Abstract
Objectives
We determined the efficacy of pediatric-based preschool vision screening, as knowledge of vision screening effectiveness in primary care pediatrics is incomplete.
Methods
Pediatricians and staff at nine primary care pediatric practices were trained in vision screening, and practices screened children aged 3–5 years from May 2007 through July 2008. Children failing or considered untestable were referred for pediatric ophthalmology examinations. We determined rates of testability, failure, referral, and ophthalmologic examination completion, as well as positive predictive values (PPVs) of screening failure and untestability. We also surveyed practices to assess the ease and accuracy of preschool vision screening.
Results
Of 2,933 children screened, 93 (3.2%) failed the vision screening and 349 (11.9%) were untestable. Untestability was highest (27.1%) among 3-year-olds. The PPV for failing any aspect of the vision screening was 66.7%; for children aged 3, 4, and 5 years, the PPVs for failing were 30.0%, 77.8%, and 87.5%, respectively. However, only 38.7% of children who failed the vision screening received ophthalmologic examinations, despite multiple follow-up attempts. Pediatricians rated the ease and accuracy of screening 3-year-old children lower than for screening older children.
Conclusions
Visual acuity-based screening had good PPV for vision loss for 4- and 5-year-old children but was less successful for 3-year-olds. Rates of referral and ophthalmologic examination completion were low, especially among children from low-income families.
Amblyopia, the primary target condition of preschool vision screening, is caused by deficient visual stimulation of an eye during the years of visual development. Untreated amblyopia leads to permanent vision loss.1 The estimated prevalence of amblyopia in the United States is 1%–4%.2–4 For detection of amblyopia or its risk factors, the U.S. Preventive Services Task Force recommends vision screening of all children at least once between the ages of 3 and 5 years.5 Vision screening is recommended as a component of the well-child examination by the American Academy of Pediatrics (AAP), the American Academy of Ophthalmology, and the American Association for Pediatric Ophthalmology and Strabismus (AAPOS).6–8 The AAP states that visual acuity screening should begin at 3 years of age as part of routine pediatric care. In addition, children aged 3–5 years should undergo assessment of the external eye appearance, ocular alignment and motility, pupils, and ocular media clarity.7
In the U.S., however, many children fail to receive timely screening examinations.9,10 Only 21%–36% of children younger than 6 years of age have undergone vision screening or comprehensive examinations.9,11 In a recent survey, 35% of pediatricians reported routinely screening 3-year-old children using eye charts, and 73% reported screening 4-year-old children.12 Barriers to primary care vision screening may include deficiencies in reimbursement, incomplete primary care education in screening, and limitations of the testing techniques themselves.12,13 Problems have been reported with primary care screening related to screening penetrance, testability, and referral.13,14 Evidence for the real-world effectiveness of preschool vision screening in the primary care setting is lacking.15 Therefore, the Children's Eye Foundation (CEF), the charitable foundation of AAPOS, established its See by Three program with the goal of significantly reducing amblyopia in young children. The CEF requested proposals for two projects to assess the effectiveness of preschool vision screening in primary care pediatric practice.
METHODS
The CEF selected Nemours Children's Clinic in Jacksonville, Florida, in collaboration with Vision Is Priceless Council (a vision-screening charity also based in Jacksonville), to conduct one of the projects. The second project was based at the University of West Virginia. We describe the Jacksonville project. The screening was performed from May 2007 through July 2008.
Patients
The target population was children aged 3–5 years receiving well-child examinations. Two private pediatric practices (PPs) agreed to participate, with 14 pediatricians practicing in three locations. Six Duval County Health Department (HD) primary care pediatric clinics, with an additional 14 pediatricians in six locations, also participated. The inclusion of PPs and HD clinics created a study population that was representative of the socioeconomic strata of the county's preschool population. Compared with the PP population, HD children were more frequently insured by Medicaid, of a lower socioeconomic status, and African American. For individual patients, however, sex, age, race/ethnicity, and primary language were not recorded. Practices agreed to screen all children arriving for annual well-child visits.
Screening tests
Of greatest interest was the effectiveness of visual acuity screening. Selected physical examination tests performed by pediatricians were also included in the study. The screening procedures were based on AAP guidelines, but with some intentional differences, which are noted hereafter. The study used the Early Treatment of Diabetic Retinopathy Study (ETDRS)-style LEA Symbols eye chart (Model 255001, Good-Lite Co., Elgin, Illinois) with illuminated cabinet, chart mask, penlights, and near-fixation target toys. Monocular linear visual acuity was measured at 10 feet. An adhesive eye patch was used to occlude the opposite eye (ATL, Menomonee Falls, Wisconsin). For children refusing the patch, we used Children's Fun Occluder Frames (Good-Lite Co.).
