Abstract
Objective
To describe trends in hysterectomy route at a large tertiary center
Study Design
We reviewed all hysterectomies performed at Magee-Womens Hospital from 2000–2010. This database was chosen over larger national surveys as it has been tracking laparoscopic procedures since 2000, well before laparoscopic hysterectomy ICD-9 codes were developed.
Results
There were 13,973 patients included who underwent hysterectomy at Magee-Womens Hospital. In 2000, 3.3% were laparoscopic (LH), 74.5% abdominal (AH), and 22.2% vaginal (VH). By 2010, LH represented 43.5%, AH 36.3%, VH 17.2%, and 3.0% laparoscopic converted to open (LH→AH). Hysterectomies performed for gynecologic malignancy represented 24.4% of cases. The average length of stay for benign LH and VH, 1.0±1.0 and 1.6±1.0 days respectively, was significantly shorter than the average 3.1±2.3 day stay associated with AH (p<.001). Average patient age was 46.9±10.9 for LH, 51.5±12.1 for AH, and 51.7±14.1 for VH, and over the study period there was a significant trend of increasing patient age b1=0.517, 0.583, and 0.513 respectively (p<.001 for all).
Conclusions
The percentage of LH increased over the last decade, and by 2010 had surpassed AH. The 43.4% LH rate in 2010 is much higher than previously reported in national surveys. This is likely due to an increase in the number of laparoscopic procedures being performed over the last few years as well as the ability of our study to capture LH prior to development of appropriate ICD-9 codes. Our unique ability to determine hysterectomy route, which predates appropriate coding, may provide a more accurate characterization of hysterectomy trends.
Keywords: hysterectomy, surgical trends
Introduction
Approximately 494,000 hysterectomies are performed annually in the United States, making this procedure one of the most commonly performed in women of reproductive age (1). Over the last three decades, technological advances in surgical equipment and training have allowed for minimally invasive approaches to hysterectomy. The first case of laparoscopic-assisted hysterectomy was published by Reich and colleagues in 1989 (2). Since that time, practice patterns have changed as laparoscopic approaches to hysterectomy have increased throughout the world.
Laparoscopic and vaginal approaches to hysterectomy are preferred to abdominal approaches as they result in shorter hospital stays, faster return to normal activities, and fewer infections. Laparoscopic assisted vaginal, total laparoscopic, and robotically assisted laparoscopic hysterectomies are being performed more commonly as surgeons become trained with the necessary surgical skills and as the technology becomes more widely accessible. Laparoscopic hysterectomy has been associated with a higher risk of urinary tract injury compared to abdominal and vaginal procedures and the risks of these minimally invasive approaches must be balanced with the benefits (3).
Over the last 20 years, the proportion of laparoscopically performed hysterectomies has increased, while abdominal hysterectomies have decreased. The reported rate of laparoscopic hysterectomy in 1990 was only 0.3% while abdominal and vaginal approaches represented 73.6% and 24.4% of cases, respectively (4). In the 2005 Nationwide Inpatient Sample, 14% of hysterectomies were laparoscopic, 64% abdominal, and 22% vaginal (5). This data, however, is limited by the fact that the code for total laparoscopic hysterectomy was not in use until 2006.
Although laparoscopic hysterectomies have been performed for many years, ICD-9 procedure codes have only recently become available (Table 1). Coding for laparoscopic-assisted vaginal hysterectomy has been available since 1996, whereas the code for total laparoscopic hysterectomy was not developed until 2006 (6). Prior studies have described trends in gynecologic surgical procedures using large databases, such as the National Hospital Discharge Survey or the Nationwide Inpatient Sample; however, these databases provide limited information on surgical approach to hysterectomy since many of the laparoscopic codes were not yet developed.
Table 1.
Year of Laparoscopic ICD-9 Code Introduction
| Code | Procedure | Effective Datea | Previous Code |
|---|---|---|---|
| 68.31 | Laparoscopic supracervical hysterectomy | 2003 | 68.3 |
| 68.39 | Subtotal abdominal hysterectomy | 2003 | 68.3 |
| 68.41 | Laparoscopic total abdominal hysterectomy | 2006 | 68.4 |
| 68.49 | Total abdominal hysterectomy | 2006 | 68.4 |
| 68.51 | Laparoscopically assisted vaginal hysterectomy | 1996 | 68.5 |
| 68.59 | Total vaginal hysterectomy | 1996 | 68.5 |
| 68.61 | Laparoscopic radical abdominal hysterectomy | 2006 | 68.6 |
| 68.69 | Modified radical abdominal hysterectomy | 2006 | 68.6 |
| 68.71 | Laparoscopic radical vaginal hysterectomy | 2006 | 68.7 |
| 68.79 | Radical vaginal hysterectomy | 2006 | 68.7 |
| 17.42 | Robotic assisted procedure | 2008 | none |
| V64.41 | Laparoscopic procedure converted to open | 2004 | none |
ICD, International Classification of Diseases
Effective date as of 10/1 of that year
Magee-Womens Hospital, a tertiary care hospital with a combination of academic and private gynecologists and an active minimally invasive gynecologic surgery division, had been tracking laparoscopic procedures via intraoperative reports prior to the development of ICD-9 codes for laparoscopic procedures. Given the availability of this information in our institution’s database, the aim of this study was to assess changes in hysterectomy route over time and identify differences in characteristics of patients undergoing laparoscopic hysterectomy compared to abdominal or vaginal routes.
