Abstract
Purpose
The purpose of this study was to determine whether a polyaxial locking plate of the latest generation (NCB PT®, Zimmer Inc.) which can be applied both open and minimally invasively, can be used as a routine method of treatment for proximal tibia fractures.
Methods
Eighty-six patients (35 women, 51 men; mean age 51 years) were enrolled in this prospective multicentre trial. Ninety-six percent of the fractures were intra-articular (AO type B and C); 36 % were treated open and 64 % minimally invasively. Follow-up was obtained three, six and 12 months after surgery.
Results
No implant failure occurred. At 12 months, the functional result using a knee-specific score was good to excellent in 95 %, and 99 % of the fractures were radiologically healed.
Conclusion
The system is a versatile implant for proximal tibia fracture treatment. Polyaxiality and a specific locking mechanism are compatible with different fracture patterns. The minimally invasive technique effectively protects soft tissues but should not be performed at the expense of fracture reduction. Early functional results and complication rate are comparable to those in the literature.
Introduction
Surgical treatment of proximal tibia fractures is challenging due to fracture displacement and intraarticular involvement including lesions of ligaments and menisci. Frequently, severe soft tissue damage is present including the risk of compartment syndrome. Common postoperative complications include infection, malalignment and delayed- or non-union. In the long-term post-traumatic arthritis with functional impairment can occur depending on the degree of intra-articular involvement [1–3]. Proximal tibia fractures are common in elderly patients, especially in osteoporotic bone, and in younger patients are attributable to high-energy trauma [4]. Simple undisplaced fractures, representing a minority of all proximal tibia fractures, can be treated conservatively, particularly in elderly patients with concurrent comorbidities. The remaining fracture patterns should, in contrast, undergo operative treatment. Operative objectives consist of anatomical reduction, joint reconstruction and high primary stability to permit early functional treatment [5–8]. To fulfill these requirements, several options are available, with the current gold standard being open reduction and internal fixation using locking plate systems [4, 5, 9]. These devices are anatomically preshaped, have a decreased contact face paired with a low implant profile and allow for unidirectional screw placement. They can be applied using the open technique or the minimally invasive percutaneous technique. The Non Contact Bridging Proximal Tibia (NCB PT®) plate (Zimmer Inc., Warsaw, USA) represents a polyaxial head-locking device of the latest generation for both minimally invasive and open treatment of proximal tibia fractures. To our knowledge no clinical results are available as yet. The purpose of this prospective multi-centre clinical study was to describe the NCB PT, the surgical technique for the treatment of proximal tibia fractures and provide early results to investigate whether the device is suitable as a routine method of treatment.
Materials and methods
Implant
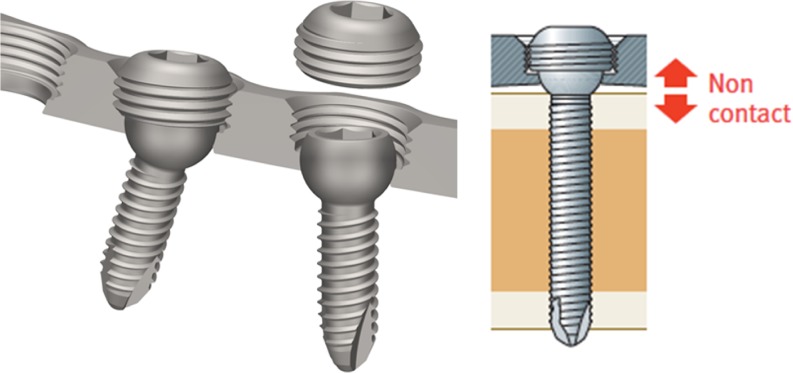
The NCB principle is in routine clinical use for proximal humerus and distal femur fractures [10–12]. The anatomically pre-shaped plate includes a 6° dorsal slope in its proximal portion and is offered with two or three proximal screw holes. Plates are available in different lengths (5, 7, 9 or 13 shaft screws). The polyaxial (30° cone perpendicular to the lower plate surface) locking mechanism differs from comparable systems. First, a conventional screw without threads in the head portion is inserted followed by a locking cap that is tightened to 6 Nm using a torque wrench (Fig. 1). This allows interfragmentary compression and indirect fracture reduction followed by locking with the same screw. During insertion the surgeon senses a degree of “tactile feedback” of screw purchase within the bone because initially the screw engages only with the bone and not with the plate. To preserve the periosteal blood supply the plate/bone compression is reduced during insertion of the locking cap by pushing the convexity of the screw head below the lower plate surface (Fig. 1). Screws are available with a self-tapping cortical or cancellous thread design. Optionally, cancellous screws are also available as a self-drilling and self-tapping cannulated version.
