Abstract
Objectives
Consistent findings show that black Americans have high rates of cardiovascular disease (CVD) and related behavioral risk factors. Despite this body of work, studies on black Americans are generally limited to the 50 U.S. states. We examined variation in CVD and related risk factors among black Americans by comparing those residing within the U.S. Virgin Islands (USVI) with those residing in the 50 U.S. states and Washington, D.C. (US 50/DC) and residing in different regions of the US 50/DC (Northeast, Midwest, South, and West).
Methods
Using data from the 2007 and 2009 Behavioral Risk Factor Surveillance System, we compared CVD and CVD risk factor prevalence in non—Hispanic black people (≥20 years of age) in the USVI and US 50/DC, examining the relative contributions of health behaviors, health insurance, and socioeconomic status (SES).
Results
Accounting for age, sex, education, health insurance, and health behaviors, US 50/DC black Americans were significantly more likely than USVI black people to report ever having a stroke and coronary heart disease, and to be hypertensive, diabetic, or obese. While there was heterogeneity by region, similar patterns emerged when comparing the USVI with different regions of the US 50/DC.
Conclusion
USVI black people have lower CVD and risk factor prevalence than US 50/DC black people. These lower rates are not explained by differences in health behaviors or SES. Understanding health in this population may provide important information on the etiology of racial/ethnic variation in health in the U.S. and elsewhere, and highlight relevant public health policies to reduce racial/ethnic group disparities.
Consistent findings show that black Americans have the highest rates of cardiovascular disease (CVD) compared with any other racial/ethnic group in the United States, seriously diminishing life expectancy and physical, social, and economic well-being throughout the life course.1,2 Despite this large and rapidly growing body of work, studies on black Americans are largely limited to the 50 U.S. states and District of Columbia (hereafter called US 50/DC). Importantly, black Americans also reside in U.S. territories, and including these populations in health studies may provide a more thorough and nuanced picture of the factors associated with health and well-being among black Americans.
Previous research has shown that examining the association between race/ethnicity and health in sites outside of the US 50/DC allows us to better understand how race and context intersect to explain health.3–5 Prior research indicates that CVD risk factor prevalence among individuals of African origin varies across regions of the U.S. and throughout the world.3–15 For example, in a well-known international collaborative study on CVD of populations in the African diaspora (collected from 1991 to 1995), large variations in the prevalence of diabetes, body mass index (BMI), and hypertension were found.6,11 Geographic variation in hypertension and stroke among black people in the US 50/DC has also been examined.9,16 However, this work has not been extended to study black Americans in U.S. territories. We sought to fill an important gap in the literature by providing a comparative study of black Americans in the US 50/DC and the U.S. Virgin Islands (USVI).
Although the health of individuals of African origin in the US 50/DC is often compared with individuals of African origin born and/or living outside of U.S. boundaries, such as Nigeria and Jamaica, little is known about the health of black Americans residing in the USVI. This comparison group might help to refine our understanding of racial disparities in CVD within the U.S. context.
The USVI is a U.S. territory located in the Caribbean, and residents are predominantly black (76.2%).17–20 Similar to the US 50/DC, many USVI black people are the descendants of slaves. However, unlike the rest of the U.S., slaves in the USVI were freed in 1848 following a slave revolt (while under the rule of Denmark), 17 years prior to emancipation in the U.S. The USVI was sold to the U.S. by Denmark in 1917.21 The USVI comprises three main islands—St. Croix, St. Thomas, and St. John—with approximately 106,405 residents according to 2010 U.S. Census data.22 Despite being U.S. citizens, the USVI population and its health have been largely overlooked in research, as well as in national policy and public health initiatives. In this study, we sought to answer two questions: (1) How does the CVD prevalence of black Americans in the US 50/DC compare with that of black Americans in the USVI?; and (2) If there are differences in CVD prevalence, what are the behavioral and sociodemographic mechanisms underlying these differences? Specifically, we examined the explanatory role of health behaviors, health insurance, and socioeconomic status (SES).
Our findings may provide some insight into the health of an understudied population that, while sharing a racial designation and national identity with black Americans in the US 50/DC, has significant cultural and historical differences. Furthermore, comparing U.S. populations that share racial characteristics but not necessarily sociocultural ones may illuminate the role of social context and place in physical health statuses and their determinants.
METHODS
The Behavioral Risk Factor Surveillance System (BRFSS) is an annual state-based, population-representative telephone health survey system of adults living in the US 50/DC, Puerto Rico, Guam, and the USVI. BRFSS data from 2007 and 2009 were combined to ensure that a sufficient number of USVI participants were included in these analyses. The Council of American Survey and Research Organizations' median response rate was 50.6% (53.3% in the USVI and ranging from 26.9%–65.4% in the U.S.) in 2007 and 52.5% (57.8% in the USVI and ranging from 37.9%–66.9% in the U.S.) in 2009.23,24 Further BRFSS details are reported elsewhere.25
Of the 62,964 US 50/DC and 3,005 USVI 2007 and 2009 self-identified non-Hispanic black BRFSS participants ≥20 years of age, 4,109 (7.0%) US 50/DC and 179 (6.0%) USVI participants were excluded for missing data on one or more health outcomes or other covariates. Another 4,661 (7.4%) US 50/DC and 243 (8.1%) USVI participants were excluded for missing data on education, insurance status, or health behaviors. These exclusions left 54,194 US 50/DC and 2,583 USVI participants for these analyses. We used 2007 and 2009 data (as opposed to 2009–2010 or 2008–2009 data) because hypertensive status, one of our CVD outcomes, was only asked every other year in the BRFSS. Because our questions focused on the health of non-Hispanic black Americans, we did not include other U.S. territories (i.e., Puerto Rico and Guam) due to small sample sizes.
