Abstract
Objective
Similar to back pain, neck pain has recently shown to have increasing prevalence. Magnetic resonance imaging (MRI) is useful in identifying the causes of neck pain. However, MRI shows not only pathological lesions but also physiological changes at the same time, and there are few Korean data. The authors have attempted to analyze the prevalence of disc degeneration in highly selective asymptomatic Korean subjects using MRI.
Methods
We performed 3 T MRI sagittal scans from C2 to T1 on 102 asymptomatic subjects (50 men and 52 women) who visited our hospital between the ages of 14 and 82 years (mean age 46.3 years). All images were read independently by three observers (two neurosurgeons and one neuroradiologist) who were not given any information about the subjects. We classified grading for cervical disc herniation (HN), annular fissure (AF), and nucleus degeneration (ND), using disc degeneration classification.
Results
The prevalence of HN, AF, and ND were 81.0%, 85.9%, and 95.4%, respectively. High prevalence of HN, AF, and ND was shown compared to previous literature.
Conclusion
In asymptomatic Korean subjects, the abnormal findings of 3 T MRI showed a high prevalence in HN, AF, and ND. Several factors might play important roles in these results, such as population-specific characters, MRI field strength, and disc degeneration grading system.
Keywords: Degeneration, Cervical disc, Magnetic resonance imaging
INTRODUCTION
Similar to back pain, neck pain has recently shown to have increasing prevalence. Among many examinations, magnetic resonance imaging (MRI) is more accurate than simple radiography, myelography, discography, and computed tomography (CT). However, MRI shows not only pathological lesions but also physiological changes at the same time. These cervical disc degenerations are common after middle age, and it affects more than 80% of patients over 60 years without producing any symptoms11). Degenerative changes could be considered to be more closely related to age-related physiological changes than to pathological changes in asymptomatic people, but there are few statistical data. Given this background, the authors attempted to analyze the prevalence of cervical disc degeneration using well known degeneration classification in asymptomatic Korean subjects.
MATERIALS AND METHODS
Study population
From December 2007 to March 2008, a total of 102 asymptomatic subjects (50 men and 52 women) who visited our hospital between the ages of 14 and 82 years (mean age 46.3 years) were selected for participation in this study (Table 1). The study was approved by the hospital Institutional Review Board. Healthy subjects were recruited from asymptomatic visitors of the Health Screening Center by history-taking. We used this selection method in order to exclude any bias as completely as possible.
Table 1.
Asymptomatic subject's mean age and standard deviation
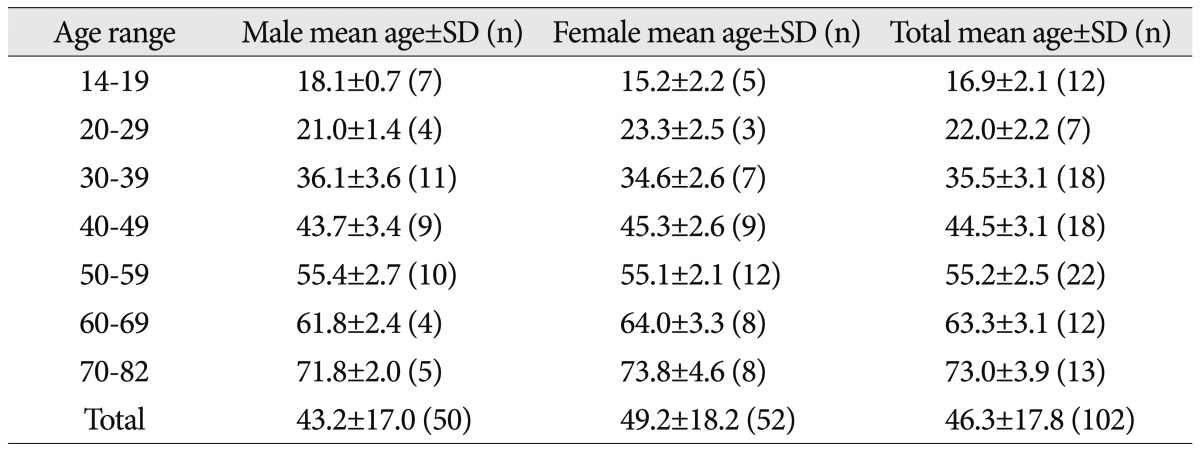
SD : standard deviation
Written informed consent was obtained from all subjects. The subjects were carefully screened using a modified neck pain questionnaire and history taking. Individuals were only enrolled if they had never experienced relevant pain in the neck area, shoulder, and elbow joint, never undergone radiation at the upper extremities and never had any neurological deficits.
