Abstract
The routes of henipavirus transmission between hosts are poorly understood. The purpose of this study was to measure the persistence of henipaviruses under various environmental conditions and thereby gain an insight into likely mechanisms of transmission. Henipaviruses survived for more than four days at 22°C in pH-neutral fruit bat urine but were sensitive to higher temperatures and pH changes. On mango flesh, survival time varied depending on temperature and fruit pH, ranging from two hours to more than two days. Desiccation of viruses substantially reduced survival time to less than two hours. The sensitivity of henipaviruses to pH, temperature and desiccation indicates a need for close contact between hosts for transmission to occur, although under ideal conditions henipaviruses can persist for extended periods facilitating vehicle-borne transmission.
Keywords: Paramyxovirus, Hendra virus, Nipah virus, Henipavirus, Virology, Dessication, Urine, Fruit, Temperature, Transmission
Introduction
Hendra virus (HeV) and Nipah virus (NiV), currently the sole members of the genus Henipavirus, family Paramyxoviridae, are recently emerged zoonotic viruses causing encephalitic and respiratory illness in humans and livestock. Fruit bats of the genus Pteropus are the probable wildlife reservoir for both viruses. HeV is restricted to Australia and of the seven outbreaks to date all have involved infection of horses from unidentified sources, with subsequent direct transmission to humans on three occasions (8, 9, 20). NiV outbreaks have occurred in Malaysia, Singapore, India and Bangladesh following various chains of transmission including intermediate host species (3), human-to-human transmission (2, 13), possible bat-to-human transmission (10) and vehicle-borne transmission (16).
In most cases, the route of transmission from bats to subsequent hosts has not been identified. The most likely route of HeV transmission to horses is through the ingestion of grass or partially eaten fruit contaminated with bat urine, saliva or other fluids. The coincidence of HeV outbreaks with birthing seasons of Australian fruit bat species (5) and the isolation of HeV from the uterine fluid and aborted foetus of a wild grey-headed fruit bat (P. poliocephalus, (7)) indicate that this may be a significant route of HeV infection for horses. We have recently demonstrated vertical transmission of NiV in experimentally infected cats further supporting this route as potentially an important natural route of tranmission (19).
Two NiV outbreaks show a reasonably clear chain of transmission from bats to humans: Malaysia in 1998–99 and Tangail, Bangladesh in 2005. During the Malaysian outbreak, 265 people were infected, primarily through contact with infected pigs (22). The pigs were probably infected by P. vampyrus bats that fed on fruit trees adjacent to the pig farms, either through direct exposure to urine or via saliva-contaminated partially eaten fruit dropped into the pigsties (4). In the Tangail outbreak, NiV transmission to humans apparently occurred via date palm sap (15, 16). The sap may have been contaminated by urine, faeces or saliva from P. giganteus which are known to feed on the sap during harvesting.
Little is known about the transmission routes for the remaining NiV outbreaks, although preliminary analysis of the 2007 outbreaks (Kushtia, Bangladesh and Nadia, India) suggests likely human to human transmission (S. Luby, Pers. Comm.). The absence of identifiable intermediate hosts may be evidence of bat-to-human transmission. In at least three outbreaks human-to-human transmission is likely to have occurred (2, 6, 12, 13), however the mode of transmission is uncertain.
A greater understanding of potential henipavirus modes of transmission may clarify the events that lead to viral spillover into new species and assist in controlling or averting outbreaks. Knowledge of virus survival in the environment is also critical in controlling human-to-human and nosocomial transmission.
The purpose of this study was to define the ability of henipaviruses to survive under a range of environmental conditions and thereby gain an understanding of the likely mechanisms of viral transmission between hosts. While we intended to mimic the natural conditions relevant to bat viral transmission as closely and accurately as possible, certain limitations on fruit selection due to seasonal availability and limitations inherent in the procurement of bat urine and saliva necessitated some generalizations.
Materials and Methods
Viruses and titrations
HeV was isolated in Vero cells from the lung of a horse infected in the Brisbane outbreak in October 1994 (21) and was passaged five times in Vero cells followed by triple plaque purification and a further five passages in Vero cells (11). NiV was isolated in Vero cells from the brain of a human fatally infected in the 1998–99 Malaysian outbreak and was passaged three times in Vero cells then double plaque purified and passaged a further three times in Vero cells (24).
