Abstract
Background
Sleep disorder is a common problem in adults and affects physical and mental health. We investigated factors associated with poor sleep quality in Korean primary care.
Methods
A total of 129 couples (129 husbands and 129 wives) aged 30 to 79 years were included in this study from March, 2009 to February, 2010. The subjects were surveyed using a specific questionnaire. Sleep disorder was defined by a Pittsburgh Sleep Quality Index global score greater than 5 (poor sleepers). The subjects were divided into a group of good sleepers (n = 160) and a group of poor sleepers (n = 98). Socio-demographic and clinical covariates including age, sex, depression, spouse sleep disorder, and spouse depression were reported.
Results
Poor sleep quality was present in 38.0% of total subjects. According to chi-square test results, female, patients with depression, and low sleep quality of spouse were significantly associated with sleep disorder. In multivariate logistic regression analysis, depression increased the risk of poor sleep quality (odds ratio [OR], 7.775; 95% confidence interval [CI], 2.555 to 23.661), and non-risky drinking decreased the risk of poor sleep quality (OR, 0.343; 95% CI, 0.128 to 0.924).
Conclusion
In our study, more than one-third of participants had poor sleep quality. Depression was a strong independent factor associated with sleep problems.
Keywords: Poor Sleep Quality, Sleep Initiation and Maintenance Disorders, Pittsburgh Sleep Quality Index, Depression
INTRODUCTION
Sleeping is crucial for health improvement, and sleep disorders can also affect physical and mental health in addition to affecting quality of life. Insomnia is a common problem in adults, and reports of its prevalence vary depending on how it is defined. Previous research revealed that the prevalence rate of insomnia in adults is 10% to 30% in Western countries.1-3) In Japan, a study on insomnia involving 3,030 subjects over the age of 20 from the general population revealed a prevalence rate of 21.4%.4) Cho et al.5) conducted a telephone survey with 5,000 study subjects between 20 and 69 years, wherein insomnia was present in 22.8% (male 20.2% and female 22.8%) of the subjects.
The known risk factors of insomnia include female sex, old age, depression, snoring, low level of physical activity, presence of underlying disease, low education level and economic status, and stress. Another study affirmed that 40% of insomnia patients suffer from comorbid psychiatric disorders.6) Depressed patients can often have accompanying insomnia, and insomnia alone increases the risk of developing depression.6) In addition, the presence of physical illness can increase the risk of insomnia, with insomnia potentially having a secondary effect on the body as well. Of great consequence, insomnia is also related to the risk of cardiovascular disease,7-9) with reports that decreased sleep time is linked to an increased risk of heart disease and diabetes.10,11)
Although various studies have pointed out factors related to sleep disorders, studies investigating patients who visit primary care facilities and analyzing the relationship between insomnia and spouse-related factors are lacking. This study was conducted to evaluate the sleep quality of patients visiting primary care facilities and to identify the prevalence of sleep disorders by using the Pittsburgh Sleep Quality Index (PSQI),12) as well as to assess related factors such as gender, age, and history of depression. Furthermore, the study sought to investigate the relevance of the spouse's sleep disorder or depression, as this could affect the sleep environment.
METHODS
1. Study Subjects
Study subjects were selected among patient couples presenting between March 2009 and February 2010 at the department of family medicine at 25 university hospitals nationwide or two other private clinics, for the treatment of chronic diseases such as diabetes, hypertension, and hyperlipidemia. Both spouses had to be over 30 years of age, live in a household consisting of two or more generations, and be able to complete the questionnaire in order to be included as subjects. From the family cohort data of 500 adult households, the data of 317 couples were selected in order of registration. Of these, 129 couples (258 individual subjects in total) who had completed all parts of the sleep quality questionnaire were selected as the final study subjects.
2. Study Methods
1) Measurement of sleep quality
The tool used for measuring sleep quality was the PSQI.12) The PSQI, a self-administered questionnaire for evaluating quality of sleep in the past month, is composed of 7 subcategories: sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, hypnotic medication use, and daytime dysfunction. Each item in the PSQI is scored between 0 and 3; the PSQI global score is the sum of these items, and scores range from 0 to 21. In the present study, a subject was categorized as a good sleeper if the PSQI global score was 5 or less, and as a poor sleeper if the PSQI global score was 6 or more.12)
2) Evaluation and definition of depression
The Korean edition of the Beck Depression Inventory13) was used to evaluate depression, and subjects with a score of 21 or higher were defined as having depression. Patients were also classified as having depression if their primary doctor reported that they had a comorbidity of depression.