Materials and Methods
De-identified data was obtained from the University of Pittsburgh Medical Center Magee-Womens Hospital coding department for years 2000–2010. All women with an ICD-9 procedure code indicating that a hysterectomy was performed during a hospital admission were included in this study. Additional data and associated information including patient date of birth, race, marital status, insurance type, date of admission and discharge, discharge diagnoses, and concomitant procedures were collected. Because this database did not contain personal identifiers, this analysis was considered exempt by the University of Pittsburgh Institutional Review Board.
Exclusion criteria included missing data and hysterectomy associated with either cesarean delivery or pelvic exenteration since both can only be performed with abdominal approaches. Using pregnancy-specific V27 ICD-9 codes, 118 hysterectomies performed at the time of delivery were excluded from the dataset. Pelvic exenteration (ICD-9 code 68.8) was not included in the initial hysterectomy data obtained from the coding department. Sixteen patients lacked laparoscopic hospital coding data and had 3-digit ICD-9 codes making determination of the route of hysterectomy impossible and were thus excluded.
The initial sample included 14,107 women. After excluding those with unidentifiable hysterectomy routes and those undergoing cesarean hysterectomy or exenteration, the total number of women in the study was 13,973 (Figure 1). Subjects with code v64.41 (154 patients), indicating that a procedure was converted from laparoscopic to open, were analyzed separately. ICD-9 codes for hysterectomy have changed over time from three digit codes to four digit codes, with those ending in "1" indicating laparoscopic procedures and those ending in "9" indicating open or vaginal procedures. When four digit laparoscopic ICD-9 codes were available, these were used to categorize hysterectomies as laparoscopic, open or vaginal and were used to confirm Magee-Womens Hospital (MWH) laparoscopic coding records. In our study period, many of the procedures were performed prior to the development of laparoscopic ICD-9 codes. When only three digit codes were available, the route of hysterectomy was differentiated by the MWH laparoscopic code (5,409 subjects). The four digit ICD-9 code was used to identify hysterectomy route for 8,264 patients. There were 146 subjects with discrepancies between the four digit ICD-9 codes and the MWH laparoscopic codes. Figure 1 demonstrates how these discrepant codes were analyzed.
Figure 1. Study Flowchart.
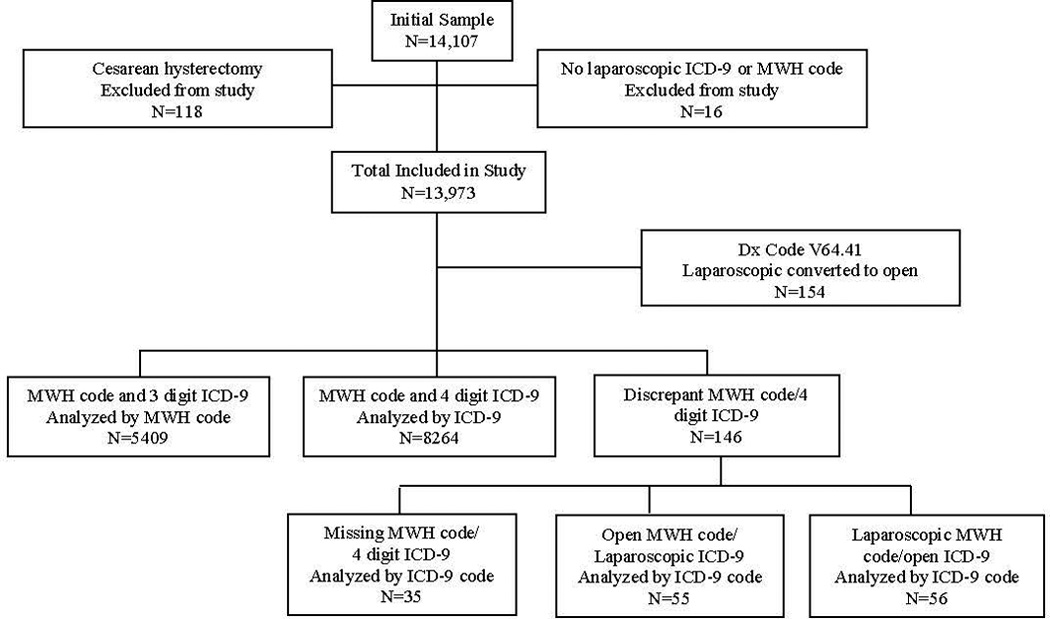
Hysterectomy group assignment by MWH and ICD-9 codes MWH code, Magee Womens Hospital institutional code ICD-9; International Classification of Diseases, 9th Revision
Patients were categorized into four groups based upon ICD-9 and MWH procedure codes: abdominal (AH), vaginal (VH), laparoscopic (LH), and laparoscopic converted to abdominal (LH→AH). ICD-9 codes used were as follows: AH (68.39-subtotal abdominal hysterectomy, 68.49-total abdominal hysterectomy, 68.69-radical abdominal hysterectomy); VH (68.59-total vaginal hysterectomy, 68.79-radical vaginal hysterectomy); LH (68.31-laparoscopic supracervical hysterectomy, 68.41-total laparoscopic hysterectomy, 68.51-laparoscopic assisted vaginal hysterectomy, 68.61-laparoscopic radical hysterectomy, 68.71-laparoscopic radical vaginal hysterectomy); and LH→AH (v64.41-laparoscopic converted to open). Robotic hysterectomies were considered laparoscopic cases, and were not analyzed separately since Magee-Womens Hospital did not acquire a robot until late 2009. Subjects who sustained a bladder or ureteral injury at the time of surgery were identified by ICD-9 codes (Non-obstetric bladder injury: 57.81, 57.82, and 57.89; Ureteral injury: 56.74, 56.75, 56.79, 56.82–86, and 56.89).
