Abstract
Both category and visual analog scales (VAS) of pain assessment have limitations, particularly when measuring pain from low-level pain conditions such as dentin hypersensitivity (DH).
AIMS
The goal of this multi-study project was to develop and test labeled magnitude (LM) scales that are sensitive to variations in pain associated with DH.
METHODS
Qualitative methods were used first to obtain words that describe the pain of DH. Magnitude estimation was then used to determine the position of these descriptive terms by relative magnitude along four vertical LM scales. Participants assessed their DH using the four LM scales following dentin stimulation with 4° and 25°C water. The LM scales were then compared to VAS using eight pain scenarios of varying severity. Finally, participants with DH completed the four horizontal LM scales and VAS after dentin stimulation with 4° and 25° water. Within-subject t-tests were used for comparisons between scales and water temperatures, and between-subject t-tests were used for comparisons between participants with and without DH.
RESULTS
Participants showed comparable differentiation between 4° and 25° C water on VAS and three of the LM scale measures. Responses on the fourth LM scale showed better differentiation than VAS between the two water temperatures. Participants used a greater portion of the LM scales than VAS when rating low-level pain scenarios.
CONCLUSION
LM scales were shown to provide some advantages compared to standard VAS scales when used to evaluate DH-associated pain. These advantages may be generalized to other low-level pain conditions.
Keywords: Dentin hypersensitivity, pain assessment, labeled magnitude scales 3
Introduction
The complex, subjective nature of pain makes its assessment challenging [1,2]. Therefore, many pain measurement tools have been developed in the last 40 years for use in research and clinical settings. The most commonly used scales involve participants indicating pain intensity using verbal descriptors (category scales) or marking a point on a line (visual analog scales (VAS)). Category scales have the advantage of being easy to use and intuitive with minimal instructions. Disadvantages include a limited number of verbal descriptors, forcing the respondent to rate perceptually different pain intensities under the same category. Another issue is the uneven spacing between categories, such that the perceived intensity of a shift from, for example, “weak” to “mild” pain is less than from “strong” to “intense” pain [3].
VAS typically have two verbal descriptors labeling each end of a 100-mm linear scale and span the entire range of pain experience from, for example, “no pain” to “worst pain imaginable”. Participants are free to mark anywhere along the line. However, without intermediate labels to guide responses, additional variability is introduced by nonsystematic variation as to where participants place the mark [3]. Another issue is that the low end of the pain range is compressed to approximately the bottom third of the scale in an effort to capture the full range of pain intensity on the line. Therefore, clinical studies of low to moderate intensity pain conditions such as dentin hypersensitivity (DH) are prone to utilize only a relatively small portion of the entire scale, subjecting studies to floor effects.
Starting in the 1970’s, investigators began to combine verbal descriptors and numerical measurements into category ratio scales of pain. Gracely and colleagues [4] 4 quantified the perceived magnitude of various sensory and affective pain descriptors using a cross-modality matching method with both magnitude estimation and handgrip force. Subsequent studies demonstrated the validity of this technique when applied to tooth pain produced either by electrical stimulation or cold applied to exposed dentin [5]. Heft and Parker [3] proposed combining such category ratio scales with line scales by using labels placed at distances “reflecting the spacings between words as the subjects perceive them”. Their graphic rating scale of pain intensity had six descriptors ranging from “faint” to “intense” aligned along a horizontal line at intervals determined by magnitude estimation of perceived differences between the words. Green subsequently developed a similar, vertical scale with six descriptors ranging from “barely detectable” to “strongest imaginable” aligned at distances determined by magnitude estimation [6]. The goal of this multi-study project was to develop and test labeled magnitude (LM) scales that are sensitive to variations in pain associated with DH. First, focus groups were conducted with people suffering from DH to discern terms used to describe the pain. Magnitude estimation studies were then completed using these terms to determine the position of terms along new, labeled scales. Finally, both experimental and paper- and-pencil tests were performed with the scales to confirm sensitivity of the scales to low and moderate pain. 5
MATERIALS AND METHODS
The University of Washington Institutional Review Board reviewed and approved all study protocols, and informed consent was obtained for all participants for each of the five studies. Studies 1-5 took place from June 2007 to July 2009. Demographic data on participants for all studies are shown in Table 1. Unless otherwise noted, within-subject t-tests were used for comparisons between scales and water temperatures. Between-subject t-tests were used for comparisons between groups.
Table 1.
