Abstract
A great deal of excitement and hope has followed the successful trials and US Food and Drug Administration approval of the drug ivacaftor (Kalydeco), the first therapy available that targets the underlying defect that causes cystic fibrosis (CF). Although this drug has currently demonstrated a clinical benefit for a small minority of the CF population, the developmental pathway established by ivacaftor paves the way for other CF transmembrane conductance regulator (CFTR) modulators that may benefit many more patients. In addition to investigating CFTR modulators, researchers are actively developing numerous other innovative CF therapies. In this review, we use the catalog of treatments currently under evaluation with the support of the Cystic Fibrosis Foundation, known as the Cystic Fibrosis Foundation Therapeutics Pipeline, as a platform to discuss the variety of candidate treatments for CF lung disease that promise to improve CF care. Many of these approaches target the individual components of the relentless cycle of airway obstruction, inflammation, and infection characteristic of lung disease in CF, whereas others are aimed directly at the gene defect, or the resulting dysfunctional protein, that instigates this cycle. We discuss how new findings from the laboratory have informed not only the development of novel therapeutics, but also the rationales for their use and the outcomes used to measure their effects. By reviewing the breadth of candidate treatments currently in development, as well as the recent progress in CF therapies reflected by the evolution of the therapeutics pipeline over the past few years, we hope to build upon the optimism and anticipation generated by the recent success of Kalydeco.
In 2009, a review publication described the “pipeline” of candidate treatments then under evaluation for cystic fibrosis (CF).1 The authors identified > 24 drugs and other therapies that were in various stages of development for CF as part of a remarkable, collaborative therapeutic development system entirely devoted to this disease. The cooperative efforts of patients and their families, private and public funding agencies, patient advocacy groups, academia, and industry had generated this formidable catalog of therapies, of diverse types and targets, and the promise offered by this list was clearly evident in the text. Six treatments had already traversed this pipeline, clearing all obstacles to become available to patients, and the remaining candidates fell into eight different categories, from those targeting bacteria and mucus to nutritional interventions, all showing promise for improving or extending the lives of people with CF. However, among the dozens of remaining candidates, the two that received the most attention were orally available, small-molecule drugs targeting the protein mutated in CF, the CF transmembrane conductance regulator (CFTR).
This excitement has now proven to be warranted: This year one of those compounds, the CFTR modulator ivacaftor (Kalydeco), was approved by the US Food and Drug Administration (FDA) for administration to people with a specific CFTR mutation (G551D), thus becoming the first available treatment to directly address the underlying defect in CF.2 Although the missense CFTR mutation G551D is present in fewer than 5% of people with CF,3 the successful trial4 and approval of Kalydeco has generated excitement and hope among people who care about this disease.
At this moment of tremendous excitement, it is easy to lose sight of the rest of the development pipeline.2 The drugs that it describes include inhaled tobramycin (TOBI) and aztreonam (Cayston), azithromycin, dornase alfa (Pulmozyme), hypertonic saline, pancreatic enzyme products (including Ultresa, Zenpep, Pancreaze, Viokace, Pertzye, and Creon),5 and fat-soluble vitamin preparations, all of which have already had a tremendous impact on the quantity and quality of life of people with CF. Beyond these available medications, new therapies are under evaluation that will likely improve and extend the lives of individuals with CF, regardless of the impact of CFTR-targeted compounds. People who already have CF lung disease, and those for whom effective CFTR genotype-specific compounds are not yet available, need better antibiotic, antiinflammatory, mucus-altering, and nutritional therapies, among others; some may need transplantation. Recent advances in cell- and gene-based techniques have also revived interest in genetically repairing (rather than chemically restoring) CFTR function. In this review, we focus on these promising therapies in development specifically for CF lung disease, with reference to those currently in use. In summarizing what is to come, we hope to show that the excitement generated by Kalydeco promises to be just the beginning of a new era in the field of CF therapeutics.
