Abstract
Objective:
We undertook this study to assess the clinical profile and outcome determinants of different snake envenomation as well as to assign species-specific severity grade to different cases based on clinico – laboratory evidence scale.
Materials and Methods:
A prospective clinico – epidemiologic evaluation for outcome determinants of snakebite envenomation was carried out based on a clinico – laboratory severity grading scale, among 76 patients over a period of 2 years, in a tertiary care hospital in southern India.
Results:
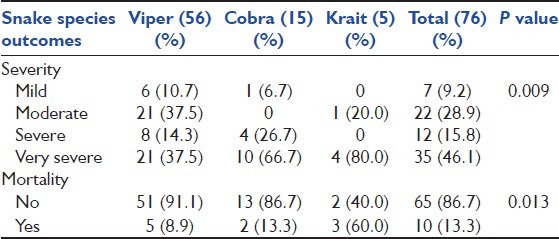
Majority of patients were male agricultural workers (53.9%) followed by housewives (19.7%), and students (9.2%). Occurrence of viper snake envenomation with hemotoxic syndrome (73.68%) was highest followed by cobra and krait envenomation with neurotoxic (19.73%) and hemo – neurotoxic (5.3%) syndrome, respectively. On the contrary, maximum mortality and severity was seen in krait (60%) followed by cobra (13.33%) and viper (8.9%) envenomation. The average dose of anti-snake venom (ASV) administered varied from 9.83 (±7.22) to 20.25 (±4.92) vials throughout grade I to IV in all snake species envenomation. An increase in severity grade, ASV dose, and mortality were observed with the corresponding delay in ‘bite to needle time.’ Also, initial traditional treatments and krait species envenomation were significantly associated with higher grades of severity and mortality.
Conclusion:
There is an urgent need to spread awareness among the community for avoidance of traditional treatment and any delay in medical intervention in snakebite incidents.
Keywords: Antivenins, envenomation, ophitoxaemia, severity grade, snakebite
Introduction
Snake envenomation is a serious medical crisis, wherein the spectrum of injury can vary from local tissue damage to involvement of almost all vital organs of the body. Clinico - toxicologically, nature of snake envenomation is categorized into hemotoxic, neurotoxic, and myotoxic syndromes.[1] Most snakebites are harmless and are caused by non-poisonous species. Nonetheless, of the 3,000 different species of snakes, about 450 are found to be dangerous for humans worldwide.[2] Out of 216 Indian snake species, 52 are poisonous.[3,4] Among these, there are 4 major poisonous species viz. cobras or Naja naja, krait or Bungarus caeruleus, Russell's viper or Daboia russelli, and saw-scaled viper or Echis carinatus.[5] World health organization (WHO) has recognized snakebite as neglected and important public health problem in rural areas of tropical and subtropical countries situated in Asia, Africa, Oceania, and Latin America.[6] According to the same WHO report, the global annual incidence of envenoming and resulting deaths ranges from a minimum of 421,000 to a maximum of 1,841,000 and 20,000 to 94,000, respectively. Also, it is mentioned that the highest burden of snakebites is in South Asia, Southeast Asia, and sub-Saharan Africa. Among these, India has the highest incidence of snakebite-resulted mortality, ranging from 13,000 to 50,000 cases annually.[7,8] Attributes for such a high mortality due to snakebite are scarcity of anti - snake venoms (ASV), difficulties with rapid access to health centers, poor health services, and traditional treatments.[9,10] Furthermore, wrong/erroneous identification of the snake species also leads to inappropriate/inadequate treatment and outcomes.[8] At presentation, a snake-bitten victim can be promptly diagnosed and treated if the clinical syndrome of snakebites are well-defined and pre - distinguished based on analysis of a series of reliably identified bites.[8] Thus, we undertook this priority area of research to study the clinical profile and outcome determinants of different snake envenomation as well as attempted to assign species-specific severity grade to different cases based on clinico – laboratory evidence scale.
