Abstract
Internet-based interventions have potential to reduce HIV and STD transmission among men who meet male sexual partners online. From November 2009 to May 2010 we surveyed dating and hook-up website users (n=3,050), website owners (n=18), and health department HIV/STD directors (n=81) to identify structural and behavioral prevention interventions that could be implemented online and which a majority of website users were willing to use, owners were willing to implement, andHIV/STD directors perceived to beeffective. A majority of each of the three stakeholder groups agreed on the following: 1) automated HIV/STD testing reminders; 2) local STD test site directories; 3) links to sex-positive safe sex videos; 4) access to sexual health experts; 5) profile options to include safer sex preference; 6) chat rooms for specific sexual interests; 7) filtering partners by their profile information; and 8) anonymous e-card partner notification for STD exposure. Findings help build consensus about how to prioritize resources for implementing online HIV and STD prevention interventions and highlight differences between stakeholders to guide future discussion about how to advance prevention efforts.
Keywords: HIV prevention, STD prevention, internet, men who have sex with men, sexual networks, structural interventions
INTRODUCTION
Many men who have sex with men (MSM) search for new relationships, both casual and romantic, on websites catering to dating and to finding sexual partners. As many websites offer memberships for free or low cost, their use is widespread, and many men search for partners on multiple sites. Prior studies have shown that MSM who use the internet to find sexual partnersare more likely to report unprotected anal intercourse with non-primary partners and more likely to report a previous STD compared to other MSM(1-3). As early as 1999, an outbreak of syphilis in MSM was associated with meeting sexual partners on the internet in San Francisco (4). By 2002, the internet surpassed bathhouses, sex clubs, and bars as the most frequently named type of venue where individuals diagnosed with syphilis reported meeting partners in some health jurisdictions(5).However, over time it appears that differences in sexual risk behavior between internet users and non-internet users may be diminishing (6).
While the effect of the internet on individual risk behavior may be unclear, its impact at the population level deserves our close attention. There are several attributes of the internet that may either increase HIV and STD transmission, or conversely, may enable or promote highly effective prevention strategies. On the one hand, the internet may affect the shape and structure of sexual networks (7, 8). For example, it enables individuals to meet new romantic and sexual partners outside their immediate social circle. Additionally, in some areas of the country, particularly rural areas with few organizations or bars catering to MSM, the internet may be one of the few ways MSM can meet. In large cities with established gay neighborhoods, organizations, bars, and clubs, the internet may provide an additional venue for partners to meet each other. On the other hand, the internet has strong appeal as a tool for disseminating health information and for delivering specific HIV and STD prevention interventions. The internet allows for communicating messages quickly and inexpensively to large numbers of people, including populations at risk for HIV and other STDs who are difficult to reach by other means, and for tailoring those messages to individuals with different demographic characteristics, preferences, and risks. Furthermore, many dating and hook-up websites already enable men to search for partners with characteristics they desire and to disclose sensitive information such as HIV status more comfortably than they may be able to do in other situations (9). On many websites, men can exchange information about HIV and STD status, drug and alcohol use, and their preferences for sex with or without condoms. To the extent that users describe themselves truthfully, exchanging information allows men to make more informed decisions about their health.
Historically, the public health field has relied on individual or small group behavioral interventions and online partner notification (10, 11). The internet’s ability to distribute information efficiently or to assist MSM in making informed choices about their partners has not been fully leveraged. This may be particularly important for those individuals who do not choose to participate in formal behavioral interventions. There is currently no consensus about which online HIV/STD prevention strategies would be most effective, with evidence through randomized controlled trials (RCTs) or other rigorous studies, or are likely to be accepted by both website owners and users. The latterhas resulted in prevention programs focusing on behavioral interventions that may be used by only a small minority of men online. Offline, few behavioral interventions have shown evidence of reducing HIV or STD incidence at the population level (12-14). In one national study, only one percent of men sampled in bath houses or bars had ever participated in individual-level interventions(15); at present, it is unlikely that many more men would have participated in prevention interventions online. Moreover, website owners and health department HIV/STD directors are likely to have very different perspectives and priorities. HIV/STD directors are not likely to focus on the business of running a dating or hook-up website, to fully appreciate the technology used to run the sites, or to consider the costs, capabilities, or limitations of the website when implementing programs. For their part, website owners cannot be expected to assess the evidence for or against specific prevention interventions, to design health promotion programs, or to prioritize user health benefits in their business models.