Demographic information for Studies 1-5.
| Study 1 | Study 2 | Study 3 | Study 4 | Study 5 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M (n=4) |
F (n=22) |
DH | Controls | M (n=3) |
F (n=17) |
M (n=16) |
F (n=24) |
M (n=5) |
F (n=22)B |
|||
| M (n=2) |
F (n=18) |
M (n=8) |
F (n=16) |
|||||||||
| Mean age (s.d.) | 37.2 (7.8) |
30.6 (11.8) |
29.4 (14.8) |
35.9 (14.0) |
29.3 (9.7) |
37.3 (11.8) |
27.6 (10.9) |
36.6 (14.8) |
34.3 (17.0) |
35.6 (16.8) |
26.0 (6.9) |
36.1 (11.0) |
| Hispanic/Latino(a) | 0 | 0 | 1 | 2 | 0 | 1 | 0 | 1 | 0 | 2 | ||
| Ethnicity | ||||||||||||
| Caucasian | 0 | 11 | 2 | 16 | 5 | 12 | 3 | 11 | 10 | 7 | 3 | 18 |
| African American | 1 | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 1 | 0 | 0 |
| Asian | 0 | 0 | 0 | 1 | 0 | 2 | 0 | 4 | 5 | 13 | 2 | 2 |
| Hawaiian/Pacific Island. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| More than one | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 0 |
| Unknown/Not reported | 2 | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Education Level A | ||||||||||||
| High school diploma | 0 | 2 | -- | -- | -- | -- | 0 | 1 | 2 | 2 | 1 | 0 |
| Some college | 0 | 3 | -- | -- | -- | -- | 1 | 5 | 6 | 11 | 1 | 4 |
| Associates Degree | 0 | 1 | -- | -- | -- | -- | 1 | 2 | 2 | 1 | 0 | 4 |
| Bachelors Degree | 2 | 5 | -- | -- | -- | -- | 1 | 6 | 2 | 5 | 3 | 7 |
| Masters Degree | 0 | 0 | -- | -- | -- | -- | 0 | 1 | 3 | 2 | 0 | 2 |
| Doctorate Degree | 0 | 0 | -- | -- | -- | -- | 0 | 2 | 1 | 3 | 0 | 5 |
| Unknown/Not reported | 2 | 11 | -- | -- | -- | -- | 0 | 0 | 0 | 0 | 0 | 0 |
Educational information was not obtained in Study 2;
One participant did not report gender in Study 5
Study 1: Quantitative and Qualitative Assessment of Dentin Stimulation Pain
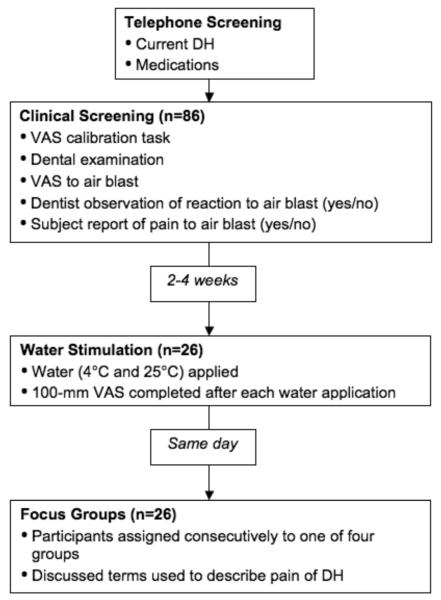
The goals of Study 1 were: A) to determine if individuals with DH could differentiate between water of differing temperatures (4°C and 25°C) applied to their sensitive teeth, and B) to develop a list of descriptive terms used by DH sufferers to describe the pain associated with their condition using stimuli clinically relevant to their condition. A dentin stimulation task, followed by focus groups, was conducted with 26 individuals suffering from DH. Figure 1 provides a flowchart representation of the structure of Study 1.
Figure 1.
Structure of Study 1 including screening sessions and focus groups.
Methods and Procedures
Participants and recruitment
Participants (n=26) were healthy adults from 18 to 75 years of age with at least three teeth affected by DH due to facial/cervical erosion, abrasion and/or gingival recession. Participants were not suffering from gross oral neglect or chronic pain conditions that could alter pain perception. Persons taking regular medications that could alter pain perception (including analgesics and mood-altering medications) or who had completed 6 recent dental treatment were excluded from the study. Recruitment was performed using flyers posted at various campus locations and in a local newspaper.
Participant Screening
Participants were first screened by telephone and in person for the presence of at least three “sensitive teeth” and absence of other chronic pain conditions. Participants completed a screening session with a trained dentist who performed a clinical examination to exclude pain due to cracked or chipped teeth, failed restorations, dental caries, gingival inflammation, etc. The dentist then delivered an evaporative air blast from a standard dental unit syringe on those teeth identified as sensitive and/or displaying cervical erosion, abrasion or recession of exposed dentin.
After each air blast, the dentist and assistant together assigned a score to each tested tooth. The score was based on: 1) the participants’ ratings on a standard 100-mm VAS, labeled on the left with “no pain” and on the right with “worst imaginable pain”; 2) an observable physical reaction to the air puff by the participant (indicated by the dentist as “yes” or “no”); and 3) an indication by the participant (“yes” or “no”) that the air puff was “definitely painful.” DH teeth were considered those that elicited a rating of at least 30 mm on the VAS and at least one of the other two criteria. Each participant was required to have at least three suitable teeth to qualify to return for the stimulation phase and focus group. In total, 86 individuals completed an in-office screening, of which 30 were determined to be eligible to participate in the water stimulation phase. 7
Water Stimulation Phase
Twenty-six of the eligible individuals returned two to four weeks later to participate in a stimulation phase and focus group. A trained dental assistant applied water of two different temperatures (4° and 25°C) to as many as three teeth designated as having DH identified during the screening session. The assistant isolated each tooth with cotton rolls prior to the water application, and then applied 0.5 ml of water for one second with a tuberculin syringe. The assistant applied the water of one temperature to a particular tooth, waited for ten minutes, and then applied the water of the second temperature to the same tooth. After each water application, participants were asked to rate the pain associated with that application on the 100-mm horizontal VAS.