Materials and Methods
We conducted a hospital-based prospective cohort study in patients admitted to a 2032-bedded tertiary referral center in South India during June 2008 to May 2010. A written informed consent was obtained from each subject included in the study. Ethical approval for the study was obtained from the hospital ethics committee prior to the commencement of the study. The catchment area for the study comprised of whole Udupi district in Karnataka, India which spreads over 929 square km, with a population of 529,225.
It is the hospital policy to admit all snakebite patients for observation, and patients with “dry bites” were discharged after 24 hours. Snakebite and species identification were confirmed by a reliable history from patients, eye witnesses, from the patient's attendants, and presence of fang marks and signs of local and systemic envenomation. Snakes brought by the patient to the hospital were identified by forensic medicine experts. All patients were interviewed using a standardized questionnaire to maintain a record of patient's history relevant to snakebite envenomation. Information about the victim, its management (first-aid/traditional treatment), time between bite, and administration of ASV was obtained in each case. Only the snakebite cases with signs of envenomation were included for the study. Non-poisonous snakebites and poisonous snakebite cases without envenomation were excluded. Patients were followed for 24 hours for “dry bite” confirmation. Patients with signs of envenomation were administered ASV manufactured by ViNS bioproducts limited, Kothur (Mandal), Mahaboobnagar (Dist.), Andhra Pradesh, India. This ASV is a sterile preparation containing equine immunoglobulin fragments F (ab’) 2 freeze-dried powder when reconstituted to 10 ml of sterile water for injections I.P. supplied along with the vial, each 1 ml has capacity of specifically neutralizing the venom of these species of snake: –0.60 mg of dried Indian Cobra (Naja naja) venom, 0.45 mg of dried Common Krait (Bungarus Caeruleus) venom, 0.60 mg of dried Russell's viper (Dabioa russelli) venom, and 0.45 mg of dried Saw – scaled Viper (Echis carinatus) venom. These anti-snake venom equine immunoglobulin and their derivatives are obtained from serum of healthy equines immunized against venoms of the above species of snakes. Further, patients were managed as per the clinical judgment of consultant based on the nature of envenomation and the severity.
An attempt was made to identify the species of the snake involved and assign the degree of envenomation on a grading scale dependent on clinical symptoms/signs and laboratory parameters [Appendix 1].[11] Two viperidae species were combined for analysis purpose because of inability to differentiate from history or laboratory data. The average quantity of ASV required in each grade of severity was estimated. We also tried to determine the risk factors associated with poor outcomes in these patients. Patients who had grade III and IV severity and who succumbed to the complications were considered to have poor outcomes. The primary outcome was the severity of the snakebite as per grading and death. The secondary outcomes assessed were the dose of ASV administered and the duration of the hospital stay. All data were analyzed using the SPSS 15.0 statistical software package for Windows.
Appendix 1.
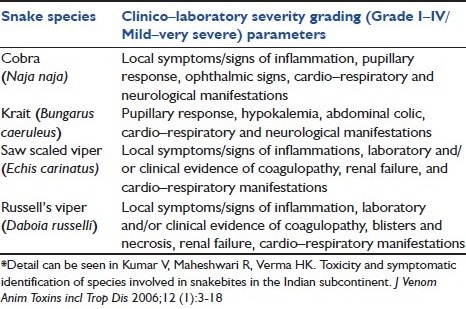
*Summary of species–specific severity grading of Indian snake envenomation based on clinico–laboratory profile
Results
A total of 130 cases of snakebites had presented to the hospital emergency department during the study period. Seventy-six patients [46 (60.52%) male, 30 (39.47%) female] satisfying the inclusion criteria were included in the present study. The rest of 54 cases had no signs of envenomation and were discharged after 24 hours. All the patients were in the age range of 16 to 82 years, with 61% cases below 50 years age. Occupationally, male agriculture worker [41 (53.95%)] were most affected followed by housewives [15 (19.74%)] and students [7 (9.21%)]. Majority of the patients had grade IV severity [35 (46.05%)] followed by grade II [22 (28.94%)] and III [12 (15.78%)]. Most of the cases occurred during the month of June to December. Seventy-five percent of patients were bitten between 6 PM to 12 AM, whereas 25% cases between 12 AM to 6 PM. Most of the bites were on the lower limb (77.63%); upper limbs were bitten in 21.95% of victims. Only one patient was bitten by krait on the trunk while sleeping over the floor.