We examined US 50/DC vs. USVI differences in three CVD outcomes (hypertension, stroke, and coronary heart disease [CHD]) and two CVD-related outcomes (obesity [BMI ≥30 kilograms per square meter, calculated from self-reported height and weight] and diabetes). All outcomes were self-reported. We adjusted for seven covariates: age (continuous), education (categorized as <high school, high school diploma or general equivalency diploma [GED], and >high school), current smoking, recommended physical activity (dichotomized as ≥20 minutes of vigorous activity at least three times a week or ≥30 minutes of moderate activity at least five times a week), heavy alcohol use (men: >2 drinks a day, women: >1 drink a day), recommended fruit and vegetable consumption (≥5 servings a day), and any kind of health insurance coverage.
We first evaluated the age-adjusted prevalence of all variables and tested for US 50/DC vs. USVI statistical differences using logistic regression. We then examined US 50/DC vs. USVI differences in the five health outcomes, sequentially adjusting for the seven covariates. Based on previous research showing heterogeneity in CVD outcomes among black people within the US 50/DC,9,16,26 we also assessed differences in these outcomes between black people living in different regions of the US 50/DC (Northeast, Midwest, South, and West) and in the USVI. Regions are based on the U.S. Census definitions.27 We conducted all analyses using SAS® version 9.2.28
RESULTS
USVI black people reported significantly lower levels of all CVD and CVD-related outcomes than US 50/DC black people (Table 1). For example, CHD and stroke prevalence were 1.7% and 1.6%, respectively, for USVI black people, but 3.7% and 4.0%, respectively, for US 50/DC black people. In addition, hypertension prevalence was 29.3% for USVI black people but 41.1% among US 50/DC black people. Differences were smaller but remained significant for diabetes and obesity. USVI black people were more likely than US 50/DC black people to lack a high school diploma/GED and to be without health insurance. USVI black people were more likely than US 50/DC black people to consume recommended levels of fruit and vegetables, and they were less likely to be current smokers. There were no differences in physical activity or heavy alcohol use between USVI and US 50/DC black people.
Table 1.
Age-adjusted prevalence of CVD and risk factors for non-Hispanic black adults >20 years of age among U.S. and USVI residents: Behavioral Risk Factor Surveillance System, U.S., 2007 and 2009
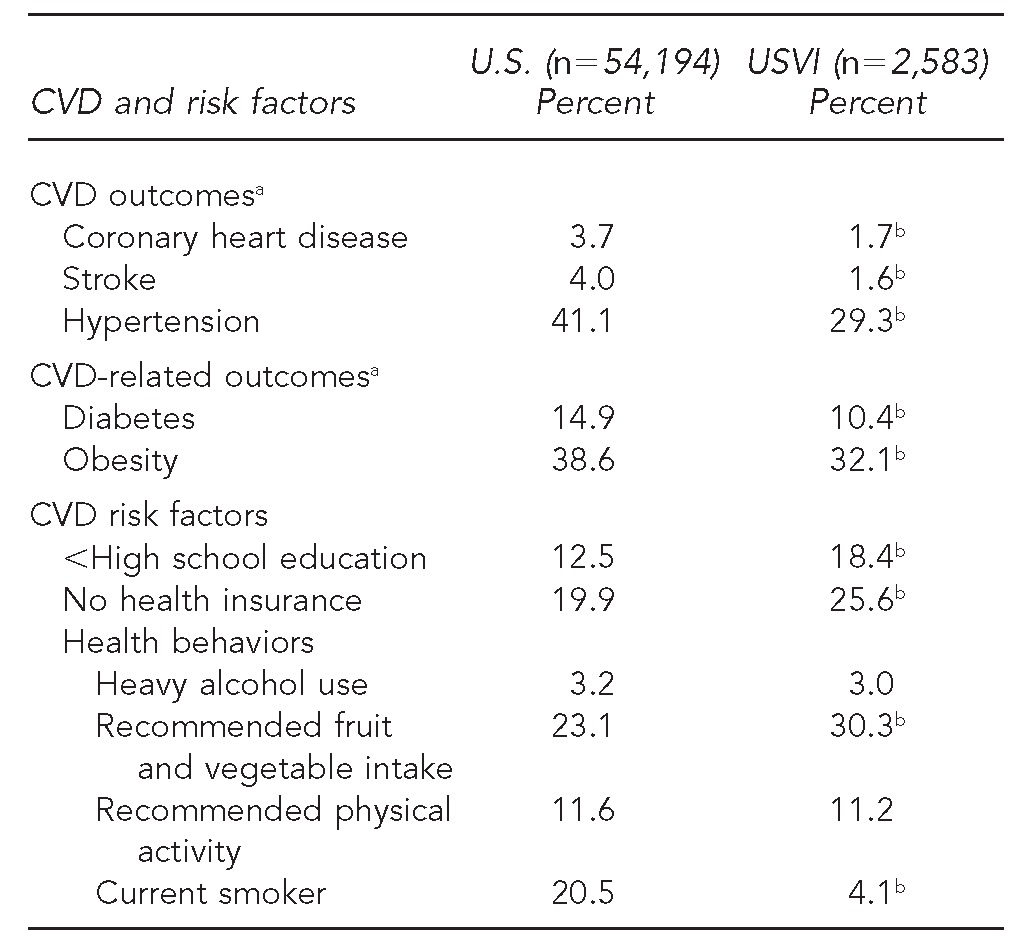
aPrevalence of all outcomes, with the exception of obesity (calculated from self-reported height and weight), were based on self-reported history of diagnosis from a doctor. Characteristics were weighted using weights provided by the Behavioral Risk Factor Surveillance System.