What Lies Ahead
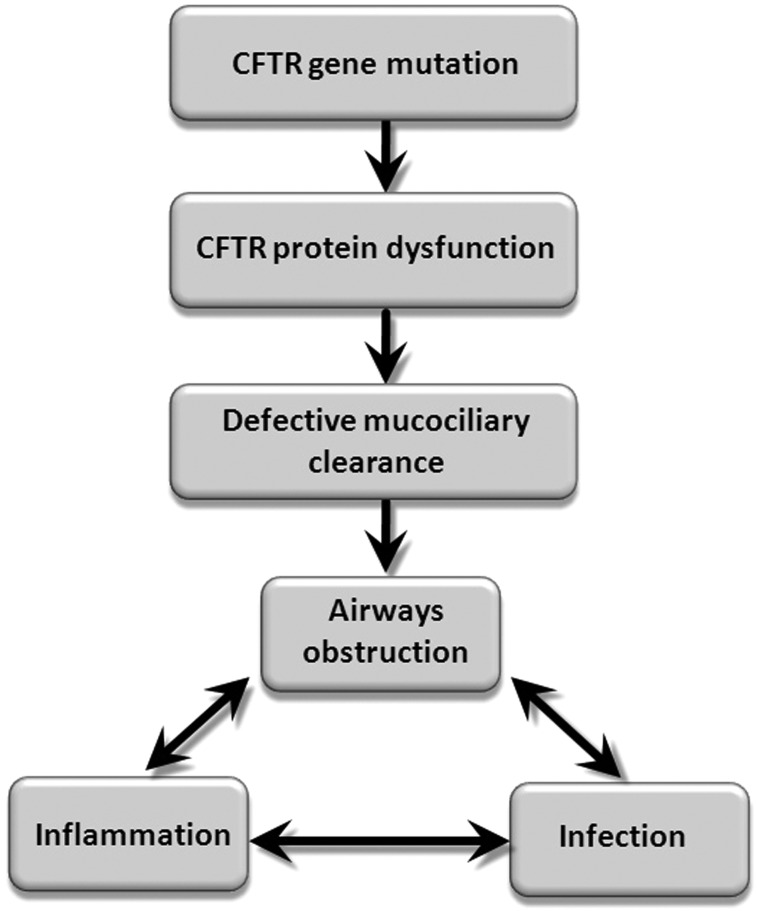
The pathophysiology of CF lung disease is known to involve self-perpetuating cycles of airway obstruction, infection, and inflammation,6 as illustrated at the bottom of Figure 1. Accordingly, many current and candidate treatments directly target one or more of these pathophysiologic elements; for example, there are multiple therapies currently addressing airway infections, inflammation, and airway mucus rheology. More encouraging are novel therapies, including CFTR modulators and airway cell genetic modification strategies, that transcend the usual categories by impacting the entire pathophysiologic cycle in Figure 1 by acting further upstream. In this article, we briefly describe some of the therapies in the advanced stages of development in each of these interrelated categories, largely restricting our discussion to therapies to prevent or treat CF lung disease for which there are published data from at least phase 2 studies (or, in specific cases, phase 1) and that are currently in the Cystic Fibrosis Foundation Therapeutics Pipeline.2
Figure 1.
A model for cystic fibrosis (CF) lung disease pathophysiology. According to this model, defective ion and fluid transport due to CFTR mutation results in inadequate clearance of mucus and the material it traps in CF airways. The retained material results in a cycle of airways obstruction, inflammation, and infection. The current and candidate therapies discussed in this review target one or many of these pathophysiologic steps, and therapies addressing the earliest steps would be expected to impact all subsequent elements. CFTR = cystic fibrosis transmembrane conductance regulator.
Infection Treatments
The candidate drugs that remain on the current development pipeline include a new preparation of inhaled tobramycin, an inhaled fluoroquinolone, an inhaled antibiotic combination, and a new inhaled aminoglycoside.2 TOBI inhaled powder (TIP) is a new, high-potency formulation of tobramycin designed to deliver to the lung amounts of this aminoglycoside that are pharmacologically similar to TOBI but with substantially shorter administration time. TIP recently completed phase 3 studies, and it has been approved in the European Union.2 Phase 4 studies of TIP are ongoing in the United States and Europe. An inhaled liquid preparation of a fluoroquinolone, levofloxacin (Aeroquin), is currently in phase 3 trials and has shown promise.7 The phase 2 study reported an 8.7% improvement in FEV1 and an approximately 1-log decrease in density of Pseudomonas aeruginosa compared with placebo following 28 days of administration of 240 mg bid by inhalation.
Two additional antibiotic preparations given by the inhaled route, each using an aminoglycoside, are also in development. Arikace is a liposomally encased preparation of amikacin, providing sustained release and rapid delivery times. Arikace has completed phase 2 trials,2,8 reporting relative improvement in FEV1 of 10.8% at 7 days with 500 mg inhaled once per day, and a phase 3 trial will soon be recruiting subjects with CF and P aeruginosa.9 Another trial not specifically for patients with CF is also listed for subjects with nontuberculous mycobacteria and is recruiting.10 A combination of the phosphonic acid antibiotic fosfomycin with tobramycin has also completed phase 2 trials11 and shows promise as the first combination inhaled antibiotic preparation being investigated for CF. Another unique feature of the inhaled fosfomycin/tobramycin combination is its relatively broad spectrum, which, viewed through the constantly shifting lens of CF microbiology, may be beneficial to patients with multiple infecting organisms.