The order of testing was counterbalanced, such that half the participants were presented with the 4°C first and then the 25°C water. The remaining participants received the water temperatures in the reverse order.
Focus Groups
Participants (n=26) were assigned consecutively to one of four focus groups as they became eligible to participate in the groups, such that the first seven participants constituted the first focus group, and so forth. Focus groups contained between five and eight members, the number of groups generally recommended in the literature [7]. After the dentin stimulation, participants met in their respective focus groups with a moderator and note-taker. The moderator led the group in a semi-structured group discussion, focusing primarily on obtaining qualitative descriptions of DH. Participants were asked to provide terms to describe the pain of DH at its most severe and least intense. 8
Specific categories of descriptors were not suggested to participants. The focus group discussions were recorded and transcribed into written form. Transcripts were reviewed and analyzed by two investigators in order to identify consistent themes with regard to descriptive terms associated with DH.
Study 2: Magnitude Estimation and Ranking Tasks of DH-Related Pain Terms
The goal of Study 2 was to determine the relative magnitude of each of the terms obtained in the Study 1 focus groups. Both individuals with DH and pain-free controls completed a magnitude estimation task with the descriptive terms obtained in Study 1.
Methods and Procedures
Participants and recruitment
Native English-speaking adult participants completed Study 2 in two groups. Pain-free controls (n=24) were recruited through flyers posted throughout the University of Washington campus. Individuals with DH (n=20) were participants in Study 1 who had consented to be contacted for future studies.
Magnitude Estimation Task
After obtaining their consent, participants were given instructions for the magnitude estimation task, which indicated how to assign a numeric value to each term. For each group of words, one word judged by the investigators to represent a moderate level of the given theme (Intensity, Duration, Tolerability, Description) was selected as the modulus for that group and given a value of 12, as has been used in prior studies [11]. This gave participants an anchor point against which they could compare the remaining words and give relative ratings.
Participants were instructed to assign further values proportionally, such that terms they perceived as three times as strong as the modulus term were to be assigned the number 36, while those half as strong were to be assigned the value 6, etc. The full 10 instructions for this task were comparable to those used in prior work. [5]
The order of the group of words presented (Intensity, Duration, Tolerability, Description) was counterbalanced across participants. Each group of words was repeated three times. To avoid participant fatigue, participants completed this task over two sessions, with two groups of words per session.
For each descriptive term, the geometric mean of participant magnitude estimates was calculated. For each scale, the resulting magnitude estimates for the descriptive terms were subsequently multiplied by a constant to produce ratings that spanned a 100-mm scale. Constants selected were whole numbers that when multiplied by the mean (geometric) magnitude for the highest term resulted in the number closest to 100 without exceeding that value.
Study 3: Initial Testing of Labeled Magnitude Scales
The goal of Study 3 was to conduct a preliminary test of the ability of participants to use LM scales to discriminate between water of two temperatures placed on sensitive teeth.
Methods and Procedures
Participants and recruitment
Participants were those individuals with DH (n=20) who had previously participated in Study 1.
Pain Calibration Task
Participants first completed a 4-item written oral pain-related calibration task containing the four LM scales (see Table 2) to help standardize participants’ interpretation of oral pain and ensure they understood how to use the scales appropriately. A research team member sat with individuals and explained the use of the scale for each sensation described. The order in which the four LM scales were presented was determined by Latin Square to ensure equal order of presentation and reduce influence of order effects on study results. Calibration items were presented in a fixed order for each participant.
Table 2.
Mean (standard deviation) LM Scale Scores – Instruction Set from Study 3
| Item | % felt before |
Mean Score (s.d.) | |||
|---|---|---|---|---|---|
| Intensity | Duration | Tolerability | Descrip -tion |
||
| 1. The touch of a pill on your tongue. |
100% | 2.3 (6.7) |
6.8 (12.5) |
4.3 (11.9) |
4.2 (10.8) |
| 2. The pain of a canker sore on the inside of your lower lip. |
95% | 42.1 (17.9) |
65.5 (20.8) |
32.8 (16.4) |
48.1 (24.0) |
| 3. The pain from biting your tongue. |
90% | 61.9 (5.0) |
46.2 (12.8) |
26.6 (13.2) |
66.9 (19.5) |
| 4. The pain of a persistent toothache. |
80% | 56.3 (12.6) |
71.8 (14.8) |
54.8 (18.0) |
64.0 (15.9) |
Water Stimulation Phase
Following calibration, participants underwent dentin stimulation with water of two temperatures (4°C and 25°C), applied to each of two teeth considered to have DH as determined in Study 1 and by the participant’s own report. The most sensitive of the two teeth was stimulated first, with water at either 4°C or 25°C, counterbalanced across participants. In the subsequent 10-minute interval, participants completed the four LM scales. 12 Following the 10-minute interval, the other water temperature was presented to the same tooth followed by completion of the four LM scales. A similar procedure was repeated for the second most sensitive tooth applying water temperatures in the reverse order.