For titrations, serial ten-fold dilutions of samples were made in EMEM and 25µl transferred to five wells of a 96-well microtitre plate. Vero E6 cells in EMEM containing 10% fetal calf serum were added (2 × 104 cells/well). Plates were incubated at 37°C for 5–7 days and wells displaying cytopathic effect were scored as infected. Virus titre was calculated using the Reed-Meunch method (23) and the limit of detection was 126 TCID50/ml virus. All work with live virus was carried out under Biosafety Level 4 (BSL-4) conditions.
Effect of pH on virus survival
The pH of 0.01M PBS was adjusted using NaOH or HCl to provide stock buffers in the range, pH 1 to 13. Viruses were diluted 1:100 in each pH buffer (n=3) then incubated at 22°C for 60 min and samples collected for titration in Vero cells.
Effect of desiccation on virus survival
Viruses were desiccated by spreading 10 µl onto a polystyrene dish and air drying at 22°C for 15 min (n=3). Dishes were stored at 22°C or 37°C and virus recovered at intervals by resuspension in 250 µl PBS followed by titration in Vero cells.
Virus survival in urine
HeV was diluted in a pooled urine sample from an Australian species (P. alecto) with a pH of 7. NiV was diluted in a pooled urine sample from a Malaysian species (P. vampyrus). The P. vampyrus urine was used either at its natural pH of 2 or following adjustment to pH 7 with NaOH to compensate for pH effects on virus survival. Viruses (n=3) were incubated at 22°C or 37°C for up to 96 hrs and samples collected at intervals for titration in Vero cells. Both P. alecto and P. vampyrus had been extensively studied in recent years (Halpin and Middleton, unpublished data) enabling the procurement of sufficient quantities of urine for these experiments but unfortunately, urine from additional species was not available at the time of testing.
Virus survival in fruit juice and flesh
Cubes of mango flesh (1cm3) were placed in tubes, 10 µl of virus (n=3) pipetted onto the surface and samples stored at 22°C or 37°C for up to 48 hrs. Virus was recovered by vortexing the sample in 0.5 ml PBS and the supernatant was titrated in Vero cells.
Virus survival was measured in juices from mango, lychee and pawpaw. As mentioned previously, the seasonal availability of fruits in Australia relevant to henipavirus infections prevented a wider range of fruits specific to the tropical locations of Nipah virus outbreaks from being tested in this study. Juices were extracted and passed through a 0.2-µm filter. Viruses were diluted in juice (n=3) and incubated at 22°C or 37°C for up to 96 hrs. Samples were collected at intervals for titration in Vero cells
Calculation of half-lives
Virus survival data was collated and half-life was calculated using non-linear regression analysis based a one phase exponential decay model using GraphPad Prism software (GraphPad Software, San Diego, CA USA).
Results
Effect of pH on virus survival
Both HeV and NiV exhibit an extremely broad tolerance to extremes of pH with viable virus recovered after a 60 min incubation in solutions ranging from pH 3 to pH 11 for NiV and pH 4 to pH 11 for HeV (Figure 1).
Figure 1.