The evolving issue of CF microbiology merits deeper discussion here. A relatively recent development in CF microbiologic research has interesting implications for the development of current and future antiinfective treatments. By using new DNA-based, culture-independent methods, microbiologists have found that CF airway secretions (particularly those from younger patients) tend to contain many more microbial species than had been appreciated using standard clinical microbiologic laboratory culture methods.12‐14 These findings have further extended an already growing list of “emerging CF pathogens,” raising questions not only about exactly which microbes contribute to CF lung disease, but also about how the complex CF sputum microbial communities respond to antibiotics currently in use and under evaluation.15 For example, the combination antibiotic therapy fosfomycin/tobramycin could provide additional benefit beyond its effect on P aeruginosa because the broad spectrum of fosfomycin, a phosphonic acid antibiotic, also targets gram-positive (including methicillin-resistant Staphylococcus aureus) and anaerobic bacterial species.11 Similar discussions may be expected in future antibiotic trials, and sequence-based microbiologic outcomes may also become commonplace both in studies and in the clinic.
The remarkable persistence of chronic CF lung infections despite intensive antibiotic therapy has inspired some innovative approaches that also warrant mention. One example is an ongoing safety and efficacy (phase 1) study of IV gallium nitrate (Ganite).16 The gallium ion is chemically similar to iron, allowing it to substitute for iron ions and inhibit iron-dependent bacterial processes. One of the processes altered by gallium is the formation of biofilms,17 multicellular structures established by many microbes that are particularly resistant to antibiotic killing and host immunity.18 Gallium has been shown to increase the efficacy of existing antibiotics19 and to have antimicrobial activity itself.17 Novel approaches such as these may greatly expand the armamentarium available to physicians for treating many chronic infections, including those in CF airways.
Antiinflammatory Treatments
Only one antiinflammatory drug (the nonsteroidal agent ibuprofen) has thus far demonstrated efficacy with an improvement in rate of decline in FEV1 over a 2-year period20 and a favorable risk profile; it is, therefore, recommended as a beneficial therapy for patients 7 to 18 years of age.21 Development of antiinflammatory therapies in CF has been challenging because their mechanism of action may be to prevent long-term clinical decline rather than to effect acute changes in more commonly used clinical outcome measures, such as lung function or frequency of pulmonary exacerbations. Thus, detection of clinical benefit requires studies of long duration and significant sample size,22 often discouraging the development of potential antiinflammatory therapies in this population. Despite these challenges, several therapies have currently passed into the phase 2 stage listed on the 2012 Cystic Fibrosis Foundation pipeline.2 Three examples include N-acetylcysteine, docosahexenoic acid, and sildenafil.
N-acetylcysteine is an oral antioxidant medication that has been shown in one phase 2 trial to impact inflammatory measures in patients with CF and baseline inflammation, an effect hypothesized to occur by addressing a redox imbalance in neutrophils.23 A recent phase 2b clinical trial of N-acetylcysteine did demonstrate an effect on lung function, but the effect on inflammation was not reproduced.2 Similarly, docosahexaenoic acid is an omega-3 fatty acid that demonstrated antiinflammatory activity in a short clinical trial in 200324 and has completed a phase 2 trial among infants; results are forthcoming. A phase 2 trial of sildenafil is currently evaluating the effect of this oral phosphodiesterase inhibitor on markers of airway inflammation.2
Although the agents mentioned comprise those described as “antiinflammatory” drugs in the current pipeline, it could be argued that other medications under investigation or already in use have significant antiinflammatory effects. For example, although azithromycin is commonly considered to be an antibiotic, this macrolide also demonstrates substantial impacts on inflammation both in vitro25 and in clinical trials26; more than one review article has even referred to azithromycin as among the most promising antiinflammatory therapies for CF.27,28 Similarly, a recent review in the Journal of Cystic Fibrosis underscored the effect of the mucolytic agent dornase alfa on markers of inflammation; this discussion highlighted how difficult it can be to firmly categorize therapeutic agents as antiinfective, antiinflammatory, or mucolytic, among other classes.29 In addition, it seems likely that treating CFTR dysfunction directly with novel agents like Kalydeco will prove to have a significant impact on airway inflammation.