The critical line for vision screening referral was 20/40. To pass the visual acuity screening, children were required to identify four of the five symbols on the critical line with each eye. This criterion differed because five figures were present on the chart's critical line rather than six figures, as described in the AAP guidelines.17 Children who were uncooperative or did not comprehend the test were categorized as untestable. Pediatricians also performed the red reflex test and the corneal light reflex test. Optionally, the Bruckner test was allowed as a substitute for the red reflex and corneal light reflex tests. Additionally, a cover test for near fixation was to be performed for each child. The AAP guidelines specify distance cover testing, but near cover testing was more adaptable to the various primary care settings. Random dot E stereo, another AAP-recommended test, was not included because of reported poor results in the preschool age group and the additional anticipated testing time.16,17
To assure consistent implementation of the study, several steps were taken. First, a research study coordinator (SC) and a nurse experienced in vision screening trained the physicians and staff at all sites. The clinic staff received face-to-face training on study design, methodology for visual acuity screening, pass/fail/untestable criteria, data documentation, and management of children categorized as failures or untestable. Second, the SC supplied the clinics with equipment and supervised its installation. And third, the pediatricians received training in vision screening techniques using verbal training and an educational compact disc (Pediatric Vision Screening®, Nemours).
Eligible children were initially enrolled in the study for nine months. To reach study enrollment goals, screening at the three PP sites was extended for an additional five months. Because of higher enrollment rates at the PP sites, extension of screening in those sites was considered the most efficient method to reach study enrollment goals.
Screening failures and untestability
All screening failures and untestable children were referred for comprehensive ophthalmologic examinations. Although AAP guidelines recommend rescreening untestable children before referral, we were interested in the significance of a single instance of untestability. We did not assess the effectiveness of a rescreening strategy for untestable children.
De-identified data were collected on children passing the screening examination. Parents of children who failed or were untestable signed a Health Insurance Portability and Accountability Act (also known as HIPAA) release of information form before contact information was sent to the SC. The children who failed or were untestable were referred for comprehensive ophthalmologic examination. Pediatricians were requested to direct all referrals to the study center's pediatric ophthalmology practice for examination by one of four pediatric ophthalmologists. The SC called each parent to facilitate ophthalmology appointment scheduling. In cases of failure to show up for examination, at least three calls were made to the parents to reschedule the appointment. In addition, the primary care pediatrics office was notified. At the ophthalmology visit, informed consent was obtained and the patient was enrolled into the study.
For children referred to but not completing an ophthalmologic examination, attempts were made by the SC to determine the reason for not receiving the examination by contacting the families. All participating pediatric ophthalmologists were educated on the study design and instructed in the examination protocol. The ophthalmologists were aware that each study participant had either failed a screening examination or was considered untestable, but no additional screening details were revealed. The ophthalmologic examination elements recorded were initial visual acuity, cover test, Bruckner test, pupils, external eye examination, slit lamp examination, cycloplegic refraction using cyclopentolate 1% ophthalmic solution, best-corrected visual acuity, and funduscopic examination. Distance linear visual acuity was measured with LEA Symbols using the SmartSystem® II PC-Plus Visual Acuity System (M&S Technologies, Inc., Park Ridge, Illinois). Results of the ophthalmology examination were recorded on standardized data forms (Scantron, Eagan, Minnesota).
Vision screening process assessment by participating practices
At the conclusion of the study, representatives of each primary care site were surveyed to obtain their assessment of different aspects of the vision screening process for each of the ages screened.
Statistical analysis
Screening results were compared with the results of the ophthalmologic examination.18 All categorical variables were summarized using frequencies and percentages. We compared the quality of two or more proportions (percentages) using Chi-square statistics with appropriate degrees of freedom. We compared the frequency and rates for pass, fail, and untestable by age groups and practice types using Chi-square analysis. We calculated positive predictive values (PPVs) with 95% confidence intervals (CIs) to compare pediatric vision screening results with ophthalmology examination results. Analyses were two-tailed, with 0.05 considered significant. We used SPSS® Statistics version 17.0.19
RESULTS
Well-child examinations and screening
Across the participating sites, there were 5,896 well-child visits by children 3, 4, or 5 years of age, and 2,970 (50.4%) visits included documented vision screening. Of the 2,970 children screened, 880 (29.6%) were 3-year-olds, 1,175 (39.6%) were 4-year-olds, and 912 (30.7%) were 5-year-olds. Ages were not recorded for three screened children. The proportion screened (screening/total visits) did not differ significantly among the age groups. The higher number of 4-year-olds screened was due to a higher number of well-child visits for that age group. There were no known cases of the same child being screened more than once, but de-identification of screening passes disallowed for the assessment of all records.