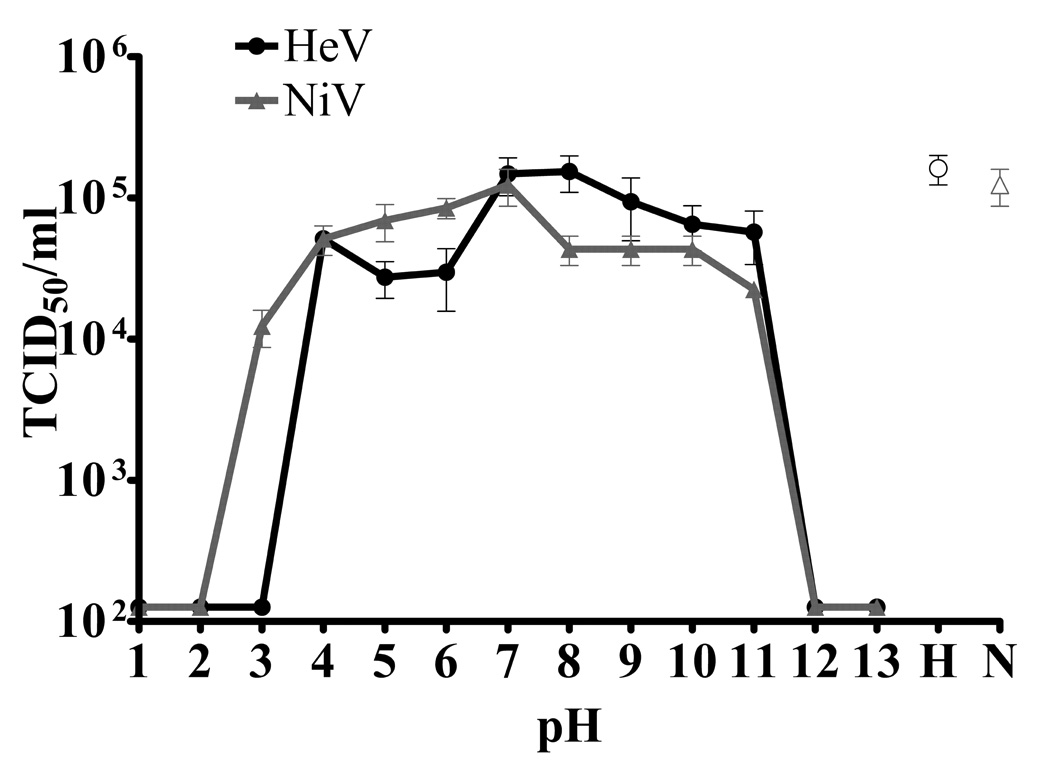
Henipavirus survival for 60 minutes at 22°C in PBS at various pH. H/N - open symbols represent control virus (Hendra and Nipah virus respectively) samples kept in growth medium (EMEM) for an equivalent period. Data are presented as Mean ± S.E.
Effect of desiccation on virus survival
Henipaviruses were rapidly inactivated by desiccation at both 22°C and 37°C. Both viruses survived for less than 15 min at 37°C (Figure 2) while HeV decreased by more than 3 logs within 30 min (half-life of 1.2 minutes) and NiV decreased by more than 2 logs within 60 min (half-life of 1.45 min) at 22°C. Limitations inherent in virus recovery under BSL4 biocontainment provided logistical restrictions to a much broader evaluation of viral dessication on other surfaces. Non-porous polystyrene media was chosen to enable maximum virus recovery, and thus represents a “best case” scenario for recovery from viral dessication.
Figure 2.
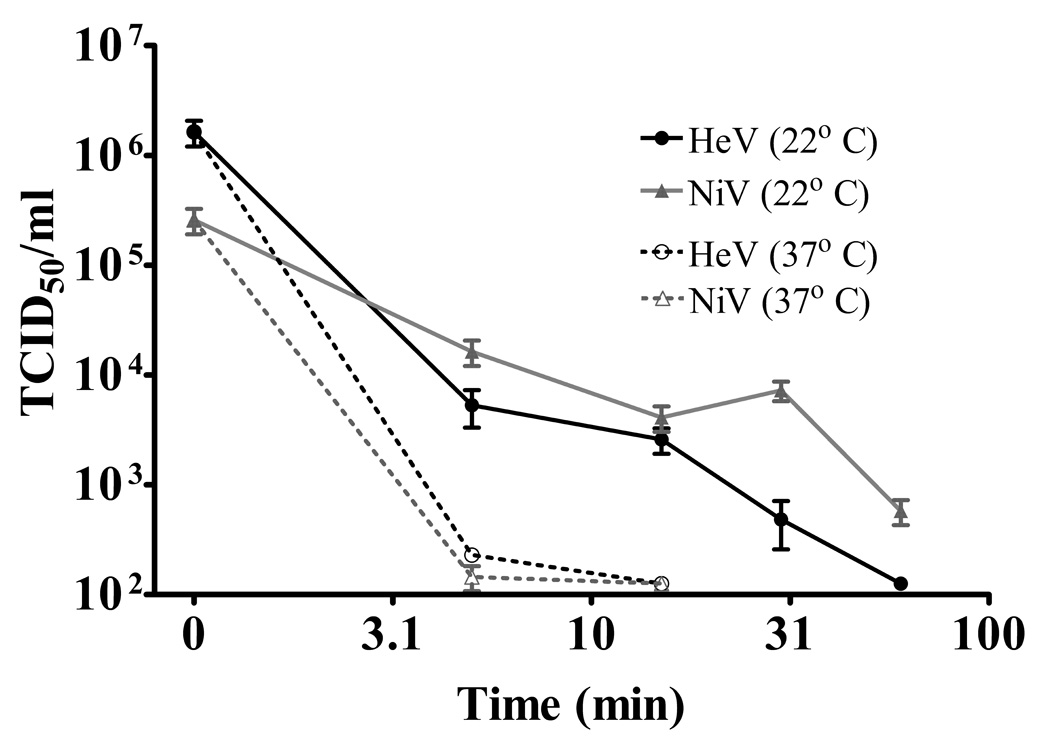
Henipavirus survival after desiccation. Viruses were air dried for 15 min at 22°C (time 0) then resuspended in growth medium and titrated at 5, 15, 30 and 60 min. Data are combined from three separate experiments and are presented as Mean ± S.E.
