Abstract
Objective
The aim of this study was to evaluate cardiac function and clinical outcomes in perioperative pediatric burn patients.
Methods
Transesophageal echocardiography data was collected on 40 patients from 2004-2007. Of the 40 patients who received exams, a complete set of cardiac parameters and outcome variables was obtained in 26 patients. The mean age of the patients was 9.7 ± 0.9 years old, and the mean total body surface area burn size was 64% ± 3%. Patients were divided into two groups based on systolic function. One group represented patients with ejection fractions of >50% and the other group ejection fractions of ≤50%. Clinical variables were then compared among the groups.
Results
In our cohort, systolic dysfunction was observed in 62% of patients (EF ≤50%). Systolic dysfunction was associated with a statistically significant increase in number of surgeries, ventilator days and length of stay in the intensive care unit. The length of stay in patients with preserved systolic function and those with systolic dysfunction was 34.3 ±3.3 days and 67.2 ± 4.0 days respectfully. Diastolic function measurements were obtained in 65% and 88% had evidence of diastolic dysfunction. Diastolic dysfunction was not associated with any statistically significant correlations.
Conclusions
This study lends evidence to the well-supported basic science models showing cardiac dysfunction following burns. Additionally, it shows that cardiac dysfunction can have clinical consequences. To our knowledge this is the first study that shows the clinical sequelae of systolic dysfunction in the perioperative pediatric burn population.
Keywords: Cardiac dysfunction in burns, Length of stay in Burn Intensive Care Units, Systolic Dysfunction
Introduction
Myocardial depression is well documented following experimental burn injury. Adams et al formally described slowed relaxation, decreased diastolic compliance, and impaired left ventricular contractility in guinea pigs following burn injury 1-3. Multiple animal models of burn injury have similarly demonstrated impaired cardiac function 4-12. Specifically, these models show that myocardial contractile dysfunction and impaired diastolic myocardial relaxation occur following burn injury.
Clinically, myocardial dysfunction following burn injury and its related sequelae remains somewhat controversial. There are several small studies that support evidence of myocardial depression. For example, Reynolds et al, 13 retrospectively reviewed a small cohort of pediatric patients with greater than 60% total body surface area (TBSA) burns using Swan-Ganz catheter recordings; they found depressed left ventricular function throughout the acute resuscitation period. Minifee et al 14 found that large TBSA burns resulted in high circulating endogenous epinephrine levels. Despite increased catecholamine levels, cardiac function remained relatively hypocontractile. In addition to myocardial depression, myocardial injury has also been described in response to thermal injury. Murphy et al 15 found that patients with greater than 15% TBSA injury had an elevation in troponin. These authors also observed a reduced stroke work despite a progressively increased pulmonary artery occlusion pressure (PAOP) in the acute resuscitation period. On the other hand, others have reported preservation of cardiac function following burn injury. Goodwin et al 16 reported an increase in internal fiber shortening using M-mode echocardiography following burn injury. More recently, Papp et al 17 published a transesophageal echocardiogram (TEE) study evaluating systolic and diastolic performance subsequent to thermal injury and found that cardiac function was not depressed.
Perioperative cardiac dysfunction can greatly impact management. Clinical quantification of cardiac function in perioperative burn patients is difficult and often indeterminate. The goals of this study were to define cardiac function using TEE after large burn injuries and determine the impact on clinical outcome.
Methods
Systolic and diastolic function was assessed using TEE in children age 2-18 years (mean 9.7 ± 0.9 yrs) with ≥35% TBSA burn admitted to the Shriner’s Hospital at Galveston. For this Institutional Review Board (IRB) approved cohort, TEE data was collected and compared to length of stay and other variables. The data collection period was from 2004 through 2007. TEE was performed as part of clinical care during the initial intensive care unit (ICU) period. Specific indications/inclusions included: patients requiring inotropic and/or pressor support after the first 24hr following burn injury, enlarged cardiac silhouette on chest X-ray, significant pulmonary edema on chest x-ray or increased extravascular lung water measured by transpulmonary thermodilution, unexplained hypotension or suspicion of endocarditis. TEE data was obtained in 40 patients. Patients with a history of esophageal or upper gastrointestinal (GI) disease, or severe coagulopathy were excluded. Outcome data was also excluded due to death (5), cardiac arrest (1), inability to obtain a complete set of clinical data from medical record (7) or electrical burn (1). After these exclusions, echocardiographic parameters of cardiac function and outcome variables were obtained in 26 patients.