Fig. 1.
Polyaxial screw locking mechanism (left) and the non contact principle (right). By inserting the cap the convexity of the screw penetrates below the lower plate surface and thus reduces the contact pressure between plate and bone (images from Zimmer Inc.)
Surgical technique
Preoperative imaging includes two plain X-rays of the affected knee joint. Additional computed tomography is strongly recommended for intraarticular fractures. The patient is positioned in a supine position supporting the knee using a roll. Alternatively, the procedure can be performed in an electrically driven leg holder, as is used for arthroscopy. A tourniquet is not recommended. For reduction verification for minimally displaced AO type B or extraarticular type A fractures with suspected internal knee derangement, an arthroscopy-assisted approach may be applied. This is not recommended for type C fractures because of an increased risk of compartment syndrome or fracture dislocation due to pressure induced by the lavage. Intraoperatively, all patients receive a single second generation cephalosporin (Zinacef® 1.5 g). Depending on the fracture pattern and soft tissue condition, either the open or minimally invasive approach can be chosen
Open technique
Depending on the fracture classification, the surgical approach might vary. For type A and B fractures a lateral incision is suggested. For type C fractures, however, a straight anterolateral and an additional posterior-medial approach, if needed, is recommended [13]. An arthrotomy with release of the lateral meniscus to assess concomitant intra-articular injuries and to control fracture reduction is considered obligatory by the authors. Fracture reduction is assessed visually or with the aid of an image intensifier and fixed preliminarily using K-wires. Subsequently, the NCB PT is inserted between the anterior tibialis muscle and the periosteum. Proximally the plate should be placed as close as possible to the cartilage. The implant is temporarily fixed proximally and distally using K-wires. Taking into consideration the fracture morphology, the first shaft screw should be placed close to the proximal metaphysis to reduce the bone against the plate. Thereafter, cancellous screws are inserted proximally, parallel to the tibia plateau followed by the remaining screws to fix the shaft. A drill guide is used to prevent exceeding the 30° cone perpendicular to the plate plane. All screws should be locked using the supplied torque wrench. Optionally, cannulated cancellous screws can be precisely placed with the help of guide wires which is considered helpful in the joint area.
Minimally invasive technique
For the minimally invasive technique, a radiolucent targeting device is used for plate application (Fig. 2). The approach should start proximal to the Gerdy’s tubercle and should be extended distally for approximately 5–6 cm depending on the fracture type and severity. The same recommendations with regard to an arthrotomy apply as in the open technique. After fracture reduction and temporary fixation, the plate is inserted with the assistance of an image intensifier. Once the plate is positioned, it is temporarily fixed with proximal and distal K-wires. The order of screw insertion is the same as for the open technique. However, for screw placement in the shaft portion, stab incisions are made and a trocar system is used that is applied using the targeting device and is threaded into the plate.
Fig. 2.
Radiolucent targeting guide with attached NCB PT plate for the minimally invasive surgical technique (images from Zimmer Inc.)
Patients and follow-up
After receiving approval for the study from the Freiburger Ethics Committee International (#06T01), 86 patients treated between July 2007 and September 2010 using the NCB PT were enrolled in this prospective multi-centre study. There were five participating centres which treated between nine and 40 fractures (n = 9, 11, 12, 14 and 40). Exclusion criteria were age below 18 years, pregnancy, pathological and periprosthetic fractures, revision operations, immobility before injury and patients not willing or capable of following instructions. Informed consent was obtained from patients after radiological and clinical assessment prior to surgery. Patient demographics and quality of life before the accident were retrospectively documented using the Short Form 12 (SF12). The follow-up included a clinical and radiological assessment at three, six and 12 months post surgery. The Hospital for Special Surgery (HSS) score was assessed at each follow-up. For this score, there is a maximum of 100 points each for pain, function, instability, muscle strength, flexion deformity and range of motion [14]. On this scale 85–100 represents an excellent, 70–81 a good, 60–69 a fair and under 60 a poor result. The SF12 is a short form of the SF36 [15]. It is used for a standardised and validated assessment of subjective quality of life, and provides mental and physical dimensions. The statistical analysis was performed using SPSS V20.0 (SPSS inc., Chicago IL, USA). Data is presented mainly descriptively. For comparison of related variables, the Wilcoxon signed rank test was applied (p = 0.05).