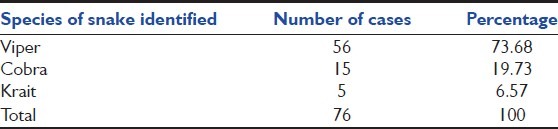
Based on the symptoms, signs, and laboratory parameters, as described by Kumar et al. 2006,[11] we attempted to identify the species of the snake and found viper as the most common species identified in 73.68% of the cases [Table 1]. Hemotoxic (defined as prolongation of PT, INR, and APTT, reversal was considered with normalization of PT, INR, and APTT) and neurotoxic nature of envenomation were observed in 56 (73.68%) and 15 (19.73%) cases respectively, whereas 4 (5.26%) cases had both hemotoxic and neurotoxic manifestations.
Table 1.
Species identified based on the grading and severity scale[11]
Clinical characteristics, complications, and severity grading of viper envenomation
Viper bite was characterized by severe local symptoms. Swelling and pain at the bite site were the commonest symptoms seen in 51 (91.07%) and 49 (87.5%) patients, respectively. Persistent bleeding from fang wounds was seen in 23 (41.07%) patients. Other bleeding manifestations such as bleeding gums in 4 (7.14%), hematemesis in 2 (3.57%), hematuria in 1 (1.78%) cases were less common. Cellulitis (Presence of localized pain, erythema, and swelling) and coagulopathy were the most common complications seen in 44 (78.57%) and 35 (62.50%) patients, respectively. Oliguria and renal failure occurred in 16 (28.57%) and 12 (21.42%) patients, respectively. Other complications were sepsis (Systemic inflammatory response syndrome with proven or suspected microbial etiology) due to wound infection in 8 (14.28%), necrotizing fasciitis in 6 (10.71%), compartmental syndrome (presence of local neurovascular compromise as judged clinically; compartmental pressure measurements were not performed) with surgical intervention requirement in 3 (5.35%), and acute respiratory distress syndrome (ARDS) in 1 (1.78%) cases. The time between bite and ASV administration varied from 15 minutes to 36 hours, with majority of patients [32 (57.14%)] presenting within 6 hours. The ASV dose, duration of hospital stay, mortality, and severity grades were found to be increased with corresponding increase in ‘bite to needle time.’ ASV dose administered was 9.83 (±7.22), 14.59 (±7.75), 15.87 (±13.67), and 14.75 (±7.91) vials in grade I, II, III, and IV severity, respectively [Table 2].
Table 2.