An experienced cardiothoracic anesthesiologist, with perioperative echocardiography board certification, performed the TEE exam. A Vivid 7 ultrasound (GE Medical System, Milwaukee, WI) system with a 6T or 9T probe was used, depending on the size of the patient. The TEE exams took place either in the ICU, at bedside, or in the operating room, on OR table, prior to surgical incision. General endotracheal anesthesia using ketamine (3-5 mg/kg) and propofol (0.5-1 mg/kg) was administered to secure the airway and facilitate insertion and manipulation of the TEE probe. Patients were mechanically ventilated and hemodynamically stable during TEE exam. TEE exams were accomplished in 10-15 min, well tolerated and without complications. Systolic function was evaluated by 2D echocardiography using a left ventricular (LV) long axis view at 60-90 degrees. End diastolic and end systolic areas were traced and end diastolic volumes (EDV) and end systolic volumes (ESV) were calculated using modified Simpson’s rule from representative recordings over 3-5 cardiac cycles. Ejection Fraction% (EF%) was determined as: EF%= (EDV-ESV)/EDV. Evaluation of diastolic function was accomplished using Doppler echocardiography and tissue Doppler imaging. Similarly, diastolic parameters were obtained from representative recordings over 3-5 cardiac cycles. The pulsed Doppler sample volume was placed at the tips of the mitral valve. The peak mitral inflow velocities (E and A waves) were recorded. Tissue Doppler was performed from the lateral aspect of the mitral annulus. From this data, early (e’) diastolic velocity was obtained. Ventricular compliance was assessed by using the ratio of transmitral E velocity to e’ ratio, as E/e’. This ratio has been shown to correlate as an index of filling pressures and is a preload-independent index of LV relaxation 18.
Patient demographics (age, gender, and %TBSA) and outcome variables (length of stay in ICU, number of surgeries, presence of inhalation injury, number of ventilator days, serum creatinine, and amount of pharmacologic cardiac support) were recorded. All recorded variables were compared to TEE findings of systolic and diastolic function. The length of ICU stay was determined by using chart review, from admission date until discharge from the unit. In the case of multiple admits, the total days on unit from each admission to the burn ICU were added together and described collectively as length of stay (LOS). The number of surgeries for each patient was obtained from nursing transport notes and confirmed by the operative anesthesia record. Ventilator days were assessed from respiratory flow sheets that were completed for each patient every day. Renal function was evaluated by serum creatinine. The values for creatinine measurements were collected via chart review. Labs were drawn on patients while they were in the ICU and serum creatinine was measured in the Shriners Hospital for Children Galveston laboratory. All creatinine values reported were drawn within 24 hours of the echocardiography exam. The use of pharmacologic cardiovascular support (pressors or inotropes) at the time of echocardiography exam was recorded from the nursing notes and physician orders. Pharmacologic agents included dobutamine, dopamine, and epinephrine. The dose of each agent was also recorded. Inhalation injury was determined by chart review, specifically by the attending anesthesiologist interpretation of the bronchoscopy performed upon admission to the burn ICU. Time until arrival at advanced burn center was measured in days from date of burn injury to date of arrival at the burn center.