Results
Patient demographics, fracture classification and details of the implant and surgery are presented in Tables 1, 2, 3 and 4. Seventy-one patients (83 %) completed the 12-month follow-up (mean 13.7 months). Six patients refused to participate at the 12-month follow-up, three patients moved away, three could not be reached, one had severe dementia and two patients died for reasons unrelated to the fracture. One patient had an open fracture (Gustilo Type 2). Overall, 45 patients (52 %) experienced 56 concomitant injuries: 16 meniscus lesions, 12 cruciate ligament ruptures, six medial or lateral ligament ruptures, and 22 experienced another type of concomitant injury unrelated to the knee joint. In 25 patients a synthetic bone void filler was used (ChronOS®, Mathys AG, Bettlach, Switzerland). Patients were immobilised in a Mecron splint until definitive treatment while in 20 patients an external fixator was applied including four patients with additional compartment release.
Table 1.
Patient demographics overview
| Gender | Age (years)a | Fractured side | Trauma type | AO classification | |||||
|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Left | Right | High energy | Low energy | A | B | C | |
| 35 (41 %) | 51 (59 %) | 51 (23–97) | 44 (51 %) | 42 (49 %) | 43 (50 %) | 43 (50 %) | 3 (4 %) | 45 (52 %) | 38 (44 %) |
a Mean (range)
Table 2.
Surgery figures
| Surgical techniquea | Plate typea | Duration trauma/surgery (days)b | Surgery duration (min)b | X-ray exposure time (min)b | ||
|---|---|---|---|---|---|---|
| Open | MIS | 2-hole | 3-hole | |||
| 31 (36 %) | 55 (64 %) | 49 (57 %) | 37 (43 %) | 6.2 (0–44) | 116 (43–297) | 2.5 (0.4–14.6) |
a Frequency
b Mean (range)
Table 3.
Functional outcome
| Parameter | Before accident (retrospective) | 3-month follow-up | 6-month follow-up | 12-month follow-up |
|---|---|---|---|---|
| HSSa | – | 75 (19–98) | 85 (39–100) | 87 (27–100) |
| Excellentb | – | 19 (27 %) | 45 (62 %) | 48 (69 %) |
| Goodb | – | 31 (44 %) | 17 (23 %) | 18 (26 %) |
| Fairb | – | 11 (15 %) | 8 (11 %) | 1 (1 %) |
| Poorb | – | 10 (14 %) | 3 (4 %) | 3 (4 %) |
| SF12 physicala | 52 (24–61) | 36 (20–56) | 41 (20–58) | 47 (20–60) |
| SF12 mentala | 55 (18–68) | 55 (27–68) | 56 (32–70) | 57 (39–65) |
| Range of motion (ROM)a | 115 (30–155) | 124 (60–160) | 124 (75–150) | |
| Fracture consolidationb | – | 53 % | 91 % | 99 % |
a Mean (range)
b Frequency
Table 4.