Characteristics of patients in different grades of Viper (V), Cobra (C), and Krait (K) envenomation
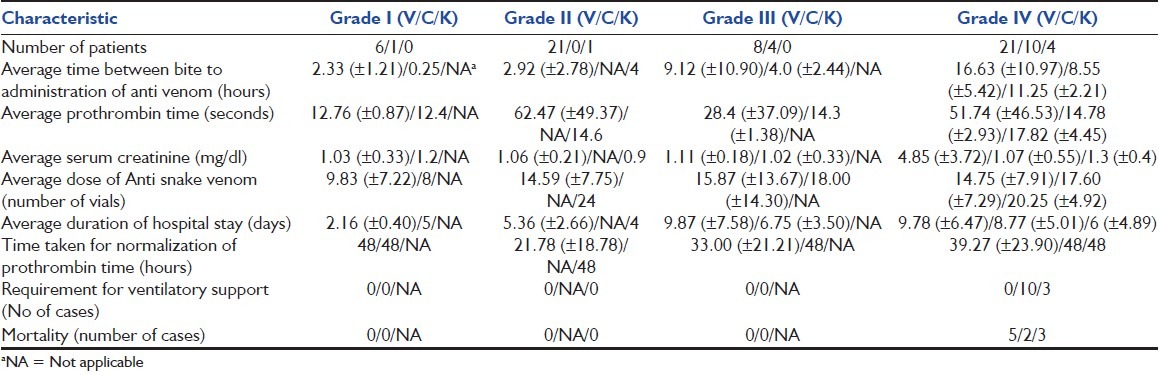
Clinical characteristics, complications, and severity grading of cobra envenomation
Pain followed by swelling and ptosis were seen in 11 (73.33%) and 13 (86.66%) patients with cobra bite, respectively. Difficulty in breathing and weakness of the limbs were seen in 11 (73.33%) patients. Diplopia, dysphagia, and dysarthria were seen in 4 (26.66%), 3 (20%), and 1 (6.66%) patients, respectively. Cellulitis seen in 12 (80%) and respiratory paralysis in 11 (73.33%) patients were the most common complications followed by sepsis and necrotizing fasciitis, which were seen in 3 (20%) patients. Renal failure, persistent vegetative state following cardiac arrest, refractory hypotension, and gangrene were the other complications occurred in 1 (6.66%) patient. As seen with viper bites, in cobra envenomation also, the grade of severity, duration of hospital stay, dose of ASV, and mortality increased with the corresponding increase in ‘bite to needle time.’ The average ASV dose administered was 18.00 (±14.30) and 17.60 (±7.29) vials in grade III and IV severity, whereas in only one case of grade I severity, it was 8 vials [Table 2].
Clinical characteristics, complications, and severity grading of krait envenomation
Abdominal pain was one of the common symptom in 4 (80%) patients followed by neurological symptoms like dyspnea in 4 (80%), ptosis in 3 (60%), dysphagia in 2 (40%), and oliguria in 1 (20%) patient. Respiratory paralysis was seen in 4 (80%) patients. Hypokalemia was seen in 3 (60%) patients. Two (40%) patients presented with coma, and 1 (20%) patient had renal failure. Of the 5 patients with krait bite, 4 (80%) presented with grade IV severity whereas, 1 (20%) with grade II severity. The average time between bite to administration of ASV was 11.25 (±2.21) hours in patients with grade IV severity. The average dose of ASV used was 20.25 (±4.92) vials in patients in grade IV severity, whereas in only 1 patient with grade II severity, the ASV dose administered was 24 vials. Three (60%) patients’ required ventilator support and all of them expired [Table 2].
Determinants of outcome
An initial visit to a traditional healer was statistically associated with an increased risk of death with an odds ratio of 4.22. Of the 13 (17.1%) patients who received traditional forms of treatment, 11 (14.47%) had grade IV severity and 4 (5.26%) expired. Delay in presentation to hospital was significantly longer for victims with higher grades (III and/or IV) of severity and mortality, which makes it a risk factor associated with poor outcome [Table 3]. Severity grade was found to be increased with corresponding increase in ‘bite to needle time.’ Mortality proportion was higher in patients with late presentation (>24 hours) than early presentation (<6 hours); P value was significant (<0.01). Krait bite itself was found to be risk factor with 60% mortality. The mortality and corresponding proportion was calculated for each species [Table 4]. Chi-square test for trend was used to find the association between the severity grading and the species. Since P = 0.009, there is a significant difference in distribution of grading between the species. Chi-square test was used to compare the mortality rates between the species. Since P = 0.013, there is a significant difference in the mortality rates between the species.
Table 3.
Correlation between time of administration of anti-snake venom and outcome
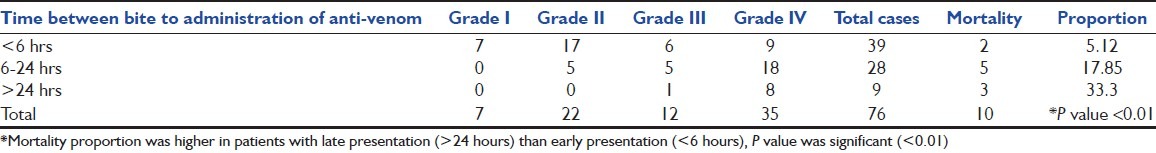
Table 4.