Data and Statistics
The patients were separated according to their systolic function (EF% of >50% and EF% of ≤50%) and compared by number of surgeries, ventilator days, pharmacologic cardiac support and overall length of ICU stay. We defined systolic dysfunction as an EF% ≤50% and normal as an EF% >50%. The cut-point for the EF% determination was based on defined standards for TEE impact used for perioperative echocardiography in cardiac surgery. The two groups were compared to outcome variables using a non-paired Student’s t test. Data are expressed as mean ± SEM. A p value of less than 0.05 was considered statistically significant.
Results
In our cohort, systolic dysfunction (EF% ≤ 50%) was observed in 16/26 patients or 62% and preserved systolic function (EF>50%) was observed in 10/26 or 38%. More males than females were studied. There were no significant differences in gender between the two systolic function groups. Mean age between the two groups did not differ significantly with 10.0 ± 1.3 years old for EF% ≤ 50% and 9.6 ± 1.2 years old for EF>50%. There were no temporal distribution differences, which is that children in who received evaluation in 2004 had no worse chance of having impaired systolic function than those examined in 2007. Finally, the TBSA% burn in the preserved EF and reduced EF groups were 59.0 ± 4.6 and 67.2 ± 4.0 respectfully. This difference did not reach statistical significance(Table 1).
Table 1.
Ejection Fraction (EF%) – preserved systolic function (EF%>50%) versus systolic dysfunction (EF%≤ 50%) and outcome variables
| EF < 50% | EF ≤ 50% | |
|---|---|---|
| AGEyrs | 10.0±1.3 | 9.6±1.2 |
| TBSA% | 59.0±4.6 | 67.2±4.0 |
| ICU LOSdays | 34.3±3.3 | 62.1±7.2* |
| Surgerynumber of | 5.1±0.7 | 8.7±1.2* |
| Mechanical Ventilationdays | 5.8±1.5 | 15±3.3* |
| Serum Creatininemg/dL | 0.86±0.06 | 1.24±0.19 |
| Pharmacologic Support% | 6/10 (60%) | 8/16 (50%) |
| Inhalation Injury% | 4/10 (40%) | 7/16 (44%) |
Data are expressed as mean ± SEM. Systolic Function versus age, total burn surface area (%TBSA), length of stay (LOS) in ICU, number of surgeries, ventilation days, renal function (serum creatinine), pharmacologic cardiovascular support and inhalation injury.
(p <0.05)
Number of Surgeries
There was an inverse relationship between ejection fraction and number of surgeries. The preserved systolic function group had 5.1 ± 0.7 surgeries, while systolic dysfunction group had 8.7 ± 1.2 surgeries. This was significantly different, (p = 0. 03).
Number of Ventilator Days
The number of ventilator days was significantly different based on systolic function, (p = 0. 03). The number of ventilator days in the preserved systolic function group was 5.8 ± 1.5, whereas, the systolic dysfunction group was 15.1 ± 3.3.
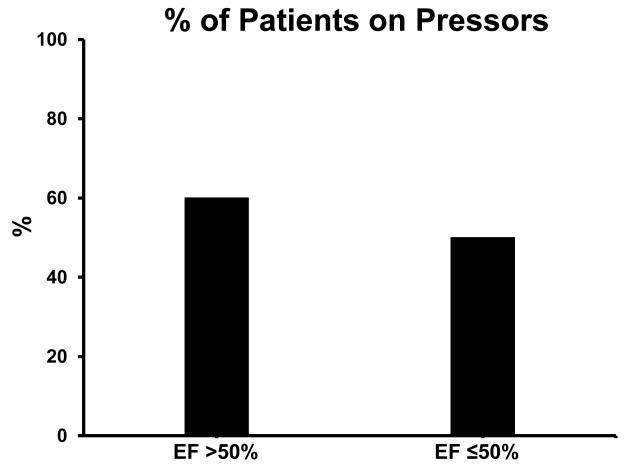
Elevated Creatinine
None of the patients with preserved systolic function had evidence of significant renal dysfunction (defined as creatinine greater than 1.5 mg/dL). In patients with systolic dysfunction, 38% had a Cr >1.5 mg/dL. There was a trend (p =0.08) for a lower creatinine in the preserved systolic group versus systolic dysfunction group, 0.86 mg/dL ± 0.06 vs. 1.24 mg/dL ± 0.19, respectively (Figure 1).