The absence of relevant symptoms in these areas was defined as never having seen a physician, physiotherapist, chiropractor, acupuncture, oriental herb medication, or other such health care professional, and never having missed workday due to these symptoms. The rationale for these criteria was the notion that episodes of transient neck pain are common and less likely to be recalled after spontaneous regression3). Cases in which hospitalization treatment was administered for trauma such as a traffic accident were also excluded, because trauma required hospitalization may have undetected cervical diseases.
MR imaging methods
From C2 to T1, magnetic resonance (MR) scans were performed with a 3.0-Tesla imager (Achieva 3.0 T X-series, Philips Medical Systems, the Netherlands) with a dedicated receive-only spine coil. The protocol included sagittal T2-weighted [2593/120 (repetition time msec/echo time msec)] turbo spin-echo imaging of the entire cervical spine with the following sequence parameters : matrix, 516×256; field of view, 270 mm; section thickness, 3 mm; intersection gap, 0.3 mm; and echo train lengths of 16 for T2-weighted images (T2WI). Though an axial sequence is also necessary to differentiated differences in disc pathology, but the authors use only sagittal imaging for convenience.
All images were sent to the in-hospital picture archive and communication system (PACS; Infinitt PACS, invented by Infinitt Co., Seoul, Korea) and reviewed using a 21.3-inch, 5-megapixel medical flat grayscale display (MFGD 5421, Barco, Kortrijk, Belgium) on a HP xw4400 workstation base unit (Hewlett-Packard Co., CA, USA). The monitor has a 2048×2560 resolution, 0.165 mm pixel pitch, 422.4×337.9 mm active screen area, 800 : 1 dark room contrast, and 700 cd/m2 luminance.
Image analysis
The imaging studies in all 102 asymptomatic subjects were read independently by three of the authors (two neurosurgeons and one neuroradiologist) who were not given any information about the subjects. To eliminate potential reading bias, the images of 30 random symptomatic patients were mixed with the subject's images. We did not analyze the random 30 patients' results in final analysis. There was no case of blocked vertebra or fusion. Six cervical disc levels were examined in each subject, and a total of 612 discs were examined.
Degree of degeneration
To establish the criteria for determining disc abnormality, we classified the three measurement categories : herniation (HN), annular fissure (AF), and nucleus degeneration (ND). There are many classifications for disc herniation and degeneration, we used the most prevalent terms9) for HN and modified Pfirrmann's classification8) for ND. The reason for the selection of the three categories is that they are abnormal findings with a high prevalence in normal healthy subjects.
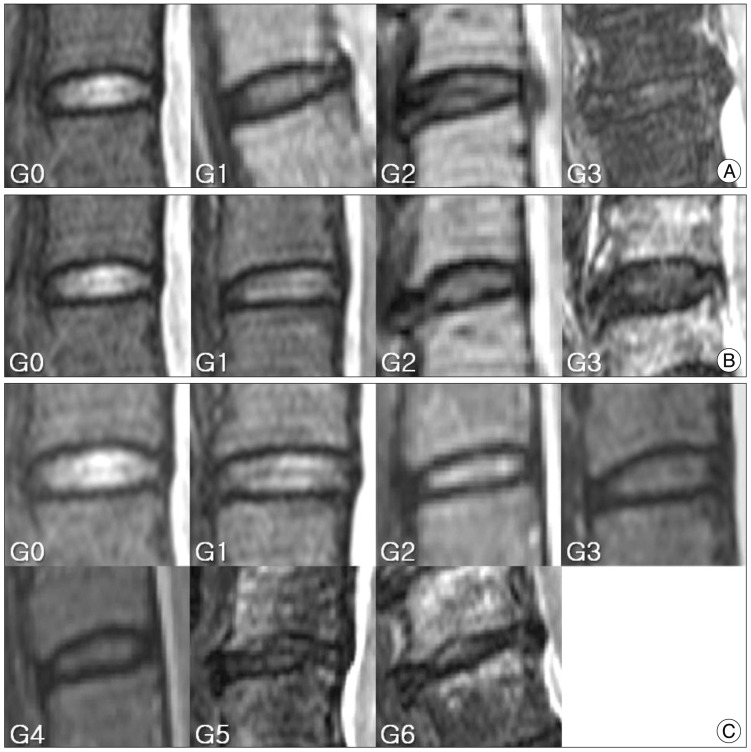
Herniation
Disc herniation was classified as local protrusion in the intervertebral space. The following terms were used to describe disc abnormalities : normal, bulging, protrusion, extrusion, and sequestration4,10). Disc was considered to be normal when it did not reach beyond the borders of the adjacent vertebral bodies. Bulging was defined as a circumferential, symmetric disc extension around the vertebral border. Protrusion was defined as a focal or asymmetric extension of the disc beyond the vertebral border, with the disc origin broader than any other dimension of the protrusion. Extrusion was defined as a more extreme extension of the disc beyond the vertebral border, with the base against the disc of origin narrower than the diameter of the extruding material and a connection between the material and the disc of origin. Sequestration was defined as a free disc fragment that was distinct from the parent disc (Table 2, Fig. 1).