The primary indication for the hysterectomy was considered to be the first diagnosis code. These ICD-9 codes were grouped into the following categories: dysfunctional uterine bleeding (626), dysmenorrhea (625.0, 625.3, 625.5), endometriosis (617), fibroids (218), gynecologic malignancy (179–184, 630, 233,621.3), pelvic organ prolapse/incontinence (618, 625.6, 788), and other. Procedures performed concomitantly at time of hysterectomy included anterior/posterior repair (70.5), colpopexy (70.77–78), cystoscopy (57.32), salpingo-oophorectomy – bilateral or unilateral (65), and urethral suspension including traditional pubovaginal and midurethral slings (59.4–5). Obesity diagnosis codes (278.00–02) were also analyzed.
Continuous variables were compared using Mann-Whitney U test or Kruskal-Wallis test. Variables with counts were compared using Chi-Square. Linear trends of rates, age and LOS during the study period were tested using Linear regression models. Outcomes with p<0.05 were considered significant. All analyses were conducted with SPSS (version 17).
Results
During 2000–2010, 13,973 women underwent hysterectomy at UPMC Magee-Womens Hospital that met our inclusion criteria. The demographics of this population are listed in Table 2. In 2000, 3.3% were LH, 74.5% AH, and 22.2% VH. By 2010, LH represented 43.5%, AH 36.3%, VH 17.2%, and LH→AH 3.0%. The majority of hysterectomies were performed for the primary diagnosis of fibroids (29.5%) followed by gynecologic cancer (24.4%) and pelvic organ prolapse (14.4%). Uterine fibroids were the most common diagnosis for hysterectomies performed laparoscopically (27.4%) whereas pelvic organ prolapse/incontinence was the most common indication for the vaginal approach (49.4%). Gynecologic malignancy and fibroids were the most common primary diagnoses for AH (32.5% and 32.8%, respectively). For procedures converted from laparoscopic to open, gynecologic malignancy was the most common primary diagnosis (37.7%).
Table 2.
Patient characteristics by hysterectomy route
| Laparoscopic | Open | Vaginal | Laparoscopic Converted to Open |
|
|---|---|---|---|---|
| n=2839 | n=8611 | n=2769 | n=154 | |
| Mean age ± SD | 46.9 ± 10.9 | 51.5 ± 12.1 | 51.7 ± 14.1 | 51.8 ± 10.6 |
| Race | ||||
| White | 86.6% | 82.4% | 85.7% | 83.1% |
| Black | 9.5% | 13.7% | 11.3% | 15.6% |
| Other | 1.6% | 1.0% | 0.7% | 1.3% |
| Marital Status | ||||
| Single | 18.8% | 20.9% | 13.5% | 24.7% |
| Married | 67.0% | 60.0% | 64.0% | 59.7% |
| Divorced | 8.6% | 8.3% | 9.9% | 6.5% |
| Other | 5.6% | 10.8% | 12.6% | 9.1% |
| Indication | ||||
| Benign, n (%) | 2316 (21.9) | 5541 (52.4) | 2615 (24.7) | 96 (0.9) |
| Malignancy, n (%) | 523 (15.4) | 2670 (78.4) | 154 (4.5) | 58 (1.7) |
SD, standard deviation
Since different factors are considered when planning the surgical route of hysterectomy for gynecologic malignancy and benign disease, separate trends were examined for these two diagnostic categories. For benign conditions (n=10,568) in the year 2000, 3.3% cases were LH, 69.7% AH, and 27% VH. By the year 2010, 46.2% of cases were LH, 28.6% AH, 23.1% VH, and 2.1% LH→AH (Figure 2). For gynecologic malignancy (n=3,405) in the year 2000, 3.4% cases were LH, 93.1% AH, and 3.4% VH. In the year 2010, 36.8% of cases were LH, 55.2% AH, 2.8% VH, and 5.1% LH→AH (Figure 3).