Virus survival in urine
Experimental infections have shown that urine is a significant route of henipavirus excretion from fruit bats (17) (Halpin et al, unpublished). Therefore, the persistence of henipaviruses in fruit bat urine was examined. Recent experimental studies with P. alecto and P. vampyrus enabled sufficient urine to be collected for these studies, however, urine from additional species was unavailable at the time of testing. HeV incubated in P.alecto urine (pH ~7) survived for more than four days at 22°C with a half-life of 19 hrs, but at 37°C was virtually inactivated in less than one day with the half-life reduced to three hours (Table 1, Figure 3).
Table 1.
Henipavirus survival in fruit bat urine.
| Virus | Fruit bat species | Urine pH | Half-life at 22°C (hrs)a | Half-life at 37°C (hrs)a |
|---|---|---|---|---|
| HeV | P. alecto | 7 | 18.8 | 3 |
| NiV | P. vampyrus | 7 | 17.8 | 1.8 |
| NiV | P. vampyrus | 2 | <0.5 | <0.5 |
Values are the mean of three separate experiments
Figure 3.
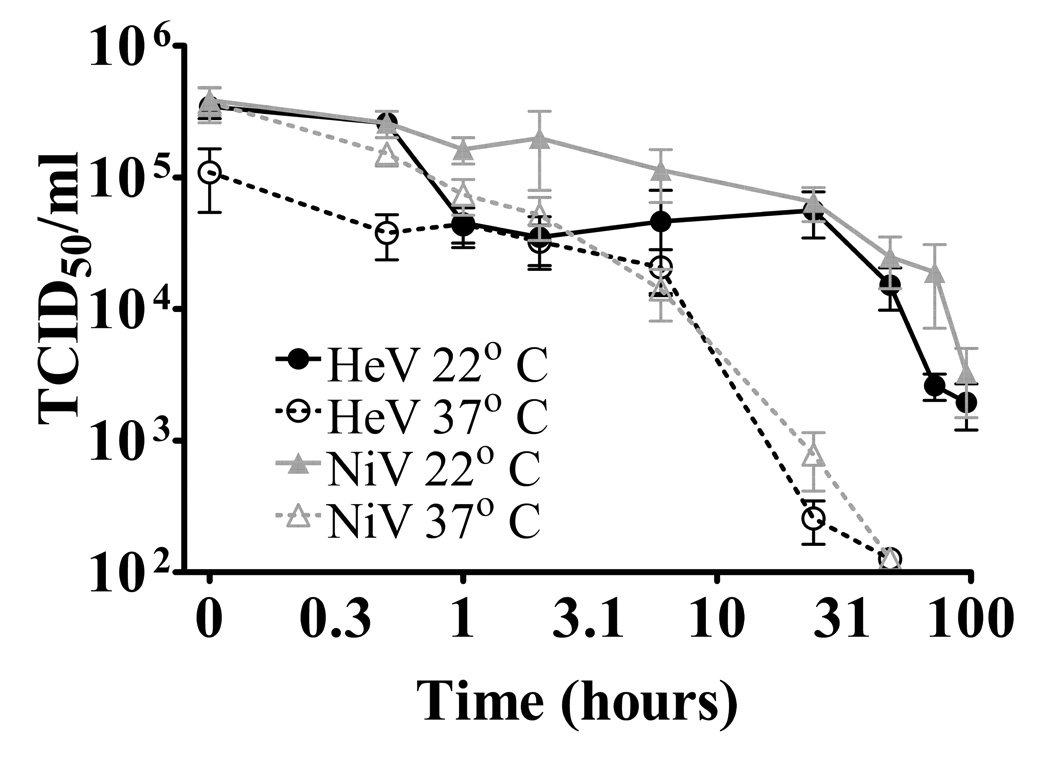
Henipavirus survival in fruit bat urine. Viruses were incubated in P.alecto urine (pH ~7) at 22°C or 37°C. Data are combined from three separate experiments and are presented as Mean ± S.E.