Table 2.
Degree of disc degeneration
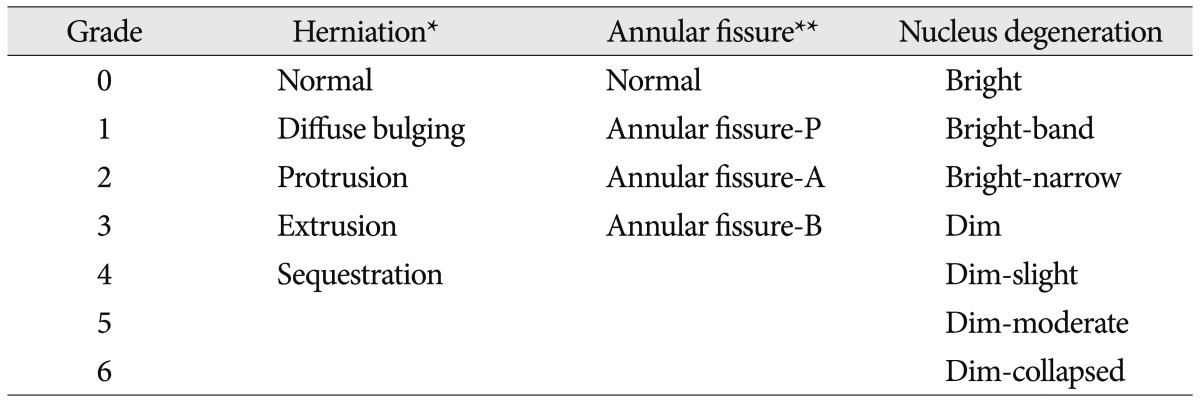
*Herniation : Disc finding on the sequential sagittal view. 1) Diffuse bulging : Nonfocal, non-osseous material extending beyond the normal disc space in a circumferential manner on the sequential sagittal view, 2) Protrusion : Nucleus pulposus contained in the annulus fibrosus but with contour abnormality, 3) Extrusion : Nucleus pulposus extending through the annulus fibrosus but still contiguous with the host nucleus, 4) Sequestration : Free fragment migration of herniated fragment away from the disc space. **Annular fissure : Nucleus signal. 0) Normal : No annular fissure or high-signal intensity zone, 1) Annular fissure-P : Annular fissure at posterior or posterolateral site, 2) Annular fissure-A : Annular fissure at anterior site, 3) Annular fissure-B : Annular fissure at both anterior and posterior site
Fig. 1.
References of image for disc degeneration are shown. The criteria of classification are described in Table 2 and 3. A : Herniation. G0, normal. G1, diffuse bulging. G2, protrusion. G3, extrusion. B : Annular fissure. G0, normal. G1, Annular fissure at posterior or posterolateral site. G2, annular fissure at anterior site. G3, annular fissure at anterior and posterior site. C : Nucleus degeneration. G0, normal. G1, normal disc height and hyperintense nucleus signal with horizontal dark band. G2, decreased disc height and hyperintense nucleus signal with or without horizontal dark band. G3, normal disc height and decreased nucleus signal with slightly or heterogeneous irregularity. G4, slightly decreased disc height and decreased nucleus signal with slightly or heterogeneous irregularity. G5, moderately decreased disc height and decreased nucleus signal with moderately. G6, collapsed disc height and hypointense nucleus signal.