Complications overview
| General complication | Count | Revision |
|---|---|---|
| DVT | 3 | |
| Pneumonia | 1 | |
| Sub-total | 4 | 0 |
| Local complication | ||
| Haematoma | 1 | 1 |
| Superficial infection | 6 | |
| Deep infection | 2 | 2 |
| Motor deficit | 4 | |
| Sub-total | 13 | 3 |
| Other complication | ||
| Three-stage thrombosis left | 1 | 1 |
| Non-union (incl. one deep infection) | 3 | 3 |
| Restricted movement due to screw (lag screw) > pain | 1 | 1 |
| Subsidence of lateral plateau, revision plate medial | 1 | 1 |
| Fracture reposition + osteosynthesis with Palacos | 1 | 1 |
| Sub-total | 7 | 6a |
| Total | 24 in 22 patients (25.6 %) | 9 (10 %) |
a Infected non-union counted as deep infection
The upper outliers considering time to definite treatment (44 days), duration of surgery (297 minutes) and image intensifier (2.5 minutes) represent polytrauma cases, which initially had to be treated in other departments and/or underwent several procedures under the same anaesthesia (Tables 1, 2, 3 and 4). In all cases, the intra- and postoperative course was uneventful, without any implant failures. After appropriate instruction, the system was easy to use. Postoperative immobilisation in the Mecron splint was continued until wound healing was confirmed. After removal of the drain, assisted physiotherapy and passive mobilisation with the aid of a motor splint was started. During the first six weeks, 20 kg partial weight bearing was used, with flexion limited to 90° and prophylaxis for thromboembolism.
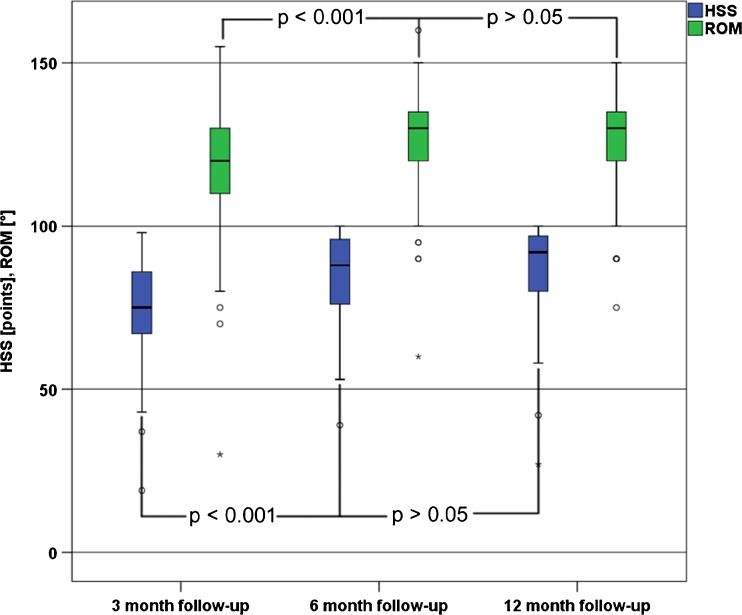
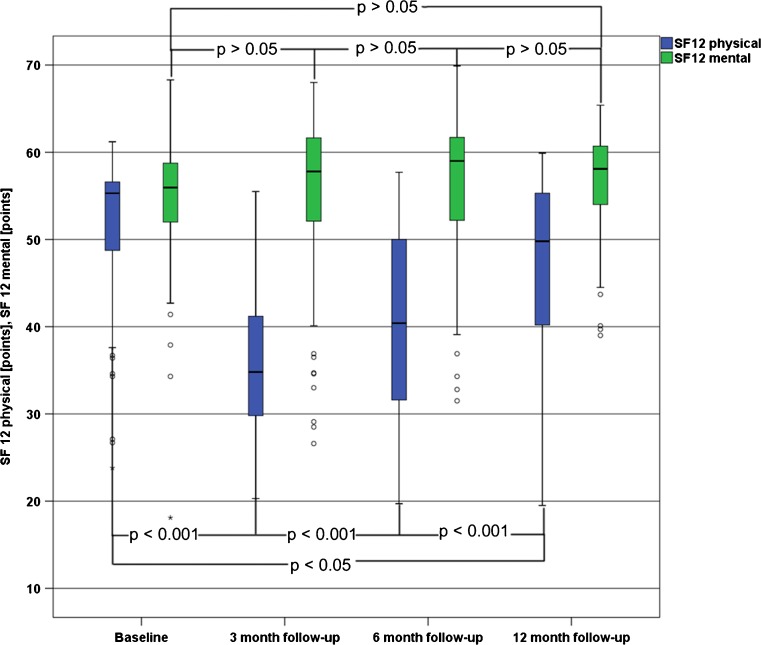
The functional results improved constantly during follow-up with partial statistical significance (Tables 1, 2, 3 and 4; Figs. 3 and 4). The mean HSS score after 12 months was 87 (27–100) corresponding to a good to excellent functional result in 95 % of the patients (Fig. 3). The mean range of motion (flexion/extension) for the affected knee joint was 124° (75–150°) after 12 months (Fig. 4). The baseline (prior to accident) SF12 reached a mean of 52 (24–61) for the physical and 55 (18–68) for the mental components with constant improvement during follow-up to 47 (20–60) and 57 (39–65), respectively, after 12 months (Fig. 4).
