Abstract
Naxos disease is a recessive inherited condition with arrhythmogenic right ventricular dysplasia (ARVD) and a peculiar cutaneous phenotype (woolly hair and a palmoplantar keratoderma). Woolly hair appears from birth, palmoplantar keratoderma develops during childhood and cardiomyopathy is clinically manifested by adolescence. Patients present with syncope, sustained ventricular tachycardia or sudden death. We report a case of a 14 year old boy from Spain, who was admitted into our emergency room after being resuscitated from cardiac arrest, secondary to malignant ventricular tachycardia that developed while he was playing basketball.
Keywords: Arrhythmogenic right ventricular dysplasia, Naxos disease, palmoplantar keratoderma, sudden death, woolly hair
Introduction
Naxos disease is a genetic disorder associated with a mutation in the gene for plakoglobin (γ-catenin) and desmoplakin, desmosomal proteins, encoded in Chromosome 17 q 21.
Defects in the linking sites of these proteins can interrupt the contiguous chain of cell adhesion and integrity of skin and heart tissue, leading in the last one to cell death, progressive loss of myocardium and fibro-fatty replacement at subepicardial and mediomural layers.[1] Surviving myocardial fibres without fibrous tissue form zones of slow conduction and provide a substrate for re-entry ventricular arrhythmias.
It was first reported in families from the Greek island of Naxos. Moreover, there are other cases described over the Aegean islands and countries close by. There is a variant of Naxos disease in families from Ecuador and India,[2] in which the heart disorder presents with predominant left ventricular involvement, known as Carvajal syndrome. A recessive syndrome in Australian calves, that associates woolly haircoat and lethal cardiomyopathy has also been described.[3]
It is a very rare, but life-threatening condition There is only one Spanish case in the reported literature. The main clinical problems are: arrhythmia (syncope), heart failure and sudden death,[4] particularly in adolescent and young adults. When the left ventricle involvement is predominant, earlier morbidity and clinical overlapping with dilated cardiomyopathy is seen.[5]
Case Report
Our young patient was born in Spain and is now 14 years old. He is not known to have Greek ancestors, presents woolly hair and his soles show areas of hyperkeratosis. He has a bigger brother who is controlled in our Arrhythmias Department Unit, because of probable Naxos disease; he also presents palmoplantar keratosis and woolly hair from infancy, but no signs of cardiomyopathy.
On February, he was playing basketball with his friends, when he suddenly collapsed after a rough game. He was unresponsive and had no pulse, so lay rescuers provided basic life support until ten minutes later the medical emergency team arrived and brought him up to our Emergency Room.
Upon arrival he had a good pulse and a normal blood pressure, but showed a Glasgow Coma Scale of 4, so we proceeded to support the airway, performing endotracheal intubation. He had a normal physical examination. Blood pressure was 130 over 70 mm Hg, heart rate was 100 per minute and his temperature was Fahrenheit 97 degrees. A 12 lead ECG, showed a sinus rhythm, with a prolongation of the QRS complex in the right precordial leads. Chest X-ray showed no pulmonary congestion. We obtained a Computerized tomography scan that showed an incidental cavernous angioma.
At this point, we brought him up to the Intensive Care Unit, blaming the probable neurological damage to the RCP manoeuvres.
Under sustained ventricular tachycardia suspicion caused by an inherited condition, and the fact that he was haemodynamically stable showing sinus rhythm at all times, and his neurological status normal, (Glasgow score of 15 after extubation), he was dismissed two days later to the Cardiology ward.
He was placed on a cardiac monitor, showing no new episodes of arrhythmia and was started on sotalol. Complete blood count was within normal limits, except for minimal increased troponin levels, secondary to the CPR, with normal serial cardiac markers. An electroencephalogram did not show relevant lesions. A two-dimensional echocardiogram. The left ventricle was normal, with no mitral regurgitation, and an ejection fraction of 57%, but the right cavities were involved, with dilatation, regional hypokinesia, and an aneurysm in the apex. The tricuspidal valve was insufficient, but there were no signs of pulmonary hypertension.
Finally, a cardiac magnetic resonance was scheduled in Barcelona and he was discharged from the hospital pending on these results.
Four months later he was brought up again to the Emergency Room after collapsing during mild exercise. The next morning, when we could get a hold of his medical records, we read his MRI [Figure 1].
Figure 1.
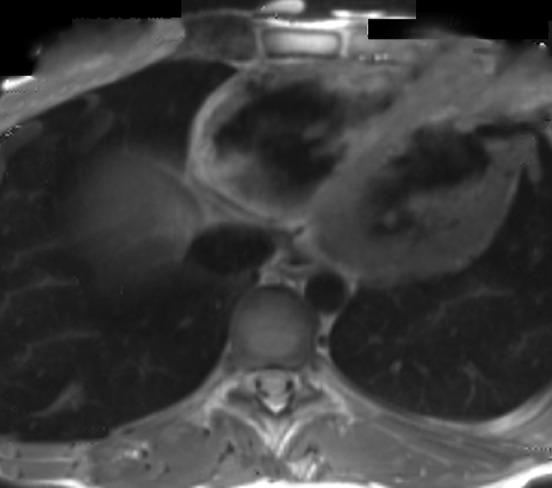
MRI finding he had Mayor criteria for arrhythmogenic right ventricular dysplasia
The new echocardiography revealed more structural and functional anomalies of the right ventricle, with more myocardial loss and more involvement at layers of posterior and apical walls. The left ventricle was slightly affected this time.
