Abstract
Double jeopardy and health congruency suggest that adolescents’ joint experience of their weight and weight perceptions are associated with depressive symptoms, but each theory offers a different prediction about which adolescents are at greatest risk. This study investigates the proposed associations and the applicability of both theoretical perspectives using data from 6,557 male and 6,126 female National Longitudinal Study of Adolescent Health (Add Health) Wave II participants. Empirically, results indicate that focusing on the intersection of weight and weight perceptions better shows which adolescents are at risk of depressive symptoms than an approach that treats both predictors as independent, unrelated constructs. Weight pessimists are at greatest risk of depressive symptoms. Thus, results support the health congruency framework, its extension to subpopulations outside of older adults, and its extension to optimism and pessimism about specific health conditions.
American adolescents receive mixed messages about weight. The media, weight loss industries, and weight-related public health campaigns encourage them to maintain slender frames while fat acceptance movements and healthy body image programs encourage them to love their bodies regardless of shape. Thus, it is unsurprising that roughly one-third of adolescents inaccurately perceive their weight, with more under- versus overestimating it (Martin, Frisco, and May 2009).
Research has not examined whether mismatched weight and weight perceptions are distressing for adolescents. Instead, two separate research strands focus on consequences of either actual weight (e.g., Needham and Crosnoe 2005; Swallen et al. 2005) or weight perceptions (e.g., Daniels 2005; Pesa, Syre, and Jones 2000) for depressive symptoms. Results suggest that actual weight is largely unrelated to depressive symptoms (especially in national samples) (see Wardle and Cooke 2005 for a review), except for adolescent subgroups such as younger teens (Needham and Crosnoe 2005) or racial/ethnic minorities (Frisco, Houle, and Martin 2009). Conversely, weight perceptions are associated with depressive symptoms even after controlling for actual weight and other confounders (e.g., Daniels 2005; Pesa et al. 2000). The take-home message from these research strands is that weight perceptions matter more than actual weight for predicting adolescent depressive symptoms.
We argue that actual and perceived weight should not be treated as competing factors predicting depressive symptoms. Adolescents simultaneously grapple with numbers on their scales and images in their mirrors. The two do not always match.
Theories of double jeopardy and health congruency offer distinct explanations about why the (mis)match of weight and weight perceptions may predict adolescent depressive symptoms. We draw from both theories to develop and test competing explanations about whether and how the intersection of the two matter and to offer insight into whether these theories are useful for understanding links between adolescent physical and mental health outcomes.
ACTUAL WEIGHT, WEIGHT PERCEPTIONS, AND DEPRESSIVE SYMPTOMS
In survey research, clinical weight categories indicating adolescent underweight, normal weight, overweight and obesity are usually derived from body mass index (BMI) percentiles that are based on height and weight data.1 They account for age- and sex-specific growth and are constructed using guidelines from Centers for Disease Control and Prevention (CDC) (2003).
Overweight and obesity are negative clinical statuses that are also stigmatized physical and social statuses (Dejong 1980; Puhl and Brownell 2003). Overweight adolescents are seen as unhealthy, ugly, lazy, dirty and stupid (Crandall and Schiffhauer 1998) and people are biased against befriending obese persons (Latner, Stunkard, and Wilson 2005; Richardson et al. 1961).
The discrimination and marginalization of heavy adolescents has led scholars to examine the mental health consequences of weight. Theoretically, weight stigma should lead to depression, withdrawal, and diminished self-worth among overweight and obese adolescents (Puhl and Brownell 2003), but little evidence links either overweight or obesity to adolescent depressive symptoms (Wardle and Cooke 2005).
Conversely, underweight predicts depressive symptoms among adolescent boys (Frisco et al. 2009). This finding supports work suggesting that underweight is stigmatizing for boys, who are expected to maintain larger builds and masculine ideals of muscularity (Harmatz, Gronendyke, and Thomas 1985).
Weight perceptions are powerful self-schemas, or views and beliefs about the self resulting from prevailing norms, social experiences, and cultural values (Markus 1977). Self-schemas organize how adolescents process and respond emotionally to their weight (Pesa et al. 2000) and are linked to adolescents’ body image. Further, there is variation in how individuals process body weight to arrive at weight perceptions (Markus, Hamill, and Sentis 1987).
The weight perceptions literature offers a simple explanation for null associations between adolescent overweight and depressive symptoms: consequences of sociocultural ideals about weight and weight stigma operate through weight perceptions, not actual weight. Research supports this idea. Overweight and underweight perceptions predict depressive symptoms net of actual weight (Daniels 2005; Pesa et al. 2000).
We conceptualize the importance of weight perceptions differently and have an alternative explanation about how weight and weight perceptions influence adolescent depressive symptoms. We hypothesize that adolescents’ emotional responses to their self-schemas depend on their actual weight. In other words, weight and weight perceptions jointly influence adolescent depressive symptoms.
Double jeopardy and weight congruency provide competing explanations about how actual weight and weight perceptions intersect to predict adolescent depressive symptoms. Double jeopardy emphasizes that poor mental health is likely when individuals occupy multiple disadvantaged statuses (Dowd and Bengston 1978). Health congruency focuses on (mis)matches between objective and perceived health statuses and predicts that poor mental health outcomes stem from pessimistic health perceptions (Chipperfield 1993).
Double jeopardy is traditionally applied in studies of adult well-being to explain consequences of jointly experiencing disadvantaged status characteristics such as old age and minority race/ethnicity (Dowd and Bengston 1978) or divorce and poverty (Smith and Waitzman 1994). A seminal study testing double jeopardy examines whether older minority persons face a double burden due to age and race/ethnicity across a range of negative outcomes (Dowd and Bengston 1978). The study findings support this notion with respect to poor self-assessed health, but not all outcomes under investigation. Research over the last three decades continues to show mixed support for double jeopardy’s applicability to adult health outcomes (e.g., Ferraro and Farmer 1996; Smith and Waitzman 1994).
The same is true of recent research on adolescent mental health outcomes. The double disadvantage of race and poverty, but not gender and poverty or race and gender, predicts adolescent depression in one study (McLeod and Owens 2004), while another study finds that gender and socioeconomic status doubly disadvantage girls with respect to internalizing symptoms (Mendelson et al. 2008). To explain why double jeopardy should lead to poor mental health outcomes, these studies turn to stress theory and postulate that multiple disadvantages lead to an accumulation of stressors, limited coping resources, and thus, an increased risk of psychological distress (e.g., Pearlin 1989).