Figure 1.
Creatinine versus systolic function in children with ≥35% total burn surface area. Just over one third of patients with systolic dysfunction (EF ≤50%, n=16) showed elevated creatinine levels compared to none in the preserved function group (EF >50%, n=10).
Inhalation Injury
The presence of inhalation injury was similar for preserved systolic function and systolic dysfunction groups 40% and 44%, respectively, had evidence of inhalation injury.
Arrival Time and admission to Shriner’s Hospital Galveston
There was a difference, albeit not statistically significant (p = 0.07), between the two systolic groups in terms of how many days it took to arrive at our burn center. The arrival time to our facility was 2 ± 0.6 and 5 ± 1.5 days for preserved systolic function and systolic dysfunction group, respectively.
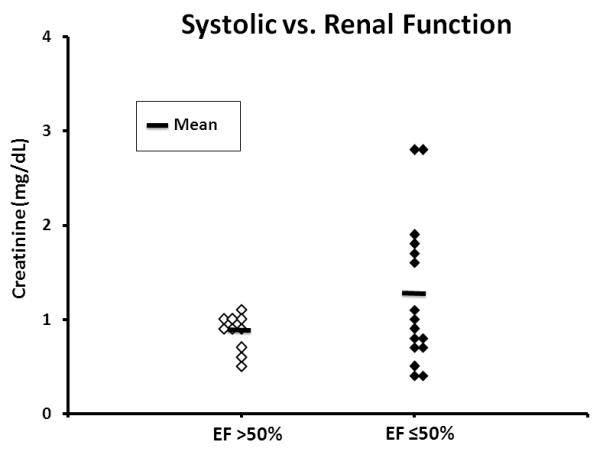
Pharmacologic Cardiovascular Support
Pharmacologic cardiovascular support was recorded if the patient was being administered the drug at the time of the TEE exam. In this cohort, 14/26 patients were receiving intravenous pharmacologic cardiovascular support (12 - dobutamine, 1 - dobutamine and dopamine, and 1 – epinephrine). Surprisingly, the administration of cardiovascular supportive agents was independent of systolic function. Specifically, 6/10 patients with preserved systolic function and 8/16 patients in the systolic dysfunction group received pharmacologic support (Figure 2).
Figure 2.
Systolic function and pressor support during echocardiography of children with ≥35% total burn surface area. Use of cardiovascular supportive agents was independent of systolic function for both preserved (EF >50%) and dysfunctional (EF ≤50%) systolic function groups.
Length of Stay in the ICU
The systolic dysfunction group had a significantly prolonged ICU stay (p <0.01). In patients with systolic dysfunction, the length of ICU stay was 62.1 ± 7.2 days versus 34.3 ± 3.3 days for patients with preserved ejection fraction. (Figure 3)
Figure 3.
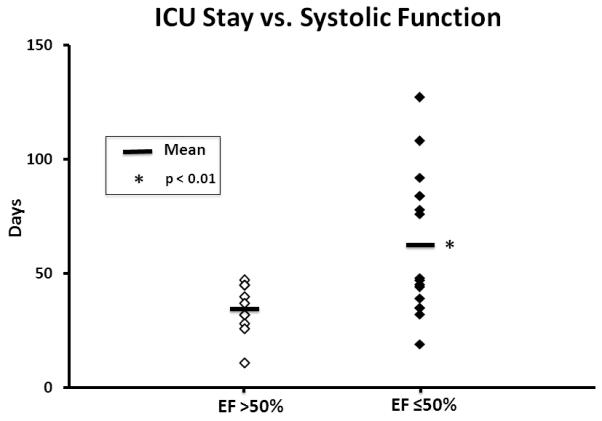
Intensive care unit length of stay (LOS) according to systolic function. LOS was significantly greater for the depressed systolic function group (p <0.05) compared to the preserved group.