3) Anthropometrics
Along with the questionnaire, healthcare providers measured subjects' height and weight by using the measuring instruments available in each hospital. Body mass index was calculated by dividing weight (kg) by height (m2), and a subject was categorized as obese if his or her body mass index was above 25 kg/m2, following the World Health Organization's Asia-Pacific standard.14)
4) Smoking and alcohol consumption
Subjects were categorized as smokers and nonsmokers. The Alcohol Use Disorders Identification Test-Korean version15) was used to assess drinking habits. Subjects were identified as risky drinkers if their score was 8 or more for males and 4 or more for females, and as non-risky drinkers if they scored below 8 for males and below 4 for females. Only persons who did not drink at all were defined as non-drinkers.
5) Statistical methods
The collected data was analyzed with SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). Sociodemographic characteristics were used for categorizing subjects as good sleepers and poor sleepers based on the PSQI global score, as well as for comparing results; the chi-square test was used for statistical analysis. Logistic regression analysis was also conducted to explore the relationship between sleep disorders and age, gender, depression, spouse's sleep disorder, and spouse's depression.
RESULTS
1. Sociodemographic Characteristics and Sleep Quality
The study subjects who completed all parts of the PSQI questionnaire were 129 couples (a total of 258 people), that is, 129 men and 129 women. Among the subjects, 98 persons (38.0%) were identified as poor sleepers, with female subjects having a higher rate of reporting poor sleep quality than male subjects. No major difference existed in the frequency of poor sleep quality among different age groups. Good sleepers had an average age of 57.8 ± 8.3 years, and poor sleepers had an average age of 56.6 ± 8.9 years, a difference that was not significant. Additionally, there was no significant difference in the two groups in terms of income, education level, drinking habits, or smoking status (Table 1).
Table 1.
Baseline characteristics of study subjects
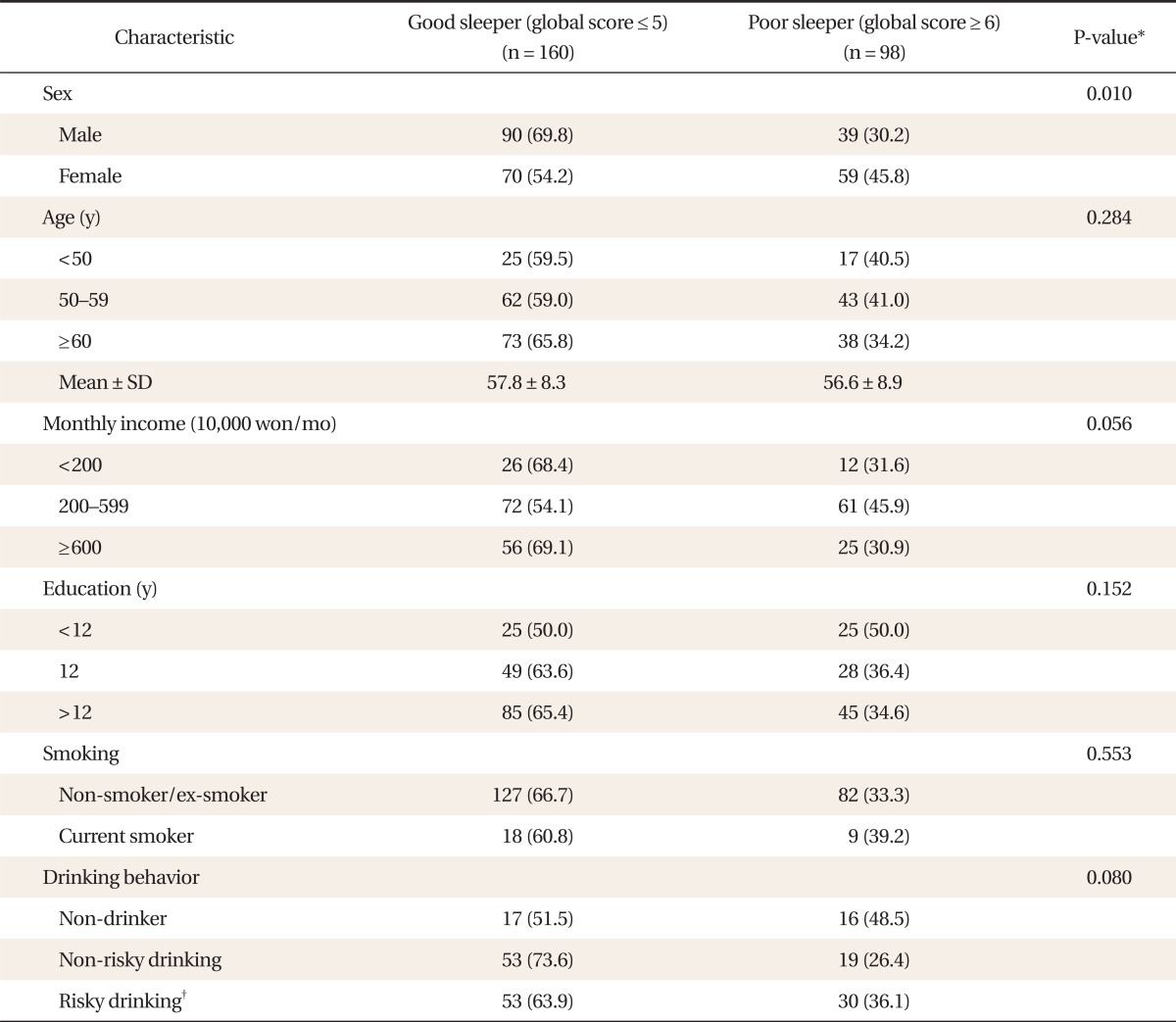
Values are presented as number (%). Missing data were excluded.
