfusion within 72 hours: gender, haemoglobin at admission, INR at admission, age and type of surgery. Regression coefficients, likelihood ratios, p values, adjusted odds ratios, and 95 % confidence intervals were determined (Table 4). The odds of a patient to receive an ABT within 72 hours were five times greater if the expected surgery was cephalomedullary nail compared to hemiarthroplasty. With regard to age, each year increased the risk to receive an ABT by one percent. With regard to haemoglobin at admission, each increase of 1 g/dl of haemoglobin decreased the risk of transfusion by 47 % (Table 4).
Table 4.
Results of the final logistic regression model for predicting allogenic blood transfusion (ABT) within 72 hours from admission in 1,484 patients with hip fractures
| Multivariate | Regression | Odds | 95 % Confidence Interval | P value |
|---|---|---|---|---|
| Predictor | Coefficient | Ratio | ||
| Gender (Female) | 0.4099 | 1.507 | (1.140, 1.992) | 0.0040 |
| Age | 0.0184 | 1.019 | (1.005, 1.032) | 0.0077 |
| Cephalomedullary nail (Vs. Hemiarthroplasty) | 1.6293 | 5.100 | (3.379, 7.698) | < .0001 |
| Dynamic hip screw (Vs. Hemiarthroplasty) | 0.7815 | 2.185 | (1.672, 2.854) | < .0001 |
| Haemoglobin at admission | −0.6213 | 0.537 | (0.490, 0.589) | < .0001 |
| INR at admission | −0.3720 | 0.689 | (0.515, 0.922) | 0.0122 |
INR international normalised ratio
Bold entries denote significant results at P value <0.05
A train-test model was used to assess the predictive performance of the multivariate logistic regression model. Patients were randomly assigned to either the train group (70 % of patients) or the test group (30 %). A regression model based on the five significant risk factors was applied to the training set. After applying the train model to the test set, the misclassification rate was 27 %, meaning the model correctly predicted 73 % of the cases (Table 4).
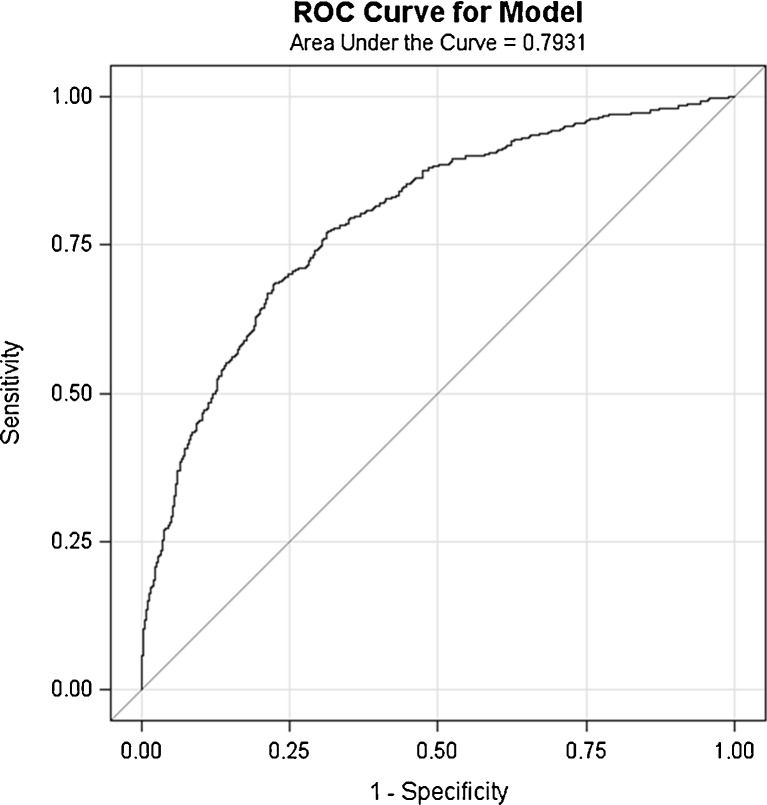
A receiver operating characteristic (ROC) curve analysis was used to evaluate the predictive performance of the logistic regression model and its ability to predict ABT transfusion within 72 hours (Fig. 1). The area under the curve (79 %) demonstrated good diagnostic performance. A predicted probability P(ABT72h) =0.42 was selected as an optimal cut-off point that best differentiates between patients who should receive ABT transfusion within 72 hours and those who should not. This cut-off point has the highest sensitivity and specificity rates; it has a false-negative rate of 21 % (i.e. the number of cases where blood was not given but the model predicted that blood is needed, n = 302) and a false positive rate of 33.8 % (i.e. the number of cases where blood was given but the model predicted that blood should not be given, n = 486).