Figure 2. Hysterectomies for benign indications.
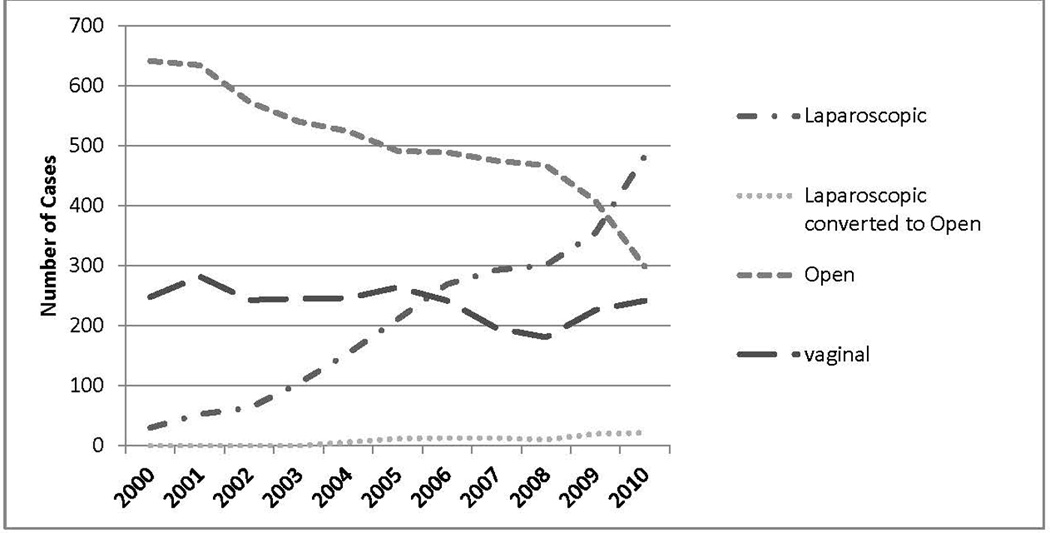
Hysterectomies performed for benign indications 2000–2010, stratified by route
Figure 3. Hysterectomies for gynecologic malignancy.
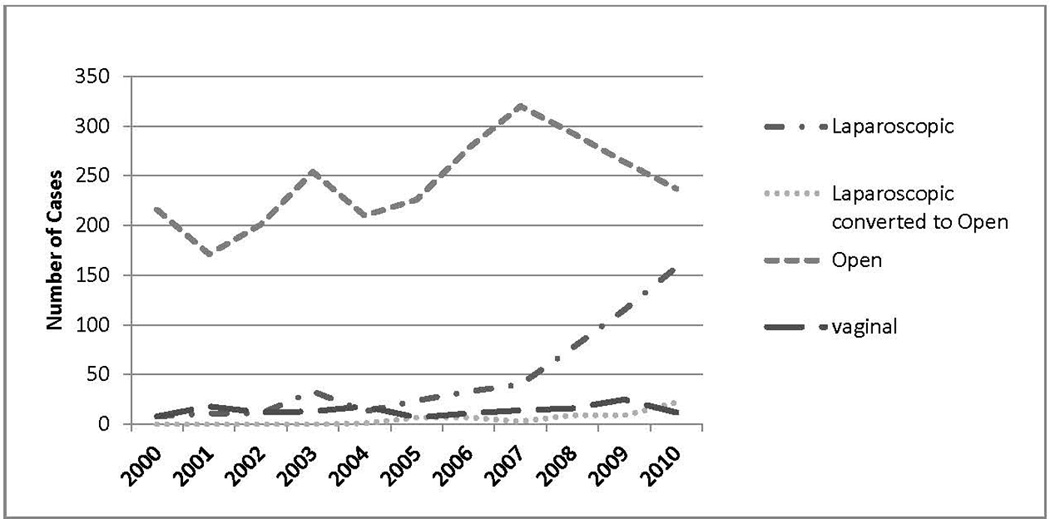
Hysterectomies performed for gynecologic malignancy 2000–2010, stratified by route
Additional procedures performed at time of hysterectomy include bilateral or unilateral salpingo-oophorectomy (63.3%), anterior/posterior repair (8.6%), colpopexy (6.9%), and urethral suspension (2.5%). Cystoscopy was performed at the time of hysterectomy in 21.2% of cases.