*P-values were calculated by chi-square test. †Alcohol Use Disorders Identification Test-Korean version score male ≥8, female ≥4.
2. Factors Related to Sleep Quality
In patients with depression, there was a significantly higher frequency of poor sleepers, albeit depression in the spouse was not related to poor sleep quality. However, the group that reported the spouse's poor sleep quality had a higher frequency of poor sleep quality. Obesity, other comorbid disorders, and medication usage showed no relation to poor sleep quality (Table 2). Multivariate logistic regression analysis was conducted with variables that had a significance level of ≤0.1 in the age and univariate analysis. Depressed subjects showed a significant increase in the risk of poor sleep quality, and non-risky drinkers had a lower risk of poor sleep quality compared to that of non-drinkers and risky drinkers (Table 3).
Table 2.
Factors associated with poor sleep quality
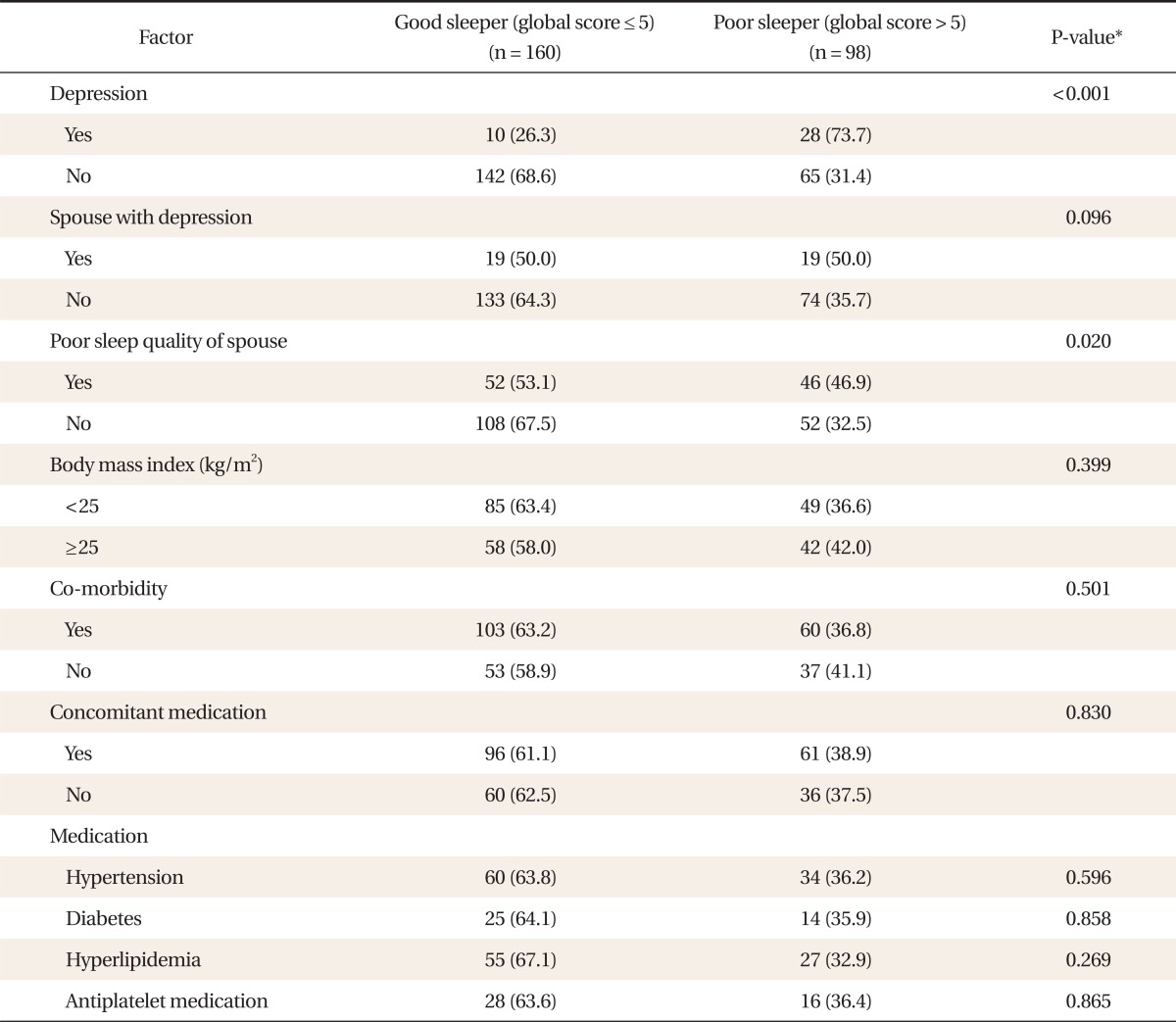
Values are presented as number (%). Missing data were excluded in each variable.