Fig. 3.
HSS (Hospital for Special Surgery) score and ROM (range of motion) after the 3-, 6- and 12-month follow-up
Fig. 4.
SF12 (Short Form) prior to the accident (baseline) and after the 3-, 6- and 12-month follow-up
Radiological fracture consolidation progressed from 53 % after three months to 91 % and 99 % after six and 12 months, respectively (Fig. 5). The analysis of the leg axis showed a deviation of more than five degrees in 13 patients. However, if the two outliers are removed, one with a rupture of the posterior and lateral cruciate ligaments and another that had to be surgically revised at 12 months due to arthrofibrosis, this sub group still reached a good to excellent functional outcome with a mean HSS of 88 (71–97) and a mean range of motion of 126° (105–135°).
Fig. 5.
X-ray series of an AO 31-C2 type fracture after minimally invasive treatment with an NCB PT plate. a Pre-surgery. b Post-surgery. c After 3 months. d After 6 months
The overall complication rate in our series was 26 % (n = 24 in 22 patients) including n = 5 (21 %) being unrelated to the fracture or surgery (Tables 1, 2, 3 and 4). Overall, nine patients (10 %) required surgical revision including a three-stage thrombosis in a 46-year-old patient with a type B fracture (Tables 1, 2, 3 and 4).
Discussion
Proximal tibia fractures represent approximately 10 % of all tibia fractures. With respect to age and aetiology, two subgroups can be identified. High energy fractures are the most common injury mechanism for younger patients while in the elderly, these are primarily osteoporotic fractures caused by simple falls [1, 5, 16]. Joint fractures are commonly associated with intra-articular injuries (menisci, cruciate ligaments, etc.) with a frequency of up to 57 % and with an increasing incidence as a function of the extent of joint involvement [17]. Because of this complexity and an often precarious soft tissue situation, surgical treatment is challenging and makes a uniform standardised approach difficult.
This is reflected in the large number of implants and surgical techniques described in the literature [3, 5, 18–20]. Locking plates have become the gold standard. Applied laterally as an internal fixator, especially for type B and also type A2 and A3 fractures, good results can be achieved [3, 5]. However, in cases of pure lateral splits (B1) a locking plate may be something of an over treatment since it is well-known that screws with additional buttress plating will also lead to good results. The angular stability to a certain degree compensates for the missing medial support. The minimally invasive approach is advantageous, because the surgical trauma is minimised, reducing the rate of infection up to 6 % [9, 21]. However, no compromise in fracture reduction should be accepted. There is no consensus in the literature regarding the treatment of bicondylar type C fractures. Jiang et al. compared unilateral treatment using LISS (Less Invasive Stabilisation System, Synthes) with double plating with two separate incisions (medial and lateral) [3]. No significant differences in loss of reduction, implant failure, infection rate or HSS score were shown. However, the authors described a significantly higher incidence of malposition and irritation above the plate hinge in the LISS plate group. Accordingly, they proposed that a double plating osteosynthesis represented the standard treatment for bicondylar fractures. Partenheimer et al. favour lateral application of a unilateral locking plate osteosynthesis for this type of fracture with severe soft tissue damage [9]. The authors reported an infection rate of 6 %; however, a secondary loss of reduction occurred in 15 %. Gosling et al. also used the LISS plate for the treatment of bicondylar proximal tibia fractures and reported a deep and a superficial infection rate of 2 % and 6 %, respectively. Secondary loss of reduction was observed in 14 % [21].
The available biomechanical data regarding type C fractures is inconsistent. Two separate studies comparing unilateral (LISS) and bilateral plating in bicondylar fracture models found no difference [21, 22]. However, in another biomechanical investigation significantly more subsidence of the medial plateau when using a laterally applied unilateral locking plate system was found [23]. In our investigation, 13 patients did have an initial leg axis deviation (varus/valgus) more than 5°. Of these, nine were type B and four were type C fractures. However, if the two outliers mentioned earlier are removed, this sub group still reached a good to excellent functional result with good range of motion.