Of those patients undergoing hysterectomy for benign indications, 52.9% of women had a concomitant bilateral oophorectomy or removal of a remaining ovary (BO/RO). The percentage of hysterectomies with concomitant BO/RO decreased significantly throughout the study period (b= −0.007, p=0.033). The average age of women undergoing BO/RO was 51.3±10.5, with a significant trend of increasing age throughout the study period (b=0.425, p<0.001) (Figure 4).
Figure 4. Mean age of women undergoing castration at time of hysterectomy.
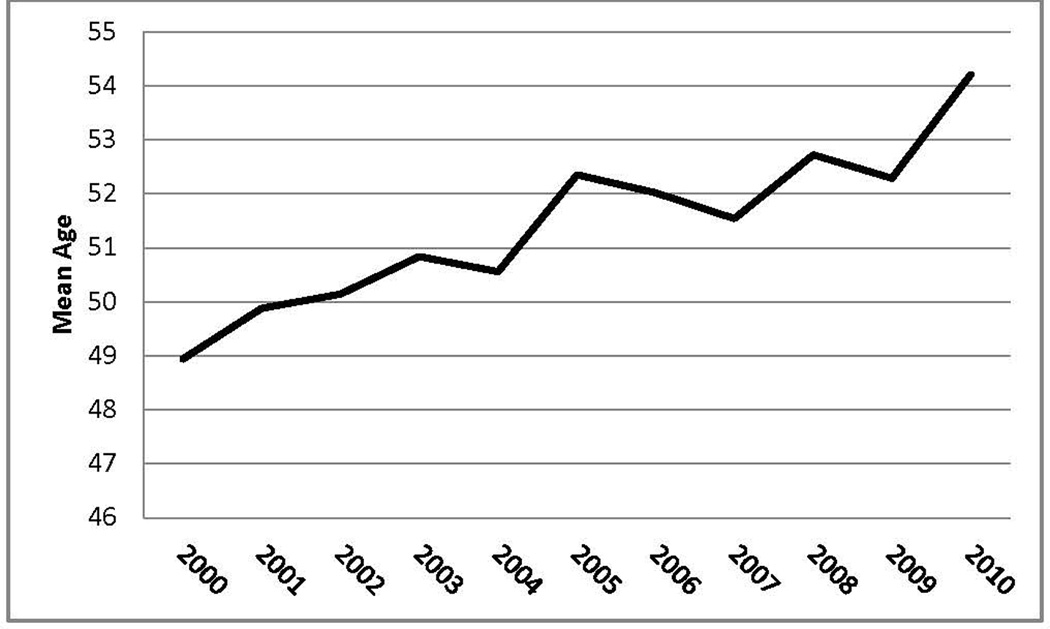
Mean age of women undergoing hysterectomy with concominant bilateral oophorectomy or removal of remaining oophorectomy 2000–2010. P < 0.001.
Between 2000–2010, there were 1569 patients (11.2%) with diagnosis codes indicating overweight or obese (855 obesity unspecified, 705 morbid obesity, and 9 overweight). On average, these patients were more likely to undergo AH (68.7%) compared to non-obese patients (57.5%). LH rates were similar (20.5% for non-obese and 18.8% for obese) while vaginal procedures were lower in obese women (10.1%) compared to non-obese (21.0%). The low percentage of overweight and obese patients in this study is likely due to inconsistent coding.
There were only 19 cases (0.1%) of ureteral injury in this series. Eighteen of these occurred in AH while one occurred in LH→AH. The primary diagnosis for hysterectomy in those cases where ureteral injuries occurred was gynecologic cancer (47.4%), fibroids (26.3%) and endometriosis (10.5%). Only 36.8% of cases where a ureteral injury occurred had concomitant cystoscopy. All ureteral injuries (100%) occurred during hysterectomies with bilateral or unilateral salpingo-oophorectomy. There were no ureteral injuries with concomitant colpopexy or anterior/posterior colporrhaphies. The number of bladder injuries was 196 (1.4%), with injuries occurring in 124 (1.5%) AH, 35 (1.2%) LH, 33 (1.2%) VH and 4 (2.5%) LH→AH. The primary diagnosis for hysterectomy in those cases with a bladder injury was fibroids (30.1%), gynecologic malignancy (23.0%), endometriosis (10.2%) and pelvic organ prolapse (9.7%). Only 44.4% of those cases with bladder injury had concomitant cystoscopy. When bladder injury occurred, the most common accompanying procedure was anterior/posterior repair (6.6%), colpopexy (3.6%), and urethral suspension (2.6%). In these cases the hysterectomy was 42.1% AH, 33% LH, 23.7% VH and 1.2% LH→AH. Our database did not allow us to determine whether the bladder injury occurred during the hysterectomy or during the concomitant procedure. There were no significant trends in bladder or ureteral injury rates over the study time period, despite the increasing proportion of laparoscopically performed hysterectomies.