In contrast, NiV incubated in P. vampyrus urine (pH 2) was inactivated in less than thirty minutes at both 22°C and 37°C (Table 1). However, in P. vampyrus urine with the pH adjusted to 7, the half-life of NiV was 18 hrs at 22°C and 2 hrs at 37°C.
Virus survival in fruit juice and flesh
Viral transmission from bats to intermediate hosts via partially eaten fruit has been posited for both NiV (4) and HeV (5) and NiV has been isolated from a swab of partially eaten fruit in the wild (4). Therefore, the survival of henipaviruses on fruit flesh and in fruit juice was examined. Survival time on fruit pulp and in fruit juices varied depending on the type and pH of the fruit. As shown in table 2, virus survival on mango flesh decreased with increasing acidity. At pH 5, half-lives for HeV and NiV were 22 hrs and 30 hrs, respectively, compared to 0.3 hrs and 1.4 hrs at pH3.
Table 2.
Henipavirus survival on mango flesh.
| Mango pH a | HeV half-life (hrs) | NiV half-life (hrs) | ||
|---|---|---|---|---|
| 22°C | 37°C | 22°C | 37°C | |
| 3.5 | 0.3 | 0.4 | 1.4 | 0.2 |
| 4.5 | 3.5 | 0.5 | 5.5 | 0.5 |
| 5 | 22.4 | 5.9 | 30.3 | 2.2 |
pH of mango flesh was determined at the time of virus inoculation only.
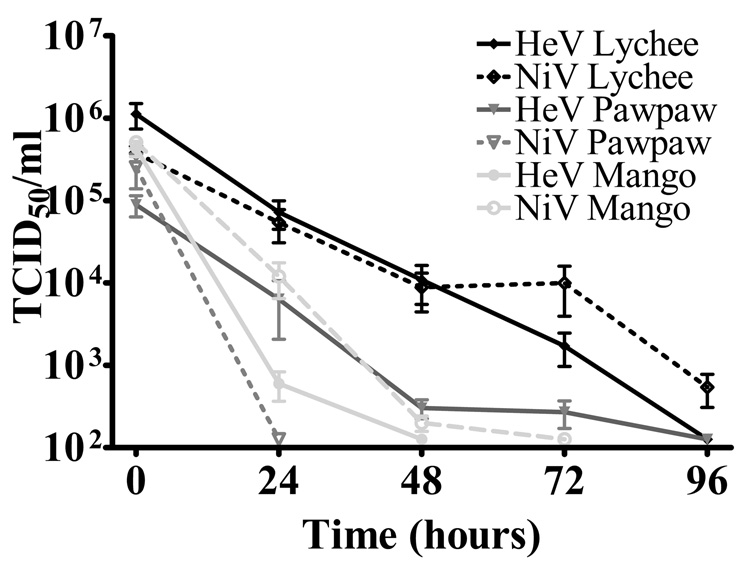
Viruses incubated in juice from lychees showed greater persistence than with either Pawpaw or mango juice with two- to three-fold longer half-lives and survival for more than three days (Figure 4). While these results do provide a general indication of virus survival in these naturally occurring fruits and juices, the lack of available bat saliva for experimental evaluations ensures some degree of artificiality with respect to interpretation of results.