Annular fissure and high-signal intensity zone
AF was defined as a high signal at the fibrous ring of an intervertebral disc on T2WI. In addition, high-signal intensity zone (HIZ) is a high-intensity signal (bright white) located in the substance of the annulus fibrosus, clearly dissociated from the signal of the nucleus pulposus. It is surrounded superiorly, inferiorly, posteriorly and anteriorly by the low-intensity (black) signal of the annulus fibrosus and is appreciably brighter than that of the nucleus pulposus. HIZ probably corresponds to annular tears1). AF was graded according to fissure site of the disc at the most clearly lesion from entire disc midsagittal T2WI. And the prevalence of HIZ was analyzed (Table 2, Fig. 1).
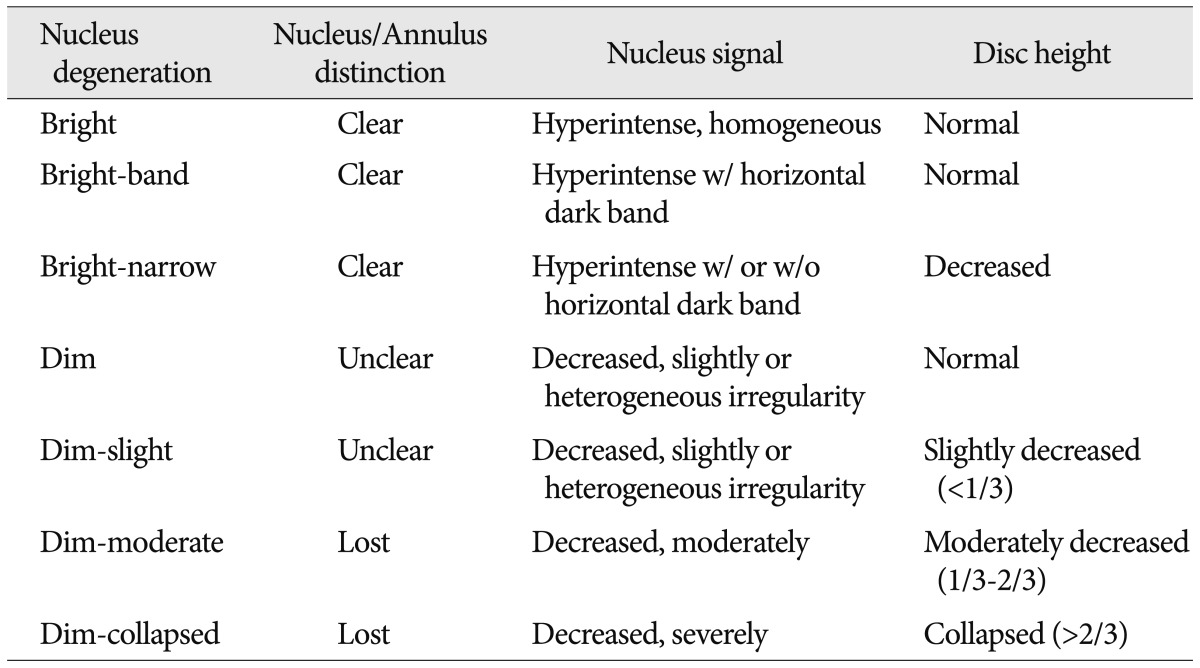
Nucleus degeneration
The extent of intervertebral disc ND was graded on midsagittal T2WI according to the criteria of modified Pfirrmann classification8). This grading correlates with the extent and loss of signal intensity in the nucleus pulposus of the intervertebral disc. Intervertebral disc narrowing was diagnosed in cases in which decrease of more than 33.3% in the intervertebral disc space was present. The seven findings in the cervical intervertebral disc were : bright (homogeneous hyperintense nucleus), bright-band (nucleus clear distinction with horizontal dark band), bright-narrow (nucleus clear with disc height decreased), dim (nucleus unclear distinction with normal height), dim-slight (nucleus unclear with slightly decreased), dim-moderate (nucleus unclear with moderately decreased), dim-collapsed (nucleus unclear with collapsed). For the purpose of this investigation, grade 0-2 were grouped together and grade 3-6 were the more advanced grades of ND (Table 2, 3, Fig. 1).
Table 3.