Fig. 1.
A receiver operating characteristic (ROC) curve analysis was used to evaluate the predictive performance of logistic regression model to predict allogenic blood transfusion (ABT) transfusion within 72 hours. The area under the curve (79 %) demonstrated good diagnostic performance
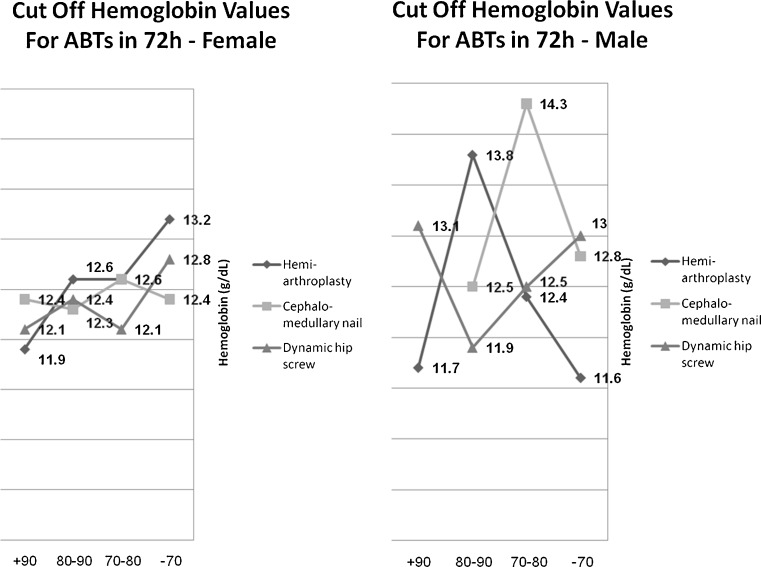
A simple clinical tool was devised to help the physician decide whether or not to order blood cross-match upon admission of a patient with a hip fracture (Fig. 2). The tool is based on four variables: gender, age, type of surgery and haemoglobin level (GASH score). Age is divided into four age groups (−70, 70–80, 80–90, 90+);, for each type of surgery, we determined the best haemoglobin cut-off point in terms of sensitivity and specificity that will predict the future need of a patient for an ABT within 72 hours. Based on ROC curves, 23 cut-off haemoglobin levels for the different groups were charted.
Fig. 2.
GASH score—A clinical tool based on four variables of patients with hip fractures: Gender, Age, Type of Surgery and Haemoglobin. The tool was devised to predict the future need of a patient for an allogenic blood transfusion (ABT) within 72 hours
Discussion
The purpose of this study was to define a method that would predict the need for an allogenic blood transfusion (ABT) in a patient admitted with a hip fracture. The importance is that this ability to predict is a first step in the management of blood transfusion in hip fracture patients [10]. Managing these transfusions has direct implications for the patients who do not always benefit from a transfusion, and has economic implications on the institutional blood bank [7]. This study focused on predictors of transfusion and algorithms that predict the need for such transfusion based on the available institutional data and its transfusion protocol. Our 30-day mortality rate was 5 % and the 90-day mortality was 9.8 % is in-line with other published survival rates [9, 11].
Clinical applications of this study include the ability to use the algorithm in a hospital computer system that monitors and gives recommendations regarding the need to order and cross-match blood for patients admitted with a hip fracture or as part of a simple medical calculator (Fig. 3). A second more practical application for the admitting physician is the GASH score (Fig. 2), which defines cutoff values for ordering a cross-match and antibody screen. At haemoglobin levels below these values, the model predicts the need for ABT and cross-match and units should therefore be ordered. Above these cut-off values, the model predicts that patients will most probably not need an ABT, and should therefore only have an ABO Rh type and antibody screen.
Fig. 3.