In brief, we perceive no clear consensus about which HIV/STD prevention strategies may be most effective, most acceptable to website owners, and most likely to be used by websiteclients. This study therefore brings together, for the first time, the voices of three groups who are key stakeholders for HIV and STD online prevention programs: website users, website owners, and public health department HIV/STD directors.
METHODS
Overall Study Goal and Design
The overarching goal of this study was to garner the opinions of three different groups of stakeholders through three separate cross-sectional surveys as to which existing and potential online interventions are perceived to be effective in reducing HIV and STD transmission, are likely to be used by large numbers of MSM, and are likely to be implemented by website owners catering to MSM. Recruitment, eligibility criteria, and survey measures differed between the three stakeholder groups who served as study subjects.
Study Subjects
We developed a comprehensive list of gay-oriented dating and hook-up websites through consultation with experts, key informants, and a review of the literature, and based our sampling frame of website owner stakeholders on this list. Some sites exclusively served gay and bisexual men; others targeted persons of all sexual orientations. Only sites with users in the United States were included. For all websites that we identified, we attempted to recruit the owner or most senior manager available through e-mail invitations and follow-up telephone calls. Several managers collected input from different staff members, but only one composite survey was submitted for analysis for each website.
We invited all directors of HIV and STD programs from state health departments and separately funded city health departments to participate, using membership rosters of the National Coalition of STD Directors (NCSD) and National Alliance of State and Territorial AIDS Directors (NASTAD).
We recruited users by placing banner advertisements on several hook-up and dating websites. In order to increase survey response in underrepresented groups such as Asian Pacific Islanders, different community organizations catering to minority MSM also sent e-newsletters inviting their members to participate. We gave no incentives for participation. Websiteusers were eligible if they were over 18 years old, lived in the United States, identified as male or female-to-male transgender, and had looked for a male sex partner online in the prior six months. We established targets to ensure inclusion from five typically underrepresented groups: 1) MSM in the ten states with the fewest number of same-sex couples (Alabama, Idaho, Iowa, Louisiana, Mississippi, Montana, North Dakota, South Dakota, West Virginia, and Wyoming) (16); 2) African American MSM; 3) MSM younger than 25 years old; 4) HIV-positive MSM; and 5) MSM with higher-risk sexual practices. We defined higher-risk sexual practices as those individuals who reported unprotected anal sex with two or more partners of unknown or opposite HIV status in the previous six months.
Measures
We asked each of the three stakeholder groups to evaluate 41 potential behavioral and structural online HIV and STD prevention interventions-a list elaborated through searching the literature (11, 17-21), cataloguing interventions currently being implemented on different websites, and focus group discussions. Additionally, we augmented this list as new possible interventions arose during the course of the surveys (see Table 1 for a complete list of interventions, as described in the surveys). Of note, the list of potential online interventions was crafted to be comprehensive without regard to whether RCT or other rigorous evidence of efficacy was available under the rationale that not all interventions in practice have been tested and that our data could help guide those that are most promising for future rigorous testing through RCTs. We first surveyed website owners and HIV/STD directors, and additional strategies that they suggested in open-ended questions in these surveys were then incorporated into the survey given to website users.
Table 1.
Brief descriptions of online HIV/STD prevention strategies assessed by HIV/STD directors, MSM website users, and website owners stakeholders.
| Broad strategy | Specific interventions |
|---|---|
| Searching for partners |
|
| Profile options |
|
| Site information |
|
| Health information |
|
| Socializing information |
|
| Education and outreach |
|
| HIV/STI testing |
|
| Partner notification |
|
The key measures of interest were to gauge opinions on likely efficacy, use, and willingness to implement various types of interventions online. We asked website owners to rate how willing they were to implement each intervention using a 5-point Likert scale (1=very unwilling, 2=unwilling, 3=neutral, 4=willing, 5=very willing). Not applicable was also given as an option. We asked website users to rate their likelihood of using different services or strategies on a 5-point Likert scale (1=very unlikely, 2=unlikely, 3=neutral, 4=likely, 5=very likely). We asked HIV/STD directors to rank how much they perceived different services or interventions would increase or decrease HIV and/or STD transmission. Survey options included a similar 5-point Likert scale (1=substantial increase, 2=some increase, 3=no impact, 4=some decrease, 5=substantial decrease). After weighing the trade-offs between a high response rate and comparability, in some cases we asked the HIV/STD directors to select strategies they preferred from a longer list of options rather than to rate each intervention individually.