Comparison of species wise severity and mortality outcomes
Discussion
The present study was carried out on 76 cases of snakebite envenomation. Male preponderance seen in our study is in close agreement with earlier studies[12–14] and may be attributed to their life styles involving outdoor activities and occupational exposure as farmers or herdsmen. Young male agricultural workers were the most common affected group in our study, making snakebite an occupational hazard. We observed the occurrence of most of the cases during the month of June to December, which is the monsoon season with agricultural activity in our study region, and also the time of increased activity of snakes as they come out of their shelters.[15] Maximum events of envenomation were seen with viper snakebite followed by cobra and krait species, whereas the proportion of mortality was highest in krait followed by cobra and viper species. This indicates that our study region i.e., Udupi district of Karnataka state in southern India is more prevalent for viper snakes envenomation than other snakes. Distribution of different snake species in a given geographic region is dependent on various environmental and climatic conditions viz. rainfall, altitude, vegetation, and abundance of preferred prey etc.[16,17] Hemotoxic syndrome was the commonest snakebite syndrome, attributable to the prevalence of viper snake species (hallmark for hemotoxic syndrome), followed by neurotoxic syndrome of cobra bites (hallmark for neurotoxic syndrome).[8,18] Simultaneous neurotoxic and hemotoxic manifestations in patients were attributable to krait envenomation.[10] These results are very similar to other reports from the neighboring states of Karnataka and other states in India.[10,19,20]
Severe local symptoms observed among viper envenomation were also in accordance with other studies.[19,21–23] Swelling and pain at the site of the bite were the most common symptoms among the patients with viper envenomation. Cellulitis and coagulopathy were found to be the most common complications with viper envenomation in accordance with other studies.[22–24] Renal failure was attributable to tubular damage by venom, hemoglobinuria, rhabdomyolysis, hypotension, and renal microthrombi formation causing acute tubular necrosis.[23,25,26]
The rationale for the use of ASV is well-defined; doses required in different envenomation situation vary greatly and are subject to the severity grade and the snake species associated.[3,18,27] In the present study, the severity grade increased as the time delay between the occurrence of bite and ASV administration i.e., ‘bite to needle time’ increased. Severity grade was also found to be in direct proportional relation with the duration of hospital stay, the mean effective neutralizing dose of ASV, the time taken for normalization of coagulation abnormalities as well as the mortality. Possibility of venom's direct toxicity on organ system is pointed by the direct proportionality between incidences of complication with venom neutralization time and delay in ASV administration.[9,28,29] Hence, an early institution of ASV is beneficial in preventing complications.
As observed with viper, in cobra envenomation also, the severity grade increased as the bite to needle time increased. Patients, who presented late, resulted in delayed administration of ASV and required more aggressive therapies like mechanical ventilator support. Of the 5 patients, identified to have bitten by Krait, 4 had grade IV severity and 3 expired. Since Krait bites are usually painless with mild local symptoms,[30] victims might not have recognized the bite and/or have not been sufficiently compelled to seek treatment immediately, resulted in delayed ASV administration and higher mortality. Patients with traditional treatments were at a higher risk of complications and mortality with an odds ratio of 4.22. Consultation with traditional healers is a classic cause of delay, which exposes the patient to useless or dangerous interventions.[7,30] Thus, there is an urgent need to spread awareness among the community for avoidance of any delay and traditional treatment in snakebite incidences. Coagulopathy could not be extensively evaluated in this study, and 2 viperidae species were studied together as it was not possible to differentiate by history and/or laboratory details, which are the limitations of the present study.
To summarize, initial consultation with traditional healers, delayed ASV administration, and krait bites were the determinants of poor outcome in our study. Majority of snake envenomation resulted from hemotoxic viper snakebites and presented with grade IV severity. Viper envenomation was also associated with significant local reaction and systemic manifestations due to coagulation abnormalities. The presence of neurological symptoms and signs with absence of local reaction, presence of abdominal pain, and hypokalemia favors a diagnosis of krait envenomation. Avoidance of consultation with traditional healers as well as prompt medical intervention can reduce both the morbidity and mortality in snakebite envenomation cases.
