Takayasu arteritis, a non-specific inflammatory disease affecting the walls of medium and large arteries, is categorized as a medium- and large-vessel vasculitis.1) This disease, which is commonly seen in the Japanese population, was first reported by Professor Mikito Takayasu in 1908, as a case of peculiar change of the central retinal artery with coronary anastomosis and arteriovenous shunt. At the time, Dr. Takayasu was the Director of Kanazawa Medical College Hospital, and it is amazing that, in the discussion of his presentation, the absence of arterial pulse at the radial artery was already mentioned as an associated finding.2) With the accumulation of experience and knowledge, it was documented that this disease involved mainly the aorta and its branches. Because a steno-occlusive lesion of the cervical branches causes a loss of pulse at the upper extremity, the name “pulseless disease” was proposed by Shimizu and Sano in 1951.3) On the other hand, Ross and McKusick suggested the name “aortic arch syndrome” because they thought the pathology was limited to the aortic arch.4) Considering that pulseless disease and aortic arch lesion or atypical co-arctation of the aorta all were attributed to one entity, Ueda et al. introduced the name (pan)-aortitis syndrome in 1965.5) This designation was the standard expression of the disease entity until recently, when there has been a change in the use of the name, mainly because the name “aortitis syndrome” has not been well accepted in the Western literature. The designation “Takayasu arteritis” has become the standard in Japan and elsewhere in appreciation of the original contribution of Professor Takayasu. Historically in Japan, two groups, the Tokyo University group and the Tokyo Medical and Dental University group6, 7) have played leading roles in the investigation of this disease entity. In particular, the former group has accomplished fruitful results in regard to the surgical treatment of this interesting lesion.8–10)
It is well known that adolescent girls and middle-aged women in the second to fourth decades of life are highly affected by this disease. The basic pathology involves medium and large elastic arteries in a pan-arterial inflammatory process that causes marked thickening of the arterial wall of the diseased segment. Pathological studies delineate active (acute) and chronic phases of the disease, although a mixed type also can be present.
The active phase shows involvement of the media and adventitia by lymphocytes, plasma cells, histiocytes, and varying numbers of multinucleated giant cells that transform granulomatous change of the arterial wall. The chronic phase demonstrates pan-arterial transluminal involvement by fibrous intimal hyperplasia, medial degeneration, and adventitial fibrosis that lead to extensive thickening of the arterial wall and subsequent luminal narrowing and occlusion. On the other hand, destruction of the pan-arterial wall results in diffuse dilatation, aneurysmal formation, and thrombosis at the intimal surface. One report described the frequency of morphological changes of the arterial tree by means of angiographic study. It was found that stenosis was the most frequent lesion, being present in 93% of patients, followed by occlusion (57%), dilatation (16%), and aneurysmal formation (7%).11)
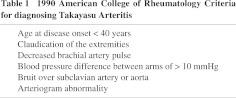
The signs and symptoms of Takayasu arteritis may have a subtle and insidious presentation. In the acute and active phases, it may be accompanied with fever, malaise, arthralgia, and so on. In some cases, the patient complains of pain along the course of the artery, particularly in the neck region. The symptoms presented in the chronic phase are varied according to the area of vascular involvement as well as the extent and nature of pathology. Involvement of the carotid artery presents varying degrees of cerebro-ischemic symptoms, including ophthalmic disorders. Steno-occlusive lesions of the branches of the aortic arch involving the subclavian artery produce pulsate changes in the arm, occasionally accompanied with upper extremity ischemic symptoms. When the ascending aorta is affected, the disease is manifested only as dilatation secondarily leading to aortic valve deformity and aortic regurgitation.12, 13) Hypertension is frequently encountered in Takayasu arteritis and is specifically associated with renal artery involvement and atypical coarctation of the aorta. Cough, dyspnea, chest pain, and pulmonary hypertension are seen in the patient with pulmonary involvement. In summary, these variable symptoms and clinical features are defined as 1) vascular, 2) central nervous system, 3) musculoskeletal, 4) constitutional, and 5) cardiac.14) The criteria for diagnosis were established by the American College of Rheumatology in 1990, and these criteria are most frequently cited. According to the criteria, the presence of at least 3 of 6 items has a sensitivity of 90.5% and a specificity of 97.8% accuracy (Table 1).15)
Since Takayasu arteritis involves various portions of the elastic arteries, several classifications have been proposed mainly on the basis of the anatomical distribution and morphological configuration of the lesion. In 1967, Nakao proposed a classification based on the angiographic findings of the disease: Type I (aortic arch), Type II (descending aorta and abdominal aorta), and Type III (extensive), but his classification dealt only with the steno-occlusive changes of the artery.16) After dilatation and aneurysmal changes were added to the pathology of Takayasu arteritis, a new classification was advocated by Ueno in 1969. In his classification, dilated and aneurysmal changes were distinguished from steno-occlusive lesions and incorporated as Type IV.17) The latest classification, proposed by Hata and Numano in 1996, is based on a report given at an international conference on comparative studies on Takayasu arteritis in Asian and South American countries. This classification was as follows: Type I involves primarily the branches of the aortic arch; Type IIa involves the ascending aorta, the aortic arch, and its branches; Type IIb refers to pathology involving the ascending aorta, aortic arch including its branches, and descending aorta as well; Type III involves the descending abdominal aorta and/or renal artery; Type IV affects only the abdominal aorta and/or renal artery; and Type V combines the features of both Type IIb and Type IV. In addition, involvement of the coronary or pulmonary artery should be defined as C(+) and P(+), respectively.7) This new classification was the first to document pulmonary involvement in Takayasu arteritis as an associated finding. However, it is necessary to be aware that there was a lack of description as to what type of morphology of vascular change was defined as pulmonary involvement in Takayasu arteritis in this classification.