Analysis
We determined areas of agreement and disagreement between the three groups of stakeholders. For each of the 41 potential online interventions, we classified the stakeholders as providing support if a majority (≥50%) of HIV/STD directors selected them as having an impact on reducing HIV or STD transmission, if a majority of MSM website users ranked them as likely or very likely to use, and if a majority of website owners were willing or very willing to implement them. We first identified those interventions supported by all three groups of stakeholders, followed by determining those interventions that no group supported, as well as interventions that two of the three stakeholder groups supported. Comparisons were examined using the chi-squared test, and p-values of less than 0.05 were considered statistically significant. Stata 11.0 was used for analysis.
The study protocol was reviewed and approved by the Committee on Human Research of the University of California at San Francisco. All participants provided online consent.
RESULTS
We collected stakeholder survey data between November 2009 and May 2010. Of 114 members of the NCSD and NASTAD identified, 81 (72%) responded to our survey. Of 31 website owners contacted, 18 (58%) completed the survey. Some participating website owners represented sites which exclusively served gay and bisexual men; others served individuals of all sexual orientations. These sites served men looking for brief sexual encounters or “hook-ups,” dating, relationships, and male escorts. Some sites catered to men looking specifically for unprotected sex. During the eight weeks of recruitment for website users, 6,896 responded to the link; 6,032 (87%) were considered eligible, consented to participate, and went on to answer the first question; 3,050 (51%) completed the survey and are included in the present analysis. The characteristics of these website users are shown in Table 2. The majority were under the age of 35 years (57%) and white (69%), with 13% identifying as African American/black and 8% as Latino. Although we did not collect demographic data on persons who did not complete the survey, our sample includes comparable but somewhat fewer white and Latino participants, more African-American participants, and similar percentages of Asian-Pacific Islander and Native American participants as one national study of MSM(22).
Table 2.
Characteristics of MSM website users completing an online survey of internet-based HIV prevention intervention approaches (n=3,050).
| Variable | Percent of website user respondents |
|---|---|
|
| |
| Age group in years: | |
| 18-24 | 27 |
| 25-34 | 30 |
| 35-54 | 37 |
| 55-64 | 5 |
| >64 | 1 |
|
| |
| Race/ethnicity: | |
| White | 69 |
| Black | 13 |
| Latino | 8 |
| Native American | 3 |
| Asian/Pacific Islander | 3 |
| Multi-racial | 3 |
| Other | 1 |
|
| |
| HIV status: | |
| HIV-negative | 76 |
| HIV-positive | 15 |
| Does not know | 7 |
| Declined to state | 2 |
|
| |
| Two or more unprotected sexual partners, last 6 months |
10 |
|
| |
| Weekly hours online looking for sexual partners: | |
| <3 | 23 |
| 3-5 | 30 |
| 6-13 | 26 |
| >13 | 21 |
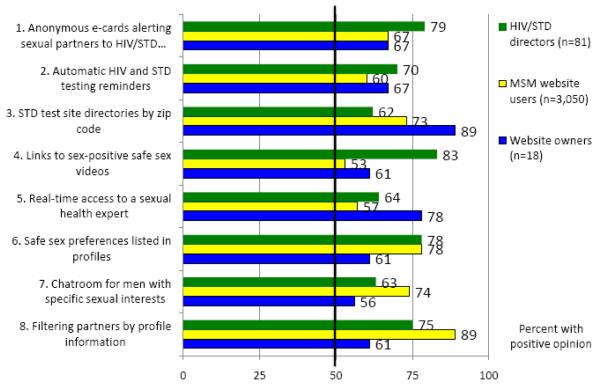
Of the 41 proposed online HIV/STD prevention interventions, there were eight which a majority of HIV/STD directors perceived would reduce HIV and/or STD transmission, a majority of website users were willing to use, and a majority of website owners were willing to implement (Figure 1). These interventions included ways of searching for partners (e.g., filtering partners by profiles, or providing chat rooms for men sharing preferences for particular kinds of sex or partners), the profile option of safer sex preference, health information delivered by a sexual health expert, education through sex-positive videos, STD testing facilitated by a directory, and automated reminders to get tested at an interval of the user’s choice. In addition, a majority of all three stakeholder groups supported the anonymous e-card approach to partner notification.
Figure 1.