Mucus Alteration and Airway Surface Liquid Modulation Therapy
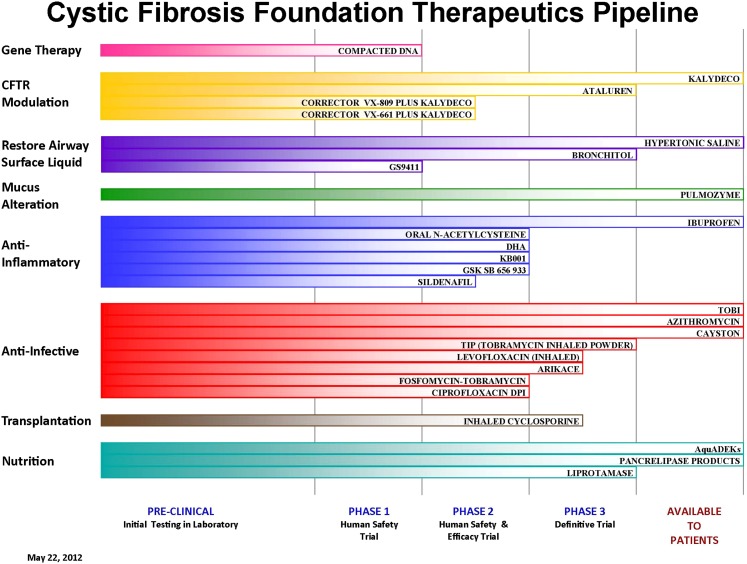
The ion and fluid transport abnormalities that result from CFTR mutations play key roles in initiating and/or perpetuating the cycle of airway obstruction, inflammation, and infection (Fig 1). Therapies that alter either the rheologic properties of the notoriously tenacious mucus (termed “mucus alteration”) that obstructs CF airways30 or the abnormal fluid and electrolyte properties of CF airway surface liquid (termed “airway surface liquid modulation”) could break that cycle by relieving airways obstruction and facilitating removal of toxic, proinflammatory material. As shown in Figure 2,2 two such treatments are currently available (Pulmozyme and hypertonic saline), and two candidate treatments (Bronchitol and Gilead GS9411) are in development.
Figure 2.
The Cystic Fibrosis Foundation Therapeutics Pipeline as it currently stands. These are CF therapies in various stages of development with the support of the Cystic Fibrosis Foundation. The therapies discussed in this article are those under the categories labeled “CFTR Modulation,” “Restore Airway Surface Liquid,” “Mucus Alteration,” “Anti-inflammatory,” and “Anti-infective” and for which there are published phase 2, and in certain cases phase 1, data available. See Figure 1 legend for expansion of abbreviations. (Reprinted with permission from the Cystic Fibrosis Foundation; interactive version available.2)
Pulmozyme, which received FDA approval in 1994,31,32 is currently used as chronic daily therapy by 81% of patients with CF who are older than 6 years in the United States.33 Chronic administration of hypertonic saline (7% solution) was demonstrated in 200634 to significantly decrease the rate of pulmonary exacerbations. It is not an FDA-approved therapy, yet it is currently used by 51% of patients with CF who are older than 6 years in the United States.33
Bronchitol is an inhalable preparation of powdered mannitol, an osmotic agent that is designed to rehydrate CF airway secretions. Multiple phase 3 trials have now taken place.35,36 One study completed in the United States demonstrated a relative improvement in FEV1 of 3.75% compared with control subjects (P < .03),35 whereas a second international study found a relative improvement of 92.9 mL (P < .001)36 compared with control subjects. Bronchitol has been approved for treatment of CF lung disease in Australia, and approval is being sought in both Europe and the United States.2
Gilead GS9411 is an agent designed to inhibit airway sodium absorption, which has been shown to be dysregulated in CF epithelial cells in vitro.37 A phase 1 trial has been completed for this agent in people with CF; results are awaited.2
Stem Cell and Gene Therapy Treatments
Since the gene for CFTR was identified in 1989,38‐40 the CF research community has maintained great hope for a therapy that will correct the underlying defect through genetic manipulation. Gene therapy was, and remains, an attractive approach. However, this method has proven to be extremely challenging for a variety of reasons, not the least of which are the robust barrier, immune, and clearance functions of the airway, the primary target organ for most of these techniques. The difficulty of gene therapy is reflected by the variable results of the 25 CF gene therapy trials performed to date.41 As a result, no current gene therapy trials are actively enrolling patients. The gene therapy field has appropriately gone “back to the drawing board” to develop novel approaches before recommencing human studies.
In a recent review of laboratory advances in this area, Oakland et al41 described the variety of both gene therapy and cell-based approaches that show promise for treating CF in the near future. Among these developments is the identification of stem cells that are capable of differentiating into respiratory epithelia. Results from in vitro and animal work are encouraging in this area, but these fields remain in early stages, and substantial improvements in cell delivery and engraftment are required to develop truly effective therapies.41 Fortunately, a recent advance in CF research that promises to accelerate the development of potential cell- and gene-based treatments is the availability of two new CF animal models, a CF pig42 and a CF ferret,43 that replicate CF lung disease more faithfully than do murine models. These models offer not only new opportunities to study lung disease pathophysiology, but also new systems to test candidate treatments.