Degree of nucleus degeneration
Analysis of the prevalence of abnormal findings
The prevalence of the various abnormalities was calculated by disc count (DC) and person count (PC). DC is the number of discs regardless of subjects (0-612) and PC is the number of subjects with disc degeneration (0-102).
Statistical analysis
The prevalence of the various abnormalities was calculated by averaging the scores of three readers. Inter-observer reproducibility was assessed using Kendall's coefficient of concordance. The Kendall correlation can be interpreted as the coefficient of concordance to measure the agreement among raters (0, no agreement; 1, complete agreement).
RESULTS
Degree of degeneration
Herniation
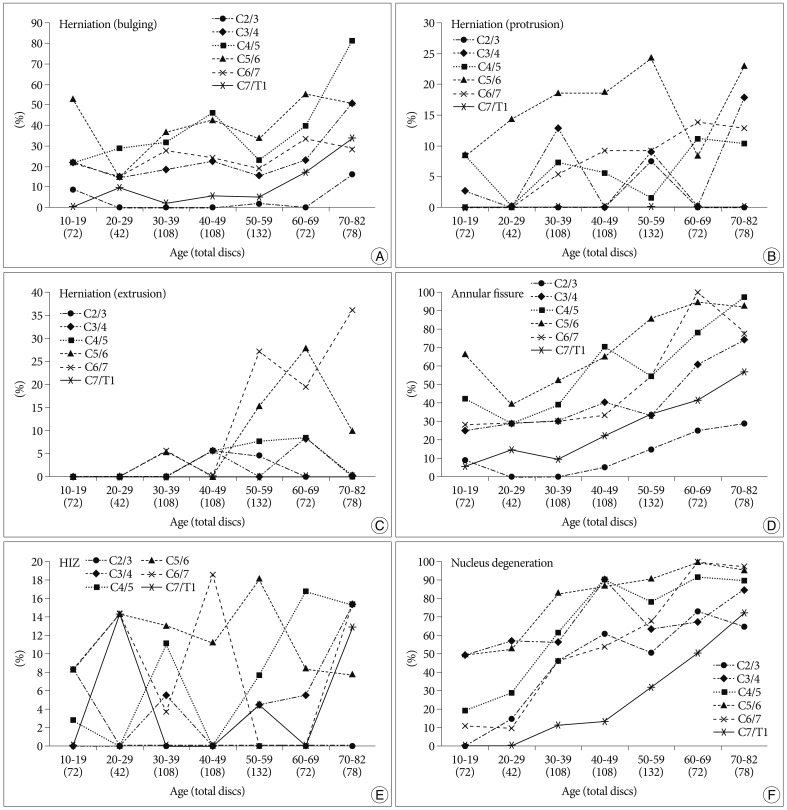
Authors found bulging of disc in 142.3 (23.3%) of all 612 discs in 70.0 (68.6%) of the 102 subjects (Table 4). The score of bulging slightly increased along with the age, but not proportional to the age. Bulging was almost not seen at the level of C2/3, but the most common levels were C5/6 and C4/5 (Fig. 2). In protrusion, there are 41.0 (6.7%) of all 612 discs in 30.0 (29.4%) of the 102 subjects (Table 4). The score of protrusion slightly increased along with the age, but not proportional to the age. Protrusion was almost not seen at the level of C2/3, but the most common levels were C5/6. Extrusion of disc was found in 30.7 (5.0%) of all 612 discs in 23.3 (22.9%) of the 102 subjects (Table 4). This showed that a peak point was reached at the level of C5/6 in the 60's. In the 70's or older, however, it was reached a peak point at the level of C6/7. Extrusion was not common in cervical levels except the level of C5/6 and C6/7. There were no sequestrations of disc (Table 4).
Table 4.