Stake holder opinions on web-based HIV prevention strategies: types of interventions favorable to the majority of HIV/STD directors, MSM website users, and website owners as to their effectiveness, likely use, or acceptability,
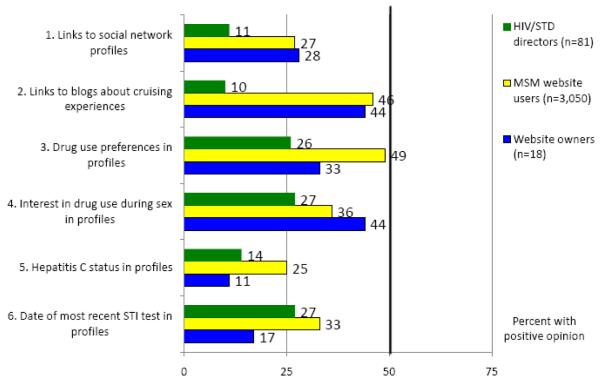
Six online interventions failed to garner support from a majority of any of the stakeholder groups (Figure 2). Only a minority of each of the three groups felt that links from dating and hook-up sites to social network profiles, links to blogs about cruising, or including in profiles drug use preferences, interest in methamphetamine use during sex (party and play or “PnP” preference), hepatitis C status, or the date of the most recent STD test would be worthwhile, appealing, or feasible.
Figure 2.
Stakeholder opinions on web-based HIV prevention strategies: types of interventions not favorable to the majority of HIV/5TD directors, M5M website users, and website owners as to their effectiveness, likely use, or acceptability,
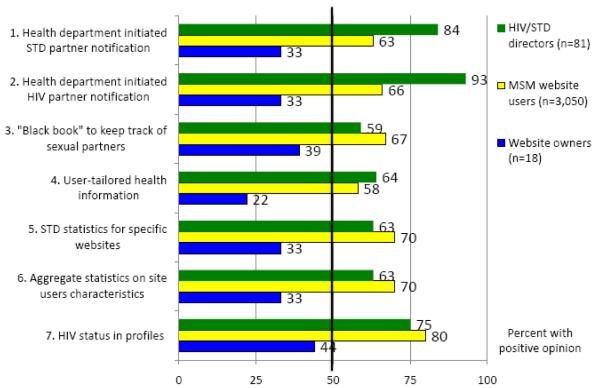
The majority of HIV/STD directors and website users supported seven interventions that only a minority of website owners were willing to implement (Figure 3). These included health department initiated partner notification for both STD and HIV exposures, keeping a “black book” of sexual partners online, and user-tailored health information. Additionally, website owners were less likely to endorse making statistics on STDs occurring among users finding partners on their website or the characteristics of users in aggregate, such as the number of men on their website who listed preferences for safe sex or barebacking, publicly available on outside websites. In contrast to health officials and the users themselves, website owners were less likely to endorse the inclusion of HIV status in profiles.
Figure 3.
Stakeholder opinions on web-based HIV prevention strategies: types of interventions favorable to the majority of HIV/STD directors and MSM website users, but not to website owners as to their effectiveness, likely use, or acceptability.
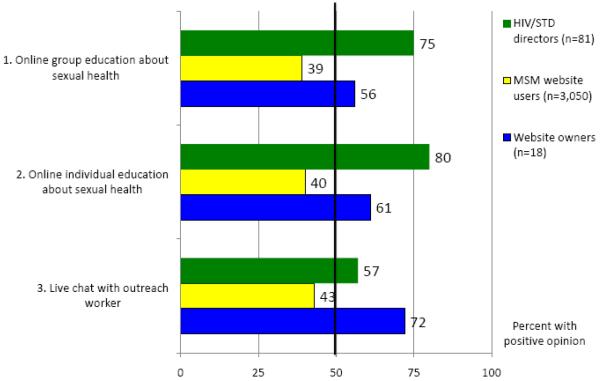
Three interventions were supported by the majority of website owners and health officials, but garnered little enthusiasm among users (Figure 4). These included online individual and group education sessions and live chat with an outreach worker.
Figure 4.
Stakeholder opinions on web-based HIV prevention strategies: types of interventions favorable to the majority of HIV/STD directors and website owners, but not to MSM website users as to their effectiveness, likely use, or acceptability.
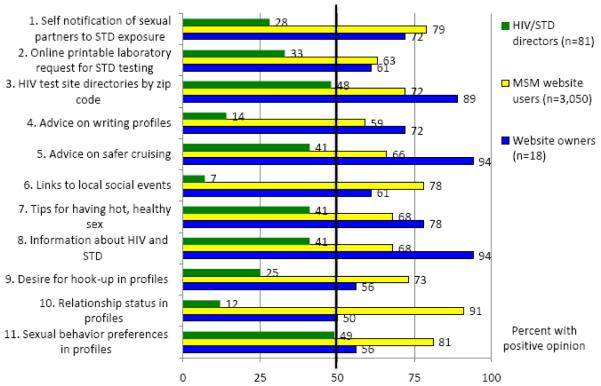
There were 11 interventions that the majority of users and owners supported, but were not deemed likely to have an impact on HIV and STD transmission by health officials (Figure 5). In contrast to e-card and health department initiated partner notification, most health officials did not support relying on individuals to notify their own partners of possible HIV or STD exposures. The ability to generate printable laboratory slips signed by a physician, enabling users to go directly to local laboratories to get tested for STDs without first being examined by a healthcare provider, was not endorsed by the majority of HIV/STD directors. Several additional interventions were appealing to users and feasible to owners, but were perceived to have little impact on transmission in the opinion of HIV/STD directors, such as advice on writing profiles, links to social events, and including relationship status and sexual behavior preferences in user profiles.