bp<0.05 for the U.S. vs. USVI difference based on a logistic regression model additionally adjusted for age
CVD = cardiovascular disease
USVI = U.S. Virgin Islands
Findings were similar when we compared US 50/DC black people across different regions with USVI black people (Table 2). There were significant overall differences by U.S. area of residence for all CVD and CVD-related outcomes as well as insurance status and education. One notable difference for health behaviors was that while there was no significant difference in physical activity between USVI and US 50/DC black people, we found that black people living in the West were substantially more likely to report meeting recommended levels of physical activity than black people living in the other areas of the U.S. (17.9% in the West vs. 10.8%–12.4% in the other regions and the USVI).
Table 2.
Age-adjusted prevalence of CVD and risk factors for non-Hispanic black adults >20 years of age among U.S. and USVI residents, by U.S. area of residence: Behavioral Risk Factor Surveillance System, U.S., 2007 and 2009
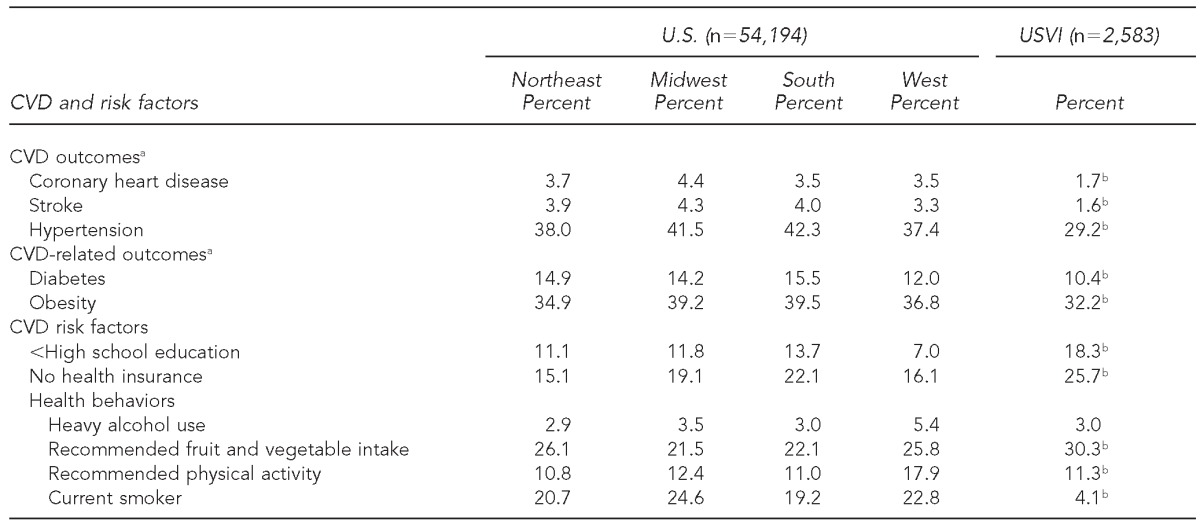
aPrevalence of all outcomes, with the exception of obesity (calculated from self-reported height and weight), were based on self-reported history of diagnosis from a doctor. Characteristics were weighted using weights provided by the Behavioral Risk Factor Surveillance System.
bp<0.05 for test of overall association between U.S. area of residence (Northeast, Midwest, South, West, and USVI) and each of the covariates, based on a logistic regression model additionally adjusted for age
CVD = cardiovascular disease
USVI = U.S. Virgin Islands
After adjusting for age, sex, and education, US 50/DC black people were 2.37 (95% confidence interval [CI] 1.63, 3.43) times as likely to have CHD compared with USVI black people (Table 3). These lower odds for USVI black people were somewhat attenuated after adjusting for health behaviors, obesity, hypertension, and diabetes (odds ratio [OR] = 1.66; 95% CI 1.14, 2.43), but the difference remained significant. As with CHD, US 50/DC black people were significantly more likely to have had a stroke compared with USVI black people (age-, sex-, and education-adjusted OR=2.81; 95% CI 1.93, 4.08), and this difference was only partially explained by adjusting for covariates (fully adjusted OR=2.13; 95% CI 1.45, 3.12). While the magnitude of the associations was weaker, USVI black people were also significantly less likely to be hypertensive, diabetic, or obese compared with US 50/DC black people after adjusting for age, sex, and education. These differences were not explained after adjusting for insurance status or health behaviors. In supplemental analysis (data not shown), we also included interactions between US 50/DC and education to determine whether socioeconomic patterning of health outcomes was different for US 50/DC compared with USVI black people, but none of these interactions were significant (p>0.05).
Table 3.