We also examine adolescent mental health and draw from stress theory to explain why the combination of a disadvantaged weight status and negative weight perception may lead to depressive symptoms. We depart from prior work by asking whether double jeopardy is useful for understanding consequences of a disadvantaged status characteristic (weight) and a negative self-schema (weight perceptions). We find this extension reasonable given that a disadvantaged or stigmatized weight status confers stressors on young people (Miller and Kaiser 2001) and leads them to have less social support due to social isolation stemming from weight stigma (Strauss and Pollack 2003). The addition of a negative self-schema may therefore compound vulnerability to psychological distress. For example, an obese adolescent girl who perceives being overweight must manage the stress of weight stigma and the burden of her negative self-appraisal while likely being socially isolated. These experiences place her at a greater risk of depressive symptoms than her normal weight peer who perceives being about the right weight who likely faces less stress as a result of her weight or weight perceptions.
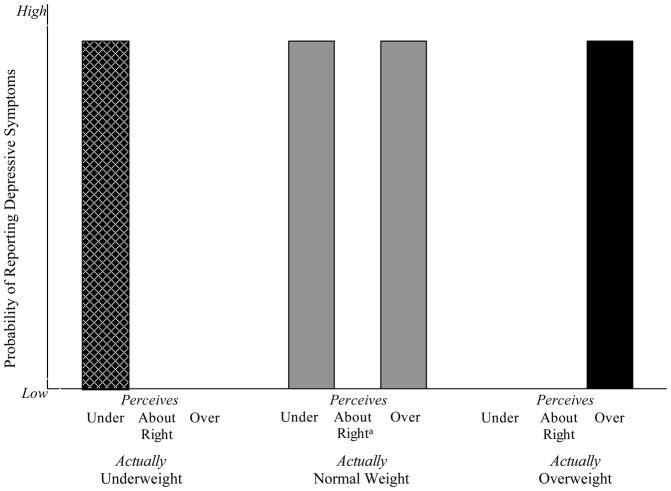
Figure 1 better depicts this example and shows adolescents hypothesized to be at greatest risk of depressive symptoms because they are doubly disadvantaged by a stigmatized weight status and negative weight perception. They include underweight boys with underweight perceptions (represented by the checkered black bar on the left side of Figure 1) and all overweight adolescents with overweight perceptions (represented by the solid black bar on the right side of Figure 1).
Figure 1.
Adolescents Most Likely to Report Depressive Symptoms due to the Intersection of Actual Weight and Weight Perceptions According to Two Theoretical Frameworks
 de Denotes group with a high probability of depressive symptoms according to double jeopardy (all adolescents)
de Denotes group with a high probability of depressive symptoms according to double jeopardy (all adolescents) Denotes group with a high probability of depressive symptoms according to double jeopardy (boys only)
Denotes group with a high probability of depressive symptoms according to double jeopardy (boys only) Denotes group with a high probability of depressive symptoms according to weight congruency
Denotes group with a high probability of depressive symptoms according to weight congruency- Bar height corresponds to a high risk of depressive symptoms only; It does not correspond to any particular predicted value.
- adenotes reference group
Figure 1 also includes grey bars representing adolescents at greatest risk of depressive symptoms according to health congruency (Chipperfield 1993). This alternative lens for considering how weight and weight perceptions jointly influence depressive symptoms was originally used to explain how and why contradictory objective and perceived health statuses influence older adults’ mortality and physical well-being (e.g., Chipperfield 1993; Idler, Hudson, and Leventhal 1999). It identifies individuals as health realists (or health congruent) if perceptions match actual health; health optimists if health perceptions are better than actual health suggests; or health pessimists if health perceptions are worse than actual health suggests (Chipperfield 1993). Health optimists and realists live longer than health pessimists (Chipperfield 1993). The underlying mechanism hypothesized to explain this connection is the power of positive illusions about health (Taylor and Brown 1988).
More recent research links health congruence to mental health among aging adults. Hong et al. (2004) find that health pessimism predicts depression for this group. Borrowing from prior research (e.g., Peterson and Bossio 1991), Hong et al. (2004) suggest that their findings stem from a general proneness to depressive symptoms among health pessimists.
Like Hong et al. (2004), we also focus on mental rather than physical health. We build on health congruency literature in two ways. We focus on its relevance during a different life course stage, adolescence. We also assess how perceptions of a specific health dimension, weight, influence mental health. Focusing on weight pessimism rather than general health pessimism is prudent because adolescents are generally very healthy. Weight is one of the few health dimensions with which adolescents may encounter or perceive problems.
We ask whether weight congruency is linked to adolescent depressive symptoms and whether weight pessimists (versus optimists and realists) are at greater risk. Weight pessimists perceive weight as worse than their actual weight classification. This includes normal weight adolescents who inaccurately perceive being over- or underweight (represented by grey bars in Figure 1). Weight optimists perceive weight as better than their actual weight classification. They include over- and underweight adolescents who perceive weight as about right. Weight realists have accurate weight perceptions. They include underweight adolescents with underweight perceptions, normal weight adolescents who perceive being about right, and overweight adolescents with overweight perceptions.
Weight congruency may influence adolescent depressive symptoms for the same reason that health congruency influences depression among older adults. Health pessimists are prone to depressive symptoms (Hong et al. 2004, Peterson and Bossio 1991). Global indicators of pessimism also predict depression (e.g., Plomin et al. 1992, Swanholm et al. 2009). Further, weight helps define adolescents’ physical appearance. Thus, weight pessimism may also reflect a negative self-evaluation, which also predicts depression (Beck 1976).
Double jeopardy and health congruency offer divergent explanations about why weight and weight perceptions jointly influence depressive symptoms and divergent predictions about who is at risk. A primary study goal is examining which theory is most applicable using data from a nationally representative adolescent cohort. This study provides a foundation for future research by medical sociologists who are interested in adapting these theories to adolescents health outcomes, consequences of health statuses and self-schemas for mental health, and consequences of (in)consistent perceptions of different health conditions (rather than general health only). An additional study contribution is our intersectional approach to understanding how actual weight and weight perceptions predict depressive symptoms. We move beyond a traditional approach where one or the other but not both matters. Thus, study findings are also relevant to scholars specifically interested in mental health consequences of weight and weight perceptions.