Ethical Approval
The study was approved by the Kasturba hospital, Manipal ethics committee.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Bhattacharya P, Chakraborty A. Neurotoxic snake bite with respiratory failure. Indian J Crit Care Med. 2007;11:161–4. [Google Scholar]
- 2.Gold BS, Dart RC, Barish RA. Bites of venomous snakes. N Engl J Med. 2002;347:347–56. doi: 10.1056/NEJMra013477. [DOI] [PubMed] [Google Scholar]
- 3.Bawaskar HS. Snake venoms and antivenoms: Critical supply issues. J Assoc Physicians India. 2004;52:14–7. [PubMed] [Google Scholar]
- 4.Meenatchisundaram S, Parameswari G, Michael A, Ramalingam S. Neutralization of the pharmacological effects of Cobra and Krait venoms by chicken egg yolk antibodies. Toxicon. 2008;52:221–7. doi: 10.1016/j.toxicon.2008.04.179. [DOI] [PubMed] [Google Scholar]
- 5.Waghmare A, Deopurkar RL, Salvi N, Khadilkar M, Kalolikar M, Gade SK. Comparison of Montanide adjuvants, IMS 3012 (Nanoparticle), ISA 206 and ISA 35 (Emulsion based) alongwith incomplete Freund's adjuvant for hyperimmunization of equines used for production of polyvalent snake antivenom. Vaccine. 2009;27:1067–72. doi: 10.1016/j.vaccine.2008.11.103. [DOI] [PubMed] [Google Scholar]
- 6.who. int [Internet]. Neglected tropical diseases: Snakebite. [Last updated on 2012 Apr 06; Last accessed on 2012 May 26]. Available from: http://www.who.int/neglected_diseases/diseases/snakebites/en/index.html .
- 7.Alirol E, Sharma SK, Bawaskar HS, Kuch U, Chappuis F. Snake bite in South Asia: A review. PLoS Negl Trop Dis. 2010;4:e603. doi: 10.1371/journal.pntd.0000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warrell DA. Snake bite. Lancet. 2010;375:77–88. doi: 10.1016/S0140-6736(09)61754-2. [DOI] [PubMed] [Google Scholar]
- 9.Narvencar K. Correlation between timing of ASV administration and complications in snake bites. J Assoc Physicians India. 2006;54:717–9. [PubMed] [Google Scholar]
- 10.Paul V, Pratibha S, Prahlad KA, Earali J, Francis S, Lewis F. High-dose anti-snake venom versus low-dose anti-snake venom in the treatment of poisonous snake bites-a critical study. J Assoc Physicians India. 2004;52:14–7. [PubMed] [Google Scholar]
- 11.Kumar V, Maheshwari R, Verma HK. Toxicity and symptomatic identification of species involved in snakebites in the Indian subcontinent. J Venom Anim Toxins incl Trop Dis. 2006;12:3–18. [Google Scholar]
- 12.Sharma SK, Khanal B, Pokhrel P, Khan A, Koirala S. Snakebite-reappraisal of the situation in Eastern Nepal. Toxicon. 2003;41:285–9. doi: 10.1016/s0041-0101(02)00289-1. [DOI] [PubMed] [Google Scholar]
- 13.Brunda G, Sashidhar RB. Epidemiological profile of snake-bite cases from Andhra Pradesh using immunoanalytical approach. Indian J Med Res. 2007;125:661–8. [PubMed] [Google Scholar]
- 14.Chattopadhyay MD, Sukul B. A profile of fatal snake bite cases in the Bankura district of West Bengal. J Forensic Leg Med. 2011;18:18–20. doi: 10.1016/j.jflm.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 15.Gutiérrez JM, Theakston RD, Warrell DA. Confronting the neglected problem of snake bite envenoming: The need for a global partnership. PLoS Med. 2006;3:e150. doi: 10.1371/journal.pmed.0030150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Silva A. Venomous snakes, their bites and treatment in Sri Lanka. In: Gopolakrishnakoon P, Chou LM, editors. Snakes of medical importance (Asia-Pacific region) Singapore: Venom and Toxin Research Group, National University; 1990. pp. 479–556. [Google Scholar]