Visual acuity and other screening
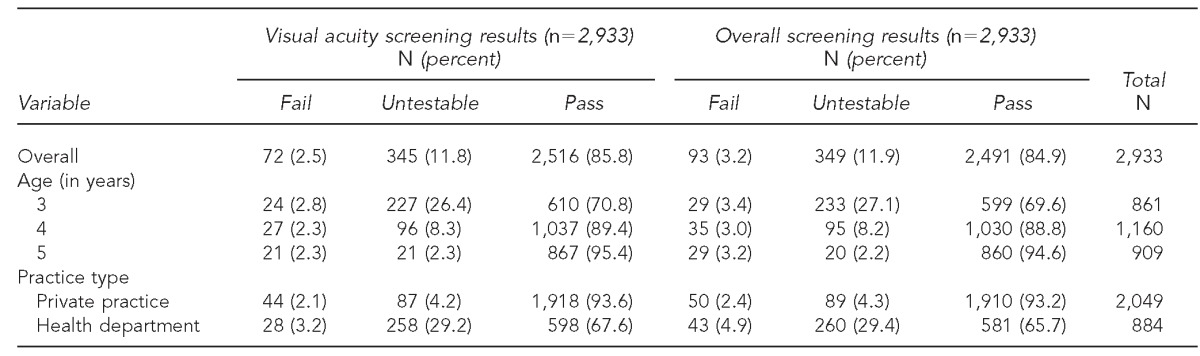
Of the 2,970 children screened, 37 (1.2%) were noted at screening to be developmentally delayed, autistic, or both. Twenty-nine of the 37 (78.4%) children with developmental delays or autism were screened at HD sites. Developmentally delayed or autistic children were excluded from further analysis. After exclusions, PP screening accounted for 62% of 861 3-year-olds, 70% of 1,160 4-year-olds, and 77% of 909 5-year-olds screened. Overall, 72 of 2,933 (2.5%) children failed visual acuity screening and 345 (11.8%) were untestable (Table 1).
Table 1.
Primary care pediatric vision screening results and frequencies for children aged 3–5 years at private practice and health department sites: Jacksonville, Florida, May 2007–July 2008
Twenty-five of 2,933 (0.8%) children failed vision screening components of the pediatrician's physical examination. Of the 25 failures on physical examination, four children also failed visual acuity screening, 15 passed visual acuity screening, and six were untestable by visual acuity (data not shown).
Overall screening
The overall screening failure rate consisted of children failing either the visual acuity screening or a physical examination test. Ninety-three of 2,933 (3.2%) children failed at least one screening component, and 349 (11.9%) were untestable (Table 1). Failure rates among the age groups did not differ significantly (p=0.852). The untestability rate was higher among 3-year-olds (27.1%, 233/861) than among 4-year-olds (8.2%, 95/1,160) and 5-year-olds (2.2%, 20/909; p<0.001). The failure rates of the two practice types differed, with a failure rate of 2.4% among PP sites (50/2,049) and 4.9% among HD sites (43/884) (p<0.001). Similarly, the untestability rates of the two practice types differed, with an untestability rate of 4.3% at PP sites (89/2,049) and 29.4% at HD sites (260/884) (p<0.001). Among the six HD sites, the untestability rates ranged from 13.5%–42.1%.
Referrals for ophthalmologic examinations
Referral of children varied among practice sites and ages (Table 2). Of those who failed screening, 76 of 93 patients (81.7%) were referred for ophthalmologic examinations. Among screening failures, fewer 3-year-olds were referred (65.5%, 19/29) than 4-year-olds (91.4%, 32/35) and 5-year-olds (86.2%, 25/29) (p=0.021).
Table 2.
Primary care pediatric vision screening referral rates and frequencies for children aged 3–5 years at private practice and health department sites: Jacksonville, Florida, May 2007–July 2008
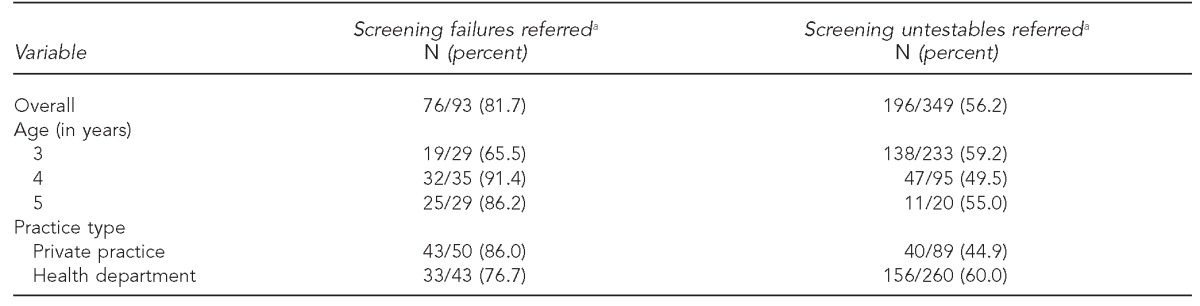
aThe denominator represents the corresponding number of screening failures or untestables.
Of 321 total referrals, 285 (88.8%) records indicated the practice to which the child was referred, and the study center's ophthalmology practice was indicated in 263 (92.3%) of these referrals. Efforts were unsuccessful in determining whether any of the children referred elsewhere received ophthalmologic examinations (data not shown).
Ophthalmologic examination completion
Of children referred to the study center, 97 of 263 (36.9%) received examinations (Table 3). Of children referred but failing to appear for ophthalmologic examinations, the majority of the families did not respond to phone calls and letters. Of the 15 parents who were successfully contacted, seven considered an examination unnecessary, four indicated insurance problems, one indicated transportation problems, and three reported plans to be examined elsewhere (data not shown).