DATA AND METHODS
Data and Sample
Add Health is a longitudinal, nationally representative survey of 20,745 7th –12th graders from 134 schools (Bearman, Jones, and Udry 1997). Respondents were selected from a stratified random sample of school students. Three waves of in-home survey data were collected in 1995, 1996 and 2000–2001. We use data from Waves I and II because of interest in relationships between adolescent weight and depressive symptoms. At Wave III, most respondents are young adults. Wave II includes 14,738 adolescents, 71% of the original Wave I sample. We restrict analyses to respondents who were age 20 or younger at Wave II who had a valid sampling weight. We also exclude 779 girls who reported ever being pregnant due to concerns about calculating a body mass index (BMI) score that did not accurately capture body fatness. Our final analytic sample includes 6,557 boys and 6,126 girls.
We use multiple imputation to iteratively replace missing values on all variables with predictions based on random draws from the posterior distributions of parameters observed in the sample, creating multiple complete data sets (Allison 2001).2 Prediction models are based on the rich set of social and economic variables available in Add Health. We impute data using “ICE”, a multiple imputation program created for Stata 9.0 (Royston 2005). We average empirical results across five imputation samples and appropriately account for random variation across these samples to calculate standard errors (Royston 2005). Findings presented here are substantively and statistically similar to findings from analyses where we handle missing data using listwise deletion.
Measures
Depressive Symptoms
Wave II of Add Health includes a modified, 19-item version of Radloff’s (1977) original Center for Epidemiological Studies Depression Scale (CES-D). Questions asked respondents how often in the past week they: felt depressed, sad, lonely, fearful, disliked, that they could not shake blues or that others are unfriendly to them; felt that life was a failure or that life was not worth living; did not feel hopeful, happy, or as good as others; did not enjoy life; had a poor appetite; were too tired to do things; talked less than usual; were bothered by things; and had trouble focusing or trouble starting new things. Responses to items range from 0 (never or rarely) to 3 (most or all of the time). Responses are summed; higher scores indicate more depressive symptoms (α = .88).
To account for the CES-D scale’s highly skewed distribution and to identify troubled adolescents, we dichotomize CES-D scores to reflect scoring at least one standard deviation above the sample mean, or 19 or higher (1 = yes). Prior studies using Add Health also use this approach (Langenkamp and Frisco 2008; Swallen et. al. 2005).3
Adolescent Weight
Wave II interviewer-measured height and weight indicators are used to create BMI percentiles.4 We use CDC (2003) guidelines for assigning age-and sex-specific BMI percentiles for youth and classifying BMI scores into categories for underweight (BMI < 5th percentile), normal weight (BMI ≥ 5th and < 85th percentile), overweight (BMI ≥ 85th and < 95th percentile), and obese (BMI ≥ 95th percentile). Overweight and obese adolescents are included in a single category, so that weight and weight perceptions categories (described below) are parallel. Analysis treating them as separate categories produces statistically and substantively similar results to those presented here.
Adolescent Weight Perceptions
Wave II respondents were asked “how do you feel about yourself in terms of weight?” Response options were “very underweight,” “slightly underweight,” “about the right weight,” “slightly overweight,” and “very overweight.” Consistent with other Add Health analyses (e.g., Pesa et al. 2000), we collapse responses into three categories and create dummy variables indicating perceptions of underweight, about the right weight, and overweight.
Control Variables
Control variables include Wave I sociodemographic and family-level variables associated with weight, weight perceptions and depressive symptoms. They include dummy variables indicating race/ethnicity (reference = White; other categories = Black, Hispanic, Asian American, Native American), nativity (1 = U.S.-born), and family structure (reference = two parent household, other categories = living in a single parent, stepparent or other household type), and parents’ obesity status (1 = at least 1 parent is obese). Age in years, parent’s highest education level, and 1994–1995 family income percentile categories are also controlled. The last two covariates indicate poor/fair health (1= yes) and regular physical activity (1 = yes; adolescents participate in school athletics, exercise at least five days/week, or play an active sport at least five days/week). They help guard against the possibility that weight represents muscle mass or poor health. Appendix A presents weighted descriptive statistics for all variables by gender.
Analytic Strategy
Our initial descriptive analyses provide readers with a picture of congruence between adolescents’ weight and weight perceptions. Estimates from these analyses show how adolescent girls’ and boys’ weight perceptions vary across weight categories.
Then, we estimate weighted logistic regression models that correct for design effects to examine how actual weight and weight perceptions predict boys’ and girls’ depressive symptoms. Model 1 estimates the independent contribution of actual weight net of confounders. Model 2 estimates the independent contribution of perceived weight net of confounders. Model 3 includes objective and perceived weight as independent predictors of depressive symptoms. Model 4 includes an interaction between actual and perceived weight to examine whether their intersection is related to depressive symptoms. It tests the applicability of the Double Jeopardy and Health Congruency frameworks. We also estimated ancillary models with different omitted reference categories to identify all within- and between-weight category differences in depressive symptoms. To easily depict findings from these models, we calculate and graph predicted probabilities of reporting depressive symptoms by weight and weight perceptions for boys and girls. Probabilities assume that all covariates except for weight and weight perceptions are set to mean or modal values. In each figure, symbol subscripts above bars denote significant differences (p<=.01) in the predicted probability of depressive symptoms between appropriate reference and comparison categories. These estimates reveal what is lost when models do not consider the intersection between actual weight and weight perceptions.
Since we use Wave II data to measure actual weight, weight perceptions, and depressive symptoms, analyses are cross-sectional and only speak to relationships between adolescents’ current weight, weight perceptions and depressive symptoms. They cannot be used to discern causality. Supplementary analyses checked whether controlling for Wave I depressive symptoms substantially changed associations between Wave II actual weight, weight perceptions and depressive symptoms. It did not. We do not include Wave I depressive symptoms in final models to avoid producing a lagged dependent variable model where results would be interpreted in terms of change over time. These results would violate causal order assumptions because one of the variables used to assess changes in depressive symptoms would precede Wave II measures of weight and weight perceptions.
RESULTS
The Intersection of Weight and Weight Perceptions
Table 1 shows weighted proportions of underweight, normal weight, and overweight boys and girls with different weight perceptions. More than half of adolescent boys and girls in each weight category have congruent weight perceptions, but differences in congruence across weight categories exist. Panel A of Table 1 indicates that 67.6% of normal weight boys perceive weight as about right. These boys are at low risk of depressive symptoms according to both theories this study tests. Their weight and weight perceptions are congruent and neither weight nor weight perceptions confer disadvantages on them. Smaller proportions of underweight (57.3%) and overweight (57.8%) boys have congruent weight perceptions. These boys are at risk of depressive symptoms according to double jeopardy (their weight and weight perceptions are disadvantaged) but not weight congruency (their weight and weight perceptions match).