Figure 5.
Stakeholder opinions on web-based HIV prevention strategies: types of interventions favorable to the majority of MSM website users and website owners, hut not to HIV/STD directors as to their effectiveness, likely use, or acceptability.
We found that African-American survey participants were generally more supportive of strategies than white participants. However, while a majority of African-American participants supported “HIV status” and “safe sex preferences” as profile options, they did so at slightly lower levels than white participants (77% vs. 82%, chi square 4.61, p<0.05, and 73% vs. 80%, chi square 8.85, p<0.01, respectively).
Fifteen percent of survey respondents self-reported as HIV-positive, 76% as HIV-negative, 7% as unknown, and 2% declined to answer. In examining differences between these groups, we found that HIV-negative respondents were generally more supportive of interventions than their HIV-positive counterparts. For example, 85% of HIV-negative participants supported including their HIV status on their profile as compared to 66% of HIV-positive participants (chi square 81.66, p<0.01). However, HIV-positive respondents were more interested than HIV-negative respondents in having chat rooms available for men with specific preferences such as “safe sex only,” “barebacking,” or “HIV-positive” (85% vs. 75%, chi square 22.90, p<0.01). HIV-positive MSM were also more interested in several profile options, including the option to include preferences for using or not using methamphetamines during sex (43% vs. 35%, chi square 10.32, p<0.01), the option to list specific sexual behaviors (e.g., “top,” “bottom,” “oral”) (85% vs. 81%, chi square 5.06, p=0.02), and the option to include preference for hooking-up (80% vs. 72%, chi square 11.05, p<0.01).
DISCUSSION
We believe the best way to succeed in promoting public health online, and more specifically to reduce HIV and STD infections, is to prioritize the implementation of theeight strategies that gained the support of a majority of all three stakeholder groups. Where rigorous evidence of efficacy is lacking, these interventions may also garner priority to be tested in future RCTs.Many of these eight strategies allow three stakeholder groups to share responsibility and play to their respective strengths and interests. In this study, we found that all three groups were willing to participate in online HIV and STD prevention efforts and to contribute their specific expertise and insight. For example, HIV/STD directors were willing to create and maintain directories of STD test sites, website owners are willing to have links to them, and users are willing to access them. With the exception of continuous availability of a medical expert online, it is notable that the strategies supported by a majority of all three stakeholder groups may be considered “structural interventions,” in that once implemented (some at relatively low, one-time costs) as policies or software code, their preventive effects would persist over long periods with wide reach (23).
In addition to moving ahead with strategies which all three groups supported, we believe that there are benefits in further discussing those interventions which two out of the three stakeholder groups endorsed. First, if experts favorably weigh the evidence and users express willingness to use certain interventions, then owners may find some of them more acceptable. These interventions included health-department initiated STD partner notification, HIV partner notification, keeping a black book of online sexual partners, user-tailored health information, STD statistics for specific websites, aggregate statistics on website user characteristics, and inclusion of HIV status in profiles. It is not surprising that a majority of owners failed to support several of these interventions. For example, publicity about high rates of syphilis occurring among men who reported meeting partners on a particular website could deter customers. Second, potential interventions supported by website owners and HIV/STD program directors may be made more acceptable or appealing to certain groups of users, such as high-risk or HIV-positive men. Interventions supported by website owners and users but not judged likely to reduce HIV and/or STD transmission by health experts, such as including specific sexual behaviors in profile screens or printable STD laboratory request slips, may be those to prioritize for future research to determine their efficacy and impact. Focused conversations between HIV/STD directors and website owners may foster greater mutual understanding and productive partnerships. While some differences may never be resolved, we expect that further dialogue andmodifying some interventions will produce strategiesmore acceptable to all parties. Where there is opposition based on a perception that users will reject the idea, we hope that the voices of the users themselves, which we have sought out, will help resolve these differences. For example, website owners may not be aware that the majority of website users, including those who are HIV-infected, support the option of listing HIV-status in their online profiles, or that they support partner notification.