Odds ratios of CVD and CVD-related outcomes for U.S. vs. USVI (reference group) non-Hispanic black adults: Behavioral Risk Factor Surveillance System, U.S., 2007 and 2009
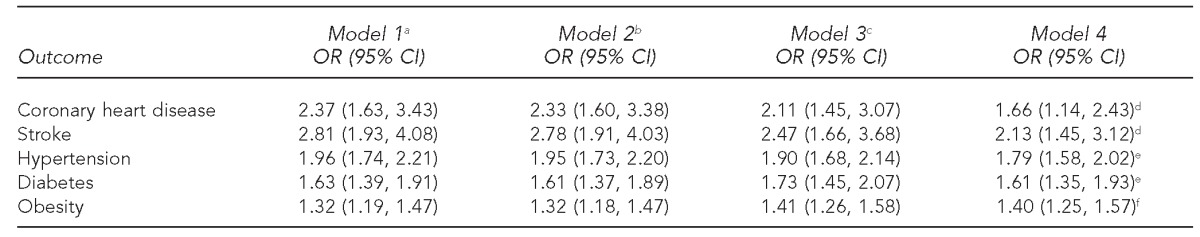
aAdjusted for age, sex, and education
bAdjusted for age, sex, education, and health insurance status
cAdjusted for age, sex, education, health insurance status, current smoking, and heavy alcohol use
dAdjusted for age, sex, education, health insurance status, current smoking, heavy alcohol use, physical activity, fruit/vegetable intake, obesity, hypertension status, and diabetes status
eAdjusted for age, sex, education, health insurance status, current smoking, heavy alcohol use, physical activity, fruit/vegetable intake, and obesity
fAdjusted for age, sex, education, health insurance status, current smoking, heavy alcohol use, physical activity, and fruit/vegetable intake
CVD = cardiovascular disease
USVI = U.S. Virgin Islands
OR = odds ratio
CI = confidence interval
While there is heterogeneity by region, US 50/DC black people in all regions were more likely to have adverse CVD and CVD-related outcomes compared with USVI black people (Table 4). In fully adjusted models, ORs for CHD comparing US 50/DC and USVI black people ranged from 1.98 (95% CI 1.14, 3.47) for black people in the West to 2.53 (95% CI 1.69, 3.77) for black people in the Midwest. Black people living in all regions of the US 50/DC were more than twice as likely to have had a stroke compared with USVI black people. Black people living in the US 50/DC were between 1.50 (West: 95% CI 1.19, 1.88) and 1.88 (South: 95% CI 1.66, 2.13) times as likely to be hypertensive and between 1.19 (Northeast: 95% CI 1.03, 1.39) and 1.45 (South: 95% CI 1.29, 1.64) times as likely to be obese. Black people living in the South, the Northeast, and the Midwest were significantly more likely to be diabetic than USVI black people. However, differences between black people living in the West and USVI black people were not significant (OR=1.29; 95% CI 0.95, 1.74).
Table 4.
Odds ratios of CVD and CVD-related outcomes for U.S. vs. USVI non-Hispanic black adults by U.S. region of residence: Behavioral Risk Factor Surveillance System, U.S., 2007 and 2009
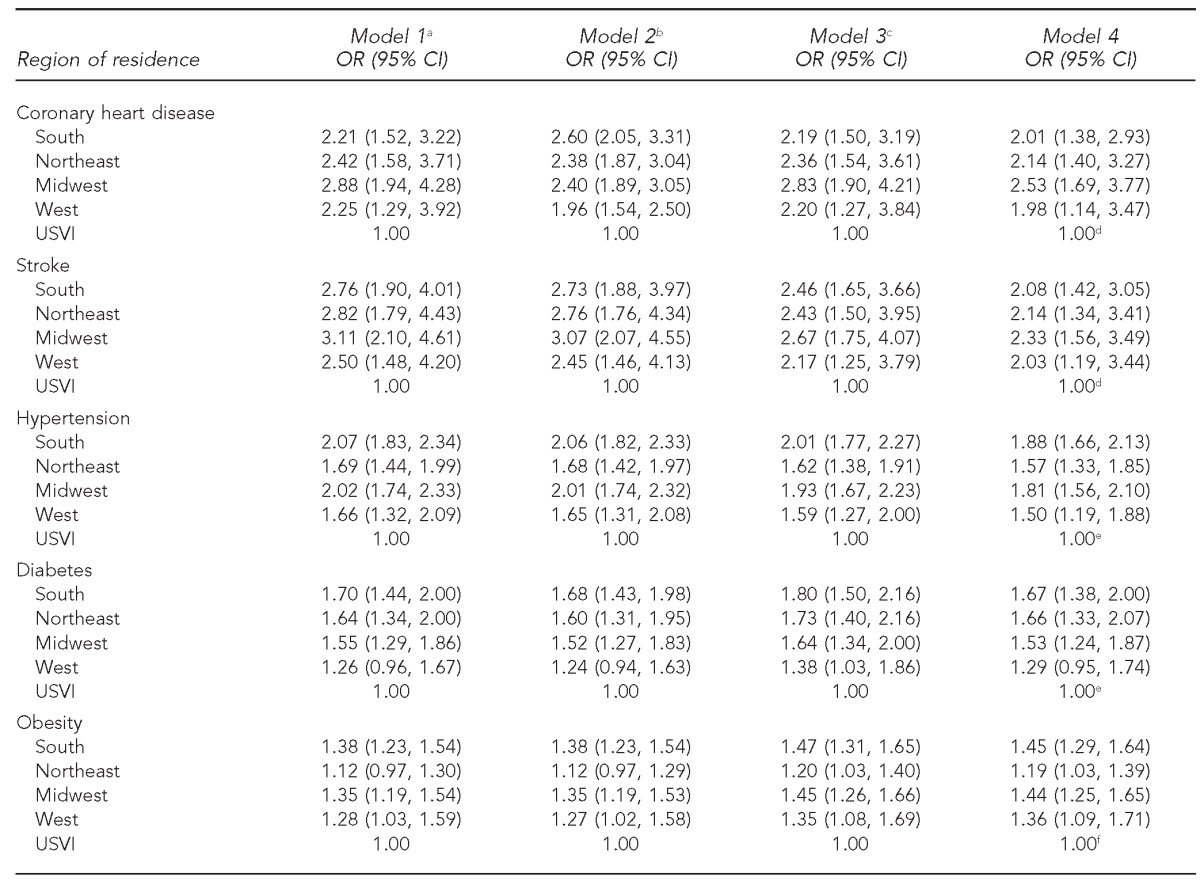
aAdjusted for age, sex, and education
bAdjusted for age, sex, education, and health insurance status
cAdjusted for age, sex, education, health insurance status, current smoking, and heavy alcohol use
dAdjusted for age, sex, education, health insurance status, current smoking, heavy alcohol use, physical activity, fruit/vegetable intake, obesity, hypertension status, and diabetes status
eAdjusted for age, sex, education, health insurance status, current smoking, heavy alcohol use, physical activity, fruit/vegetable intake, and obesity
fAdjusted for age, sex, education, health insurance status, current smoking, heavy alcohol use, physical activity, and fruit/vegetable intake
CVD = cardiovascular disease
USVI = U.S. Virgin Islands
OR = odds ratio
CI = confidence interval
DISCUSSION
The results of this study revealed that USVI black people have better cardiovascular health profiles and healthier lifestyles than their US 50/DC counterparts, despite having lower education and health insurance coverage. While there was some heterogeneity by region, similar patterns emerged when comparing the USVI with different regions of the US 50/DC. In fact, CVD differences were largely unchanged after accounting for health behaviors or SES, suggesting that there may be contextual factors, both social and physical, that influence these differences in health behaviors and CVD outcomes among black people living in the US 50/DC and the USVI.
The results support the notion that the black race is a fluid construct. This notion is a critical consideration given that being categorized as black is generally treated as a static risk factor for disease and given its persistent relation to poor health,29,30 even after considering SES, health-care coverage, and health behaviors. This trend in the literature presents significant challenges to the implementation of policies and interventions that could improve health within the diverse black American population.11,31 A growing body of research provides evidence of the contextual nature of racial-group categorization, revealing that the health of individuals of African origin, particularly CVD risk factor prevalence, varies across regions of the U.S. and throughout the world.3–14 These within-group differences among black people in different national and cultural contexts highlight the importance of sociostructural determinants of health that can most effectively be addressed at local and national policy levels to reduce racial/ethnic health disparities in the U.S. and elsewhere and to improve the health of black Americans specifically.