Pulmonary involvement of Takayasu arteritis has been documented from the early stage of investigation into this lesion. Saito, in 1974, described precisely the histopathological details of changes in the pulmonary artery.18) He stated that the histological changes in the pulmonary artery were generally similar to those seen at systemic arteries. However, the wall of the former was thin and, therefore, a) intimal changes were attributed to the occupation of granulation tissue rather than inflammatory edema, b) the normal structure of the arterial wall was completely disrupted, and c) there was unusual communication with the bronchial artery. He also stressed that the extremely peripheral segments were also affected in certain cases. The unusual communication with the bronchial artery would be attributable to the compensatory mechanism of blood supply to the diseased segment of the pulmonary tissues from the systemic circulation and has also been reported as a characteristic clinical finding associated with pulmonary involvement.19-20) The pulmonary vascular changes were studied by means of pneumoangiography by Kozuka et al. and reported in 1968. They observed various changes in the pulmonary arterial tree such as narrowing, rigidity, and obstruction of the main pulmonary artery and stenosis of the segmental artery extending to the peripheral branches. It was concluded that the various changes such as irregularity, stenosis, and obstruction were observed in different aspects of various different segments beginning from large to small in the pulmonary arterial tree.21)
Numano et al. also studied pulmonary artery involvement in patients who were clinically followed under the diagnosis of Takayasu arteritis by means of pulmonary scintigram and found abnormal perfusion in 73% of the population. Perfusion defects were as follows: lobar perfusion defect in 27%, segmental perfusion defect in 42%, and non-segmental defect in 30%. It is interesting to note that again in this study in the area where perfusion defects were detected the presence of pulmonary circulation by way of the bronchial artery was confirmed.22) In summary, it has been clearly documented histopathologically as well as clinically that the pulmonary artery is affected to a certain degree concomitantly with pathology in the systemic arteries in Takayasu arteritis.
On the other hand, we have recently encountered several reports in the literature dealing with predominant, isolated, or initial involvement of the pulmonary artery in Takayasu arteritis.23-26) The characteristics of these reports were that the pathological changes were detected only in the pulmonary artery but not in systemic arteries such as the aorta and its branches, and that these changes in the pulmonary artery, morphologically demonstrated as severe narrowing or total occlusion of the lumen, were most frequently seen at areas of large caliber of the pulmonary arterial tree, such as the left and right or lobar pulmonary arteries. Surgical treatment, mostly by means of a bypass procedure using prosthetic graft, has already been undertaken in some of these lesions.27)
There appear to be two distinctive patterns of pulmonary involvement in Takayasu arteritis. One type is associated with pathological changes of the systemic arteries, whereas the other type is the so-called “isolated type” in which pathological changes are only noted in the pulmonary artery. In this type, the morphological changes are most frequently in the large caliber segment(s). Although the diagnosis of Takayasu arteritis is based on various characteristics, among them, the morphological features are the most definitive. Furthermore, in the “isolated” type, even the criteria proposed by the American College of Rheumatology have not been adopted in establishing the diagnosis of Takayasu arteritis. The presence of a small number of cases of the “isolated” type is particularly interesting in reference to whether this type is also incorporated into the category of Takayasu arteritis or is better placed in the category of pulmonary vasculitis.28) Further investigation is needed.