Study 4: Scale Orientation Study
The goals of Study 4 were: 1) to examine any differences in ratings that may occur on LM scales presented either horizontally or vertically, and 2) to assess the sensitivity of the LM scales for non-oral pain sensations. Study 4 also served as the first direct comparison of the LM scales and VAS. 13
Methods and Procedures
Participants and recruitment
Participants (n=40) were adults aged 18 and above who were recruited through on-campus flyers.
Procedures
Participants completed paper-and-pencil measures, rating the pain associated with eight hypothetical pain scenarios on both the LM scales and VAS. Half (n=20) of the participants completed the LM scales in the vertical orientation (“no pain” at the bottom, highest pain descriptor near the top, see Figure 2), while the remaining half completed the scales in a horizontal orientation (“no pain” at the left, highest pain descriptor to the right); participants were randomly assigned to scale orientation. VAS measures were presented in the horizontal orientation for all participants, consistent with previous studies. Scales were presented in the same fixed order for each participant (Intensity, Duration, Tolerability, Description, VAS).
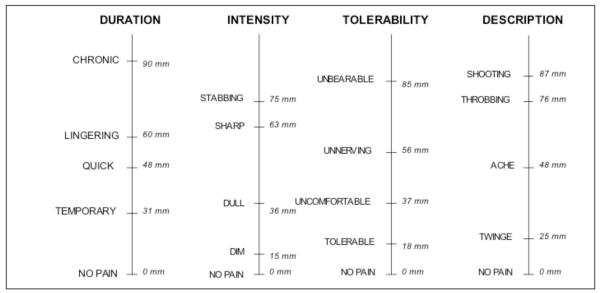
Figure 2.
Labeled Magnitude (LM) Scales Resulting from the Magnitude Estimation Task in Study 2.
Study 5: Comparison of LM Scales with VAS using Direct Stimulation
The goals of Study 5 were 1) to compare the ability of the LM scales and VAS to distinguish between sensations resulting from 4°C and 25°C water stimulation, and 2) to determine participants’ preferences for the LM scales or VAS in measuring the pain associated with DH.
Methods and Procedures
Participants and recruitment
Participants included 15 individuals with DH from Study 1 as well as 13 newly-enrolled participants recruited and screened as described for Study 1.
Procedures
Study 5 participants were asked by the study dentist to identify teeth or areas that were sensitive. The dentist then delivered an evaporative air blast from a standard dental unit syringe on teeth identified as sensitive and/or displaying cervical erosion, abrasion or recession of exposed dentin. Immediately after the air blast, the participant rated the pain experienced on a 100-mm VAS. Participants were determined to be eligible for this portion of the study based on having at least two teeth with DH. (Participants screened during Study 1 were re-screened to be certain their DH pain levels remained adequate for participation in Study 5.) 16
Eligible participants (n=28) underwent dentin stimulation as described in Study 3. Water of two temperatures (4°C and 25°C) was applied to each of the two teeth identified with DH. Each tooth was stimulated with one temperature of water at a time. Participants waited ten minutes between each water stimulation, during which time they completed pain assessments using the four LM scales and one VAS for that particular stimulation. Presentation of the scales, whether LM scales or VAS first, was counterbalanced across participants. In addition, the order of presentation of water temperatures was randomized and counterbalanced for each participant.
After completing the water stimulation, participants (n=25) completed individual interviews consisting of questions about the LM scales and VAS. Participants were shown their individual completed LM scales and VAS and asked, “did you find one type of scale easier to complete than the other?” Interviews were audio-recorded and transcribed into written documents. The written transcripts were then analyzed for themes.
RESULTS
Study 1 Results
Participants assigned higher VAS ratings to the 4°C water (57.6; s.d. = 23.0) in comparison to the 25°C water (31.0; s.d. = 26.4), regardless of the order in which the water was presented (t=5.2, p< 0.01).
When asked about the water stimulation in the focus groups, most individuals noted that the 4°C water was “worse,” “more intense,” and “more painful” compared with the 25°C water. Many were able to determine that the 4°C was colder. Results from the focus groups were consistent with the VAS ratings.