Small-Molecule CFTR Modulators
Candidate drugs in this promising class of agents are further divided into three therapeutic categories: one CFTR “potentiator,” two CFTR “correctors,” and another agent that promotes ribosomal read-through of nonsense mutations. Each of these agents has therapeutic potential for a specific patient population.
Kalydeco (ivacaftor, referred to in the Introduction) is an oral CFTR “potentiator,” signifying that it increases chloride transport by CFTR molecules that are already on the epithelial cell surface.44 The target clinical population and its CFTR mutations were described earlier. The results of a successful phase 3 trial were published in 2011,4 demonstrating a 10% improvement in FEV1 by 2 weeks that was sustained for 48 weeks. Clinically significant improvements in the frequency of exacerbations, weight gain, and respiratory symptoms and a decline in sweat chloride were noted. In January 2012, this agent became the first drug that targets CFTR itself to become available to patients.2 Although Kalydeco monotherapy has demonstrated efficacy for a limited fraction of patients with CF, it is hoped that it may be useful when combined with other therapies in the many patients with CF and other mutations.
This idea underlies a second approach using Kalydeco, currently in a phase 2 trial. In this study, Kalydeco is administered in combination with another agent, VX-809, which is an oral CFTR “corrector.” CFTR “correctors” are designed to facilitate the trafficking of more CFTR molecules to the airway epithelial surface. Although VX-809 showed efficacy in vitro by enhancing △F508 CFTR processing and chloride transport in cultured epithelial cells, the effect was modest.45 Early human studies with VX-809 monotherapy indicated a small effect on the sweat gland but no effect on lung function.46 Based on in vitro data in cultured epithelial cells, the combination of a corrector and a potentiator was hypothesized to be more effective than either agent alone. Thus, a VX-809/Kalydeco combination approach has progressed to phase 2 studies. Interim analysis results from this ongoing phase 2 trial enrolling people homozygous for the common △F508 CFTR mutation are encouraging, demonstrating an 8.5% mean improvement in lung function compared with placebo.2,47
Ataluren (PTC124) is an oral drug that permits ribosomes to continue producing functional CFTR protein despite the presence of premature stop codons. These alleles comprise 5% to 10% of disease-causing CFTR mutations worldwide, but > 60% among Israeli patients with CF, often conferring severe disease.48 Ataluren showed promise in early studies, and a multinational phase 3 trial of this agent was completed in 2011. The results of this trial were presented at the 2012 European CF conference, as described in a company press release.49 There was a 3% difference in relative change in FEV1 from baseline compared with placebo at 48 weeks (the study’s primary end point), which did not reach significance (P > .1).
Conclusion
The past 20 years have transformed the field of CF treatment so that changing the course of this fatal illness is becoming a reality. The view of the road ahead has never been so encouraging in CF therapeutics, and there is cause for unprecedented optimism for anyone who cares for people with this devastating disease. In the next decade, it is likely that both a CFTR potentiator (Kalydeco) and at least one CFTR corrector may be available for the majority of patients with CF. These drugs have a high likelihood of slowing the rate of progression of lung disease. With the added benefit of existing therapies such as Pulmozyme and hypertonic saline, it is likely that most patients will soon be able to maintain normal lung function and nutritional status well into adulthood. The course of lung infection may similarly change, with delayed establishment of chronic infections with pathogens such as P aeruginosa. Newer antimicrobial approaches will focus on disarming these pathogens before they can establish structures associated with persistence, such as biofilms. The airway will be considered an integrated microbial community, rather than the domain of a few key pathogens, with a focus on maintaining a healthy ecologic balance. Because future therapies will aim to prevent, rather than improve, existing organ damage, one future challenge will be developing better measures of early organ dysfunction well before patients become symptomatic. Armed with important insights from newborn screening programs in Australia, we have a better understanding of the very earliest changes that occur in the infant lung.50‐52 From these observations, early biomarkers that identify previously undetectable regional changes will become available, enabling physicians to more closely monitor the progress of disease and deliver tailored, individualized therapy to those who need it most.
Acknowledgments
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Hoffman receives grant funding from the Cystic Fibrosis Foundation and the National Institutes of Health. Dr Ramsey, in her capacity as director of the Cystic Fibrosis Foundation Therapeutics Development Network Coordinating Center, has received grants from the following companies in the past 3 years: AlgiPharma AS; Amgen, Inc; Aradigm Corporation; Axcan Pharma, Inc; Bayer Healthcare AG; Chiesi Pharmaceuticals Inc; CSL Behring LLC; Gilead Sciences, Inc; GlaxoSmithKine, Inc; Inspire Pharmaceuticals, Inc; KaloBios, Inc; MerLion Pharmaceuticals GmbH; Mpex Pharmaceuticals, Inc; MPM Asset Management LLC; N30 Pharmaceuticals LLC; Novartis Pharmaceuticals Corp; Pharmaxis Ltd; PTC Therapeutics, Inc; Solvay Pharmaceuticals, Inc; Insmed, Inc; Vectura Ltd; and Vertex Pharmaceuticals Incorporated. She also receives grant funding from the Cystic Fibrosis Foundation and the National Institutes of Health.