The average length of stay (LOS) for women undergoing LH and VH for benign indications was 1.0±1.0 and 1.6±1.0 days respectively, which was significantly shorter than the average 3.1±2.3 day stay associated with AH (p<.001). In women with a diagnosis code of gynecologic malignancy, the average LOS for LH and VH was 1.1±1.1 and 1.6±1.3 days respectively, which was significantly shorter than the 4.6±3.3 day LOS associated with AH (p<0.001). From 2000–2010, there was a trend toward shorter LOS for LH (b1= −0.157, p<.001)) and VH (b1= −0.134, p<.001)). LOS remained constant for AH (3.85 days in 2000, 3.82 days in 2010, p=0.535).
The average age of patients undergoing hysterectomy was 46.9 ± 10.9 for LH, 51.3±12.1 for AH, and 51.7±14.1 for VH. There was no significant difference in average age of patients undergoing VH compared to AH; however, from 2003–2010 the average patient age was significantly younger in patients undergoing LH compared to VH (p<.026). Patients undergoing LH were significantly younger than those undergoing AH in all years except 2001 (p<.022). From 2000–2010, there was a significant trend of increasing patient age at time of hysterectomy: LH b1=0.517 (p<.001), AH b1=0.583 (p<.001), and VH b1=0.513 (p<.001).
Of the 13,973 patients undergoing hysterectomy during this time, 83.9% were Caucasian, 12.4% African American, and 3.7% unknown or other. According to United States Census data from 2010, the population of Pittsburgh, Pennsylvania is 66.0% Caucasian and 26.1% African American (7). This is relatively unchanged from 2000 data with 67.6% Caucasian and 27.1% African American (8). Therefore, a larger proportion of Caucasian women underwent hysterectomy during this time period than African American women. Additionally, Caucasian women were more likely than African American women to have a laparoscopic hysterectomy (21% vs 15.6%) or VH (20.2% vs 18.0%) and were less likely to undergo AH (57.7% vs 65.0%) and LH → AH (1.1% vs 1.4%). We were unable to determine how the type of insurance influenced route of hysterectomy as the codes for insurance types changed multiple times throughout the study period.
Comment
The percentage of hysterectomies performed laparoscopically has increased over the last decade and by the year 2010 surpassed the number of open hysterectomies performed at our tertiary care hospital. In addition, we found that the proportion of hysterectomies performed laparoscopically is much higher than previously reported in studies using national databases. This is likely due to the more accurate hospital-specific codes utilized at our institution, allowing identification of laparoscopic hysterectomies prior to appropriate ICD-9 codes being available. In a cross-sectional analysis of the 2003 Nationwide Inpatient Sample, Wu et al reported benign hysterectomy rates of 66.1% open, 21.8% vaginal and 11.8% laparoscopic (9). Similar results were demonstrated by Jacoby et al in a cross-sectional analysis of the 2005 Nationwide Inpatient Sample with rates of hysterectomy for benign disease reported as 64% open, 22% vaginal and 14% laparoscopic (5). Our tertiary center had a higher percentage of minimally-invasively performed hysterectomies in 2005 with 51.4% open, 27.0% vaginal, and 21.6% laparoscopic. The 43.4% laparoscopic hysterectomy rate found in our study in 2010 may represent a dramatic increase in laparoscopic hysterectomies over the last few years due to more providers receiving minimally-invasive training, and an increase in patient demand for laparoscopic surgery. This discrepancy in rates of laparoscopic hysterectomy compared to previously reported national data may also be explained by different physician practice patterns geographically or miscoding/under-coding of laparoscopic hysterectomies in national surveys using ICD-9 codes due to lack of appropriate codes in the recent past.
In this data series, the percentage of vaginal hysterectomies performed for benign disease decreased from 27.0% to 23.1% over the ten year period. This decrease in vaginal hysterectomies is consistent with data from the National Hospital Discharge Survey (10), as well as the Nationwide Inpatient Sample (4, 5, 9). The decrease in the proportion of vaginal hysterectomies is important as previous evidence suggests that vaginal hysterectomy, when feasible, is the approach of choice based upon its improved outcomes and lower complication rates (11). This decrease in vaginal hysterectomies may reflect changes in gynecologic resident surgical training with more emphasis on laparoscopy techniques and decreased surgeon comfort levels with performing hysterectomies via a vaginal route.
Throughout the study period, there was a significant trend of increasing age in women undergoing hysterectomy and concomitant BO/RO for benign disease and a significant decrease in the percentage of benign hysterectomies performed with BO/RO. Our regional findings are consistent with data presented from national databases (12). We speculate that these trends are due to the growing body of literature demonstrating the potential benefits of ovarian preservation.