Table 1.
Weighted Proportion of Adolescents With (In)Congruent Weight Perceptions
| Weight Perceptions
|
|||||
|---|---|---|---|---|---|
| Actual Weight | Underweight | About Right | Overweight | Total | Row % |
| Panel A. Boys (N=6,557) | |||||
| Underweight | 0.573 (162) | 0.373 (106) | 0.054 (15) | 1.000 | 0.043 (283) |
| Normal | 0.254 (1095)a | 0.676 (2918)a | 0.070 (301)a | 1.000 | 0.658 (4314) |
| Overweight | 0.033 (64) | 0.389 (763)a | 0.578 (1133)a | 1.000 | 0.299 (1960) |
| Column % | 0.202 (1321) | 0.578 (3787) | 0.221 (1449) | 1.000 | 1.000 |
|
| |||||
| Panel B. Girls (N=6,126) | |||||
| Underweight | 0.583 (122) | 0.310 (65) | 0.107 (22) | 1.000 | 0.034 (209) |
| Normal | 0.117 (503)a | 0.639 (2740)a | 0.244 (1048)a | 1.000 | 0.700 (4290) |
| Overweight | 0.019 (32) | 0.174 (283)a | 0.807 (1312)a | 1.000 | 0.266 (1627) |
| Column % | 0.107 (655) | 0.504 (3088) | 0.389 (2384) | 1.000 | |
Notes:
- Indicates a statistically significant difference between adolescent boys and girls derived from logit models
- χ2 test for gender difference in association of weight and weight perceptions = 5333.59 (p<.001)
- Cell N in parentheses
- Source: National Longitudinal Study of Adolescent Health
Panel B indicates that weight congruence is most prevalent among overweight girls. Almost 81% perceive being overweight. These girls are at risk of depressive symptoms according to double jeopardy, but not weight congruency. Among underweight and normal weight girls, 58.3% and 63.9% have congruent weight perceptions, respectively. The latter group has a low risk of depressive symptoms according to both theories.
Statistically significant gender differences emerge across two of three congruent weight perceptions groups.5 Overweight girls are more likely to have congruent weight perceptions than boys but a slightly larger proportion of normal weight boys (versus girls) perceive being about right.
Gender differences in weight incongruence also exist. Normal weight boys versus girls are more likely to perceive being underweight (25.4% vs. 11.7%), while normal weight girls versus boys are more likely to perceive being overweight (24.4% vs 7.0%). Weight congruency predicts that these weight pessimists are at risk of depressive symptoms. More male (39%) than female (17.4%) adolescents are weight optimists (are overweight but perceive being about the right weight) with a low risk of depressive symptoms.
Weight, Weight Perceptions &Depressive Symptoms among Boys
Table 2 shows how weight, weight perceptions and (in)consistencies between them are associated with depressive symptoms. Models are estimated separately by gender because weight and weight perceptions are expected to affect mental health differently for boys and girls. Wald tests confirmed the appropriateness of this modeling strategy.
Table 2.
Weighted Estimates (Logits) from Logistic Regression Models predicting Adolescent Depressive Symptoms
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Panel A: Boys (N=6,557) | |||
| Actual Weight (ref = normal) | |||
| Underweight | .680 (.208) **a | .574 (.205) **a | |
| Overweight | .044 (.120) | −.170 (.160) | |
| Weight Perceptions (ref = about right) | |||
| Perceives underweight | .566 (.125) *** | .487 (.134) *** | |
| Perceives overweight | .522 (.147) *** | .637 (.180) *** | |
| Constant | −4.74 (.733) *** | −4.97 (.737) *** | −4.87 (.731) ***a |
|
| |||
| Panel B: Girls (N=6,126) | |||
| Actual Weight (ref = normal) | |||
| Underweight | −.341 (.241) a | −.470 (.266) a | |
| Overweight | −.150 (.125) | −.429 (.151) ** | |
| Weight Perceptions (ref = about right) | |||
| Perceives underweight | .454 (.144) ** | .513 (.155) *** | |
| Perceives overweight | .426 (.099) *** | .604 (.115) *** | |
| Constant | −3.01 (.554) *** | −3.23 (.565) *** | −3.05 (.553) ***a |
p <= .001
p <= .01
p <= .05
Notes:
- Indicates a statistically significant gender difference
- Standard errors in parentheses
- All models also include control variables representing respondents’ race/ethnicity, nativity, age, fair or poor self-assessed health, whether respondents are physically active at least 5 days/week, family structure, family income percentile, parents’ highest education level, and parents’ obesity status
- Source: National Longitudinal Study of Adolescent Health
Panel A in Table 2 presents estimates for boys. When models include weight only (Model 1) or weight perceptions only (Model 2), findings are consistent with past literature (Frisco et. al. 2009; Daniels 2005). Underweight and perceptions of over- and underweight predict depressive symptoms. Underweight boys’ odds of depressive symptoms are nearly double (odds ratio, OR = exp(.680) = 1.973) that of normal weight boys, net of controls. Their estimated odds of depressive symptoms are also significantly larger than their underweight female counterparts. With respect to weight perceptions, boys who perceive being under- or overweight have 76.1% (OR = exp(.566) = 1.761) and 68.5% (OR = exp(.522) = 1.685) higher odds of depressive symptoms, respectively, than boys who perceive being about right. When we include actual and perceived weight in the same model, estimated effects of weight and weight perceptions are only slightly attenuated and gender differences in the effect of underweight remain significant (see Model 3).