Diastolic Function
Diastolic measurements were obtained in 65% of the cohort. Normal diastolic function was defined as an E/e’ ratio of < 8. In 88% of the studied population, we observed varying degrees of diastolic dysfunction, as evidenced by an E/e’ ratio > 8. However, there was no statistically significant difference in clinical outcomes between patients with normal diastolic parameters and those with diastolic dysfunction.
Discussion
This study looked at a cohort of 26 children in which TEE data on systolic function was compared to outcome variables during their perioperative ICU stay. To our knowledge this is the first study to evaluate the clinical sequelae of cardiac dysfunction in burned children during the perioperative period. The TEE was performed in the operating room, prior to surgical incision, or in the patient’s ICU room. We found that a significant number of children with large TBSA burns had reduced systolic function, defined as an ejection fraction less than or equal to 50%. Further, systolic dysfunction was associated with approximately a two-fold increase in ICU stay. Additionally, systolic dysfunction, following burn injury, was associated with increased number of days on ventilation support, creatinine and number of surgeries. Interestingly, very few patients in this cohort had normal diastolic parameters, defined as an E/e’ ratio of < 8. However, diastolic dysfunction was not significantly associated with length of stay or any of the other clinical parameters. This finding is interesting and difficult to explain. It may be that diastolic dysfunction is a transient finding.
Mechanisms for cardiac dysfunction following burn injury have been extensively reported. It has been shown that thermal injury produces myocardial depression. It is known that circulating inflammatory cytokines (TNF-alpha, IL-beta, IL-6) 4, macrophage inhibitory factor 5, and oxygen free radicals 6-8 are systemically released following burn injury and contribute to myocardial depression. The specific site or origin of these mediators appears to be multifocal. Ferrara et al 9 showed that lymph isolated from the burned hind limb of dogs had high levels of inflammatory mediators and resulted in poorer regional myocardial blood flow and contractile performance. Sambol et al 10 showed that the mediators of cardiac depression are derived from the gut by diverting lymph drainage from the mesentery of burned animals, which prevented burn-related myocardial contractile depression. Subsequent studies have also implicated sodium and calcium loading in the cardiac myocyte as a possible mechanism for the burn induced cardiac dysfunction 11-12.
In addition, it is widely known that sepsis can cause reversible myocardial depression 19-22. The cardiac manifestations of sepsis can include decreased contractility, impaired ventricular response to fluid therapy and, on occasion, ventricular dilatation 20. The proposed mechanisms behind sepsis induced cardiac dysfunction are multi-factorial and include the presence of circulating depressant factors, such as cytokines (TNF-alpha, IL-beta), lysozyme c, endothelin 1, nitric oxide dependent factors and possibly mitochondrial dysfunction and apoptosis 19-22. Studies have also found that in burns, sepsis serves as an additive factor to the cardiac dysfunction already presents in burns 23-24. We did not exclude patients with sepsis in our cohort and acknowledge that this disease process may be present.
Our findings suggest that a large percentage of pediatric burns patients suffer from cardiac dysfunction. This directly counters the results of others that have previously demonstrated a lack of myocardial depression following burn injury 16-17. These differences may be accounted for by the various methodologies used to assess left ventricular performance, or they may represent differences in the timing chosen to assess cardiac performance. For example, we used quantifiable 2D image acquisition and volumetric calculation to determine ejection fraction. Previous investigators had used M-mode echocardiography and fractional area shortening. These methods are known to overestimate ejection fraction if the views are foreshortened 25, 17. Furthermore, we did not perform TEE in the first 24 hrs when loading conditions are rarely optimized and often results in hyperdynamic ventricular motion.