The majority of hysterectomies in this study were performed for the primary indication of uterine fibroids, which is consistent with previous studies (9). Interestingly, uterine fibroids were also the primary diagnosis in the majority of hysterectomies that were converted from laparoscopic to open. Conversion to open in these situations is likely due to surgeon skill and experience, difficulty in visualization, increased vascularity, and prolonged operating time and bleeding that may be associated with large leiomyoma.
Hysterectomy performed for a diagnosis of gynecologic cancer demonstrated a dramatic decrease in AH (93.1% in 2000 to 55.2% in 2010) and increase in LH (3.4% in 2000 to 36.8% in 2010). Unfortunately, there is limited data available in the gynecologic oncology literature regarding current national trends of hysterectomy route, and therefore comparison of our institutional data with national data is not possible. Recent studies utilizing national hospital discharge data have only included benign disease in the analysis of hysterectomy route (5, 9).
The number of ureteral and bladder injuries in this dataset is well below the national average. Since cystoscopy is not routinely performed after hysterectomy, there may be unrecognized injuries resulting in under-reporting and thus delayed identification. This study does not account for patients who had delayed diagnosis of lower urinary tract injury as this analysis only included the admission during which the hysterectomy was performed. This may specifically limit the ability to detect urinary tract injuries in laparoscopically performed procedures since the LOS is shorter (1.0 days) and therefore patients may be discharged prior to injuries being recognized. Jelovsek et al reported lower urinary tract injury rates of 4% with total laparoscopic hysterectomy with only 40% of injuries recognized without the use of concomitant cystoscopy (13). Therefore, this retrospective analysis may underestimate the number of urethral or bladder injuries, since the rate of cystoscopy at time of hysterectomy was only 21.2%. Previous studies have demonstrated that bladder, ureteral, and bowel complications were lower for those surgeons who had performed >30 laparoscopic hysterectomies as compared to those who had performed fewer (14). In this study, there did not appear to be an improvement in lower urinary tract injury rates over time; however, it is impossible to determine if individual surgeons had lower complication rates over time since there were many providers included in this analysis. It is important to note that this study did not demonstrate an increase in the number of urinary tract injuries as the proportion of laparoscopically performed hysterectomies increased throughout the study period. However, this study would only detect those injuries diagnosed during the hospitalization for the hysterectomy and does not account for delayed injuries that may be more common with laparoscopic techniques and would present later.
Vaginal and laparoscopic hysterectomies are associated with a shorter length of stay compared with abdominal hysterectomy, and over the last decade both procedures have demonstrated a trend towards even shorter hospital stays. Our results are similar to data from the 2005 Nationwide Inpatient Sample with the shortest LOS seen in LH followed by VH and AH (5). The average age of women undergoing laparoscopic hysterectomy in this study was lower than that of abdominal or vaginal approaches. Other studies have demonstrated similar findings (5, 9), which may be explained by a high demand for laparoscopic surgery and cosmesis in younger women. Also, the younger age of women undergoing laparoscopic hysterectomy may represent women who are having a hysterectomy for an indication of pain. There was a significant trend of increasing patient age for all surgical approaches to hysterectomy over the ten year period. This may be due to younger women choosing alternatives to hysterectomy, such as progestin-based intrauterine devices, uterine artery embolization, endometrial ablation, or leuprolide. Also, as the risk of anesthesia has decreased and as minimally-invasive surgical approaches have become more widely practiced (15), older patients are more likely to be offered and undergo advanced surgical procedures.
Racial differences were noted in the percentages of women undergoing hysterectomy as well as the route of hysterectomy. The larger proportion of Caucasian women undergoing hysterectomy compared to African American women may be due to differences in access to care or differences in referral patterns. The finding of racial differences in route of hysterectomy is consistent with national data (9). We speculate that our finding of higher rates of AH and LH → AH and lower rates of LH and VH in African American women is due to the higher percentage of fibroids in this population compared with Caucasian women.
The main strength of this study is its large size and capacity to determine the route of hysterectomy even before laparoscopic ICD-9 codes were available at a national level. The ability to characterize laparoscopic cases prior to the development of laparoscopic ICD-9 codes will perhaps result in a more accurate depiction of regional trends and may be an estimate of national trends. The main weaknesses of this study include its retrospective design and inability to verify correct coding of 146 out of 13,973 procedures (1.0%). Because procedure and diagnosis codes are only included for the admission during which the hysterectomy was performed, any patient who was readmitted with a delayed diagnosis of lower urinary tract injury would not be included in this study. Another limitation is generalizability to other US hospitals as our data is from a large tertiary hospital with an active minimally invasive surgery division. Lastly, our institution had relatively late adoption of robotic technology, and therefore robotically performed hysterectomies were not analyzed separately from laparoscopic hysterectomies. This may make our data less representative of recent national trends.