References
- Weyand CM, Goronzy JJ. Medium- and large-vessel vasculitis. N Engl J Med. 2003; 349: 160–9 [DOI] [PubMed] [Google Scholar]
- Takayasu M. A case of peculiar change of central retinal artery(in Japanese). Acta Soc Opth Jpn. 1908; 12: 554–5 [Google Scholar]
- Shimizu K, Sano K. Pulseless disease. J Neuropathol Clinic Neurol. 1951; 1: 37–47 [PubMed] [Google Scholar]
- Ross RS, McKusick VA. Progress in Internal Medicine - Aortic Arch Syndromes. AMA Arch Intern Med. 1953; 92: 701–40 [DOI] [PubMed] [Google Scholar]
- Ueda H, Ito I, Saito K. Aortitis syndrome. (in Japanese) Medicine. 1965; 15: 239–56 [Google Scholar]
- Kitamura H, Kobayashi Y, Kimura A, Numano F. Association of clinical manifestations with HLA-B alleles in Takayasu arteritis. Int J Cardiol. 1998; 66 (suppl 1): S121–6 [DOI] [PubMed] [Google Scholar]
- Hata A, Noda M, Moriwaki R, Numano F. Angiographic findings of Takayasu arteritis: new classification. Int J Cardiol. 1996; 54 (suppl): S155–63 [DOI] [PubMed] [Google Scholar]
- Tada Y, Sato O, Ohshima A, Miyata T, Shindo S. Surgical treatment of Takayasu arteritis. Heart Vessels Suppl. 1992; 7: 159–67 [DOI] [PubMed] [Google Scholar]
- Miyata T, Sato O, Koyama H, Shigematsu H, Toda Y. Long-term survival after surgical treatment of patients with Takayasu's arteritis. Circulation. 2003; 108: 1474–80 [DOI] [PubMed] [Google Scholar]
- Miyata T, Sato O, Deguchi J, Kimura H, Namba T, Kondo K, et al. Anastomotic aneurysms after surgical treatment of Takayasu's arteritis: a 40-year experience. J Vasc Surg. 1998; 27: 438–45 [DOI] [PubMed] [Google Scholar]
- Vanoli M, Daina E, Salvarani C, Sabbadini MG, Rossi C, Bacchiani G, et al. Takayasu's arteritis: A study of 104 Italian patients. Arthritis Rheum. 2005; 53: 100–7 [DOI] [PubMed] [Google Scholar]
- Nakajima N, Yutani C. Study on dilatative change in aortitis syndrome (in Japanese). Report on Research Committee on Intractable Vasculitides sponsored by Health Sciences Research 1991; 57–60
- Nakajima N, Ando M, Utani C. A patho-clinical study on valvular changes in aortitis syndrome (A preliminary Report) (in Japanese). Report of Research Committee on Intractable Vasculitides sponsored by Health Science Research1990
- Savage BJ, Gupta RK, Angle J, Okusa MD. Takayasu arteritis presenting as a pulmonary-renal syndrome. Am J Med Sci. 2003; 325: 275–81 [DOI] [PubMed] [Google Scholar]
- Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990; 33: 1129–34 [DOI] [PubMed] [Google Scholar]
- Nakao K, Ikeda M, Kimata S, Niitani H, Niyahara M. Takayasu's arteritis. Clinical report of eighty-four cases and immunological studies of seven cases. Circulation. 1967; 35: 1141–55 [DOI] [PubMed] [Google Scholar]
- Ueno A. Pathophysiology and treatment of aneurysm (in Japanese). J Jpn Coll Angiol. 1969; 9: 119–24 [Google Scholar]
- Saito K. Histopathological study of Takayasu arteritis (in Japanese). Report of Research Committee on Aortitis Syndrome sponsored by Health Science Report 1974; 9–14
- Ishikawa T. Systemic artery—pulmonary artery communication in Takayasu's arteritis. AJR Am J Roentgenol. 1977; 128: 389–93 [DOI] [PubMed] [Google Scholar]
- Matsunaga N, Hayashi K, Sakamoto I, Ogawa Y, Matsuoka Y, Imamura T, et al. Coronary-to-pulmonary artery shunts via the bronchial artery: analysis of cineangiographic studies. Radiology. 1993; 186: 877–82 [DOI] [PubMed] [Google Scholar]
- Kozuka T, Nosaki T, Sato K, Ihara K. Aortitis syndrome with special reference to pulmonary vascular changes. Acta Radiol Diagn (Stockh). 1968; 7: 25–32 [DOI] [PubMed] [Google Scholar]
- Numano F, Isohisa I, Mashimo S, Numano F, Maezawa H. Pulmonary functions in Takayasu's disease (author's transl) (in Japanese). Nippon Naika Gakkai Zasshi. 1977; 66: 1248–59 [DOI] [PubMed] [Google Scholar]
- Elsasser S, Soler M, Bolliger C, Jager K, Steiger U, Perruchoud AP. Takayasu disease with predominant pulmonary involvement. Respiration. 2000; 67: 213–5 [DOI] [PubMed] [Google Scholar]
- Lie JT. Isolated pulmonary Takayasu arteritis: clinicopathologic characteristics. Mod Pathol. 1996; 9: 469–74 [PubMed] [Google Scholar]
- Nakabayashi K, Kurata N, Nangi N, Miyake H, Nagasawa T. Pulmonary artery involvement as first manifestation in three cases of Takayasu arteritis. Int J Cardiol. 1996; 54 (Suppl): S177–83 [DOI] [PubMed] [Google Scholar]
- Hara M, Sobue R, Ohba S, Kitase M, Sasaki S, Ogino H, et al. Diffuse pulmonary lesions in early phase Takayasu arteritis predominantly involving pulmonary artery. J Comput Assist Tomogr. 1998; 22: 801–3 [DOI] [PubMed] [Google Scholar]
- Nakajima N, Masuda M, Imamaki M, Ishida A, Tanabe N, Kuriyama T. A case of pulmonary artery bypass surgery for a patient with isolated Takayasu arteritis and review of literature. Ann Thorac Cardiovasc Surg. in press [PubMed] [Google Scholar]
- Seo P, Stone JH. Large-vessel vasculitis. Arthritis Rheum. 2004; 51: 128–39 [DOI] [PubMed] [Google Scholar]