This study also addresses the utility of TEE in burned children. It is well established that TEE provides detailed information about cardiac structure and function in patients. Again, our results suggest a high prevalence of cardiac dysfunction in this population. Furthermore, we have demonstrated that a reduced EF is correlated with poorer clinical outcomes. The potential drawback that TEE requires sedation is overcome by the fact that burned patients are commonly undergoing procedures with general anesthesia. The addition of a perioperative TEE is therefore seamless and provides abundant clinically relevant information in these medically complex patients. It is our opinion that transesophageal echocardiography or at least transthoracic echocardiography should be routine practice in the burn ICU.
It remains to be seen whether the clinical consequences of cardiac dysfunction seen in this study could be ameliorated by treatment. This will require future investigation.
Limitations
Although we report a compelling association between systolic function and length of ICU stay, this study has several limitations. The cardiac depression described in our study may not be solely due to burn-induced myocardial dysfunction. TEE exams were not performed at a specified point during the ICU stay. Rather, these exams were performed to evaluate a clinical question e.g., unexplained hypotension or perfusion, pulmonary edema or suspicion of endocarditis. This resulted in the examinations being completed at variable times in a critically ill patients’ acute course. Cardiac dysfunction is known to occur in sepsis but the clinical definition of sepsis following burn injury is controversial and difficult to define. We acknowledge that cardiac dysfunction may be multifactorial in etiology with the common factor of burn-induced myocardial dysfunction and varying contributions of sepsis-induced dysfunction or other drivers of cardiac depression. The quality of acute fluid resuscitation in patients with large burn injury could also contribute to cardiac performance at time of the TEE. Many of the patients in this study were transferred to our facility from an outside hospital and the exact parameters of their fluid resuscitation are unknown. There was a difference in the time until arrival between the two groups, with the depressed systolic function group being longer. This difference, however, was not significantly different. Delays in resuscitation could in part account for reduced systolic function. It should also be noted that although there were similar numbers of vasoactive drug used in each systolic groups, we couldn’t distinguish the extent of or the varying degrees of resuscitation efforts. Lactate and base excess values were not obtained and are a limitation. Unfortunately ventricular wall thickness was not measured in this cohort. In general, ventricular wall thickness is lower in children than adults.26 We cannot exclude that preexisting or acquired abnormalities of the myocardium could have been contributory to cardiac dysfunction.
The children who received echocardiography during their stay in the burn ICU were those who had clinical indications for the exam. It should be noted that within this sample there is a possibility for bias due to children who met the clinical criteria for requiring echocardiography but did not receive the exam.
There was a significant difference in the number of surgeries and ventilator days for the impaired vs. preserved systolic function group. The number surgeries could be a confounding variable for number of ventilator days. The increase in the number of surgeries in the systolic dysfunction group could also be confounded by other ICU variables. Our data did not extract the detail for the rationale for surgeries. Thus, we cannot ascertain if the surgeries were due to graft loss from hypoperfusion, infection or other variables. The data obtained was not blinded and could have influenced decisions made in the care of these children especially in the perioperative period. Unfortunately we cannot say to what extent the information influenced the care. Future studies will incorporate these measurements in order to stratify patients based on cardiac function. Specifically, we hope to determine if optimizing cardiac function can improve outcomes and decrease resource utilization.
While our study does show differences in kidney function between the two systolic groups, it is not known if patients in either group developed acute kidney injury. The creatinine measurements are only a snapshot in time and thus a limitation.