Abnormal disc degeneration findings according to person and disc count
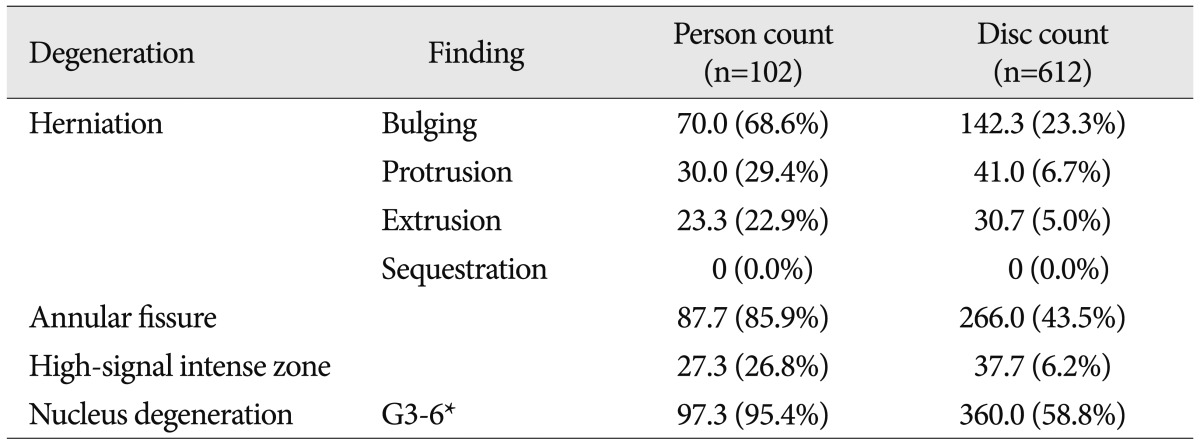
*Advanced grade
Fig. 2.
Graph of disc degeneration prevalence according to age and level, calculated by disc count. A, B and C : Herniation. D : Annular fissure. E : High-signal intensity zone (HIZ). F : Nucleus degeneration.
Annular fissure and high-signal intensity zone
The authors found AF of disc in 266.0 (43.5%) of all 612 discs in 87.7 (85.9%) of the 102 subjects (Table 4). This showed that the score of AF was proportional to the age at all levels. The most common level was C5/6, and the levels of rare were C2/3 and C7/T1 (Fig. 2).
HIZ of disc was found in 37.7 (6.2%) of all 612 discs in 27.3 (26.8%) of the 102 subjects (Table 4). The score of HIZ slightly increased along with the age, but not proportional to the age. HIZ was almost not seen at the level of C2/3. But a peak value was found at the level of L5/6 in the 50's, and at the level of C6/7 in the 40's (Table 4).
Nucleus degeneration
For the analysis of prevalence, grade 0-2 were grouped together and grade 3-6 were the more advanced grades of ND. We defined that advanced grades of ND is abnormal finding of disc. The authors found disc ND in 360.0 (58.8%) of the 612 discs analyzed and in 97.3 (95.4%) of the 102 subjects (Table 4). The graph of ND according to age and level was analyzed. The graph was proportional to age at all levels. Severe ND was found at all levels in elderly group, even in young-aged people at C3/4 and C4/5. The most common level was C5/6, and the level of age-dependent were C6/7>C4/5>C7/T1 in order (Fig. 2).
The results are summarized in Table 4. Table 4 is DC and PC of herniation, annular fissure, and nucleus degeneration of abnormal findings according to subject age and level.
Inter-observer reproducibility
The agreement values for the ND, AF, and HN were 0.968, 0.964, and 0.972 (p<0.0001), using Kendall's coefficient of concordance.
DISCUSSION
Similar to back pain, neck pain has recently shown to have increasing prevalence. Fejer et al.6) reported the prevalence of neck pain by performing a meta-analysis. The point, one year, and lifetime prevalence of neck pain was reported to be 7.6%, 37.2%, and 48.5%, respectively. However, cervical disc degeneration is frequently found on MRI, even in the absence of neck pain. Christe et al.5) reported that disc herniation (above of bulging) was found in 30.6% of asymptomatic subjects.
The authors' analysis showed that the prevalence of HN, AF, and ND in asymptomatic subjects were 81.4%, 85.9%, and 95.4%, respectively. In our results, abnormal findings on MRI were observed with a high prevalence of more than 80%. Miyazaki et al.12) reported that the prevalence of degeneration in symptomatic cases was 72.3%. Our results showed higher prevalence than symptomatic cases. These results led us to reconsider the relationships between cervical symptoms and abnormal findings on MRI.
In our results, ND showed higher score than HN and AF. Notably, degeneration was more frequent in the upper cervical segments than in the lower cervical segments, such as C2/3 and 3/4. These findings may come from frequent rotation of the upper segment, rare radiculopathy due to upper cervical disc degeneration, high power resolution of 3 T MRI, and so on. Another possibility is the effects of lower disc height and presence of artifacts from surrounding bones (mandible, teeth, mastoid, occiput, and so on).