Upon all these new findings he went under implantation of an automatic cardioverter defibrillator and was discharged after recovery.
Discussion
Naxos disease is an autosomal recessive disorder that combines ectodermal dysplasia (skin, hair) and mesodermal abnormalities (cardiomyopathy).[6] This last one presents with increased arrhythmogenicity, especially in adolescent and young adults.[7] It is a very rare, but life-threatening condition, so it should be considered as a diagnosis in any child who has woolly hair and keratoderma, as our young patient.[8] Early diagnosis is important because it permits cardiac evaluation and prevention of sudden cardiac death.
Implantation of an automatic cardioverter defibrillator is indicated for prevention of sudden cardiac death. Antiarrhythmic drugs are used to prevent recurrences of ventricular Tachycardia, classical pharmacological treatment is used for congestive heart failure, and heart transplantation is considered at the end stages.[9]
Genetic screening of the population at risk must be made, to identify the heterozygous carriers of the plakoglobin gene mutation. We have no data from the genetic test in our patient.
Our boy was started on a β-blocker drug after he collapsed the first time, while after having the second episode the primary goal was to prevent sudden cardiac death, by implantation of an automatic cardioverter defibrillator.[10]
Over the last few years, the Implantable cardioverter defibrillator has developed to become a device that is now as easily implanted as a pacemaker, and can rapidly and successfully resuscitate patients who develop malignant arrhythmias. The implant in our case was programmed on a VVI pacing mode, and it discharges energies of 15 to 35 Julius when it detects Ventricular Tachycardia between 180 and 230 beats per minute. The device was checked out when he came for a routinist follow up, not showing any discharge. It did show some non-sustained Ventricular Tachycardias, but all were short and self-limited. He keeps asymptomatic at the moment, and has a normal teenager life for now.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Adhisivam B, Mahadevan S. Naxos disease. Indian J Pediatr. 2006;73:359–60. doi: 10.1007/BF02825834. [DOI] [PubMed] [Google Scholar]
- 2.Durán M, Avellán F, Carvajal L. Miocardiopatía dilatada en las displasias del ectodermo. Observaciones electroecocardiográficas en la hiperqueratosis palmoplantar con pelo lanoso. Rev Esp Cardiol. 2000;53:1296–300. doi: 10.1016/s0300-8932(00)75233-x. [DOI] [PubMed] [Google Scholar]
- 3.Kilic T, Babaoglu K, Aygün F, Vural A, Ural D, Agacdiken A, et al. Biventricular involvement in a Turkish boy with palmoplantar hyperkeratosis and curly hair, an unusual presentation of Naxos-Carvajal syndrome. Int J Cardiol. 2007;115:122–5. doi: 10.1016/j.ijcard.2006.08.097. [DOI] [PubMed] [Google Scholar]
- 4.Alonso-Orgaz S, Zamorano-León J, Fernandez-Arquero M, Villacastín J, Pérez-Castellanos N, García Torrent M, et al. Case report of a Spanish patient with arrhythmogenic right ventricular cardiomyopathy and palmoplantar keratoderma without plakoglobin and desmoplakin gene modifications. Int J Cardiol. 2007;118:275–7. doi: 10.1016/j.ijcard.2006.06.065. [DOI] [PubMed] [Google Scholar]
- 5.Turkay S, Odemis E, Karadag A. Woolly hair, palmoplantar keratoderma and arrhythmogenic dilated cardiomyopathy in a 7-year-old Turkish girl: Carvajal síndrome. Ann Trop Paediatr. 2006;26:73–7. doi: 10.1179/146532806X90646. [DOI] [PubMed] [Google Scholar]
- 6.Protonotarios N, Tsatsopoulou A, Patsourakos P, Alexopoulos D, Gezerlis P, Simitsis S, et al. Cardiac abnormalities in familial palmoplantar keratosis. Br Heart J. 1986;56:321–6. doi: 10.1136/hrt.56.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Protonotarios N, Tsatsopoulou A. Naxos disease and Carvajal syndrome: Cardiocutaneous disorders that highlight the pathogenesis and broaden the spectrum of arrhythmogenic right ventricular cardiomyopathy. Cardiovasc Pathol. 2004;13:185–94. doi: 10.1016/j.carpath.2004.03.609. [DOI] [PubMed] [Google Scholar]
- 8.Peirone A, Bruno E, Rossi N, Alday L. Wooly hair and palmoplantar hyperkeratosis may present with hypertrophic cardiomyopathy. Pediatr Cardiol. 2005;26:470–2. doi: 10.1007/s00246-004-0779-1. [DOI] [PubMed] [Google Scholar]
- 9.Protonotarios N, Tsatsopoulou A. Naxos disease: Cardiocutaneous syndrome due to cell adhesión defect. Orphanet J Rare Dis. 2006;13:1–4. doi: 10.1186/1750-1172-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. N Engl J Med. 1997;337:1576–83. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]