Figure 4.
Henipavirus survival in fruit juice at 22°C. The pH of Lychee juice was 4, Pawpaw juice pH 6 and Mango juice pH 5. Data are combined from three separate experiments and are presented as Mean ± S.E.
Discussion
This study demonstrates that survival of henipaviruses in the environment is highly sensitive to temperature and desiccation. Under most conditions survival time was brief, with half-lives limited to a few hours, indicating that transmission to a new host requires close contact with an infected animal or exposure to contaminated material shortly after excretion. However, under optimal conditions henipaviruses can persist for a number of days and under these circumstances, vehicle-borne transmission may be possible.
This extended survival time may have contributed to the NiV outbreak in Tangail, Bangladesh in 2005 where there was a strong epidemiological link between human NiV cases and drinking raw date palm sap (16). Fruit bats are known to drink from the pots in which the sap is collected and fruit bat excrement in or on the pots is sometimes observed. The conditions under which date palm sap is collected and consumed provide an opportunity for NiV transmission. The sap is collected at night during the coldest months of the year when the average minimum temperature is 13°C −15°C. The pH of palm sap is near neutral (1) and it is consumed within a few hours after sunrise before it ferments. While date palm sap was not available for testing here, under these conditions, the current study indicates that there is likely to be only minimal loss of viral titre before consumption.
The sensitivity of henipaviruses to environmental conditions may contribute to their observed low transmissibility under most circumstances. Attempts to recreate transmission events in a laboratory setting have been largely unsuccessful. A study by Westbury et al (25) found HeV transmission to one of two cats in contact with HeV infected cats and none of two cats housed contiguously with infected cats indicating low transmissibility. Similarly, Williamson et al (26) demonstrated one incidence of cat-to-horse transmission but were unable to demonstrate transmission from bats to bats (using P. poliocephalus), bats to horses, horses to horses or horses to cats. They also noted an absence of live virus in urine collected from the floor of horse stalls despite high titres in bladder urine from the horses, indicating viral inactivation shortly after excretion.
The sensitivity of henipaviruses to the pH of fruit bat urine and fruit flesh may be relevant to the timing of henipavirus outbreaks. Changes in the diet of fruit bat populations due to season or bat migration may influence urine pH and therefore henipavirus persistence after excretion through this route. The marked difference in urine pH between P. alecto and P. vampyrus despite being fed similar diets may indicate that certain species of fruit bat are more suited to henipavirus dispersal. Similarly, variations in fruit pH may reflect differences in their suitability for transmitting virus. We were unable to evaluate the effect of bat saliva on fruit pH and subsequent virus survival in this study such that any conclusions regarding oral transmission of virus by bats still remain to be tested scientifically.
Human-to-human NiV transmission has been observed or suspected in six outbreaks (2, 6, 12, 13, 14, S. Luby, Pers. Comm.). It is usually associated with close contact with a NiV patient who has respiratory symptoms. Except for the outbreak in Siliguri, India in 2001 (2) nosocomial infections have not occurred despite an absence of barrier nursing methods and exposure to body fluids of NiV patients (18). However, the outbreak in Siliguri demonstrates that nosocomial transmission may be a major source of infection and as demonstrated in the current study, the potential for vehicle-borne transmission exists. Therefore barrier nursing practices should be employed when dealing with HeV and NiV patients.
Acknowledgements
Financial support: RF, KH, ADH and PD are supported in part by a National Institutes of Health/National Science Foundation "Ecology of Infectious Diseases" (R01-TW05869) award from the John E. Fogarty International Center and by core funding to the Consortium for Conservation Medicine from the V. Kann Rasmussen Foundation.