The NCB PT permits an open or minimally invasive approach. The locking mechanism allows for lag and locking function with the same screw helping to address different fracture patterns (compression intra-articular, locking for enhanced primary stability and bridging techniques). In addition, polyaxiality allows flexible screw positioning, which can be helpful in periprosthetic fractures [12]. The low non-union rate found in this investigation may in part result from the minimal invasiveness of this implant with regard to minimised contact pressure between the plate and bone periosteum due to the plate’s “non-contact” feature. The functional results assessed with the HSS score correspond to a good to excellent result in 95 % of the patients and compares well with the literature [24].
In this study the minimally invasive procedure using the NCB PT effectively preserved the soft tissues resulting in two superficial and one deep infection compared to four superficial and one deep infection for the open technique. Provided that anatomical reduction is not restricted, the technique represents a soft tissue-sparing treatment option in tibia plateau fractures in which precarious soft tissues are frequently present. The results presented here including the complication rate are comparable to the literature but emphasise the challenging nature of the treatment of fractures of the proximal tibia. The limitations of our study are the relatively small sample size, short follow-up period and the lack of randomisation to a control group. Additionally, patient selection which included all types of fractures, and thus patients with a supplemental posteromedial approach, for example, may have influenced the results. However, the study design intentionally included all types of fractures to gain as much experience as possible with this new device in a first step. In the future, a larger cohort is needed with a longer follow-up period and more restrictive indications for the use of the implant to confirm the results of this study, i.e. that the NCB PT plate is a versatile method for routine care.
Acknowledgments
Conflict of interest
The institutions received financial reimbursement from Zimmer, Inc. for conducting this follow-up. None of the authors received financial reimbursement or anything of value for conducting this follow-up. The last author is an instructional lecturer for trauma courses at the Zimmer Institute™.
References
- 1.Dirschl DR, Dawson PA. Injury severity assessment in tibial plateau fractures. Clin Orthop Relat Res. 2004;423:85–92. doi: 10.1097/01.blo.0000132626.13539.4b. [DOI] [PubMed] [Google Scholar]
- 2.Rademakers MV, Kerkhoffs GM, Sierevelt IN, Raaymakers EL, Marti RK. Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma. 2007;21(1):5–10. doi: 10.1097/BOT.0b013e31802c5b51. [DOI] [PubMed] [Google Scholar]
- 3.Jiang R, Luo CF, Wang MC, Yang TY, Zeng BF. A comparative study of less invasive stabilization system (LISS) fixation and two-incision double plating for the treatment of bicondylar tibial plateau fractures. Knee. 2008;15(2):139–143. doi: 10.1016/j.knee.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Tejwani NC, Hak DJ, Finkemeier CG, Wolinsky PR. High-energy proximal tibial fractures: treatment options and decision making. Instr Course Lect. 2006;55:367–379. [PubMed] [Google Scholar]
- 5.Biggi F, Di Fabio S, D’Antimo C, Trevisani S. Tibial plateau fractures: internal fixation with locking plates and the MIPO technique. Injury. 2010;41(11):1178–1182. doi: 10.1016/j.injury.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Reynders P. Open acute segmental tibial fracture fixation using the less invasive stabilization system (LISS): study of 23 consecutive cases. Injury. 2009;40(4):449–454. doi: 10.1016/j.injury.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Boldin C, Fankhauser F, Hofer HP, Szyszkowitz R. Three-year results of proximal tibia fractures treated with the LISS. Clin Orthop Relat Res. 2006;445:222–229. doi: 10.1097/01.blo.0000203467.58431.a0. [DOI] [PubMed] [Google Scholar]