We reviewed literatures about MR images in asymptomatic subjects (Table 5). The authors didn't use open call recruitment. We stayed all day long at doctor's office of Health Screening Center and chose subject by history-taking without mention of study purpose. In the table, there were very high prevalence in HN, AF, and ND.
Table 5.
International literatures comparison of herniation, annular fissure, and nucleus degeneration in asymptomatic subjects (%)
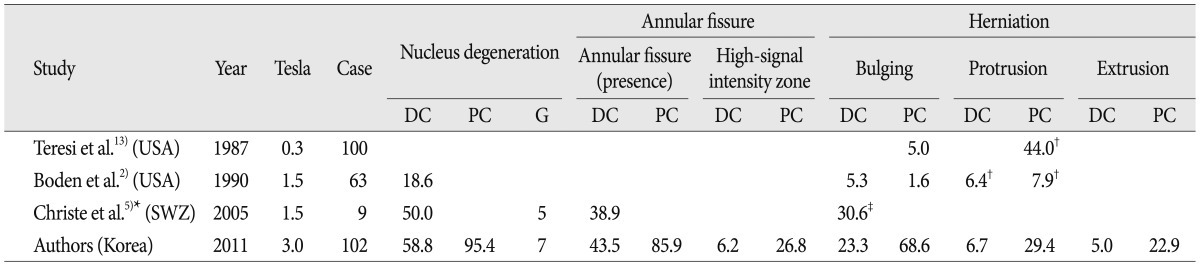
*Autopsy study, †Included protrusion and more advanced herniation (extrusion and sequestration), ‡Included bulging and more advanced herniation (protrusion, extrusion, and sequestration). DC : disc count, PC : person count, G : grade, US : the United States of America, SWZ : Switzerland
Because all studies used different criteria, we performed a modified statistical analysis (Table 6). This comparison was made in the same manner as the previous reports, using the previous criteria of grading and selecting age of population. The modified results were similar to the original results.
Table 6.
Comparison of herniation, annular fissure, and nucleus degeneration between the previous reports and authors' modified results which were changed according to the criteria of previous studies
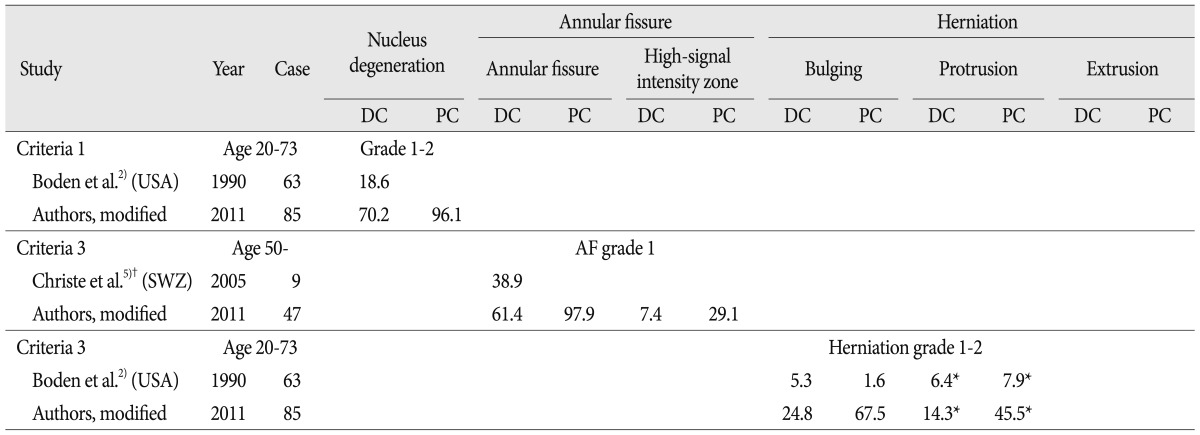
*Included protrusion and more advanced herniation (extrusion and sequestration), †Autopsy study. DC : disc count, PC : person count, USA : the United States of America, SWZ : Switzerland, AF : annular fissure
We used a more detailed grading system to asymptomatic subject, not symptomatic patient. And, we used 3 T MRI. However, the authors think that these factors have a small effect on prevalence. High prevalence would be the population-specific prevalence, especially came from in old peoples.
The overall resolution power of MRI, which was the first used in clinical practice around 1976, improved in spatial resolution by the 3 T MRI. It can make imaging thinner slices7). But, the authors thought that 3 T MRI would not have far superior images in spine than 1.5 T MRI. Therefore, the additional study will be needed on the comparison between 3 T and 1.5 T MRI images in same subjects. However, there is no doubt that 3 T MRI will become more prevalent in future.