We also identified several possible online interventions that did not attract support from any of the three stakeholders, indicating that even if proven efficacious, their public health impact may be limited. Without health program directors’ support, funding for development may be more difficult to obtain. Without interest among website users, interventions will have little chance of being effective at reducing transmission at a population level. If interventions are believed by website owners to be against their own or their customers’ interests, particularly those that depend on changes to the website’s architecture and business model, they will not be feasible. Our study identified six online interventions which did not appeal to the majority of any stakeholder group: links to social network profiles like Facebook, links to blogs about cruising experiences, profile options for drug use preferences, interest in recreational drug use during sex (“PnP”), hepatitis C status, and date of most recent STD tests. We recognizethat should evidence for the efficacy of these interventions be found, their appeal to some or all of the stakeholder groups may change.
We recognize that the lack of data on the true efficacy of many of the interventions we surveyed (i.e., from RCTs) is a broad limitation to our study. In fact, few interventions have direct evidence of efficacy in reducing HIV or STD incidence in RCTs, and few have evidence that they are not efficacious in RCTs(12-14). Unless directors were familiar with specific studies related to these interventions, they were unable to base their perceptions of existing interventions on data. Furthermore, many of the interventions – such as automatic reminders to get tested generated by the dating sites at intervals of the users’ choice, or a website that would provide aggregate statistics on site user characteristics (i.e. percent of men who say they are looking for “safe sex only”) -do not exist. Additionally, in some cases the perceptions of programs’ effectiveness have not been supported by data. For example, studies published after this survey was conducted have shown e-cards to be less effective than directors initially perceived (24-26). In contrast, data support directors’ perceptions that relying on infected individuals to notify their own partners is not the most effective strategy (27). Forthis study, we rely on the knowledge and judgment of the public health directors of HIV and STD control programs, since in many instances this is what drives investment in programs.
Our study also suffers from the limitation of the sampling design. We believe that given the large proportion of all state and territorial HIV and STD directors who participated, we have a solid understanding of their current opinions. Similarly, our study included most of the largest websites used for finding sexual partners. However, like most online, anonymous surveys, the sample of users presents the highest degree of uncertainty as to who they represent due to self-selection. However, our demographic data for website users are comparable to recent estimates of the make-up of MSM in the United States (22). We also recognize limitations in our measures. We found it difficult to concisely describe the content of real and hypothetical interventions, and it is possible that interpretations of what was meant varied greatly, despite efforts to maximize internal validity by piloting the surveys with key informants and target population members.
In the interest of minimizing time demands and increasing the response rate, we shortened the survey of HIV/STD program directors to allow them to pick their top strategies rather than to assess each one separately, thus introducing some incompleteness and lack of comparability for several items. Part of the rationale for this decision was also that, unlike website owners and users who only rated each intervention on one scale, HIV/STD directors were asked to estimate strategies’ impact on STDs and HIV separately. This required more time. We therefore compromised in order to limit the survey length. Of note, these methods were able to garner opinions on most of the interventions, and we gained the participation of the large majority of HIV/STD directors in the United States.If asked to evaluate each intervention individually, it is possible that HIV/STD directors may have supported more of the proposed interventions.
Finally, the use of technology to seek new sexual partners is a rapidly evolving field. Since our study, use of Global Positioning Systems technology to allow searching for nearby partners has increased. While we did not include the owners of these mobile applications in our survey, many of the interventions proposed may still be applicable.
Rapid change in technology will alter the way men find new partners, and likely affect rates of sexually transmitted infections, including HIV. The challenge for public health is to leverage these new technologies in order to unleash their full potential for prevention. A combination of online strategies will need to be offered to benefit the diverse MSM who use dating and hook-up websites, even if they do not choose to participate in a direct dialogue with prevention practitioners. Further dialogue and development of mutually beneficial partnerships between public health and website owners is necessary for increasing implementation of prevention strategies and for measuring their success. By solidifying these partnerships, we can create environments that help reduce HIV and STD transmission. This will be an important step towards assuring that that the mission of public health as described in 1988 by the Institute of Medicine – “to fulfill society’s interest in assuring conditions in which people can be healthy” (28) – includes the online environments of the twenty-first century.