- 17.Kasturiratne A, Pathmeswaran A, Fonseka MM, Lalloo DG, Brooker S, de Silva HJ. Estimates of disease burden due to land-snake bite in Sri Lankan hospitals. Southeast Asian J Trop Med Public Health. 2005;36:733–40. [PubMed] [Google Scholar]
- 18.Sharma N, Chauhn S, Faruqi S, Bhat P, Varma S. Snake envenomation in a north Indian hospital. Emerg Med J. 2005;22:118–20. doi: 10.1136/emj.2003.008458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Punde DP. Management of snake-bite in rural Maharashtra: A 10-year experience. Natl Med J India. 2005;18:71–5. [PubMed] [Google Scholar]
- 20.Adhisivam B, Mahadevan S. Snakebite envenomation in India: A rural medical emergency. Indian Pediatr. 2006;43:553–4. [PubMed] [Google Scholar]
- 21.Chippaux JP. [Venomous and poisonous animals. II. Viper bites] Med Trop (Mars) 2006;66:423–8. [PubMed] [Google Scholar]
- 22.Hayat AS, Khan AH, Shaikh TZ, Ghouri RA, Shaikh N. Study of snake bite cases at Liaquat University Hospital Hyderabad/Jamshoro. J Ayub Med Coll Abbottabad. 2008;20:125–7. [PubMed] [Google Scholar]
- 23.Mahasandana S, Rungruxsirivorn Y, Chantarangkul V. Clinical manifestations of bleeding following Russell's viper and Green pit viper bites in adults. Southeast Asian J Trop Med Public Health. 1980;11:285–93. [PubMed] [Google Scholar]
- 24.Bandyopadhyay SK, Ghosh S, Bandyopadhyay R, Dutta A. Prognostic factors in haemotoxic viper bite: Analysis of data from a referral hospital. J Indian Med Assoc. 2009;107:12–3. [PubMed] [Google Scholar]
- 25.Danis R, Ozmen S, Celen MK, Akin D, Ayaz C, Yazanel O. Snakebite-induced acute kidney injury: Data from Southeast Anatolia. Ren Fail. 2008;30:51–5. doi: 10.1080/08860220701742021. [DOI] [PubMed] [Google Scholar]
- 26.Sitprija V. Snakebite nephropathy (Review article) Nephrology (Carlton) 2006;11:442–8. doi: 10.1111/j.1440-1797.2006.00599.x. [DOI] [PubMed] [Google Scholar]
- 27.WHO/SEARO Guidelines for the clinical management of snake bites in the Southeast Asian region. Southeast Asian J Trop Med Public Health. 1999;30(Suppl 1):1–85. [PubMed] [Google Scholar]
- 28.Vijeth SR, Dutta TK, Shahapurkar J. Correlation of renal status with hematologic profile in viperine bite. Am J Trop Med Hyg. 1997;56:168–70. doi: 10.4269/ajtmh.1997.56.168. [DOI] [PubMed] [Google Scholar]
- 29.Gutierrez JM, Lomonte B, Leon G, Rucavado A, Chaves F, Angulo Y. Trends in snakebite envenomation therapy: Scientific, technological and public health considerations. Curr Pharm Des. 2007;13:2935–50. doi: 10.2174/138161207782023784. [DOI] [PubMed] [Google Scholar]
- 30.Sharma SK, Chappuis F, Jha N, Bovier PA, Loutan L, Koirala S. Impact of snake bites and determinants of fatal outcomes in southeastern Nepal. Am J Trop Med Hyg. 2004;71:234–8. [PubMed] [Google Scholar]