This study confirms that rates of laparoscopic procedures for hysterectomy have dramatically increased over the last decade at our tertiary hospital, which is consistent with other reports in the literature. As national initiatives encourage minimally-invasive procedures for hysterectomy, this procedure will likely become even more common (11). Recent development of specific procedure codes for laparoscopic gynecologic procedures will improve tracking of trends in these procedures nationally.
Acknowledgments
Financial Support:
This publication was made possible by Grant Number 2UL1RR024153-06 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presentation: Oral presentation; 32nd Annual American Urogynecologic Society Scientific Meeting. Providence, RI. Sept 16th, 2011.
Disclosures: The authors report no conflict of interest.
References
- 1.CDC website. National Center for Health Statistics. Number of all-listed procedures for discharges from short-stay hospitals: United States, 2010. 2013 Jan; http://www.cdc.gov/nchs/data/nhds/10Detaileddiagnosesprocedures/2010det10_alllistedprocedures.pdf,
- 2.Reich H, DeCaprio J, McGlynn F. Laparoscopic hysterectomy. J Gynecol Surg. 1989;5:213. [Google Scholar]
- 3.Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr L, Garry R, van Voorst S, Mol MWJ, Kluivers KB. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database of Systematic Reviews. 2009;(Issue 3) doi: 10.1002/14651858.CD003677.pub4. Art. No.CD003677. [DOI] [PubMed] [Google Scholar]
- 4.Farquhar CM, Steiner CA. Hysterectomy rates in the United Sstates 1990–1997. Obstet Gynecol. 2002;22:229–234. doi: 10.1016/s0029-7844(01)01723-9. [DOI] [PubMed] [Google Scholar]
- 5.Jacoby VL, Autry A, Jacobson G, Domushh R, Nakagawa S, Jacoby A. Nationwide use of laparoscopic hysterectomy compared with abdominal and vaginal approaches. Obstet Gynecol. 2009;114:1041–1048. doi: 10.1097/AOG.0b013e3181b9d222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC website. Conversion Table of New ICD-9-CM Codes. 2010 Oct; http://www.cdc.gov/nchs/data/icd9/icdcnvFY11.pdf,
- 7.United States Census Bureau. State & County QuickFacts. 2012 Dec; http://quickfacts.census.gov/qfd/states/42/4261000.html,
- 8.2000 Pittsburgh Census. 2012 Dec; http://www.city.pittsburgh.pa.us/cp/assets/census/2000_census_pgh_jan06.pdf.
- 9.Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy Rates in the United States, 2003. Obstet Gynecol. 2003;110:1091–1095. doi: 10.1097/01.AOG.0000285997.38553.4b. [DOI] [PubMed] [Google Scholar]
- 10.Oliphant SS, Jones KA, Wang L, Bunker CH, Lowder JL. Trends over time with commonly performed obstetric and gynecologic inpatient procedures. Obstet Gynecol. 2010;116(4):926–931. doi: 10.1097/AOG.0b013e3181f38599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choosing the route of hysterectomy for benign disease. ACOG Committee Opinion No. 444. American College of Obstetricians and Gynecologist. Obstet Gynecol. 2009;114:1156–1158. doi: 10.1097/AOG.0b013e3181c33c72. [DOI] [PubMed] [Google Scholar]
- 12.Lowder JL, Oliphant SS, Ghetti C, Burrows LJ, Meyn LA, Balk J. Prophylactic bilateral oophorectomy or removal of remaining ovary at the time of hysterectomy in the United States, 1979–2004. Am J Obstet Gynecol. 2010;202:538, e1–e9. doi: 10.1016/j.ajog.2009.11.030. [DOI] [PubMed] [Google Scholar]
- 13.Jelovsek JE, Chiung C, Chen G, Roberts SL, Paraiso MF, Falcone T. Incidence of lower urinary tract injury at the time of total laparoscopic hysterectomy. JSLS. 2007;11:422–427. [PMC free article] [PubMed] [Google Scholar]
- 14.Mäkinen J, Johansson J, Tomás C, Tomás E, Heinonen PK, Laatikainen T, Kauko M, Heikkinen AM, Sjöberg J. Morbidity of 10,110 hysterctomies by type of approach. Human Reproduction. 2001;16(7):1473–1478. doi: 10.1093/humrep/16.7.1473. [DOI] [PubMed] [Google Scholar]
- 15.Gerten KA, Markland AD, Lloyd LK, Richter HE. Prolapse and incontinence surgery in older women. J Urol. 2008;179(6):2111–2118. doi: 10.1016/j.juro.2008.01.089. [DOI] [PMC free article] [PubMed] [Google Scholar]