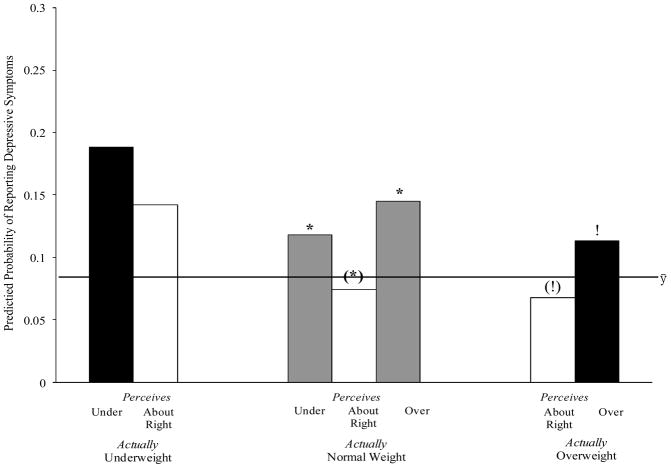
Figure 2 depicts how boys’ depressive symptoms depend on their joint weight and weight perceptions.6 Consistent with Figure 1, black bars represent boys with the highest risk of depressive symptoms according to double jeopardy and grey bars represent boys with the highest risk of depressive symptoms according to weight congruency. This allows for easy demonstration of how each theory applies to our findings. The horizontal line represents the predicted probability of reporting depressive symptoms for a boy with the average or modal value on all covariates. It allows readers to compare an average boy’s risk of depressive symptom to that of boys in different weight by weight perceptions categories.
Figure 2.
The Predicted Probability of Reporting Depressive Symptoms by Actual Weight and Weight Perceptions among Boys
-
Reference groups for comparison:
- (*): Normal weight boys who perceive being about the right weight
- (!): Overweight boys who perceive being about the right weight
- Denoted differences between groups are statistically significant at or below the p = .01 level
 Denotes group with a high probability of depressive symptoms according to double jeopardy
Denotes group with a high probability of depressive symptoms according to double jeopardy Denotes group with a high probability of depressive symptoms according to weight congruency
Denotes group with a high probability of depressive symptoms according to weight congruency- ȳ line denotes average probability of depressive symptoms for boys
We first discuss which boys are more likely to report depressive symptoms than normal weight boys who perceive weight as about right (the group expected to have the lowest risk of depressive symptoms). This includes normal weight boys with overweight perceptions and normal weight boys with underweight perceptions (weight pessimists) These boys are also more likely to report depressive symptoms than the average boy. These findings support weight congruency; weight pessimists are at risk of depressive symptoms.
Figure 2 also suggests that overweight boys with overweight perceptions are more likely to report depressive symptoms than overweight boys who perceive being about the right weight (and the average boy). This is consistent with double jeopardy. However, overweight boys with overweight perceptions are not at greater risk of depressive symptoms than normal weight boys with overweight perceptions. Thus, the interpretation that overweight boys with overweight perceptions are doubly disadvantaged with respect to depressive symptoms is tenuous.
The estimated effect of underweight does not vary by weight perceptions. Underweight and perceptions of underweight have independent, not intersectional associations with boys’ depressive symptoms.
Weight, Weight Perceptions & Depressive Symptoms among Girls
Panel B of Table 2 shows estimated associations between weight, weight perceptions and girls’ depressive symptoms. In Model 1, actual weight and depressive symptoms are unrelated. In Model 2, girls who perceive being underweight and overweight (versus about right) have 58% (OR = exp(.454) = 1.575) and 53% (OR = exp(.426) = 1.531) higher odds, respectively, of reporting depressive symptoms. Including actual and perceived weight in Model 3 does not significantly change associations between weight perceptions and depressive symptoms, but it reveals a suppressed association between being overweight and depressive symptoms. Net of confounders, overweight girls’ odds of depressive symptoms are lower than normal weight girls’.
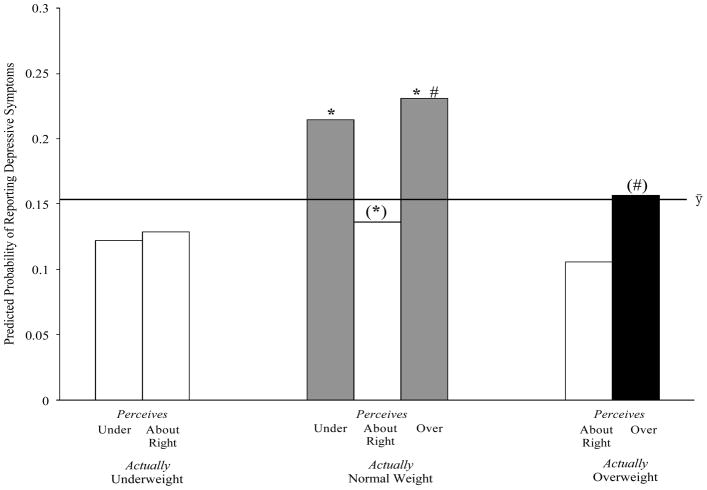
Figure 3 shows the joint influence of weight and weight perceptions on girls’ risk of depressive symptoms. Black bars represent girls with the highest risk of depressive symptoms according to double jeopardy and grey bars represent girls with the highest risk of depressive symptoms according to weight congruency.7 The horizontal line again denotes the predicted probability of reporting depressive symptoms for the “average girl” in our analysis.
Figure 3.
The Predicted Probability of Reporting Depressive Symptoms by Actual Weight and Weight Perceptions among Girls
-
Reference groups for comparison:
- (*): Normal weight girls who perceive being about the right weight
- (#): Overweight girls who are actually overweight
- Denoted differences between groups are statistically significant at or below the p = .01 level
 Denotes group with a high probability of depressive symptoms according to double jeopardy
Denotes group with a high probability of depressive symptoms according to double jeopardy Denotes group with a high probability of depressive symptoms according to weight congruency
Denotes group with a high probability of depressive symptoms according to weight congruency- ȳ line denotes average probability of depressive symptoms for boys
Like Figure 2, Figure 3 suggests that normal weight adolescents’ risk of depressive symptoms depends on weight perceptions. Normal weight girls with overweight and underweight perceptions are more likely to report depressive symptoms than both normal weight girls who perceive being about right and the “average girl”. These findings further support weight congruency.
Figure 3 also presents a contrast between two groups with overweight perceptions. Among these girls, overweight girls have a lower predicted probability of depressive symptoms than normal weight girls. These findings contradict double jeopardy, which predicts that overweight girls with overweight perceptions are doubly disadvantaged by weight and weight perceptions. Instead, this finding supports weight congruency. Weight realists, overweight girls with overweight perceptions, fare better than weight pessimists, normal weight girls with overweight perceptions.
DISCUSSION
This study makes important contributions to literature on mental health consequences of actual weight and weight perceptions and to medical sociology generally. Previous research treats adolescents’ weight and weight perceptions as independent predictors of depressive symptoms. We examine whether the complexity that arises from adolescents simultaneously grappling with both a number on a scale and an image in the mirror better predicts depressive symptoms using two theoretical frameworks as our guide. The study also shows whether it is appropriate to adapt these theories to topics outside of their traditional applications.