Abbreviations
- NiV
Nipah virus
- HeV
Hendra virus
- EMEM
Eagles modified essential medium
- TCID
tissue culture infectious dose
- BSL4
Biosafety level 4
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Aidoo KE, Nout MJ, Sarkar PK. Occurrence and function of yeasts in Asian indigenous fermented foods. FEMS Yeast Res. 2006;6:30–39. doi: 10.1111/j.1567-1364.2005.00015.x. [DOI] [PubMed] [Google Scholar]
- 2.Chadha MS, Comer JA, Lowe L, Rota PA, Rollin PE, Bellini WJ, Ksiazek TG, Mishra A. Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis. 2006;12:235–240. doi: 10.3201/eid1202.051247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chua KB, Bellini WJ, Rota PA, Harcourt BH, Tamin A, Lam Sai Kit K, Ksiazek TG, Rollin PE, Zaki SR, Shieh WJ, Goldsmith CS, Gubler DJ, Roehrig JT, Eaton BT, Gould AR, Olson J, Field HE, Daniels PW, Ling AE, Peters CJ, Anderson LJ, Mahy BWJ. Nipah virus : a recently emergent deadly paramyxovirus. Science. 2000;288:1432–1435. doi: 10.1126/science.288.5470.1432. [DOI] [PubMed] [Google Scholar]
- 4.Chua KB, Lek KC, Hooi PS, Wee KF, Khong JH, Chua BH, Chan YP, Lim ME, Lam Sai Kit K. Isolation of Nipah virus from Malaysian Island flying-foxes. Microbes and Infection. 2002;4:145–151. doi: 10.1016/s1286-4579(01)01522-2. [DOI] [PubMed] [Google Scholar]
- 5.Field HE, Young PL, Yob JM, Mills JN, Hall LS, MacKenzie JS. The natural history of Hendra and Nipah viruses. Microbes and infection. 2001;3:307–314. doi: 10.1016/s1286-4579(01)01384-3. [DOI] [PubMed] [Google Scholar]
- 6.Gurley E, Montgomery JM, Hossain MJ, Bell M, Azad AK, Islam MR, Molla MAR, Carroll DS, Ksiazek T, Rota PA, Lowe L, Comer JA, Rollin P, Czub M, Grolla A, Feldmann H, Luby SP, Woodward JL, Breiman RF. Person-to-person transmission of Nipah virus in a Bangladeshi community. Emerg Infect Dis. 2007 Jul; doi: 10.3201/eid1307.061128. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halpin K, Young PL, Field HE, Mackenzie JS. Isolation of Hendra virus from pteropid bats: a natural reservoir of Hendra virus. Journal of General Virology. 2000;81:1927–1932. doi: 10.1099/0022-1317-81-8-1927. [DOI] [PubMed] [Google Scholar]
- 8.Hanna JN, McBride WJ, Brookes DL, Shield J, Taylor CT, Smith IL, Craig SB, Smith GA. Hendra virus infection in a veterinarian. Med J Aust. 2006;185:562–564. doi: 10.5694/j.1326-5377.2006.tb00692.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hooper PT, Gould AR, Russell GM, Kattenbelt JA, Mitchell G. The retrospective diagnosis of a second outbreak of equine morbillivirus infection. Aust Vet J. 1996;74:244–245. doi: 10.1111/j.1751-0813.1996.tb15414.x. [DOI] [PubMed] [Google Scholar]
- 10.Hsu VP, Hossain MJ, Parashar UD, Ali MM, Ksiazek TG, Kuzmin I, Niezgoda M, Rupprecht C, Bresee J, Breiman RF. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis. 2004;10:2082–2087. doi: 10.3201/eid1012.040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hyatt AD, Selleck PW. Ultrastructure of Equine Morbillivirus. Virus research. 1996;43:1–15. doi: 10.1016/0168-1702(96)01307-x. [DOI] [PubMed] [Google Scholar]
- 12.ICDDRB. Outbreaks of encephalitis due to Nipah/Hendra-like viruses, Western Bangladesh. Health and Science Bulletin. 2003;1:1–6. [Google Scholar]
- 13.ICDDRB. Person-to-person transmission of Nipah virus during outbreak in Faridpur District, 2004. Health and Science Bulletin. 2004;2:5–9. [Google Scholar]