The most common terms describing the pain of DH in the focus groups were grouped into themes. Four common themes emerged: intensity, duration, tolerability, and description. Intensity included such terms as “sharp,” “faint,” and “stabbing”. Duration terms included “temporary,” “lingering,” and “sudden”. Tolerability, the theme describing how well participants were able to endure the pain of DH, included terms such as “annoying,” “uncomfortable,” and “unbearable.” “Description” terms included those that encompassed both intensity and duration. For example, “twinge” suggested experiencing a low level of pain for a short time, while “ache” was suggestive of a higher level of pain for a longer period of time. 9
Study 2 Results
Magnitude estimates did not differ significantly between the DH and control groups for most terms (p value >0 .05). However, in the one case where the two groups differed on a term (“unbearable”), the mean rating from the DH group was used, as the final scales are designed for use in a DH patient population. Some terms produced nearly identical magnitude estimates (e.g., “throbbing,” and “jolt”). In these cases, focus group transcripts were reviewed and the term appearing most frequently was used. The resulting four LM scales with corresponding values for each term in millimeters (mm) are shown in Figure 2. 11
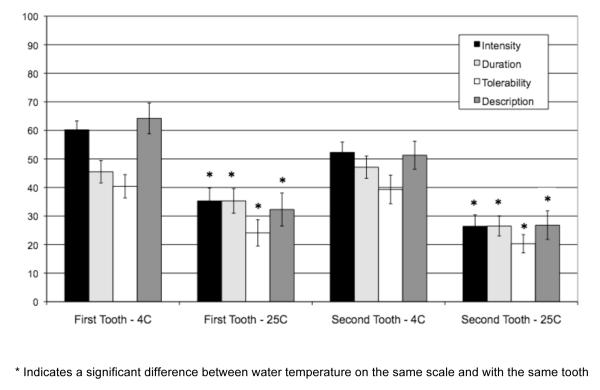
Study 3 Results
Participants’ mean scores for each of the four LM scales for the calibration task are shown in Table 2. Figure 3 shows the mean LM scales ratings from Study 3. Participants gave higher mean ratings for the 4°C than for the 25°C water stimulation for each of the four scales. This was true for both the most sensitive tooth tested (Intensity t=4.7, p<.001; Duration t=2.3, p<.05; Tolerability t=4.1, p<.001; Description t=4.4, p<.001) and the second most sensitive tooth tested (Intensity t=5.7, p<.001; Duration t=4.9, p<.001; Tolerability t=4.4, p<.001; Description t=4.9, p<.001). Although the mean ratings given by the participants tended to be higher on all scales for the first stimulated tooth (identified as the most sensitive) when compared with the second tooth, these differences were not statistically significant (p > .05).
Figure 3.
Mean Ratings of Pain after Dentin Stimulation using LM Scales in Study 3
Study 4 Results
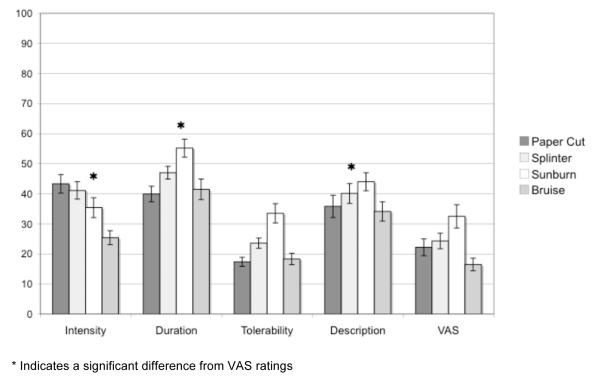
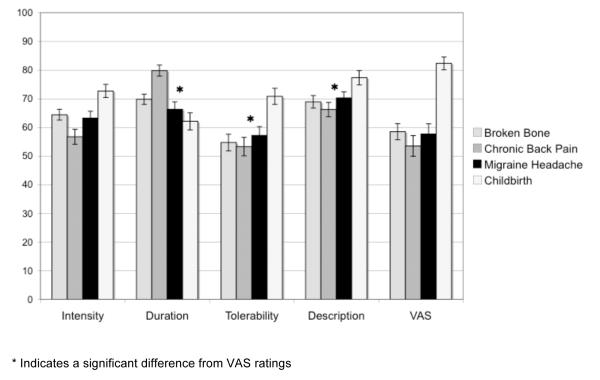
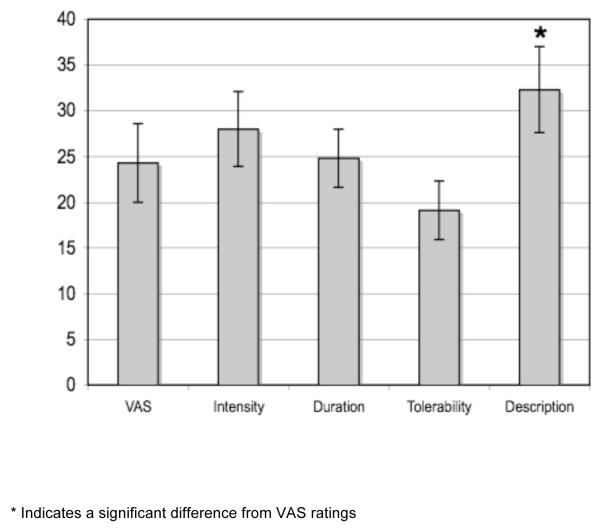
The eight pain scenarios included both low- (paper cut, splinter, sunburn, bruise) and high-level (broken bone, chronic back pain, migraine headache, childbirth) non-oral pain sensations. No significant differences were found between LM scales presented horizontally or vertically (t’s < 2.0) or for VAS ratings (p’s > .05) following the different orientations. Data from the two orientations, therefore, were collapsed for further 14 analyses. Figure 4 shows both low-level (Figure 4a) and high-level (Figure 4b) pain scenarios as rated on the LM scales and VAS.