Empirically, we find that treating weight and weight perceptions as independent constructs leads to an incomplete picture of associations between actual weight, weight perceptions and depressive symptoms. For example, being overweight is negatively associated with girls’ depressive symptoms, but interactive models suggest that this finding derives from normal weight girls with overweight perceptions having higher probabilities of depressive symptoms than overweight girls with overweight perceptions.8 We also find that normal weight adolescents are not immune to depressive symptoms; their weight perceptions shape their risk of this negative mental health outcome.
Theoretically, weight congruency is a better lens than double jeopardy for understanding how actual weight and weight perceptions are jointly related to adolescent depressive symptoms. Among normal weight adolescents, pessimists are more likely to report depressive symptoms than realists. Moreover, normal weight girls with overweight perceptions (pessimists) are more likely to report depressive symptoms than realists who are doubly disadvantaged by weight and weight perceptions (overweight girls with overweight perceptions).
These findings suggest that health congruency is applicable to topics outside of its traditional application. Perceptions of actual health are not only important for elderly person’s well-being; they also have consequences for adolescents’ well-being. Furthermore, we show that perceptions of a specific health indicator (weight) matter. Future research can extend our findings by examining whether health pessimism matters during other life course stages and whether pessimism about other health conditions influences mental health outcomes.
We find little support for double jeopardy. Overweight boys with overweight perceptions have greater odds of depressive symptoms than overweight boys who perceive being about right, but there is no significant difference between overweight boys with overweight perceptions and normal weight boys with accurate weight perceptions—the most important comparison for a double jeopardy model. Other doubly disadvantaged adolescents (i.e., underweight boys with underweight perceptions and overweight girls with overweight perceptions) also have no greater odds of depressive symptoms than peers with other weight/weight perceptions combinations.
It may be that double jeopardy does not apply to the intersection of objective and perceived characteristics. Prior research using this framework traditionally examines the interaction of two status characteristics (e.g., Dowd and Bengston 1978; Ferraro and Farmer 1996; Mendelson et al. 2008; Smith and Waitzman 1994). However, even studies focused on objective measures often find no support for double jeopardy (Ferraro and Farmer 1996), support in specific contexts only (Mendelson et al. 2008) or among specific groups (Smith and Waitzman 1994). As Ferraro and Farmer (1996) speculate, the theory may be less germane to mental health and mortality than originally hypothesized.
While findings are robust, this study has limitations. We only estimate associations between current weight, weight perceptions and depressive symptoms because these measures are assessed concurrently. Theory and supplemental analysis (described in the methods section) suggest that the intersection of adolescent weight and weight perceptions predicts depressive symptoms, but the reverse is possible given depressed persons’ tendency to have negative self-concepts (e.g., Beck 1976).9 We also cannot assess weight and weight perceptions joint association with depressive symptoms for girls and boys separately by race/ethnicity due to inadequate statistical power.
Despite limitations, this is the first study to show that objective and perceived measures of weight should not be treated as independent predictors of adolescent depressive symptoms. The image in the mirror and number on the scale often differ and are jointly consequential. In a society that provides adolescents with discordant weight messages, understanding the impact of mismatched weight and weight perceptions is critical for clinicians and policy makers interested in alleviating their negative consequences. Identifying a theoretical lens for this process also provides inroads into understanding how self-schemas, perceptions, and objective statuses intersect to shape well-being over the life course.
Acknowledgments
This study uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. To obtain Add Health data files, contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516-2524 (addhealth@unc.edu). No direct support was received from grant P01-HD31921 for this analysis. Instead, the authors received support from the Penn State Population Research Institute, NICHD grant R01 HD40428-02 (PI: Gary Sandefur), and NICHD grant K 12HD055882 (PI: Carol Weisman). Opinions reflect those of the authors and not necessarily those of the granting agencies. We thank Kristin Burnett, Adam Lippert, Claudia Nau, Kristi Williams and Kristina Zeiser for their helpful comments as we prepared this manuscript.
Biographies
Michelle L. Frisco, PhD, is an Assistant Professor of Sociology and Demography at Penn State University. Her research focuses on the intersection of family, health and education during adolescence and early adulthood. Her most recent work focuses on the consequences of obesity for adolescents and young adults, especially as it influences mental health and childbearing.
Jason Houle is a PhD candidate in Sociology and Demography at Penn State University. His research interests include social stratification and mobility, mental health, and the life course. Specific interests include the impact of intra-and intergenerational mobility on mental health and well-being, and mental health during the transition to adulthood.
Molly A. Martin, PhD, is an Assistant Professor of Sociology and Demography at Penn State University. Martin is interested in the intersection of socioeconomic status and family processes for generating inequalities in youth health and well-being.
Appendix A: Weighted Descriptive Statistics, by Gender
| Boys (N=6,557) | Girls (N=6,126) | |||
|---|---|---|---|---|
| Mean or Proportion | SD | Mean or Proportion | SD | |
| Depressive symptoms | .110 | .176 | ||
| Actual Weight, (ref. = normal) | .659 | .701 | ||
| Underweight | .042 | .030 | ||
| Overweight | .299 | .268 | ||
| Weight Perceptions (ref. = about right) | .577 | .504 | ||
| Underweight perceptions | .202 | .107 | ||
| Overweight perceptions | .221 | .389 | ||
| Sociodemographic Background | ||||
| Race/Ethnicity (ref. = White) | .680 | .698 | ||
| Black | .153 | .146 | ||
| Latino/a | .126 | .119 | ||
| Asian/Pacific Islander | .041 | .037 | ||
| Nativity (1 = U.S. born) | .941 | .933 | ||
| Age (in years) | 16.083 | 1.658 | 15.800 | 1.598 |
| Income percentile group | 2.140 | 1.540 | 2.172 | 1.594 |
| Parent’s highest education level | 5.378 | 1.709 | 5.414 | 1.726 |
| Family Structure, lives with: (ref. = both parents) | .557 | .575 | ||
| Parent and a stepparent | .167 | .156 | ||
| Single parent | .230 | .235 | ||
| Other | .045 | .034 | ||
| Other Control Variables | ||||
| At least one parent is obese (1 = yes) | .227 | .224 | ||
| High Level of Physical Activity (1 = yes) | .753 | .692 | ||
| Fair/poor self-assessed health (1 = yes) | .060 | .073 | ||
- Source: The National Longitudinal Study of Adolescent Health
- Parent’s highest education level is an ordinal variable ranging from 1 (no schooling) to 8 (post-college education) with a mean value of 5.4, which represents that at least 1 parent attended some postsecondary institution. Family Income percentile categories range from 1 to 6 with an average value of 2.4, which represents a family income in the 50th percentile of the distribution.