ACKNOWLEDGEMENTS
We would like to extend a heartfelt thank you to all of the participants of this study: the thousands of website users whose feedback will help assure us that whatever strategies are adopted will be well-accepted by the community; HIV and STD program directors, who took time to assess what would have the biggest impact on health; and the website owners and managers who have taken time from their work to help us understand how best to leverage the internet’s many resources to promote health for us all. Additionally, we would like to thank Dana Cropper-Williams, Kelly Mayor, Dave Kern, Julie Scofield, Ed Halteman, Stephan Adelson, Matthew Amsden, Coco Auerswald, Kyle Bernstein, Sheana Bull, Mary Ann Chiasson, Kevin Cranston, Alberto Curotto, Beau Gratzer, Paul Harterink, Sabina Hirshfield, Shana Krochmal, Deb Levine, Spencer Lieb, Julia Marcus, Laura Nixon, Jeffrey O’Malley, Jackson Peyton, John Peterson, Jim Pickett, Frank Strona, Jo Ellen Stryker, Patrick Sullivan, Adam Vaughn, Edward White, Ron Stall, Bill Woods, Terry Dyer, Andy Connors, Kyriell Noon, Jason Riggs, Jorge Vieto, Michael Hyde, Greg Ford, Heidi Bauer, Gail Bolan, Jessica Frasure, Alice Gandelman, Tom Gray, Holly Howard, Greg Mehlhaff, Emily Quinn, Daniella Matthews-Trigg, Michael Samuel, Michael Waddell, Eric Nielson, Kevin O’Malley, Tai Lockspeiser and Alan Le.
Funding: This study was supported by grant #107503-45-RGBR from amfAR, the Foundation for AIDS Research. Jonathan Volk’s contribution was supported by grant T32 MH19105 from the National Institutes of Mental Health of the US Public Health Service.
Footnotes
(NOTE: A report with a more detailed discussion of the different interventions, qualitative data including quotes from participants, examples of recruitment advertisements, more detailed analyses of sub-group differences, and lengthier discussions of comparisons of this sample with national population estimates of MSM is available at www.stopaids.org/online.)
REFERENCES
- 1.McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. JAMA. 2000;284(4):443–6. doi: 10.1001/jama.284.4.443. Epub 2000/07/25. [DOI] [PubMed] [Google Scholar]
- 2.Elford J, Bolding G, Davis M, Sherr L, Hart G. Web-based behavioral surveillance among men who have sex with men: a comparison of online and offline samples in London, UK. J Acquir Immune Defic Syndr. 2004;35(4):421–6. doi: 10.1097/00126334-200404010-00012. [DOI] [PubMed] [Google Scholar]
- 3.Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: prevalence, predictors, and implications for HIV prevention. Arch Sex Behav. 2002;31(2):177–83. doi: 10.1023/a:1014739203657. [DOI] [PubMed] [Google Scholar]
- 4.Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA. 2000;284(4):447–9. doi: 10.1001/jama.284.4.447. [DOI] [PubMed] [Google Scholar]
- 5.California Department of Public Health Sexually Transmitted Disease Control Branch State of California Syphilis Elimination Surveillance Data. 2009 [Google Scholar]
- 6.Al-Tayyib AA, McFarlane M, Kachur R, Rietmeijer C. Finding Sex Partners on the Internet: What is the Risk for Sexually Transmitted Infections? Sexually transmitted infections. 2008 doi: 10.1136/sti.2008.032631. [DOI] [PubMed] [Google Scholar]
- 7.O’Leary C, Kerndt P. Syphilis and HIV in Sexual Networks of Men who have Sex with Men (MSM) in Los Angeles County, California; National STD Prevention Conference; March 11; Chicago, IL. 2008. [Google Scholar]
- 8.Wohlfeiler D, Potterat JJ. [Google Scholar]
- 9.Chiasson MA, Hirshfield S, Remien RH, Humberstone M, Wong T, Wolitski RJ. A comparison of on-line and off-line sexual risk in men who have sex with men: an event-based on-line survey. J Acquir Immune Defic Syndr. 2007;44(2):235–43. doi: 10.1097/QAI.0b013e31802e298c. [DOI] [PubMed] [Google Scholar]
- 10.Bull S, Pratte K, Whitesell N, Rietmeijer C, McFarlane M. Effects of an Internet-based intervention for HIV prevention: the Youthnet trials. AIDS and behavior. 2009;13(3):474–87. doi: 10.1007/s10461-008-9487-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chiasson MA, Shaw FS, Humberstone M, Hirshfield S, Hartel D. Increased HIV disclosure three months after an online video intervention for men who have sex with men (MSM) AIDS care. 2009;21(9):1081–9. doi: 10.1080/09540120902730013. [DOI] [PubMed] [Google Scholar]
- 12.Herbst JH, Sherba RT, Crepaz N, Deluca JB, Zohrabyan L, Stall RD, et al. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. J Acquir Immune Defic Syndr. 2005;39(2):228–41. Epub 2005/05/21. [PubMed] [Google Scholar]
- 13.Johnson WD, Hedges LV, Ramirez G, Semaan S, Norman LR, Sogolow E, et al. HIV prevention research for men who have sex with men: a systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2002;30(Suppl 1):S118–29. [PubMed] [Google Scholar]
- 14.Institute of Medicine . No Time to Lose: Getting More from HIV Prevention. National Academy Press; Washington, D.C.: 2001. p. xxiii.p. 227. [PubMed] [Google Scholar]
- 15.Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, Dinenno E, et al. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors--United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003-April 2005. MMWR Surveill Summ. 2006;55(6):1–16. [PubMed] [Google Scholar]
- 16.Gates G. Same-sex Couples and the Gay, Lesbian, Bisexual Population: New Estimates from the American Community Survey. 2006 Available from: http://escholarship.org/uc/item/8h08t0zf.