Other contributions: The authors thank the patients and families for their participation in studies so necessary for furthering research, the many investigators and physicians who contributed to the development of these therapies, and the Cystic Fibrosis Foundation for its support, leadership, and vision.
Abbreviations
- CF
cystic fibrosis
- CFTR
cystic fibrosis transmembrane conductance regulator
- FDA
US Food and Drug Administration
- TIP
TOBI inhaled powder
Footnotes
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Ashlock MA, Beall RJ, Hamblett NM, et al. A pipeline of therapies for cystic fibrosis. Semin Respir Crit Care Med. 2009;30(5):611-626 [DOI] [PubMed] [Google Scholar]
- 2.Drug development pipeline. Cystic Fibrosis Foundation website http://www.cff.org/research/drugdevelopmentpipeline. Accessed June 26, 2012.
- 3.Accurso FJ, Rowe SM, Clancy JP, et al. Effect of VX-770 in persons with cystic fibrosis and the G551D-CFTR mutation. N Engl J Med. 2010;363(21):1991-2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramsey BW, Davies J, McElvaney NG, et al. VX08-770-102 Study Group A CFTR potentiator in patients with cystic fibrosis and the G551D mutation. N Engl J Med. 2011;365(18):1663-1672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Updated questions and answers for healthcare professionals and the public: use an approved pancreatic enzyme product (PEP). US Food and Drug Administration website. http://www.Fda.Gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm204745.Htm. Accessed June 26, 2012.
- 6.Ratjen F. What’s new in CF airway inflammation: an update. Paediatr Respir Rev. 2006;7(suppl 1):S70-S72 [DOI] [PubMed] [Google Scholar]
- 7.Geller DE, Flume PA, Staab D, Fischer R, Loutit JS, Conrad DJ. Mpex 204 Study Group Levofloxacin inhalation solution (MP-376) in patients with cystic fibrosis with Pseudomonas aeruginosa. Am J Respir Crit Care Med. 2011;183(11):1510-1516 [DOI] [PubMed] [Google Scholar]
- 8.Okusanya OO, Bhavnani SM, Hammel J, et al. Pharmacokinetic and pharmacodynamic evaluation of liposomal amikacin for inhalation in cystic fibrosis patients with chronic pseudomonal infection. Antimicrob Agents Chemother. 2009;53(9):3847-3854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Study to evaluate Arikace™ in CF patients with chronic Pseudomonas aeruginosa infections. NCT01315678. Clinicaltrials.gov. Bethesda, MD; National Institutes of Health; 2011. http://clinicaltrials.gov/ct2/show/NCT01315678. Updated March 2012. Accessed June 26, 2012.
- 10.Arikace® for nontuberculous mycobacteria. NCT01315236. Clinicaltrials.gov. Bethesda, MD; National Institutes of Health; 2011. http://clinicaltrials.gov/ct2/show/NCT01315236. Updated June 2012. Accessed June 26, 2012.
- 11.Trapnell BC, McColley SA, Kissner DG, et al. Phase 2 FTI Study Group Fosfomycin/tobramycin for inhalation in patients with cystic fibrosis with pseudomonas airway infection. Am J Respir Crit Care Med. 2012;185(2):171-178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rogers GB, Carroll MP, Serisier DJ, Hockey PM, Jones G, Bruce KD. characterization of bacterial community diversity in cystic fibrosis lung infections by use of 16s ribosomal DNA terminal restriction fragment length polymorphism profiling. J Clin Microbiol. 2004;42(11):5176-5183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tunney MM, Klem ER, Fodor AA, et al. Use of culture and molecular analysis to determine the effect of antibiotic treatment on microbial community diversity and abundance during exacerbation in patients with cystic fibrosis. Thorax. 2011;66(7):579-584 [DOI] [PubMed] [Google Scholar]
- 14.Zhao J, Schloss PD, Kalikin LM, et al. Decade-long bacterial community dynamics in cystic fibrosis airways. Proc Natl Acad Sci U S A. 2012;109(15):5809-5814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rogers GB, Hoffman LR, Döring G. Novel concepts in evaluating antimicrobial therapy for bacterial lung infections in patients with cystic fibrosis. J Cyst Fibros. 2011;10(6):387-400 [DOI] [PubMed] [Google Scholar]
- 16. A pharmacokinetic and safety study of IV gallium nitrate (Ganite) in cystic fibrosis patients. NCT01093521. ClinicalTrials.gov. Bethesda, MD: National Institutes of Health; 2010. http://clinicaltrials.gov/ct2/show/nct01093521. Updated June 14, 2012. Accessed June 26, 2012.