Figure 4.
a. LM Scales and VAS Ratings for Low-level Pain Scenarios in Study 4
b. LM Scales and VAS Ratings for High-level Pain Scenarios in Study 4
Ratings on the VAS for the low-level pain scenarios remained in the bottom third of the scale, with the means ranging from 18.1 to 32.6 mm, and averaging 23.9 mm across all four low-level scenarios. For the LM scales, however, higher mean ratings on the four low-level pain scenarios were observed for three of the four scales. Intensity ranged from a mean of 25.4 to 44.0, averaging 36.3 across all low-level pain scenarios; Duration, from 37.0 to 53.8, and 45.9 overall; Tolerability, from 16.9 to 32.2 mm, and 23.2 mm overall; Description, from 32.2 to 45.5 mm, and 38.5 mm overall.
A 4 (item) × 5 (scale) analysis of variance identified significant main effects of item and scale, as well as item by scale interactions (p’s < .0001). Planned comparisons confirmed that, collapsing across items, Intensity, Duration, and Description produced significantly higher ratings than did VAS (p’s < .0001), while Tolerability did not differ from VAS (p = .71; Figure 4a).
A comparable 4 (item) × 5 (scale) analysis of variance for high-level pain scenarios also identified significant main effects of item and scale, as well as item by scale interactions (p’s < .0001). By collapsing across items, planned comparisons confirmed that Duration, Tolerability, and Description produced significantly higher ratings than did VAS (p’s < .02), while Intensity did not differ from VAS (p = .45; Figure 4b). 15
Study 5 Results
The mean ratings involving the stimulation of the participants’ most sensitive teeth are shown in Table 3. Participants consistently rated the pain associated with placement of the 4°C water as significantly more painful on each of the four LM scales as well as on the VAS when compared with the 25°C water (Table 3).
Table 3.
Mean (standard deviation) LM Scale and VAS Scores for Dentin Stimulation in Study 5
| 4°C | 25°C | Mean Difference | t-value | p-value | |
|---|---|---|---|---|---|
| Intensity | 50.9 (16.6) | 22.9 (19.9) | 28.0 (21.6) | 6.9 | <.001 |
| Duration | 49.4 (16.0) | 25.4 (19.0) | 24.0 (16.5) | 7.6 | <.001 |
| Tolerability | 35.6 (19.0) | 16.5 (13.4) | 19.1 (17.1) | 5.9 | <.001 |
| Description | 54.2 (24.8) | 21.9 (19.5) | 32.3 (24.6) | 6.9 | <.001 |
| VAS | 49.3 (22.7) | 25.1 (21.2) | 24.3 (22.7) | 5.6 | <.001 |
The Description LM scale showed the greatest mean difference between 4°C and 25°C temperature water (t=6.9, p<.001; Figure 5).The mean of the Description difference score (mean=32.3, s.d.=24.6) was significantly larger than that of the mean VAS 17 difference score (mean=24.3, s.d.=22.7; t=2.2, p<.05). These results were replicated with the second most sensitive tooth tested.
Figure 5.
LM Scales and VAS difference scores from Study 5.
Due to scheduling difficulties and equipment failures, five participant interviews were either not completed or recorded, resulting in a final sample size of 23 for the qualitative portion of the study. Three participants did not express a preference for one scale over the other. Seven participants expressed a clear preference for the VAS, while thirteen expressed a preference for the LM scales.
Participants who preferred the VAS to the LM scales noted that the VAS was more familiar to them, and that the words presented on the LM scales were sometimes confusing. These individuals were more likely to describe the LM scales as “categorical,” and noted that the categories did not always fit their pain experiences. Participants with a preference for the LM scales over the VAS, meanwhile, reported that having descriptors allowed them to be more precise in their measurements, and that they found the VAS to be vague and open-ended.
DISCUSSION
The current series of studies aimed to develop and test a set of four LM scales specific for the assessment of the pain associated with DH. Pain intensity scales, such as VAS, are commonly used in the measurement and assessment of various acute and chronic pain conditions. While these scales have proven useful in the measurement of high-intensity pain conditions such as post-operative pain [8,9], the nature of low-level pain may not be fully captured by these standard measures. The goal of the current set of studies was to develop scales that 18 would encourage participants to use a greater portion of the 100-mm scales, thereby avoiding floor effects seen when using the VAS with such low-level pain conditions, as well as to broaden the scope of the pain assessment beyond “Intensity” to cover other condition-specific dimensions that characterize the DH pain response.