*P-values were calculated by chi-square test.
Table 3.
Multivariate logistic regression analysis of factors associated with poor sleep quality
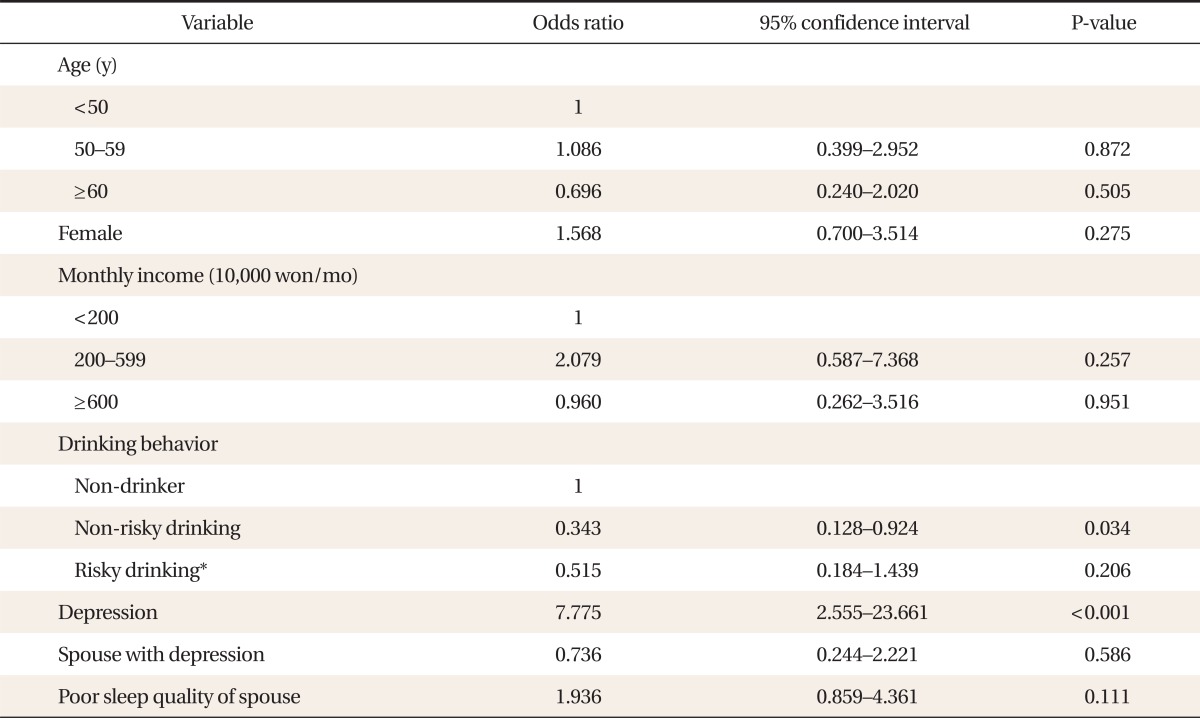
*Alcohol Use Disorders Identification Test-Korean version score male ≥ 8, female ≥ 4.