- 17.Kaneko Y, Thoendel M, Olakanmi O, Britigan BE, Singh PK. The transition metal gallium disrupts Pseudomonas aeruginosa iron metabolism and has antimicrobial and antibiofilm activity. J Clin Invest. 2007;117(4):877-888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parsek MR, Singh PK. Bacterial biofilms: an emerging link to disease pathogenesis. Annu Rev Microbiol. 2003;57(677-701 [DOI] [PubMed] [Google Scholar]
- 19.Halwani M, Yebio B, Suntres ZE, Alipour M, Azghani AO, Omri A. Co-encapsulation of gallium with gentamicin in liposomes enhances antimicrobial activity of gentamicin against Pseudomonas aeruginosa. J Antimicrob Chemother. 2008;62(6):1291-1297 [DOI] [PubMed] [Google Scholar]
- 20.Konstan MW, Schluchter MD, Xue W, Davis PB. Clinical use of Ibuprofen is associated with slower FEV1 decline in children with cystic fibrosis. Am J Respir Crit Care Med. 2007;176(11):1084-1089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Konstan MW, Byard PJ, Hoppel CL, Davis PB. Effect of high-dose ibuprofen in patients with cystic fibrosis. N Engl J Med. 1995;332(13):848-854 [DOI] [PubMed] [Google Scholar]
- 22.Chmiel JF, Konstan MW. Inflammation and anti-inflammatory therapies for cystic fibrosis. Clin Chest Med. 2007;28(2):331-346 [DOI] [PubMed] [Google Scholar]
- 23.Tirouvanziam R, Conrad CK, Bottiglieri T, Herzenberg LA, Moss RB, Herzenberg LA. High-dose oral N-acetylcysteine, a glutathione prodrug, modulates inflammation in cystic fibrosis. Proc Natl Acad Sci U S A. 2006;103(12):4628-4633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Vizia B, Raia V, Spano C, Pavlidis C, Coruzzo A, Alessio M. Effect of an 8-month treatment with omega-3 fatty acids (eicosapentaenoic and docosahexaenoic) in patients with cystic fibrosis. JPEN J Parenter Enteral Nutr. 2003;27(1):52-57 [DOI] [PubMed] [Google Scholar]
- 25.Meyer M, Huaux F, Gavilanes X, et al. Azithromycin reduces exaggerated cytokine production by M1 alveolar macrophages in cystic fibrosis. Am J Respir Cell Mol Biol. 2009;41(5):590-602 [DOI] [PubMed] [Google Scholar]
- 26.Wolter JM, Seeney SL, McCormack JG. Macrolides in cystic fibrosis: is there a role?. Am J Respir Med. 2002;1(4):235-241 [DOI] [PubMed] [Google Scholar]
- 27.Jones AM, Helm JM. Emerging treatments in cystic fibrosis. Drugs. 2009;69(14):1903-1910 [DOI] [PubMed] [Google Scholar]
- 28.Prescott WA, Jr, Johnson CE. Antiinflammatory therapies for cystic fibrosis: past, present, and future. Pharmacotherapy. 2005;25(4):555-573 [DOI] [PubMed] [Google Scholar]
- 29.Konstan MW, Ratjen F. Effect of dornase alfa on inflammation and lung function: potential role in the early treatment of cystic fibrosis. J Cyst Fibros. 2012;11(2):78-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rubin BK. Mucus, phlegm, and sputum in cystic fibrosis. Respir Care. 2009;54(6):726-732 [DOI] [PubMed] [Google Scholar]
- 31.Innes JA. DNase in cystic fibrosis: the challenge of assessing response and maximising benefit. Thorax. 1998;53(12):1003-1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fuchs HJ, Borowitz DS, Christiansen DH, et al. The Pulmozyme Study Group Effect of aerosolized recombinant human DNase on exacerbations of respiratory symptoms and on pulmonary function in patients with cystic fibrosis. N Engl J Med. 1994;331(10):637-642 [DOI] [PubMed] [Google Scholar]
- 33. Cystic Fibrosis Foundation. Patient registry: annual data report 2010. Cystic Fibrosis Foundation website. http://www.cff.org/UploadedFiles/LivingWithCF/CareCenterNetwork/PatientRegistry/2010-Patient-Registry-Report.pdf. Accessed June 26, 2012.