The insertion of the TEE probe requires sedation or general anesthesia. Most of our exams were performed following induction of anesthesia but prior to surgical incision. It is recognized that some general anesthetic agents depress myocardial contractility and that general anesthesia could be a confounding variable or a contributing factor for these observations. The same anesthetic regimen (admixure of ketamine-propofol ) was used for all TEE exams. Ketamine, which is the standard of care anesthetic at our institution for perioperative burn surgery, preserves or even increases cardiac function compared to other general anesthetic agents. However, in patients with decompensated heart failure or catecholamine depleted states, myocardial depression after ketamine administration has been reported A relatively low dose of ketamine and propofol was used to facilitate the TEE exam. Larger doses of these agents were used for surgery (after TEE exam). Our clinical observations did not suggest significant cardiovascular effects after GETA or during the TEE exam. Specifically, blood pressure, heart rate and cardiac output (in patients with a continuous cardiac output device) remained unchanged. To some extent, the prevalence of cardiac dysfunction is likely to have been underestimated in our cohort due to the high number of patients on inotropic support. Table 1 shows that over 50% of the patients in this cohort were receiving pharmacologic cardiovascular support. One would anticipate that these agents should inflate the true ejection fraction as well improve diastolic parameters. Finally, We did not capture data on the time course of systolic function. Data presented in this cohort was based on a single TEE performed during the patient’s acute stay in the burn ICU. A future focus will utilize serial echocardiograms to better delineate the onset and persistence of cardiac dysfunction in perioperative burn patients. Future studies using serial echocardiograms, biomarkers, and stratification and therapeutic strategies are needed to address this. It is our hope that this study will spur future clinical investigation regarding cardiac dysfunction in perioperative burns patients.
Acknowledgments
Funding Provided By: This study was funded in part by NIH 1R01HL092253-01
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Adams HR, Baxter CR, Parker JL. Contractile function of heart muscle from burned guinea pigs. Circ Shock. 1982;9:63–73. [PubMed] [Google Scholar]
- 2.Adams HR, Baxter CR, Izenberg SD. Decreased contractility and compliance of the left ventricle as complications of thermal trauma. Am Heart J. 1984;108:1477–1487. doi: 10.1016/0002-8703(84)90695-1. [DOI] [PubMed] [Google Scholar]
- 3.Adams HR, Baxter CR, Parker JL, et al. Development of acute burn shock in unresuscitated guinea pigs. Circ Shock. 1981;8(6):613–625. [PubMed] [Google Scholar]
- 4.Maass DL, Hybki Peters D, White J, et al. The time course of cardiac NF-KB activation and TNF-alpha secretion by cardiac myocytes after burn injury: contribution to burn-related cardiac contractile dysfunction. Shock. 2002;17:293–299. doi: 10.1097/00024382-200204000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Garner LB, Willis MS, Carlson DL, et al. Macrophage migration inhibitory factor is a cardiac-derived myocardial depressant factor. Am J Physiol. 2003;285:2500–2509. doi: 10.1152/ajpheart.00432.2003. [DOI] [PubMed] [Google Scholar]
- 6.Horton JW, White DJ. Role of xanthine oxidase and leukocytes in postburn cardiac dysfunction. J Am Coll Surg. 1995;181:129–137. [PubMed] [Google Scholar]
- 7.Horton JW, White DJ. Free radical scavengers prevent ischemia-reperfusion-mediated cardiac dysfunction. J Surg Res. 1993;55:282–89. doi: 10.1006/jsre.1993.1141. [DOI] [PubMed] [Google Scholar]
- 8.Horton JW, Mileski WJ, White DJ, et al. Monoclonal antibody to intercellular adhesion molecule-1 reduces cardiac contractile dysfunction after burn injury in rabbits. J Surg Res. 1996;64:49–56. doi: 10.1006/jsre.1996.0305. [DOI] [PubMed] [Google Scholar]