When discriminating between water of two temperatures, both the LM scales and VAS showed good differentiation between cold (4°C) and room temperature (25°C) water. However, the magnitude of the difference between water temperatures was greatest for the Description LM scale, whose terms combined both temporal and intensity aspects of pain.
In comparing the VAS and LM scales on eight hypothetical pain scenarios, participants utilized a greater portion of the 100-mm measures of the LM scales than the VAS, particularly when rating low-level pain, such as a bruise, paper cut, and splinter. Using the LM scales for low-level pain may thus reduce floor effects seen with the VAS. Historically, line-based pain scales have been presented either horizontally [3] or vertically [6]. In the current study, no significant differences emerged on ratings given on vertically- and horizontally-presented LM scales. This suggests that the LM scales may be presented in either orientation. When presented in conjunction with the VAS, however, users may want to present all scales on the horizontal orientation for ease of use by participants.
Many scales [4,5,6,10,11], including the standard VAS, focus just on the aversiveness or just on the perceived intensity of the pain experience. In doing so, the scales fail to take into account other aspects of clinical pain. The McGill Pain Questionnaire (MPQ), in contrast, is the most comprehensive pain assessment in frequent use 19 [12, 13]. This questionnaire consists of four major classes of terms used to describe pain: Sensory, Affective, Evaluative, and Miscellaneous. These terms are further divided into 20 different subclasses. Within the subclasses the terms are rank ordered according to intensity ratings (on a 1 to 5 scale). Participants choose a word in each subclass that describes their pain experience. Additionally they are asked to choose words that describe the pattern of the pain as well as the strength of the pain. Scores for each class (Sensory, Affective, Evaluative, and Miscellaneous) are obtained by adding the rank values of words selected in each subclass comprising that particular class. The MPQ has demonstrated reliability and validity for numerous pain conditions, and is sensitive to differences in pain arising from reversibly inflamed versus necrotic tooth pulp [14, 15].
Because of concerns that that standard measures, including the MPQ, were targeted to more acute, higher intensity pain experiences, unique lists of terms were developed to describe the episodic, low-level pain of DH. This was accomplished by conducting focus groups with people suffering from the condition on the same day that their pain was elicited by application of cold water to exposed dentin. A number of the terms elicited in this way do overlap with terms in the MPQ. “Throbbing”, “shooting”, “stabbing”, “dull”, “sharp”, and “aching” all appear in the Sensory Class of terms on the MPQ. These terms are found on the Intensity and Description LM scales. “Unbearable” appears at the high end of the Evaluative Class in the MPQ and was also at the high end of the Tolerability LM scale. However, many of the terms used to describe the pain of DH 20 do not appear on the MPQ. Consistent with the concern that other scales are not geared to low-level pain, the non-overlapping terms include many terms at the low end of the LM scales such as “dim” (Intensity), “twinge” (Description), “tolerable” (Tolerability) and “uncomfortable” (Tolerability). The LM scale Tolerability term “unnerving” also does not appear on the MPQ. Perhaps because of the rapid onset and offset normally associated with DH, the LM Duration scale terms are not the same as those in the MPQ. LM Duration terms instead include the words “temporary”, “quick”, “lingering”, and “chronic”. The MPQ, however, does contain synonyms such as “continuous”, “steady”, “constant”, “brief”, “momentary” and “transient”. Yet, these terms do not fall into one of the 20 sub-classes of the MPQ, but instead fall under a separate category about how the pain changes with time. This may be due in part to the fact that the relative intensity of DH pain experience is low, but also to the character and, therefore, manifestation of pain is condition-specific.
The LM scales further differ from the MPQ in allowing participants to mark intermediate points on the four scales for cases in which the labels listed do not exactly match the pain level experienced. Both the MPQ and the LM scales order terms based on intensity ratings gathered from developmental work. Developmental work on the MPQ found intensity (magnitude), but not rank ordering, differences between patient and physician ratings. In the magnitude estimation work presented here, there was good agreement between patients with hypersensitivity and healthy controls in the perceived magnitude of the terms. The LM 21 scales, therefore, utilize magnitude differences between terms operationalized as distance along a 100-mm line.
When asked in interviews about the ease of use of the LM scales and VAS, results were mixed. Evidence emerged for more individuals to prefer the LM scales, with comments such as, “I found the [scales] with words in them to be more helpful... it was much easier for me to describe what I was feeling.” Specifically, 13 out of 23 participants expressed preference for the LM scales, in comparison to seven who preferred to use the VAS. However, some participants noted that they were more familiar with the VAS, and that they needed to spend more time completing the LM scales. These results suggest the need for clear instructions for the LM scales, particularly for those participants unfamiliar with the scales.
One limitation in the current study involves the use of many of the same participants in both the development and testing phases of the study. While additional participants were included in Study 5 that did not participate in Studies 1-4, further testing of the LM scales is needed to ensure that the current results are generalized appropriately. Currently, larger clinical studies using the LM scales and VAS are being conducted with unique patient samples, which will provide further data regarding the utility of the LM scales.