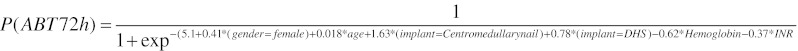
A predictive formula based on the five significant risk factors model used to predict the need for an allogenic blood transfusion (ABT) within 72 hours of admission in patients with hip fracture
This study should be interpreted in the light of its limitations. It is a retrospective study based on prospectively collected database information. It adheres to a standard institution blood transfusion protocol that varies between institutions, which makes comparisons between trials problematic. Most institutions use a transfusion trigger haemoglobin of 8–9 g/dl in healthy patients and 10 g/dl in patients with severe cardiac disease [3, 5, 12]. Due to the large nature of this trial, non-database information such as radiographs and patient charts were not reviewed. Haemoglobin at admission was used as the baseline value. Anaemia in males (Hb < 13 g/dl) was present in 51 % of these only 4 % was microcytic (MCV < 80). Anaemia in females (Hb < 12 g/dl) was prevalent in 42 %; of these, 10 % were microcytic (MCV < 80). Recent studies have suggested that on admission, haemoglobin level is falsely reassuring due to haemo-concentration, and perioperative crystalloid fluid dilution could lead to a low postoperative haemoglobin level [13]. The small percentage of patients with microcytic anaemia may indicate that the initially low haemoglobin was induced by bleeding from the fracture and not by iron deficiency.
Provision of ABT is becoming increasingly expensive, with a cost estimate of $500 for one unit of allogenic red blood cells [14]. Cross-matching two units of blood for patients with hip fractures, a common routine in many hospitals, equates to a substantial financial burden for hospitals. Due to the fatal risk involved in a mistake in identification that leads to transfusion of the wrong ABT to the wrong patient, many centres use a complicated routine when drawing two separate blood samples for a type and cross-match and for transfusing a patient with ABT, requiring a physician to take an active part in all steps of this process. For safety reasons, this cross-match expires within 72 hours, necessitating an additional sample to be drawn. By focusing on surgical procedure instead of ICD-9 diagnosis, the initial Hb drop takes into account both the blood loss due to the fracture pattern and the operative blood loss related to the surgical procedure [15]. This, we believe, is a more practical approach. The initial Haemoglobin drop by surgical procedure was 2.87 g/dl (SD 1.37) in hemiarthroplasty, 2.8 g/dl (SD 1.63) in dynamic hip screw fixation and 3.3 g/dl (SD 1.69) in proximal femoral nails. In addition, the procedure code is a billing code that is monitored and audited, contrary to the diagnosis code (ICD-9), which is not. Therefore, we feel there are fewer mistakes in the procedure code. A review of 100 patient radiographic charts was conducted and validated this. It found 100 % of the procedure codes to be accurate.
A restrictive transfusion trigger haemoglobin of 7 g/dl has recently been supported by a Cochrane database meta-analysis study that showed no higher risk of mortality, cardiac events, pulmonary oedema, cerebrovascular accident (CVA), thromboembolism, or mental confusion [3, 5]. In addition, the study showed fewer infections in the restrictive transfusion group. A recent study focused on high-risk patients admitted with a hip fracture and a cardiovascular disease. This randomised prospective study compared two groups of patients; the first was kept at a post-operative haemoglobin level of 10 g/dl and the second at 8 g/dl. The study showed no difference with regard to either survival or functional outcome at 60 days [6].
Our current cross-matching protocol is based on “a conservative” transfusion trigger haemoglobin of 9–10 g/dl. The difference between the conservative and restrictive haemoglobin levels may be viewed as a safety buffer when implementing this protocol.
The epidemiologic data and the ABT cross-matching protocol is a large scale attempt to manage cross-matching and transfusion in hip fracture patients. Studies have shown that ABT are often transfused if ready, even if it is not needed [16]. The next logical step is to change to a more restrictive transfusion trigger protocol, thus decreasing the number of ABT units used. This may benefit patient health and decrease institutional burden. Since hip fracture patients require urgent surgery, other measures of blood conservation, such as pre-donation and perioperative haemo-dilution, are not applicable.
We believe that several measures are required in order to significantly reduce blood transfusion and its associated risks and costs. First, adhering to the restrictive blood transfusion approach, proven safe on a large-scale clinical trial [6]; second, cross-match and order blood units only to those patients whose clinical characteristic make them more likely to receive a transfusion during their hospital stay. Making this paradigm shift requires more clinical trials to prove its safety and financial value.
Conclusion
Blood resources are scarce, costly, and are associated with risk. This study of 1,484 hip fracture patients treated at a single level I 1,400 bed institution, presents large scale epidemiologic data of perioperative blood loss and transfusion requirements. Using a “conservative” transfusion trigger point, a blood cross-matching protocol is suggested. Implementing such a protocol is the first step in managing allogenic blood transfusion in this group of patients, thus enabling a shift to a more restrictive transfusion trigger protocol, which studies show is safe and beneficial to the patient and the institution.
Acknowledgments
The authors would like to thank Dr. Ahuva Meilik and Mila Ozerski for their help in creating the Tel Aviv Sourasky Medical Center hip fracture registry.