Given the increasingly well-documented health consequences of racial discrimination and other forms of social marginalization, such as segregation, one plausible explanation for the present findings is that the unique sociodemographic context of the USVI (i.e., majority black at 76.2%) compared with the US 50/DC (only 12.6% black people32) reduces the incidence of racialized experiences of chronic stress and stigma, which may, in turn, differentially influence health behaviors and outcomes.33–36 The majority of the USVI population is black, possibly making racial residential segregation—and its consequent social, economic, and political marginalization—less prevalent and experiences with racial discrimination less likely. Thus, these stressors associated with poor physical and mental health may be less prevalent and salient in the USVI than in the US 50/DC.35,36
It is also possible that the unique sociohistorical differences in the understanding of race and racial identity differ for USVI black people. As discussed previously, slavery in the USVI was abolished in 1848 while under Danish rule, 17 years prior to the abolition of slavery in the continental U.S.21 Therefore, USVI black people may have a longer legacy of leadership positions and some level of economic freedom than US 50/DC black people. In addition, because the Danish slave trade was abolished in the early 19th century (1803), slave health and health care became a central concern for plantation owners and colonial administrators in the Danish West Indies, who were trying to reduce the high mortality rates of slaves who could not be replaced with additional slaves from Africa.37 Due to these economic reasons, there may have been a more established infrastructure serving the basic health needs of this population of black people that was not available in the continental U.S. until considerably later.
Research comparing Caribbean-born black people currently residing in the U.S. with native-born black people also finds a health advantage among black Caribbean Americans residing in the U.S. mainland.26,38–41 Although issues of selection (e.g., healthier individuals may be more likely to migrate than less healthy individuals) might explain some of these differences, there are additional explanations that can be applied to our study. One important example is that Caribbean black people who immigrate to the U.S. may have fewer experiences with racialized stress and discrimination, which have been linked to poor health.36,42,43 As discussed previously, Caribbean islands such as the USVI have a profoundly different racial context than that of the U.S. mainland. Black people are unlikely to be the minority in any social setting. These majority black settings afford Caribbean black people the opportunities and the ability to gain cultural and social capital that is less available to native-born US 50/DC black people and is protective of health.40,43
In addition to the sociodemographic and sociohistorical contexts, the cultural and tropical climates in the USVI may facilitate health-promoting activities and avenues for social interaction and support, including outdoor activities with family, neighbors, and friends, as well as availability and affordability of locally grown fruit and vegetables for consumption (dry goods and other grocery store items, however, tend to be more expensive in the USVI than in the US 50/DC).44–46 Data limitations prohibit exploration of these potential explanations for the health advantages evidenced among USVI black people at the present time, making this an important area for future research. Disentangling these patterns will require additional data collection efforts that include obtaining detailed social, demographic, and health (including biological) information for this population.