- 8.Stevens DG, Beharry R, McKee MD, Waddell JP, Schemitsch EH. The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma. 2001;15(5):312–320. doi: 10.1097/00005131-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Partenheimer A, Gosling T, Muller M, Schirmer C, Kaab M, Matschke S, Ryf C, Renner N, Wiebking U, Krettek C. Management of bicondylar fractures of the tibial plateau with unilateral fixed-angle plate fixation. Unfallchirurg. 2007;110(8):675–683. doi: 10.1007/s00113-007-1271-1. [DOI] [PubMed] [Google Scholar]
- 10.Erhardt JB, Grob K, Röderer G, Hoffmann A, Forster TN, Kuster MS. Treatment of periprosthetic femur fractures with the non-contact bridging plate: a new angular stable implant. Arch Orthop Trauma Surg. 2008;128(4):409–416. doi: 10.1007/s00402-007-0396-6. [DOI] [PubMed] [Google Scholar]
- 11.Röderer G, Erhardt J, Graf M, Kinzl L, Gebhard F. Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma. 2011;24(7):400–406. doi: 10.1097/BOT.0b013e3181ccafb3. [DOI] [PubMed] [Google Scholar]
- 12.Pressmar J, Macholz F, Merkert W, Gebhard F, Liener UC. Results and complications in the treatment of periprosthetic femur fractures with a locked plate system. Unfallchirurg. 2010;113(3):195–202. doi: 10.1007/s00113-009-1665-3. [DOI] [PubMed] [Google Scholar]
- 13.Lobenhoffer P, Gerich T, Bertram T, Lattermann C, Pohlemann T, Tscheme H. Particular posteromedial and posterolateral approaches for the treatment of tibial head fractures. Unfallchirurg. 1997;100(12):957–967. doi: 10.1007/s001130050218. [DOI] [PubMed] [Google Scholar]
- 14.Ranawat CS, Shine JJ. Duo-condylar total knee arthroplasty. Clin Orthop Relat Res. 1973;94:185–195. doi: 10.1097/00003086-197307000-00023. [DOI] [PubMed] [Google Scholar]
- 15.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):1171–1178. doi: 10.1016/S0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 16.Higgins TF, Kemper D, Klatt J. Incidence and morphology of the posteromedial fragment in bicondylar tibial plateau fractures. J Orthop Trauma. 2009;23(1):45–51. doi: 10.1097/BOT.0b013e31818f8dc1. [DOI] [PubMed] [Google Scholar]
- 17.Abdel-Hamid MZ, Chang CH, Chan YS, Lo YP, Huang JW, Hsu KY, Wang CJ. Arthroscopic evaluation of soft tissue injuries in tibial plateau fractures: retrospective analysis of 98 cases. Arthroscopy. 2006;22(6):669–675. doi: 10.1016/j.arthro.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 18.Cole PA, Zlowodzki M, Kregor PJ. Compartment pressures after submuscular fixation of proximal tibia fractures. Injury. 2003;34(Suppl 1):A43–A46. doi: 10.1016/S0020-1383(03)00257-2. [DOI] [PubMed] [Google Scholar]
- 19.Gaudinez RF, Mallik AR, Szporn M. Hybrid external fixation of comminuted tibial plateau fractures. Clin Orthop Relat Res. 1996;328:203–210. doi: 10.1097/00003086-199607000-00032. [DOI] [PubMed] [Google Scholar]
- 20.Koval KJ, Sanders R, Borrelli J, Helfet D, DiPasquale T, Mast JW. Indirect reduction and percutaneous screw fixation of displaced tibial plateau fractures. J Orthop Trauma. 1992;6(3):340–346. doi: 10.1097/00005131-199209000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res. 2005;439:207–214. doi: 10.1097/00003086-200510000-00036. [DOI] [PubMed] [Google Scholar]
- 22.Mueller KL, Karunakar MA, Frankenburg EP, Scott DS. Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop Relat Res. 2003;412:189–195. doi: 10.1097/01.blo.0000071754.41516.e9. [DOI] [PubMed] [Google Scholar]
- 23.Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: how does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma. 2007;21(5):301–306. doi: 10.1097/BOT.0b013e3180500359. [DOI] [PubMed] [Google Scholar]
- 24.Liu F, Tao R, Cao Y, Wang Y, Zhou Z, Wang H, Gu Y. The role of LISS (less invasive stabilisation system) in the treatment of peri-knee fractures. Injury. 2009;40(11):1187–1194. doi: 10.1016/j.injury.2009.03.012. [DOI] [PubMed] [Google Scholar]