Table 3.
Primary care pediatric vision screening rates of ophthalmologic examination completion for children aged 3–5 years referred to the study center at private practice and health department sites: Jacksonville, Florida, May 2007–July 2008
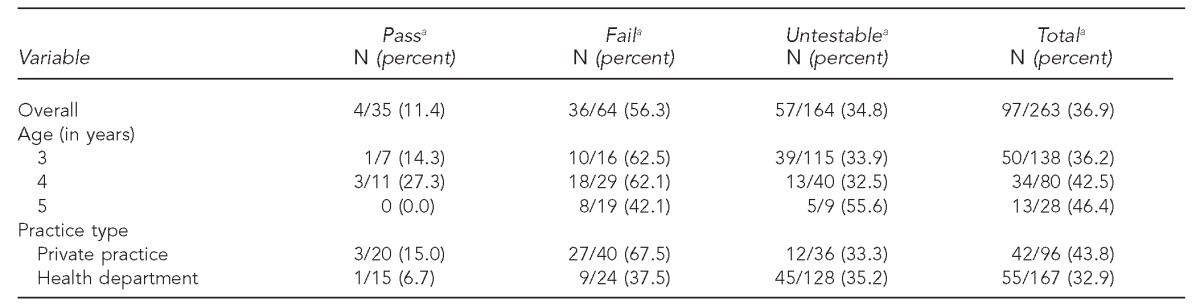
aThe denominator represents the corresponding number of referrals to the study center.
Dropout from screening to receiving an ophthalmologic examination
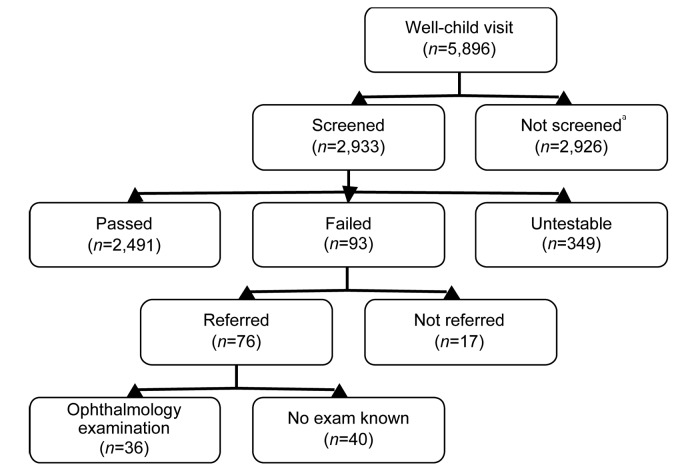
Combining failure-to-refer and failure-to-appear reasons for not receiving an ophthalmologic examination, 36 (38.7%) of the 93 children who failed vision screening received examinations at the study center (Figure). Of screening failures, 34.9% of 3-year-olds, 51.0% of 4-year-olds, and 27.0% of 5-year-olds appeared for ophthalmologic examinations. More screening failures from PPs (54.0%) underwent ophthalmologic examinations than from HD sites (20.9%) (p=0.002) (data not shown).
Ophthalmologic examination results and screening reliability
A screening failure was a true positive result if, on ophthalmologic examination, the child failed one of the AAPOS amblyogenic factors or if distance visual acuity measured 20/50 or worse for either eye.18 The overall PPV of screening failures compared with ophthalmologic examinations was 66.7% (95% CI 48.9, 80.9) (Table 4). By age groups, the PPV was 30.0% for 3-year-old failures, 77.8% for 4-year-olds, and 87.5% for 5-year-olds. The PPV of visual acuity screening failure was 64.5% (95% CI 45.4, 80.2). The overall PPV of untestability for an ophthalmologic abnormality was 28.1% (95% CI 17.4, 41.8). For children who failed screening for reasons other than visual acuity, seven received ophthalmologic examinations. Six of the seven (85.7%, 95% CI 42.0, 99.0) were found to have an abnormality. Four of the seven had passed visual acuity screening and, of those, three of four had an abnormality (data not shown).
Table 4.