Our work supports a growing literature on the importance of place and context for the health of black people and people of African origin in the U.S. and throughout the world.3–14 These studies highlight the fluid nature of the relationship between race and health, as well as differences in social, economic, and environmental contexts across geographical space, complicating questions regarding the nature of policies that can improve the health of Americans of African origin. Beyond the basic and necessary provision of insurance coverage and health-care access, we must consider the role of public policies that are not often directly linked to health in popular discourse. Examples of these policies include urban planning and zoning laws, which have direct implications for access to healthy foods, opportunities for physical activity, and facilitation of community social cohesion.47–51 Additional research attention and funding directed at examining variability in health, both within and between ethnic groups, will help to pinpoint relevant policies and public health strategies for reducing disparities and improving health among black people and people in other racial/ethnic minority groups.
Limitations
This study had several limitations. The telephone sampling may have underrepresented those without regular access to telephones and those who exclusively use cellular telephones. In addition, the BRFSS has a low response rate. The BRFSS data were weighted to adjust for both selection and nonresponse,52 but lower response rates may have increased the potential for bias. However, national estimates from state-aggregated BRFSS data have been shown to be comparable with estimates from the National Health Interview Survey and other surveys with higher response rates.53 Another limitation was that the data were self-reported and, thus, subject to recall and misclassification bias. However, our results for U.S. outcomes are comparable with reports using available clinical examination measures.54 Some of our estimates differ from the only USVI study conducted with measured health outcomes, possibly due to differences in the study population and design (e.g., data from that study came exclusively from the island of St. Croix and were collected between 1995 and 1999).18,19
The BRFSS does not include data on nativity, citizenship, and acculturation, which are important contextual factors for CVD and other related health outcomes55–60 that might have impacted our results. For example, black people in the US 50/DC may include foreign-born black people whose health profile might be better than native-born black people, which could likely underestimate the differences in CVD outcomes between U.S. black people and USVI black people found in this study. Future research in this area should attempt to account for these important factors. Lastly, we could not account for potential differences in lower CVD risk factor screening rates in the USVI, which might contribute to the lower prevalence observed in the present study. It should be noted that our findings do not diminish considerable health and health-care needs for the USVI population, as levels of underinsurance are higher for USVI black people than for US 50/DC black people.
CONCLUSION
We provide one of the first comparisons of health behaviors, sociodemographic factors, and CVD and related outcomes between US 50/DC and USVI non-Hispanic black people. We highlight the value of examining geographic and cultural variation in the health and well-being of the U.S. black population. Treating race as a fluid construct that is largely dependent upon context can help to illuminate how we think about race as it relates to health. Further, understanding health in the USVI black population may provide important information on the etiology of racial/ethnic variation in health and health disparities in the U.S. and the Caribbean.
Footnotes
The authors thank the Robert Wood Johnson Foundation Health – Society Scholars Program for its financial support, and the Robert Wood Johnson Senior Health Policy Program, the National Institute on Minority Health and Health Disparities, the National Institutes of Health (NIH), and the National Institute on Aging.
Kiarri Kershaw was supported by NIH grant #T32-HL-069771-07. The funding sources had no role in the study design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the article for publication. This study was exempt from Institutional Review Board approval.
REFERENCES
- 1.Kramer H, Han C, Post W, Goff D, Diez-Roux A, Cooper R, et al. Racial/ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA) Am J Hypertens. 2004;17:963–70. doi: 10.1016/j.amjhyper.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Williams RA. Cardiovascular disease in African American women: a health care disparities issue. J Natl Med Assoc. 2009;101:536–40. doi: 10.1016/s0027-9684(15)30938-x. [DOI] [PubMed] [Google Scholar]
- 3.Agyemang C, Kunst A, Bhopal R, Zaninotto P, Unwin N, Nazroo J, et al. A cross-national comparative study of blood pressure and hypertension between English and Dutch South-Asian- and African-origin populations: the role of national context. Am J Hypertens. 2010;23:639–48. doi: 10.1038/ajh.2010.39. [DOI] [PubMed] [Google Scholar]