- 14.ICDDRB. Nipah encephalitis outbreak over wide area of Western Bangladesh, 2004. Health and Science Bulletin. 2004;2:7–11. [Google Scholar]
- 15.ICDDRB. Nipah virus outbreak from date palm juice. Health and Science Bulletin. 2005;3:1–5. [Google Scholar]
- 16.Luby SP, Rahman M, Hossain MJ, Blum LS, Husain MM, Gurley E, Khan R, Ahmed B-N, Rahman S, Nahar N, Kenah E, Comer JA, Ksiazek TG. Foodborne transmission of Nipah virus, Bangladesh. Emerging Infectious Diseases. 2006;12:1888–1894. doi: 10.3201/eid1212.060732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Middleton DJ, Morrissy CJ, van der Heide BM, Russell GM, Braun MA, Westbury HA, Halpin K, Daniels PW. Experimental Nipah Virus Infection in Pteropid Bats (Pteropus poliocephalus) J Comp Pathol. 2007;136:266–272. doi: 10.1016/j.jcpa.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Mounts AW, Kaur H, Parashar UD, Ksiazek TG, Cannon D, Arokiasamy JT, Anderson LJ, Lye MS. A cohort study of health care workers to assess nosocomial transmissibility of Nipah virus, Malaysia, 1999. J Infect Dis. 2001;183:810–813. doi: 10.1086/318822. [DOI] [PubMed] [Google Scholar]
- 19.Mungall BA, Middleton DJ, Crameri GS, Halpin K, Bingham J, Eaton BT, Broder CC. Vertical transmission and fetal replication of Nipah virus in an experimentally infected cat. J Infect Dis. 2007;196(6):812–816. doi: 10.1086/520818. [DOI] [PubMed] [Google Scholar]
- 20.Murray K, Rogers R, Selvey L, Selleck P, Hyatt A, Gould A, Gleeson L, Hooper P, Westbury H. A novel morbillivirus pneumonia of horses and its transmission to humans. Emerg Infect Dis. 1995;1:31–33. doi: 10.3201/eid0101.950107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murray K, Selleck P, Hooper P, Hyatt A, Gould A, Gleeson L, Westbury H, Hiley L, Selvey L, Rodwell B, et al. A morbillivirus that caused fatal disease in horses and humans. Science. 1995;268:94–97. doi: 10.1126/science.7701348. [DOI] [PubMed] [Google Scholar]
- 22.Parashar UD, Sunn LM, Ong F, Mounts AW, Arif MT, Ksiazek TG, Kamaluddin MA, Mustafa AN, Kaur H, Ding LM, Othman G, Radzi HM, Kitsutani PT, Stockton PC, Arokiasamy JT, Gary HE, Jr, Anderson LJ. Case-control study of risk factors for human infection with a new zoonotic paramyxovirus, Nipah virus, during a 1998–1999 outbreak of severe encephalitis in Malaysia. Journal of infectious diseases. 2000;181:1755–1759. doi: 10.1086/315457. [DOI] [PubMed] [Google Scholar]
- 23.Reed LJ, Muench H. Simple method for estimating fifty percent end points. Am J Hygiene. 1938;27:493–497. [Google Scholar]
- 24.Shiell BJ, Gardner DR, Crameri GS, Eaton BT, Michalski WP. Sites of phosphorylation of P and V proteins from Hendra and Nipah viruses: newly emerged members of Paramyxoviridae. Virus research. 2003;92:55–65. doi: 10.1016/s0168-1702(02)00313-1. [DOI] [PubMed] [Google Scholar]
- 25.Westbury HA, Hooper PT, Brouwer SL, Selleck PW. Susceptibility of cats to equine morbillivirus. Aust Vet J. 1996;74:132–134. doi: 10.1111/j.1751-0813.1996.tb14813.x. [DOI] [PubMed] [Google Scholar]
- 26.Williamson MM, Hooper PT, Selleck PW, Gleeson LJ, Daniels PW, Westbury HA, Murray PK. Transmission studies of Hendra virus (equine morbillivirus) in fruit bats, horses and cats. Aust Vet J. 1998;76:813–818. doi: 10.1111/j.1751-0813.1998.tb12335.x. [DOI] [PubMed] [Google Scholar]