Results from this series of studies provide valuable information regarding the experience and measurement of DH, a low-grade, episodic pain condition. The LM scales, alone or in combination with the standard VAS, can provide information regarding the intensity, duration, tolerability, and description of the pain associated with this condition, affording reduced opportunity for the floor effects seen when low-grade pain is measured with the VAS. These scales permit 22 participants to rate broader and condition-specific aspects of their pain, allowing researchers and clinicians to better understand not only the DH pain condition but also other low-level pain conditions, and ideally to evaluate the effectiveness of treatment-based management strategies. 23
Supplementary Material
Acknowledgements
This research was funded by GlaxoSmithKline Consumer Healthcare, Weybridge, Surrey, United Kingdom. Study procedures were carried out through the University of Washington’s Regional Clinical Dental Research Center, which is supported by Grant UL1RR025014 from the NIH National Center for Research Resources. The authors would like to thank Dr. Masahiro Heima, Dr. Luisa Valbuena, Mary K. Hagstrom, Gregory Mueller, Marilynn Rothen, and Dr. Joseph Sowinski for their important contributions to this research, and Dr. Marc Heft for his valuable review and comments on an earlier version of this paper. 24
References
- 1.Beecher HK. The subjective response and reaction to sensation; the reaction phase as the effective site for drug action. Am J Med. 1956 Jan;20(1):107–13. doi: 10.1016/0002-9343(56)90178-4. [DOI] [PubMed] [Google Scholar]
- 2.Merskey H, Bogduk N, editors. Classification of chronic pain: description of chronic pain syndromes and definitions of pain terms. IASP Press; Seattle: 1994. [Google Scholar]
- 3.Heft MW, Parker SR. An experimental basis for revising the graphic rating scale for pain. Pain. 1984 Jun;19(2):153–61. doi: 10.1016/0304-3959(84)90835-2. [DOI] [PubMed] [Google Scholar]
- 4.Gracely RH, McGrath F, Dubner R. Ratio scales of sensory and affective verbal pain descriptors. Pain. 1978 Jun;5(1):5–18. doi: 10.1016/0304-3959(78)90020-9. [DOI] [PubMed] [Google Scholar]
- 5.Heft MW, Gracely RH, Dubner R, McGrath PA. A validation model for verbal description scaling of human clinical pain. Pain. 1980 Dec;9(3):363–73. doi: 10.1016/0304-3959(80)90050-0. [DOI] [PubMed] [Google Scholar]
- 6.Green BG, Shaffer GS, Gilmore MM. Derivation and evaluation of a semantic scale of oral sensation magnitude with apparent ratio properties. Chem Senses. 1993;18:683–702. [Google Scholar]
- 7.Halcomb EJ, Gholizadeh L, DiGiacomo M, Phillips J, Davidson PM. Literature review: considerations in undertaking focus group research with culturally and linguistically diverse groups. J Clin Nurs. 2007 Jun;16(6):1000–11. doi: 10.1111/j.1365-2702.2006.01760.x. [DOI] [PubMed] [Google Scholar]
- 8.Breivik EK, Skoglund LA. Comparison of present pain intensity assessments on horizontally and vertically oriented visual analogue scales. Methods Find Exp Clin Pharmacol. 1998 Oct;20(8):719–24. doi: 10.1358/mf.1998.20.8.487509. [DOI] [PubMed] [Google Scholar]
- 9.Gagliese L, Weizblit N, Ellis W, Chan VW. The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. Pain. 2005 Oct;117(3):412–20. doi: 10.1016/j.pain.2005.07.004. 25. [DOI] [PubMed] [Google Scholar]
- 10.Gracely RH, Dubner R. Reliability and validity of verbal descriptor scales of painfulness. Pain. 1987 May;29(2):175–85. doi: 10.1016/0304-3959(87)91034-7. [DOI] [PubMed] [Google Scholar]
- 11.Heaton LJ, Garcia LJ, Gledhill LW, Beesley KA, Coldwell SE. Development and validation of the Spanish Interval Scale of Anxiety Response (ISAR) Anesth Prog. 2007;54(3):100–8. doi: 10.2344/0003-3006(2007)54[100:DAVOTS]2.0.CO;2. Fall. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ljunggren AE, Strand LI, Johnsen TB. Development of the Norwegian Short-Form McGill Pain Questionnaire (NSF-MPQ) Adv Physiotherapy. 2007;9(4):169–80. [Google Scholar]
- 13.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987 Aug;30(2):191–7. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 14.Grushka M, Sessle BJ. Applicability of the McGill Pain Questionnaire to the differentiation of ‘toothache’ pain. Pain. 1984 May;19(1):49–57. doi: 10.1016/0304-3959(84)90064-2. [DOI] [PubMed] [Google Scholar]
- 15.Melzack R. Pain Measurement and Assessment. Raven Press; New York: 1983. The McGill Pain Questionnaire; pp. 41–8. 26. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.