- 4.Cooper RS, Wolf-Maier K, Luke A, Adeyemo A, Banegas JR, Forrester T, et al. An international comparative study of blood pressure in populations of European vs. African descent. BMC Med. 2005;3:2. doi: 10.1186/1741-7015-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rotimi CN, Cooper RS, Okosun IS, Olatunbosun ST, Bella AF, Wilks R, et al. Prevalence of diabetes and impaired glucose tolerance in Nigerians, Jamaicans and US blacks. Ethn Dis. 1999;9:190–200. [PubMed] [Google Scholar]
- 6.Cooper RS, Rotimi CN, Kaufman JS, Owoaje EE, Fraser H, Forrester T, et al. Prevalence of NIDDM among populations of the African diaspora. Diabetes Care. 1997;20:343–8. doi: 10.2337/diacare.20.3.343. [DOI] [PubMed] [Google Scholar]
- 7.Ferguson T, Tulloch-Reid M. Cardiovascular disease risk factors in blacks living in the Caribbean. Curr Cardio Risk Rep. 2010;4:76–82. [Google Scholar]
- 8.Gillum RF. The epidemiology of cardiovascular disease in black Americans. N Engl J Med. 1996;335:1597–9. doi: 10.1056/NEJM199611213352110. [DOI] [PubMed] [Google Scholar]
- 9.Kershaw KN, Diez Roux AV, Carnethon M, Darwin C, Goff DC, Jr, Post W, et al. Geographic variation in hypertension prevalence among blacks and whites: the Multi-Ethnic Study of Atherosclerosis. Am J Hypertens. 2010;23:46–53. doi: 10.1038/ajh.2009.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lane DA, Lip GY. Ethnic differences in hypertension and blood pressure control in the UK. QJM. 2001;94:391–6. doi: 10.1093/qjmed/94.7.391. [DOI] [PubMed] [Google Scholar]
- 11.Cooper R, Rotimi C, Ataman S, McGee D, Osotimehin B, Kadiri S, et al. The prevalence of hypertension in seven populations of West African origin. Am J Public Health. 1997;87:160–8. doi: 10.2105/ajph.87.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agyemang C, Kunst AE, Bhopal R, Anujuo K, Zaninotto P, Nazroo J, et al. Diabetes prevalence in populations of South Asian Indian and African origins: a comparison of England and the Netherlands. Epidemiology. 2011;22:563–7. doi: 10.1097/EDE.0b013e31821d1096. [DOI] [PubMed] [Google Scholar]
- 13.Boyne MS. Diabetes in the Caribbean: trouble in paradise. Insulin. 2009;4:94–105. [Google Scholar]
- 14.Durazo-Arvizu RA, Luke A, Cooper RS, Cao G, Dugas L, Adeyemo A, et al. Rapid increases in obesity in Jamaica, compared to Nigeria and the United States. BMC Public Health. 2008;8:133. doi: 10.1186/1471-2458-8-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hendriks ME, Wit FW, Roos MT, Brewster LM, Akande TM, de Beer IH, et al. Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PloS One. 2012;7:e32638. doi: 10.1371/journal.pone.0032638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howard G, Evans GW, Pearce K, Howard VJ, Bell RA, Mayer EJ, et al. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26:1153–8. doi: 10.1161/01.str.26.7.1153. [DOI] [PubMed] [Google Scholar]
- 17.Census Bureau (US). Census 2000 data for the U.S. Virgin Islands. [cited 2012 Nov 29]. Available from: URL: https://www.census.gov/census2000/usvi.html.
- 18.Tull ES, LaPorte R, Kriska A, Mark J, Hatcher AT. Glucose intolerance by race and ethnicity in the U.S. Virgin Islands. J Natl Med Assoc. 2002;94:135–42. [PMC free article] [PubMed] [Google Scholar]
- 19.Tull ES, Thurland A, LaPorte RE. Metabolic syndrome among Caribbean-born persons living in the U.S. Virgin Islands. Rev Panam Salud Publica. 2005;18:418–26. doi: 10.1590/s1020-49892005001000005. [DOI] [PubMed] [Google Scholar]
- 20.Census Bureau (US). Population and housing profile 2000: U.S. Virgin Islands. [cited 2012 Nov 29]. Available from: URL: http://www.census.gov/prod/cen2000/island/VIprofile.pdf.
- 21.Dookhan I. A history of the Virgin Islands of the United States. Kingston (Jamaica): University of the West Indies Press; 1994. [Google Scholar]
- 22.Census Bureau (US). 2010 census population counts for the U.S. Virgin Islands 2010. Washington: Census Bureau; 2011. [Google Scholar]
- 23.Centers for Disease Control and Prevention (US). 2007 Behavioral Risk Factor Surveillance System summary data quality report. 2008. [cited 2012 Nov 29]. Available from: URL: http://www.cdc.gov/brfss/technical_infodata/quality.htm.
- 24.Centers for Disease Control and Prevention (US). 2009 Behavioral Risk Factor Surveillance System summary data quality report. 2011. [cited 2012 Nov 29]. Available from: URL: http://www.cdc.gov/brfss/technical_infodata/quality.htm.
- 25.Centers for Disease Control and Prevention (US). BRFSS annual survey data and documentation. [cited 2012 Nov 9]. Available from: URL: http://www.cdc.gov/brfss/technical_infodata/surveydata.htm.
- 26.Fang J, Madhavan S, Alderman MH. The association between birthplace and mortality from cardiovascular causes among black and white residents of New York City. N Engl J Med. 1996;335:1545–51. doi: 10.1056/NEJM199611213352101. [DOI] [PubMed] [Google Scholar]
- 27.Census Bureau (US). Geographic areas reference manual. [cited 2012 Nov 29]. Available from: URL: http://www.census.gov/geo/www/garm.html.