Primary care pediatric vision screening PPVs of screening failure and untestability for children aged 3–5 years at private practice and health department sites: Jacksonville, Florida, May 2007–July 2008
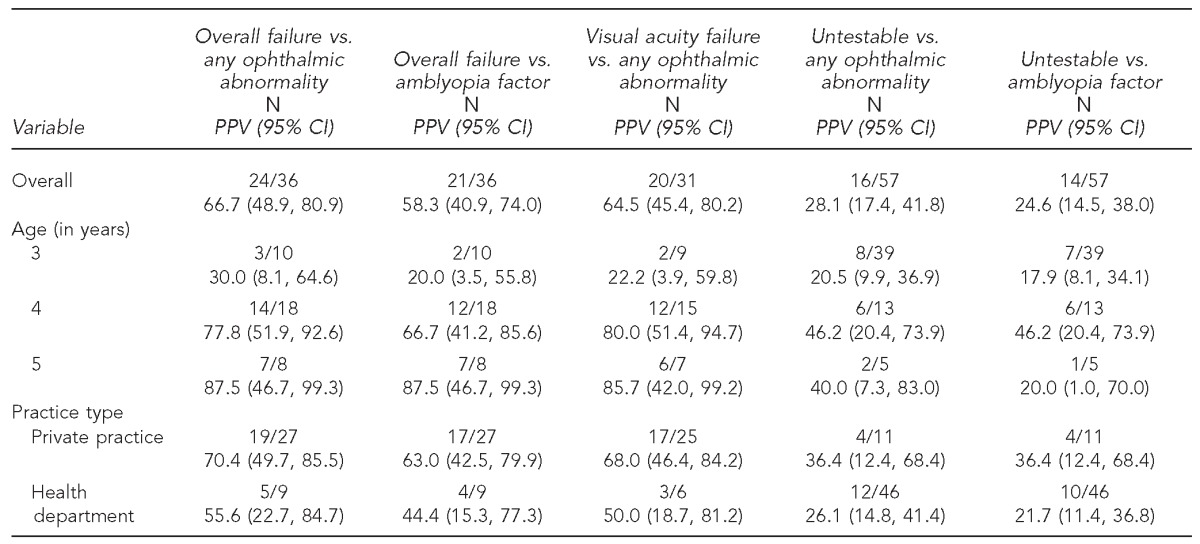
PPV = positive predictive value
CI = confidence interval
For 50 of 58 children (86.2%) who were untestable by screening, visual acuity was obtainable at the ophthalmologic examination. Forty-two of the 58 children had normal visual acuity, eight failed, and eight were again untestable (data not shown).
Vision screening process assessment by practice
Questionnaire responses for the primary care sites are listed in Table 5. The ease and accuracy of preschool screening as well as the likelihood of continuing to screen was rated higher for 4- and 5-year-old children than for 3-year-olds. Of barriers to screening, the time required to test was rated as the most significant barrier.
Table 5.
Post-study assessment of the vision screening process for children aged 3–5 years by primary care practices participating in a vision screening study: Jacksonville, Florida, May 2007–July 2008
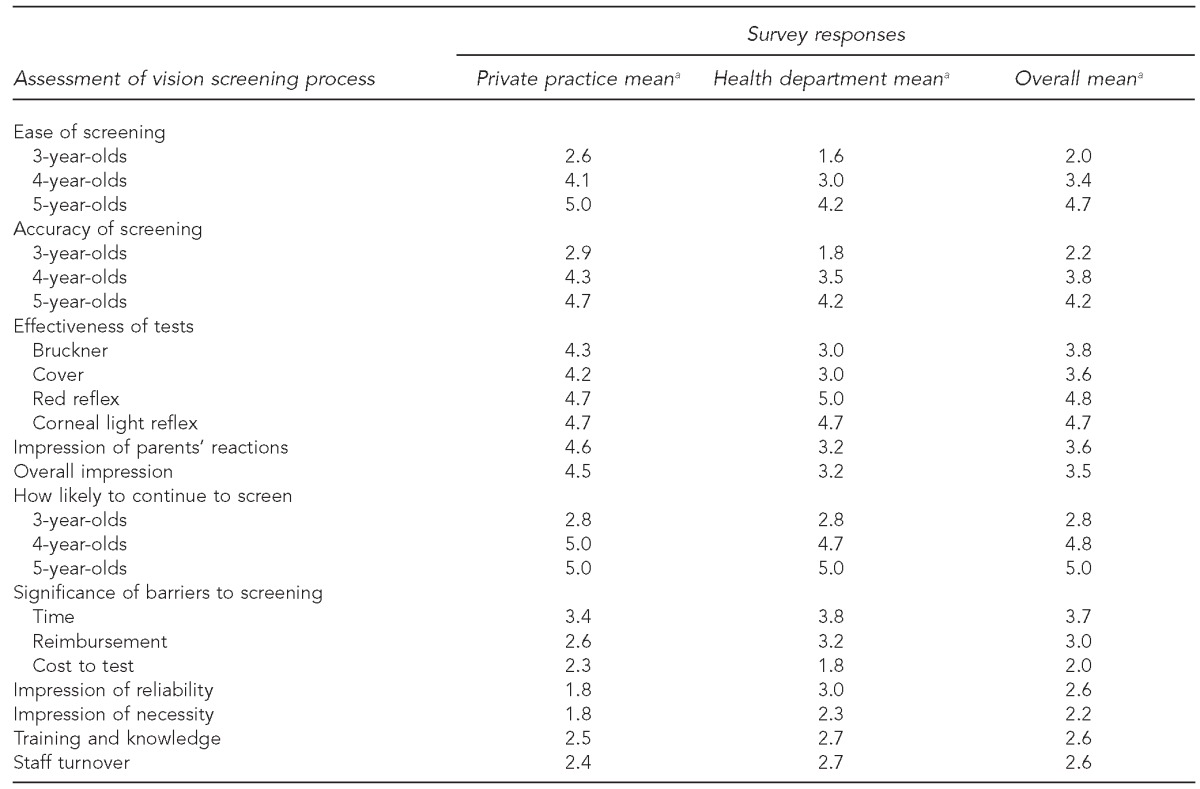
aAll responses were on a five-point Likert scale, where 5 = very easy, accurate, effective, important, or likely; and 1 = not at all easy, accurate, effective, important, or likely.