Footnotes
BMI percentiles and CDC weight categories are widely used because they account for growth, development, sex and height and are time- and cost-effective. They are relatively reliable and correlate well with other body fatness assessments (e.g., dual energy x-ray absorptiometry) (CDC 2003).
Few variables required substantial imputation. Height and weight, weight perceptions, and depressive symptoms were imputed for 0.9% (n=114), 0.03% (n=43), and .34% (n=43) of cases, respectively. All respondents reported age and family structure. Missing data on other covariates ranged from .01% to 8.20%.
Controversy exists over operationalizing depressive symptoms using the CES-D scale. Scholars advocate our approach (Wheaton 2001) and using the scale as a continuous or log-transformed variable (Mirowsky and Ross 2002). Each measure taps different mental health issues. Dichotomous measures capture persons likely distressed to the point of impairment (Schwartz 2002; Wheaton 2001). Most Add Health studies dichotomize scale scores using our cut-point or 22(boys) and 24 (girls) (e.g., Goodman 1999). One other study uses 16 (Needham and Crosnoe 2005). To test findings’ sensitivity to depressive symptoms operationalizations, we predicted it using alternative operationalizations. All results are substantively and statistically similar.
Waves I and II include height and weight. We use Wave II measures because Wave I measures are self-reported, making them more subjective than measured weight, confounded with weight perceptions (Brener et al. 2004), and prone to misreports by respondents dissatisfied with their weight (Elgar et al. 2005). Self-reported data introduces unnecessary error into the study and diminishes precision of statistical estimates.
Significant gender differences are determined by regression weight perceptions on gender separately for each weight category.
We omit bars representing underweight boys with overweight perceptions (N=15) and overweight boys with underweight perceptions (N=64). These extreme cases of weight over- and underestimation are rare and may indicate body disorders (Brener et al. 2004).
We omit bars representing underweight girls with overweight perceptions (N=22) and overweight girls with underweight perceptions (N=33) for reasons described in footnote 6.
Prior research suggests alternative explanations including overweight adolescents’ ability to find niches in certain settings (Crosnoe and Muller 2004). Accounting for weight schemas may also lead to unexpected links between weight and depressive symptoms given internally and externally mediated body-mind connections (Hayes and Ross 1986).
Exploratory analyses predicted a variable indicating the Wave II intersection of weight and weight perceptions using Wave I depressive symptoms. Among boys, depressive symptoms predicted greater odds of being normal weight with underweight perceptions and underweight with underweight perceptions (versus normal weight and perceiving weight as about right). Among girls, depressive symptoms predicted greater odds of being normal weight with overweight perceptions and overweight with overweight perceptions.
References
- Allison Paul. Missing Data. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- Bearman Peter S, Jones Jo, Richard Udry J. The National Longitudinal Study of Adolescent Health: Research Design. Carolina Population Center; Chapel Hill, NC: 1997. [Google Scholar]
- Beck Aaron T. Cognitive Theory and Emotional Disorder. New York: International Universities Press; 1976. [Google Scholar]
- Brener Nancy D, Eaton Danice K, Lowry Richard, McManus Tim. The association between weight perception and BMI among high school students. Obesity Research. 2004;12:1866–1874. doi: 10.1038/oby.2004.232. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. BMI-for-Age. Division of Nutrition and Physical Activity; 2003. [Google Scholar]
- Chipperfield Judith G. Incongruence Between Health Perceptions and Health Problems: Implications for Survival Among Seniors. Journal of Aging and Health. 1993;5:475–496. [Google Scholar]
- Crandall Christian, Schiffhauer Kristin. Anti-fat Prejudice: Beliefs, Values, and American Culture. Obesity Research. 1998;6:458–460. doi: 10.1002/j.1550-8528.1998.tb00378.x. [DOI] [PubMed] [Google Scholar]
- Crosnoe Robert, Muller Chandra. Body mass index, academic achievement, and school context: examining the educational experiences of adolescents at risk of obesity. Journal of Health & Social Behavior. 2004;45:393–407. doi: 10.1177/002214650404500403. [DOI] [PubMed] [Google Scholar]
- Daniels J. Weight and weight concerns: are they associated with reported depressive symptoms in adolescents. Journal of Pediatric Health Care. 2005;19:33–41. doi: 10.1016/j.pedhc.2004.07.007. [DOI] [PubMed] [Google Scholar]
- Dejong William. The Stigma of Obesity: The Consequences of Naïve Assumptions Concerning the Causes of Physical Deviance. Journal of Health and Social Behavior. 1980;21:75–87. [PubMed] [Google Scholar]
- Dowd James J, Bengston Vern L. Aging in Minority Populations: An Examination of the Double Jeopardy Hypothesis. Journal of Gerontology. 1978;33:427–436. doi: 10.1093/geronj/33.3.427. [DOI] [PubMed] [Google Scholar]
- Elgar Frank, Roberts Chris, Tudor-Smith Chris, Moore Laurence. Validity of Self-Reported Height and Weight as Predictors of Bias in Adolescents “. Journal of Adolescent Health. 2005;37:371–375. doi: 10.1016/j.jadohealth.2004.07.014. [DOI] [PubMed] [Google Scholar]
- Ferraro Kenneth F, Farmer Melissa M. Double Jeopardy to Health Hypothesis for African Americans: Analysis and Critique. Journal of Health and Social Behavior. 1996;37:27–43. [PubMed] [Google Scholar]
- Frisco Michelle, Houle Jason N, Martin Molly. Adolescent Weight and Depressive Symptoms: For Whom is Weight a Burden? Social Science Quarterly. 2009;90:1019–1038. doi: 10.1111/j.1540-6237.2009.00676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman Elizabeth. The Role of Socioeconomic Status Gradients in Explaining Differences in US Adolescents’ Health. American Journal of Public Health. 1999;89:1522–1528. doi: 10.2105/ajph.89.10.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmatz Morton G, Gronendyke James, Thomas Todd. The Underweight Male: The Unrecognized Problem Group of Body Image Research. The Journal of Obesity and Weight Regulation. 1985;4:258–267. [Google Scholar]