- 34.Elkins MR, Robinson M, Rose BR, et al. National Hypertonic Saline in Cystic Fibrosis (NHSCF) Study Group A controlled trial of long-term inhaled hypertonic saline in patients with cystic fibrosis. N Engl J Med. 2006;354(3):229-240 [DOI] [PubMed] [Google Scholar]
- 35.Aitken ML, Bellon G, De Boeck K, et al. CF302 Investigators Long-term inhaled dry powder mannitol in cystic fibrosis: an international randomized study. Am J Respir Crit Care Med. 2012;185(6):645-652 [DOI] [PubMed] [Google Scholar]
- 36.Bilton D, Robinson P, Cooper P, et al. CF301 Study Investigators Inhaled dry powder mannitol in cystic fibrosis: an efficacy and safety study. Eur Respir J. 2011;38(5):1071-1080 [DOI] [PubMed] [Google Scholar]
- 37.Donaldson SH, Boucher RC. Sodium channels and cystic fibrosis. Chest. 2007;132(5):1631-1636 [DOI] [PubMed] [Google Scholar]
- 38.Rommens JM, Iannuzzi MC, Kerem B, et al. Identification of the cystic fibrosis gene: chromosome walking and jumping. Science. 1989;245(4922):1059-1065 [DOI] [PubMed] [Google Scholar]
- 39.Riordan JR, Rommens JM, Kerem B, et al. Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA. Science. 1989;245(4922):1066-1073 [DOI] [PubMed] [Google Scholar]
- 40.Kerem B, Rommens JM, Buchanan JA, et al. Identification of the cystic fibrosis gene: genetic analysis. Science. 1989;245(4922):1073-1080 [DOI] [PubMed] [Google Scholar]
- 41.Oakland M, Sinn PL, McCray PB., Jr Advances in cell and gene-based therapies for cystic fibrosis lung disease. Mol Ther. 2012;20(6):1108-1115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rogers CS, Stoltz DA, Meyerholz DK, et al. Disruption of the CFTR gene produces a model of cystic fibrosis in newborn pigs. Science. 2008;321(5897):1837-1841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sun X, Sui H, Fisher JT, et al. Disease phenotype of a ferret CFTR-knockout model of cystic fibrosis. J Clin Invest. 2010;120(9):3149-3160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van Goor F, Hadida S, Grootenhuis PD, et al. Rescue of CF airway epithelial cell function in vitro by a CFTR potentiator, VX-770. Proc Natl Acad Sci U S A. 2009;106(44):18825-18830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van Goor F, Hadida S, Grootenhuis PD, et al. Correction of the F508del-CFTR protein processing defect in vitro by the investigational drug VX-809. Proc Natl Acad Sci U S A. 2011;108(46):18843-18848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clancy JP, Rowe SM, Accurso FJ, et al. Results of a phase IIa study of VX-809, an investigational CFTR corrector compound, in subjects with cystic fibrosis homozygous for the F508del-CFTR mutation. Thorax. 2012;67(1):12-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Vertex corrects and provides additional data from recent interim analysis of phase 2 combination study of VX-809 and KALYDECO™ (ivacaftor) in people with cystic fibrosis who have two copies of the F508del mutation. Vertex Pharmaceuticals Inc website. http://investors.vrtx.com/releasedetail.Cfm?Releaseid=677520. Published May 29, 2012. Accessed June 26, 2012.
- 48.Kerem B, Chiba-Falek O, Kerem E. Cystic fibrosis in Jews: frequency and mutation distribution. Genet Test. 1997;1(1):35-39 [DOI] [PubMed] [Google Scholar]
- 49. Top-line data from phase 3 trial of ataluren in patients with nonsense mutation cystic fibrosis show promising results. PTC Therapeutics, Inc website. http://ptct.Client.Shareholder.Com/releasedetail.Cfm?Releaseid=681445. Published June 8, 2012. Accessed June 26, 2012.
- 50.Pillarisetti N, Williamson E, Linnane B, et al. Australian Respiratory Early Surveillance Team for Cystic Fibrosis (AREST CF) Infection, inflammation, and lung function decline in infants with cystic fibrosis. Am J Respir Crit Care Med. 2011;184(1):75-81 [DOI] [PubMed] [Google Scholar]
- 51.Ranganathan SC, Parsons F, Gangell C, Brennan S, Stick SM, Sly PD. Australian Respiratory Early Surveillance Team for Cystic Fibrosis Evolution of pulmonary inflammation and nutritional status in infants and young children with cystic fibrosis. Thorax. 2011;66(5):408-413 [DOI] [PubMed] [Google Scholar]
- 52.Gangell C, Gard S, Douglas T, et al. AREST CF Inflammatory responses to individual microorganisms in the lungs of children with cystic fibrosis. Clin Infect Dis. 2011;53(5):425-432 [DOI] [PubMed] [Google Scholar]