DISCUSSION
This study indicates that pediatric vision screening may be effective, particularly after the age of 48 months. For children aged 4 and 5 years, untestability was only 5% and the PPV of screening failure was nearly 80%. These results compare favorably with results from other primary care screening studies.13,14,20,21 Screening results for 3-year-olds and overall rates of ophthalmology examination completion, however, were poor. Visual acuity screening results among 3-year-olds specifically indicates problems with the use of eye charts for young preschoolers in the primary care setting. The low referral and ophthalmology examination completion rates, however, indicate additional problems related to the acceptance of preschool vision screening by pediatricians, office staff, and parents.
The 77.8% and 87.5% PPV of screening failure among 4- and 5-year-olds, respectively, is consistent with previous studies and supports the potential effectiveness of visual acuity screening in more mature preschoolers. The PPV of the combined screening battery was higher than for visual acuity alone, supporting the added value of screening techniques performed by the pediatrician rather than relying on visual acuity screening alone. The 30.0% PPV for screening failure among 3-year-olds is of great concern. The CI for this PPV was particularly wide because relatively few 3-year-olds completed an ophthalmologic examination, but this result in combination with the high untestability rate, the low referral rate, and the results of the questionnaire indicate significant dysfunction in primary care visual acuity screening of 3-year-old children. For those younger than 4 years of age, objective techniques such as photoscreening are emerging as preferred alternatives to visual acuity testing.22,23
This study found a high percentage of 3-year-old children to be untestable. Among individual sites, untestability rates varied greatly and were as high as 42.1%, suggesting variability in successful training or acceptance of screening. Although there are limited comparative data, other studies show similarly high untestability rates among 3-year-olds in the primary care setting.13,14 Interestingly, our study found that for 86.0% of the children referred because of untestability, visual acuity was measurable in the ophthalmology office. It is therefore unlikely that higher untestability rates at the HD sites occurred because of differences between the HD and PP pediatric populations. Other studies have also found much higher testability rates when visual acuity screening is performed by pediatric eye care providers.24,25 Reasons for lower testability rates in PP offices may include lack of screening experience, staff turnover, time constraints, and distractions in the office setting.12,26–28
The 24.6% PPV of untestability for the presence of an amblyogenic factor is significantly higher than the prevalence of amblyopia in the general preschool population and also higher than the 16.0% of low-income preschoolers with refractive errors found in a recent study.29 Abnormal ocular conditions may be twice as prevalent among untestable preschoolers compared with those who pass a screening test.30 The high rates of untestability and of treatable conditions in the untestable group combined to threaten screening sensitivity. Prompt rescreening or referral should be considered for children who are considered untestable. Rescreening may reduce the rate of referral, but would necessitate additional visits to the pediatrician. This study did not attempt to determine whether rescreening or immediate referral is the better option.
Limitations
This study was subject to several limitations. For one, the study sites failed to screen all eligible children. Documentation of screening events was dependent on completion of data forms, however, and it is likely that some screening was performed but not recorded, resulting in an underestimation of screening rates. Secondly, many children who failed screening were not referred for ophthalmologic examinations. The particularly low rate of referral among 3-year-olds is consistent with previous studies that report lower acceptance among pediatricians of eye chart screening in 3-year-olds.12,26,27 It is also consistent with the lack of confidence in 3-year-old screening indicated by this study's survey responses.
Thirdly, of screening failures referred, many children did not appear for ophthalmologic examinations. Kemper et al. found that minority and low-income families were less likely to follow up, consistent with the lower rate we found among children referred by the HD sites.31
Fourth, the study results related to screening rates, untestability, underreferral, and failure to show for ophthalmologic examinations were suboptimal, perhaps due to incomplete acceptance of screening among staff at certain primary care sites and among some parents. Confirmatory examination and treatment are necessary following a screening failure. For children screened in day care centers, many parents do not follow through to obtain comprehensive eye examinations.32 Unfortunately, this study demonstrated a similar problem with confirmatory examination completion when screening was performed in the pediatrics office. Lack of follow-up underscores the need for the health-care system to reduce barriers to referral to ophthalmology for preschool children. Additionally, primary care practices must actively track children who have failed vision screening to assure adequate follow-up. In this study, no additional educational materials other than those routinely provided by the practices were supplied to parents of children who had failed screening. Perhaps increased education of parents on the meaning of a failed vision screening may increase the proportion seeking appropriate follow-up.