- Hayes Diane, Ross Catherine E. Body and Mind: The Effect of Exercise, Overweight, and Physical Health on Psychological Well-Being. Journal of Health and Social Behavior. 1986;27:387–400. [PubMed] [Google Scholar]
- Hong Tantina B, Zarit Steven H, Malmberg Bo. The Role of Health Congruence in Functional Status and Depression. The Journals of Gerentology. 2004;59B:151–157. doi: 10.1093/geronb/59.4.p151. [DOI] [PubMed] [Google Scholar]
- Idler Ellen L, Hudson Shawna V, Leventhal Howard. The Meanings of Self-Ratings of Health: A Qualitative and Quantitative Approach “. Research on Aging. 1999;21:458–476. [Google Scholar]
- Langenkamp Amy, Frisco Michelle L. Family Transitions and Adolescent Severe Emotional Distress: The Salience of Family Context. Social Problems. 2008;55:238–253. doi: 10.1525/sp.2008.55.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latner Janet D, Stunkard Albert J, Terence Wilson G. Stigmatized Students: Age, Sex, and Ethnicity Effects in the Stigmatization of Obesity. Obesity Research. 2005;13:1226–1231. doi: 10.1038/oby.2005.145. [DOI] [PubMed] [Google Scholar]
- Markus Hazel. Self-schemata and the processing of information about the self. Journal of Personality and Social Psychology. 1977;35:63–78. [Google Scholar]
- Markus Hazel, Hamill Ruth, Sentis Keith P. Thinking Fat: Self-Schemas for Body Weight and the Processing of Weight Relevant Information. Journal of Applied Social Psychology. 1987;17:50–71. [Google Scholar]
- Martin Molly A, Frisco Michelle L, Ashleigh L. Gender and Race/Ethnic Differences in Inaccurate Weight Perceptions among U.S. Adolescents. Women’s Health Issues. 2009;19:292–299. doi: 10.1016/j.whi.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod Jane D, Owens Timothy J. Psychological Well-Being in the Early Life Course: Variations by Socioeconomic Status, Gender, and Race/Ethnicity. Social Psychology Quarterly. 2004;67:257–278. [Google Scholar]
- Mendelson Tamar, Kubzansky Laura D, Datta Geetanjali D, Buka Stephen L. Relation of Female Gender and Low Socioeconomic Status to Internalizing Symptoms Among Adolescents: A case of double jeopardy? Social Science and Medicine. 2008;66:1284–1986. doi: 10.1016/j.socscimed.2007.11.033. [DOI] [PubMed] [Google Scholar]
- Miller Carol T, Kaiser Cheryl R. A Theoretical Perspective on Coping with Stigma. Journal of Social Issues. 2001;57:73–92. [Google Scholar]
- Mirowsky John, Ross Catherine E. Measurement for a Human Science. Journal of Health and Social Behavior. 2002;43:152–170. [PubMed] [Google Scholar]
- Needham Belinda L, Crosnoe Robert. Overweight Status and Depressive Symptoms During Adolescence. Journal of Adolescent Health. 2005;36:48–55. doi: 10.1016/j.jadohealth.2003.12.015. [DOI] [PubMed] [Google Scholar]
- Pearlin Leonard I. The Sociological Study of Stress. Journal of Health and Social Behavior. 1989;30:241–256. [PubMed] [Google Scholar]
- Pesa Jacqueline A, Syre Thomas R, Jones Elizabeth. Psychosocial Differences Associated with Body Weight Among Female Adolescents: The Importance of Body Image. Journal of Adolescent Health. 2000;26:330–337. doi: 10.1016/s1054-139x(99)00118-4. [DOI] [PubMed] [Google Scholar]
- Peterson Christopher, Bossio Lisa. Health and Optimism: New Research on the Relationship between Positive Thinking and Physical Well-being. New York: Free Press; 1991. [Google Scholar]
- Plomin Robert, Scheier Michael F, Bergeman CS, Pedersen NL, Nesselroade JR, McClern GE. Optimism, Pessimism, and Mental Health: A Twin/Adoption Analysis. Personality and Individual Differences. 1992;12:921–930. [Google Scholar]
- Puhl RM, Brownell KD. Psychosocial Origins of Obesity Stigma: Toward Changing a Powerful and Pervasive Bias. Obesity Reviews. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- Radloff Lenore Sawyer. The CES-D Scale: A self-report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Richardson Stephen A, Goodman Norman, Hastorf Albert H, Dornbusch Sanford M. Cultural Uniformity in Reaction to Physical Disabilities. American Sociological Review. 1961;26:241–247. [Google Scholar]
- Royston Patrick. Multiple Imputation of Missing Values: Update of Ice. Stata Journal. 2005;5:527–536. [Google Scholar]
- Schwartz Sharon. Outcomes for the Sociology of Mental Health. Journal of Health and Social Behavior. 2002;43:223–235. [PubMed] [Google Scholar]
- Smith Ken R, Waitzman Norman J. Double Jeopardy: Interaction Effects of Marital and Poverty Status on the Risk of Mortality. Demography. 1994;31:487–507. [PubMed] [Google Scholar]
- Strauss Richard, Pollack Harold A. Social Marginalization of Overweight Children. Archives of Pediatrics and Adolescent Medicine. 2003;157:746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- Swallen Karen, Reither Eric N, Haas Steven A, Meier Ann M. Overweight, Obesity, and Health-Related Quality of Life Among Adolescents: The National Longitudinal Study of Adolescent Health. Pediatrics. 2005;115:340–347. doi: 10.1542/peds.2004-0678. [DOI] [PubMed] [Google Scholar]
- Swanholm Eric, Vosovick Mark, Chwee-Lyee Chng. Pessimism, Trauma, Risky Sex: Covariates of Depression in College Students. American Journal of Health Behavior. 2009;33:309–318. doi: 10.5993/ajhb.33.3.9. [DOI] [PubMed] [Google Scholar]
- Taylor Shelley E, Brown Jonathon. Illusion and Well-being: A Social Psychological Perspective on Mental Health. Psychological Bulletin. 1988;103:193–210. [PubMed] [Google Scholar]
- Wardle Jane, Cooke Lucy. The impact of obesity on psychological well-being. Best practice and research. Clinical endocrinology and metabolism. 2005;19:421–40. doi: 10.1016/j.beem.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Wheaton Blair. The Role of Sociology in the Study of Mental Health... and the Role of Mental Health in the Study of Sociology. Journal of Health and Social Behavior. 2001;42:221–234. [PubMed] [Google Scholar]