Institutional review board approval
The study has been approved by the local institutional review board (0032-11-TLV) on March 2011.
Conflicts of interests and disclosure of funding
No funding was received for this paper. This paper had no pharmaceutical or other industry support. We declare that there are no apparent conflicts of interests for this paper.
International conferences
This study has been accepted for presentation at the American Academy of Orthopedic Surgeons (AAOS) annual meeting on March 19–23, 2013 in Chicago, IL
Appendix
References
- 1.Schilling PL, Hallstrom BR, Birkmeyer JD, Carpenter JE. Prioritizing perioperative quality improvement in orthopaedic surgery. J Bone Joint Surg Am. 2010;92(9):1884–1889. doi: 10.2106/JBJS.I.00735. [DOI] [PubMed] [Google Scholar]
- 2.Spahn DR, Moch H, Hofmann A, Isbister JP. Patient blood management: the pragmatic solution for the problems with blood transfusions. Anesthesiology. 2008;109(6):951–953. doi: 10.1097/ALN.0b013e31818e3d75. [DOI] [PubMed] [Google Scholar]
- 3.Carson JL, Hill S, Carless P, Hebert P, Henry D. Transfusion triggers: a systematic review of the literature. Transfus Med Rev. 2002;16(3):187–199. doi: 10.1053/tmrv.2002.33461. [DOI] [PubMed] [Google Scholar]
- 4.Khan AM, Mushtaq N, Giannakas K, Sochart DH, Andrews JG. Cross-match protocols for femoral neck fractures-finding one that can work. Ann R Coll Surg Engl. 2004;86(1):11–14. doi: 10.1308/003588404772614614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carless PA, Henry DA, Carson JL, Hebert PP, McClelland B, Ker K. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2010;6(10):CD002042. doi: 10.1002/14651858.CD002042.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453–2462. doi: 10.1056/NEJMoa1012452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foss NB, Kristensen MT, Jensen PS, Palm H, Krasheninnikoff M, Kehlet H (2009) The effects of liberal versus restrictive transfusion thresholds on ambulation after hip fracture surgery. Transfusion 49 (2);227–234. [DOI] [PubMed]
- 8.Carson JL, Altman DG, Duff A, Noveck H, Weinstein MP, Sonnenberg FA, et al. Risk of bacterial infection associated with allogeneic blood transfusion among patients undergoing hip fracture repair. Transfusion. 1999;39(7):694–700. doi: 10.1046/j.1537-2995.1999.39070694.x. [DOI] [PubMed] [Google Scholar]
- 9.Jiang HX, Majumdar SR, Dick DA, Moreau M, Raso J, Otto DD, et al. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20(3):494–500. doi: 10.1359/JBMR.041133. [DOI] [PubMed] [Google Scholar]
- 10.Dillon MF, Collins D, Rice J, Murphy PG, Nicholson P, Mac Elwaine J. Preoperative characteristics identify patients with hip fractures at risk of transfusion. Clin Orthop Relat Res. 2005;439:201–206. doi: 10.1097/01.blo.0000173253.59827.7b. [DOI] [PubMed] [Google Scholar]
- 11.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;10(331(7529)):1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young SW, Marsh DJ, Akhavani MA, Walker CG, Skinner JA. Attitudes to blood transfusion post arthroplasty surgery in the United Kingdom: a national survey. Int Orthop. 2008;32(3):325–329. doi: 10.1007/s00264-007-0330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar D, Mbako AN, Riddick A, Patil S, Williams P. On admission haemoglobin in patients with hip fracture. Injury. 2011;42(2):167–170. doi: 10.1016/j.injury.2010.07.239. [DOI] [PubMed] [Google Scholar]
- 14.Whitaker B (2011) Report of the US Department of Health and Human Services. The 2009 national blood collection and utilization survey report. Wash ington, DC: US Department of Health and Human Services, Office of the Assistant Secretary for Health, ISBN 978-1-56395-328-6
- 15.Morritt DG, Morritt AN, Kelley SP, Stone MH. Blood ordering protocol based on proposed surgical implant in fractured neck of femur patients. Ann R Coll Surg Engl. 2005;87(6):445–448. doi: 10.1308/003588405X71036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roberts M, Ahya R, Greaves M, Maffulli N. A one-centre prospective audit of peri- and postoperative blood loss and transfusion practice in patients undergoing hip or knee replacement surgery. Ann R Coll Surg Engl. 2000;82(1):44–48. [PMC free article] [PubMed] [Google Scholar]