CONCLUSIONS
This study supports the use of visual acuity screening among 4- and 5-year-old children in PPs. For children aged 4 years and older, a visual acuity screening failure indicates a high probability of having a vision disorder and necessitates referral for a comprehensive ophthalmologic examination. This study also generally supports the use of certain additional screening tests for children aged 3–5 years. The study calls into question the effectiveness of eye chart visual acuity screening of 3-year-olds. Visual acuity screening of 3-year-olds, compared with 4- and 5-year-olds, resulted in higher untestability rates, lower referral rates of screening failures, and lower PPVs. The AAP vision screening policy may require modification, recommending that visual acuity screening be initiated at 4 years of age. Substitution of photoscreening for visual acuity screening may be a better option for children younger than 4 years of age. Low primary care screening rates and inadequate rates of referral and completion of an ophthalmologic examination indicate that a different screening device will not in itself result in optimal detection and treatment of vision loss. Rather, improvements are needed in the entire process of preschool vision screening in the primary care setting, from screening to definitive diagnosis and, ultimately, to successful treatment.
Figure.
Flow of children aged 3–5 years arriving for well-child visits at primary care pediatric practice study sites, from well-child visit to completion of an ophthalmology examination: Jacksonville, Florida, May 2007–July 2008
aAn additional 37 children were screened, for a total of 2,970. However, they were excluded from further analysis because of development delay or autism.
Acknowledgments
This study was funded by the Children's Eye Foundation, with additional funding from Nemours. The authors acknowledge the efforts of the Children's Eye Foundation See by Three Committee and thank its chair, Denise Chamblee, MD. The authors also thank Mary Warde, a research coordinator, and Marjorie Rothstein, a nurse educator, for assistance with this study; the physicians and staff of the Duval County Health Department, Jacksonville Pediatric Associates, The Carithers Pediatric Group, and the Nemours Division of Ophthalmology; the staff of Vision Is Priceless Council; and Nemours Biomedical Research.
Nemours and the University of Florida and Florida Department of Health Institutional Review Boards approved the study protocol.
REFERENCES
- 1.Simons K, Preslan M. Natural history of amblyopia untreated owing to lack of compliance. Br J Ophthalmol. 1999;83:582–7. doi: 10.1136/bjo.83.5.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson JR, Woodruff G, Hiscox FA, Strong N, Minshull C. The incidence and prevalence of amblyopia detected in childhood. Public Health. 1991;105:455–62. doi: 10.1016/s0033-3506(05)80616-x. [DOI] [PubMed] [Google Scholar]
- 3.Multi-ethnic Pediatric Eye Disease Study Group. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months: the Multi-ethnic Pediatric Eye Disease Study. Ophthalmology. 2008;115:1229–36. doi: 10.1016/j.ophtha.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Friedman DS, Repka MX, Katz J, Giordano L, Ibironke J, Hawse P, et al. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months: the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116:2128–34. doi: 10.1016/j.ophtha.2009.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Preventive Services Task Force. Vision screening for children 1 to 5 years of age: U.S Preventive Services Task Force recommendation statement. Pediatrics. 2011;127:340–6. doi: 10.1542/peds.2010-3177. [DOI] [PubMed] [Google Scholar]
- 6.Coffield AB, Maciosek MV, McGinnis JM, Harris JR, Caldwell MB, Teutsch SM, et al. Priorities among recommended clinical preventive services. Am J Prev Med. 2001;21:1–9. doi: 10.1016/s0749-3797(01)00308-7. [DOI] [PubMed] [Google Scholar]
- 7.Committee on Practice and Ambulatory Medicine; Section on Ophthalmology. American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians. Pediatrics. 2003;111(4 Pt 1):902–7. [PubMed] [Google Scholar]
- 8.American Academy of Family Physicians. Summary of recommendations for clinical preventive services. Leawood (KS): AAFP; 2006, updated in 2012. [Google Scholar]
- 9.Visual impairment and use of eye-care services and protective eyewear among children—United States, 2002. MMWR Morb Mortal Wkly Rep. 2005;54(17):425–9. [PubMed] [Google Scholar]
- 10.Wu C, Hunter DG. Amblyopia: diagnostic and therapeutic options. Am J Ophthalmol. 2006;141:175–84. doi: 10.1016/j.ajo.2005.07.060. [DOI] [PubMed] [Google Scholar]
- 11.Ehrlich MI, Reinecke RD, Simons K. Preschool vision screening for amblyopia and strabismus. Programs, methods, guidelines, 1983. Surv Ophthalmol. 1983;28:145–63. doi: 10.1016/0039-6257(83)90092-9. [DOI] [PubMed] [Google Scholar]