- 9.Ferrara JJ, Frankin EW, Kukuy EL, et al. Lymph isolated from a regional scald injury produces a negative inotropic effect in dogs. J Burn Care Rehabil. 1998;19:296–304. doi: 10.1097/00004630-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Sambol JT, White J, Horton JW, et al. Burn induced impairment of cardiac contractile function due to gut derived myocardial depressant factors. Shock. 2002;18:272–276. doi: 10.1097/00024382-200209000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Ballard-Croft C, Carlson D, Maass DL, et al. Burn trauma alters calcium transporter protein expression in the heart. J Appl Physiol. 2004;97:1470–1476. doi: 10.1152/japplphysiol.01149.2003. [DOI] [PubMed] [Google Scholar]
- 12.Maass DL, White DJ, Sanders B, et al. Cardiac Myocyte Accumulation of Calcium in Burn Injury: Cause or Effect of Myocardial Contractile Dysfunction. Journal of Burn Care and Rehab. 2005;26(3):252–259. [PubMed] [Google Scholar]
- 13.Reynolds EM, Ryan DP, Sheridan RL, et al. Left Ventricular Failure Complicating Severe Pediatric Burn Injuries. Journal of Pediatric Surgery. 1995;30:264–70. doi: 10.1016/0022-3468(95)90572-3. [DOI] [PubMed] [Google Scholar]
- 14.Minifee PK, Barrow RE, Abston S, et al. Improved myocardial oxygen utilization following propranolol infusion in adolescents with postburn hypermetabolism. J Pedri Surg. 1989;24:806–811. doi: 10.1016/s0022-3468(89)80541-x. [DOI] [PubMed] [Google Scholar]
- 15.Murphy JT, Horton JW, Purdue GF, et al. Evaluation of Troponin-I as an Indicator of Cardiac Dysfunction after Thermal Injury. Journal of Trauma. 1998;45:700–4. doi: 10.1097/00005373-199810000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Goodwin CW, Dorethy J, Lam V, et al. Randomized Trial of Efficacy of Crystalloid and Colloid Resuscitation on Hemodynamic Response and Lung Water Following Thermal Injury. Ann Surg. 1983;197:520–31. doi: 10.1097/00000658-198305000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Papp A, Uusaro I, Hartikainen J, et al. Myocardial function and haemodynamics in extensive burn trauma: evaluation by clinical signs, invasive monitoring, echocardiography and cytokine concentrations. A prospective clinical study. Acta Anesthesiologica Scandinavica. 2003;47:1257–63. doi: 10.1046/j.1399-6576.2003.00235.x. [DOI] [PubMed] [Google Scholar]
- 18.Nagueh SF, Middleton KJ, Kopelen HA, et al. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30:1527. doi: 10.1016/s0735-1097(97)00344-6. [DOI] [PubMed] [Google Scholar]
- 19.Parker MM. Pathophysiology of cardiovascular dysfunction in septic shock. New Horiz. 1998;6(2):130–138. [PubMed] [Google Scholar]
- 20.Court O, Kumar A, Parrillo JE, et al. Clinical review: Myocardial depression in sepsis and septic shock. Crit Care. 2002;6(6):500–508. doi: 10.1186/cc1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zanotti-Cavazzoni SL, Hollenberg SM. Cardiac dysfunction in severe sepsis and septic shock. Curr Opin Crit Care. 2009;15(5):392–397. doi: 10.1097/MCC.0b013e3283307a4e. [DOI] [PubMed] [Google Scholar]
- 22.Rudiger A, Singer M. Mechanisms of sepsis induced cardiac dysfunction. Crit Care Med. 2007;35(6):1599–1608. doi: 10.1097/01.CCM.0000266683.64081.02. [DOI] [PubMed] [Google Scholar]
- 23.Horton JW. A Model of Myocardial Inflammation and Dysfunction in Burn Complicated by Sepsis. Shock. 2007;28(3):326–333. doi: 10.1097/01.shk.0000238064.54332.c8. [DOI] [PubMed] [Google Scholar]
- 24.Horton JW, Maass DL, White J, et al. Myocardial Inflammatory responses to Sepsis Complicated by Previous Burn Injury. Surgical Infections. 2003;4(4):363–377. doi: 10.1089/109629603322761427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lang RM, Bierig M, Devereux RB, et al. Recommendations for Chamber Quantification: A Report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Kampmann C, Wiethoff CM, Wenzel A, et al. Normal values of M mode echocardiographic measurements of more than 2000 healthy infants and children in central Europe. Heart. 2000;83:667–672. doi: 10.1136/heart.83.6.667. [DOI] [PMC free article] [PubMed] [Google Scholar]