The authors performed cervical MRI on asymptomatic subjects, and reported that abnormal findings were detected with high prevalence. With this result, physicians must be thoughtful for these abnormal findings when making a decision of spinal surgery. Because degenerative changes are observed in most subjects aged 40 and older, disc degeneration can be result from both physiological changes and pathological lesions.
CONCLUSION
In asymptomatic Korean subjects, the abnormal findings of 3 T MRI showed a high prevalence in herniation, annular fissure, and nucleus degeneration. Several factors might play important roles in these results, such as population-specific characters, MRI field strength, and disc degeneration grading system.
Acknowledgements
The authors thank Ji Min Sung, Ph.D. and Dae Hyung Lee, Ph.D., for their assistance in statistical design and testing.
References
- 1.Aprill C, Bogduk N. High-intensity zone : a diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol. 1992;65:361–369. doi: 10.1259/0007-1285-65-773-361. [DOI] [PubMed] [Google Scholar]
- 2.Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:1178–1184. [PubMed] [Google Scholar]
- 3.Boos N, Rieder R, Schade V, Spratt KF, Semmer N, Aebi M. 1995 Volvo Award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine (Phila Pa 1976) 1995;20:2613–2625. doi: 10.1097/00007632-199512150-00002. [DOI] [PubMed] [Google Scholar]
- 4.Brant-Zawadzki MN, Jensen MC, Obuchowski N, Ross JS, Modic MT. Interobserver and intraobserver variability in interpretation of lumbar disc abnormalities. A comparison of two nomenclatures. Spine (Phila Pa 1976) 1995;20:1257–1263. doi: 10.1097/00007632-199506000-00010. discussion 1264. [DOI] [PubMed] [Google Scholar]
- 5.Christe A, Läubli R, Guzman R, Berlemann U, Moore RJ, Schroth G, et al. Degeneration of the cervical disc : histology compared with radiography and magnetic resonance imaging. Neuroradiology. 2005;47:721–729. doi: 10.1007/s00234-005-1412-6. [DOI] [PubMed] [Google Scholar]
- 6.Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population : a systematic critical review of the literature. Eur Spine J. 2006;15:834–848. doi: 10.1007/s00586-004-0864-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fries P, Runge VM, Kirchin MA, Watkins DM, Buecker A, Schneider G. Magnetic resonance imaging of the spine at 3 Tesla. Semin Musculoskelet Radiol. 2008;12:238–252. doi: 10.1055/s-0028-1083107. [DOI] [PubMed] [Google Scholar]
- 8.Griffith JF, Wang YX, Antonio GE, Choi KC, Yu A, Ahuja AT, et al. Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2007;32:E708–E712. doi: 10.1097/BRS.0b013e31815a59a0. [DOI] [PubMed] [Google Scholar]
- 9.Harris RI, Macnab I. Structural changes in the lumbar intervertebral discs; their relationship to low back pain and sciatica. J Bone Joint Surg Br. 1954;36-B:304–322. doi: 10.1302/0301-620X.36B2.304. [DOI] [PubMed] [Google Scholar]
- 10.Masaryk TJ, Ross JS, Modic MT, Boumphrey F, Bohlman H, Wilber G. High-resolution MR imaging of sequestered lumbar intervertebral disks. AJR Am J Roentgenol. 1988;150:1155–1162. doi: 10.2214/ajr.150.5.1155. [DOI] [PubMed] [Google Scholar]
- 11.Matsumoto M, Fujimura Y, Suzuki N, Nishi Y, Nakamura M, Yabe Y, et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80:19–24. doi: 10.1302/0301-620x.80b1.7929. [DOI] [PubMed] [Google Scholar]
- 12.Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC. Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech. 2008;21:288–292. doi: 10.1097/BSD.0b013e31813c0e59. [DOI] [PubMed] [Google Scholar]
- 13.Teresi LM, Lufkin RB, Reicher MA, Moffit BJ, Vinuela FV, Wilson GM, et al. Asymptomatic degenerative disk disease and spondylosis of the cervical spine : MR imaging. Radiology. 1987;164:83–88. doi: 10.1148/radiology.164.1.3588931. [DOI] [PubMed] [Google Scholar]