- 12.Kemper AR, Clark SJ. Preschool vision screening in pediatric practices. Clin Pediatr (Phila) 2006;45:263–6. doi: 10.1177/000992280604500309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartmann EE, Bradford GE, Chaplin PK, Johnson T, Kemper AR, Kim S, et al. ; PUPVS Panel for the American Academy of Pediatrics. Project Universal Preschool Vision Screening: a demonstration project. Pediatrics. 2006;117:e226–37. doi: 10.1542/peds.2004-2809. [DOI] [PubMed] [Google Scholar]
- 14.Kemper AR, Helfrich A, Talbot J, Patel N, Crews JE. Improving the rate of preschool vision screening: an interrupted time-series analysis. Pediatrics. 2011;128:e1279–84. doi: 10.1542/peds.2010-3679. [DOI] [PubMed] [Google Scholar]
- 15.Mathers M, Keyes M, Wright M. A review of the evidence on the effectiveness of children's vision screening. Child Care Health Dev. 2010;36:756–80. doi: 10.1111/j.1365-2214.2010.01109.x. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt P, Maguire M, Dobson V, Quinn G, Ciner E, Cyert L, et al. Vision in Preschoolers Study Group. Comparison of preschool vision screening tests as administered by licensed eye care professionals in the Vision In Preschoolers Study. Ophthalmology. 2004;111:637–50. doi: 10.1016/j.ophtha.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 17.Hope C, Maslin K. Random dot stereogram E in vision screening of children. Aust N Z J Ophthalmol. 1990;18:319–24. doi: 10.1111/j.1442-9071.1990.tb00627.x. [DOI] [PubMed] [Google Scholar]
- 18.Donahue SP, Arnold RW, Ruben JB, AAPOS Vision Screening Committee Preschool vision screening: what should we be detecting and how should we report it? Uniform guidelines for reporting results of preschool vision screening studies. J AAPOS. 2003;7:314–6. doi: 10.1016/s1091-8531(03)00182-4. [DOI] [PubMed] [Google Scholar]
- 19.SPSS, Inc. SPSS Statistics: Version 17.0. Chicago: SPSS, Inc.; 2008. [Google Scholar]
- 20.Salcido AA, Bradley J, Donahue SP. Predictive value of photoscreening and traditional screening of preschool children. J AAPOS. 2005;9:114–20. doi: 10.1016/j.jaapos.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Arnold RW, Stange CA, Ryan C. The compared predictive value of Bröockner, acuity, and strabismus from pediatric referrals. Am Orthop J. 2006;56:15–21. [Google Scholar]
- 22.Kirk VG, Clausen MM, Armitage MD, Arnold RW. Preverbal photoscreening for amblyogenic factors and outcomes in amblyopia treatment: early objective screening and visual acuities. Arch Ophthalmol. 2008;126:489–92. doi: 10.1001/archopht.126.4.489. [DOI] [PubMed] [Google Scholar]
- 23.Arthur BW, Riyaz R, Rodriguez S, Wong J. Field testing of the plusoptiX S04 photoscreener. J AAPOS. 2009;13:51–7. doi: 10.1016/j.jaapos.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 24.Vision in Preschoolers Study Group. Preschool vision screening tests administered by nurse screeners compared with lay screeners in the vision in preschoolers study. Invest Ophthalmol Vis Sci. 2005;46:2639–48. doi: 10.1167/iovs.05-0141. [DOI] [PubMed] [Google Scholar]
- 25.Cotter SA, Tarczy-Hornoch K, Wang Y, Azen SP, Dilauro A, Borchert M, et al. ; Multi-Ethnic Pediatric Eye Disease Study Group. Visual acuity testability in African-American and Hispanic children: the Multi-ethnic Pediatric Eye Disease Study. Am J Ophthalmol. 2007;144:663–7. doi: 10.1016/j.ajo.2007.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wasserman RC, Croft CA, Brotherton SE. Preschool vision screening in pediatric practice: a study from the Pediatric Research in Office Settings (PROS) Network. American Academy of Pediatrics [published erratum appears in Pediatrics 1992;90:1001] Pediatrics. 1992;89(5 Pt 1):834–8. [PubMed] [Google Scholar]
- 27.Wall TC, Marsh-Tootle W, Evans HH, Fargason CA, Ashworth CS, Hardin JM. Compliance with vision-screening guidelines among a national sample of pediatricians. Ambul Pediatr. 2002;2:449–55. doi: 10.1367/1539-4409(2002)002<0449:cwvsga>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 28.Hered RW, Rothstein M. Preschool vision screening frequency after an office-based training session for primary care staff. Pediatrics. 2003;112(1 Pt 1):e17–21. doi: 10.1542/peds.112.1.e17. [DOI] [PubMed] [Google Scholar]
- 29.Brody BL, Roch-Levecq AC, Klonoff-Cohen HS, Brown SI. Refractive errors in low-income preschoolers. Ophthalmic Epidemiol. 2007;14:223–9. doi: 10.1080/01658100701486822. [DOI] [PubMed] [Google Scholar]
- 30.Maguire MG, Vision in Preschoolers Study Group. Children unable to perform screening tests in vision in preschoolers study: proportion with ocular conditions and impact on measures of test accuracy. Invest Ophthalmol Vis Sci. 2007;48:83–7. doi: 10.1167/iovs.06-0384. [DOI] [PubMed] [Google Scholar]
- 31.Kemper AR, Uren RL, Clark SJ. Barriers to follow-up eye care after preschool vision screening in the primary care setting: findings from a pilot study. J AAPOS. 2006;10:476–8. doi: 10.1016/j.jaapos.2006.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Preslan MW, Novak A. Baltimore vision screening project. Ophthalmology. 1996;103:105–9. doi: 10.1016/s0161-6420(96)30753-7. [DOI] [PubMed] [Google Scholar]