- 28.SAS Institute Inc. SAS®: Version 9.2 for Windows. Cary (NC): SAS Institute, Inc.; 2009. [Google Scholar]
- 29.Lillie-Blanton M, Laveist T. Race/ethnicity, the social environment, and health. Soc Sci Med. 1996;43:83–91. doi: 10.1016/0277-9536(95)00337-1. [DOI] [PubMed] [Google Scholar]
- 30.Williams DR. Race and health: basic questions, emerging directions. Ann Epidemiol. 1997;7:322–33. doi: 10.1016/s1047-2797(97)00051-3. [DOI] [PubMed] [Google Scholar]
- 31.Mbanya JC, Cruickshank JK, Forrester T, Balkau B, Ngogang JY, Riste L, et al. Standardized comparison of glucose intolerance in West African-origin populations of rural and urban Cameroon, Jamaica, and Caribbean migrants to Britain. Diabetes Care. 1999;22:434–40. doi: 10.2337/diacare.22.3.434. [DOI] [PubMed] [Google Scholar]
- 32.Census Bureau (US). 2010 census summary file 1: race and Hispanic or Latino origin. Washington: Census Bureau; 2011. [Google Scholar]
- 33.Tormala TT, Deaux K. Black immigrants to the United States: confronting and constructing ethnicity and race. In: Mahalingam R, editor. Cultural psychology of immigrants. Mahwah (NJ): Lawrence Erlbaum Associates; 2006. pp. p. 131–50. [Google Scholar]
- 34.Waters MC. Explaining the comfort factor: West Indian immigrants confront American race relations. In: Lamont M, editor. The cultural territories of race: black and white boundaries. Chicago: University of Chicago Press; 1999. pp. p. 63–96. [Google Scholar]
- 35.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–8. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jensen NT. For the health of the enslaved: slaves, medicine and power in the Danish West Indies, 1803–1848. Copenhagen: Museum Tusculanum Press; 2012. [Google Scholar]
- 38.Griffith DM, Johnson JL, Zhang R, Neighbors HW, Jackson JS. Ethnicity, nativity, and the health of American blacks. J Health Care Poor Underserved. 2011;22:142–56. doi: 10.1353/hpu.2011.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nazroo J, Jackson J, Karlsen S, Torres M. The black diaspora and health inequalities in the US and England: does where you go and how you get there make a difference? Sociol Health Illn. 2007;29:811–30. doi: 10.1111/j.1467-9566.2007.01043.x. [DOI] [PubMed] [Google Scholar]
- 40.Read JG, Emerson MO. Racial context, black immigration and the U.S. black/white health disparity. Soc Forces. 2005;84:181–99. [Google Scholar]
- 41.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol. 2002;74:83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- 42.Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health: selectivity and acculturation. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical perspectives on racial and ethnic differences in health in late life: Panel on Race, Ethnicity, and Health in Later Life. Washington: National Academies Press; 2004. pp. p. 227–66. [PubMed] [Google Scholar]
- 43.Waters MC. Black identities: West Indian immigrant dreams and American realities. New York: Russell Sage Foundation; 1997. [Google Scholar]
- 44.Kamphuis CB, Giskes K, de Bruijn GJ, Wendel-Vos W, Brug J, van Lenthe FJ. Environmental determinants of fruit and vegetable consumption among adults: a systematic review. Br J Nutr. 2006;96:620–35. [PubMed] [Google Scholar]
- 45.Popkin BM, Duffey K, Gordon-Larsen P. Environmental influences on food choice, physical activity and energy balance. Physiol Behav. 2005;86:603–13. doi: 10.1016/j.physbeh.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 46.Momsen JH. Caribbean tourism and agriculture: new linkages in the global era? In: Klak T, editor. Globalization and -neoliberalism: the Caribbean context. Lanham (MD): Rowman – Littlefield Publishers, Inc.; 1998. pp. p. 115–34. [Google Scholar]
- 47.Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93:215–21. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maantay J. Zoning, equity, and public health. Am J Public Health. 2001;91:1033–41. doi: 10.2105/ajph.91.7.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Massey DS, Denton NA. American apartheid: segregation and the making of the underclass. Cambridge (MA): Harvard University Press; 1993. [Google Scholar]
- 50.Odoms-Young AM, Zenk S, Mason M. Measuring food availability and access in African-American communities: implications for intervention and policy. Am J Prev Med. 2009;36(4 Suppl):S145–50. doi: 10.1016/j.amepre.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 51.Osypuk TL, Acevedo-Garcia D. Beyond individual neighborhoods: a geography of opportunity perspective for understanding racial/ethnic health disparities. Health Place. 2010;16:1113–23. doi: 10.1016/j.healthplace.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Centers for Disease Control and Prevention (US). Vital signs: current cigarette smoking among adults aged ≥18 years—United States, 2005–2010. Atlanta: CDC; 2011. [Google Scholar]
- 53.Nelson DE, Holtzman D, Bolen J, Stanwyck CA, Mack KA. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS) Soz Praventivmed. 2001;46(Suppl 1):S3–42. [PubMed] [Google Scholar]
- 54.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 55.Gorman BK, Read JG, Krueger PM. Gender, acculturation, and health among Mexican Americans. J Health Soc Behav. 2010;51:440–57. doi: 10.1177/0022146510386792. [DOI] [PubMed] [Google Scholar]
- 56.Kaushal N. Adversities of acculturation? Prevalence of obesity among immigrants. Health Econ. 2009;18:291–303. doi: 10.1002/hec.1368. [DOI] [PubMed] [Google Scholar]
- 57.Koya DL, Egede LE. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007;22:841–6. doi: 10.1007/s11606-007-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lopez-Gonzalez L, Aravena VC, Hummer RA. Immigrant acculturation, gender and health behavior: a research note. Soc Forces. 2005;84:581–93. [Google Scholar]
- 59.Pabon-Nau LP, Cohen A, Meigs JB, Grant RW. Hypertension and diabetes prevalence among U.S. Hispanics by country of origin: the National Health Interview Survey 2000–2005. J Gen Intern Med. 2010;25:847–52. doi: 10.1007/s11606-010-1335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Padilla R, Steiner JF, Havranek EP, Beaty B, Davidson AJ, Bull S. A comparison of different measures of acculturation with cardiovascular risk factors in Latinos with hypertension. J Immigr Minor Health. 2011;13:284–92. doi: 10.1007/s10903-010-9434-5. [DOI] [PubMed] [Google Scholar]