- 17.Bull SS, McFarlane M, King D. Barriers to STD/HIV prevention on the Internet. Health education research. 2001;16(6):661–70. doi: 10.1093/her/16.6.661. [DOI] [PubMed] [Google Scholar]
- 18.Levine D, Rebchook G, Curotto A. CaliforniaMen.net: The Development of an Online Structural HIV Prevention Intervention for MSM; National HIV Prevention Conference; Atlanta, GA. 2007 December 3; [Google Scholar]
- 19.Hooper S, Rosser BR, Horvath KJ, Oakes JM, Danilenko G. An online needs assessment of a virtual community: what men who use the internet to seek sex with men want in Internet-based HIV prevention. AIDS and behavior. 2008;12(6):867–75. doi: 10.1007/s10461-008-9373-5. Epub 2008/04/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bowen AM, Horvath K, Williams ML. A randomized control trial of Internet-delivered HIV prevention targeting rural MSM. Health education research. 2007;22(1):120–7. doi: 10.1093/her/cyl057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mimiaga MJ, Fair AD, Tetu AM, Novak DS, Vanderwarker R, Bertrand T, et al. Acceptability of an internet-based partner notification system for sexually transmitted infection exposure among men who have sex with men. American journal of public health. 2008;98(6):1009–11. doi: 10.2105/AJPH.2006.098467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lieb SM, Stephen J, Fallon P, Samuel R, Friedman P, Daniel R, Thompson M, Gary J, Gates P, Liberti TM, et al. Statewide Estimation of Racial/Ethnic Populations of Men Who Have Sex with Men in the U.S. Public Health Reports. 2011;126(1):60–72. doi: 10.1177/003335491112600110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wohlfeiler D, Ellen J. The Limits of Behavioral Interventions for HIV Prevention. In: Cohen L, Chávez V, Chehimi S, editors. Prevention is primary: strategies for community well-being. 2nd ed Jossey-Bass; San Francisco, CA: 2010. pp. 352–70. [Google Scholar]
- 24.Kerani RP, Fleming M, DeYoung B, Golden MR. A randomized, controlled trial of inSPOT and patient-delivered partner therapy for gonorrhea and chlamydial infection among men who have sex with men. Sexually transmitted diseases. 2011;38(10):941–6. doi: 10.1097/OLQ.0b013e318223fcbc. Epub 2011/09/22. [DOI] [PubMed] [Google Scholar]
- 25.Rietmeijer CA, Westergaard B, Mickiewicz TA, Richardson D, Ling S, Sapp T, et al. Evaluation of an online partner notification program. Sexually transmitted diseases. 2011;38(5):359–64. doi: 10.1097/OLQ.0b013e31820ef796. Epub 2011/02/24. [DOI] [PubMed] [Google Scholar]
- 26.Plant A, Rotblatt H, Montoya JA, Rudy ET, Kerndt PR. Evaluation of in SPOTLA.org: an Internet partner notification service. Sexually transmitted diseases. 2012;39(5):341–5. doi: 10.1097/OLQ.0b013e31824e5150. SPOTLA.org Epub 2012/04/17. [DOI] [PubMed] [Google Scholar]
- 27.Mathews C, Coetzee N, Zwarenstein M, Lombard C, Guttmacher S, Oxman A, Schmid G. Strategies for partner notification for sexually transmitted diseases. Cochrane Database Syst Rev. 2001:CD002843. doi: 10.1002/14651858.CD002843. [DOI] [PubMed] [Google Scholar]
- 28.Institute of Medicine (U.S.) Committee for the Study of the Future of Public Health. The future of public health. xii. National Academy Press; Washington, D.C.: 1988. p. 225. [Google Scholar]