DISCUSSION
The purpose of this study was to investigate the factors related to the incidence of poor sleep quality in patients who visited primary care facilities. Depression was shown to be a risk factor for poor sleep quality, and non-risky drinkers were shown to have significantly lower frequencies of poor sleep quality than non-drinkers and risky drinkers. The merit of this study lies in its systematic approach to evaluating the quality of sleep in patients visiting primary care facilities, primarily through the use of survey tools. Furthermore, it is a study that once again emphasizes the greatly increased risk of depression in patients complaining of poor sleep quality. Although this is not a large-scale study, it makes an important contribution to existing knowledge in that it investigated the relationship between sleep quality and various patient factors, including lifestyle habits such as smoking, drinking, and exercising, as well as socioeconomic factors.
As seen in the results of the present study, depression remains the main risk factor for developing a sleep disorder.16) Various studies have reported that insomnia is linked to depression, anxiety disorders, and substance abuse, and that insomnia is also a suicide predictor.17-20) Along these lines, other studies state that one-third of patients who have both insomnia and mood disorders suffer from sleep disorders prior to developing mood disorders.20,21) Potentially forming a cyclical connection, insomnia can be a symptom of depression but may also lead to depression.17-20) Therefore, it should be recognized that patients complaining of insomnia and sleep disorders are at high risk for depression, and that appropriate evaluation and treatment for depression is necessary.
The study also showed a reduced risk of poor sleep quality in non-risky drinkers. This finding is in contrast with those of previous studies, most which indicate that alcohol consumption affects sleep by decreasing the rapid eye movement (REM) sleep phase as well as the total sleep time.22) However, according to a study conducted with Japanese subjects, 48.3% of men and 18.3% of women used alcohol as a sleep inducer,23) so an appropriate amount of alcohol might help to improve the quality of sleep.
In this study, increasing age did not lead to decreased quality of sleep. By contrast, it is generally reported that increasing age is associated with increases in sleep disorders,24) due to changes in sleep factors such as decreased amount of total nocturnal sleep time, increased sleep latency, decreased sleep efficiency, and decreased REM sleep.24) The major reason such age-based differences were not observed in the present study is likely due to the average age of the subjects being 57.3 years, with the majority being middle-aged or older. Another possible reason for this finding is that subjects were not selected from the general population, but instead from among patients who visited the department of family medicine in university hospitals for the treatment of chronic diseases such as diabetes, hypertension, cardiovascular disease, and depression.
Women are known to have a higher risk of developing sleep disorders during their menstrual period as well as during menopause.25) They also have a higher incidence of sleep disorders than men because women are more sensitive to stress and the influence of their external environment. In the present study, women had more frequent complaints of poor sleep quality, but this was not shown to be an independent factor in the multivariate analysis. However, various studies have reported that the prevalence of sleep disorders is 1.3 to 1.8 times higher in females than in males; similarly, the present study also showed that poor sleep quality was approximately 1.5 times more frequent in females (30.2% male and 45.8% female).
Despite reports of a connection between low socioeconomic status and sleep disorders,5,26) the present study found no statistically significant relationship between monthly income and sleep disorders. A possible reason is that when subjects' monthly income was categorized into various levels, they differed from the monthly income characteristics of the general population. Of note, the annual average monthly income per household was 3,440,000 KRW in 2009.27)
Among the subjects whose spouses had a sleep disorder, the prevalence of poor sleep quality was higher according to the chi-square test; however, this was not significant in the multivariate logistic regression analysis. A US study previously reported that the presence of sleep disorders in 29 couples who sleep together was affected by the relationship of the couple during the daytime.28) Thus, the results of the present study likely did not show a significant statistical difference because the factors that could affect the couple's relationship, such as the presence of depression in either of the spouses, were corrected for in the multivariate logistic regression analysis. Ultimately, a spouse's sleep disorder is not an independent factor for poor sleep quality; rather, it appears to affect the incidence of sleep disorders in conjunction with other factors that influence the relationship of the couple, such as depression.
Interestingly, some study studies have found that insomnia patients suffer from various concomitant physical illnesses, and that the incidence of insomnia increases with the number of physical illnesses.20,21) However, the prevalence of poor sleep quality did not significantly differ according to concomitant disease states or medication use for diseases such as diabetes, hypertension, and hyperlipidemia. Several possible reasons exist for such a finding. First, the subjects of the studies were patients visiting primary care facilities. Second, since the number of concomitant diseases, disease severity, medication-use according to disease state, and other treatment methods varied for each study subject, the effects on sleep disorder were also different. Hence, no statistically significant relationship was found between diseases present and sleep disorders.
The present study has the following limitations. First, a subjective survey method was used instead of an objective testing method such as polysomnography. However, since the PSQI questionnaire used in the study is a useful tool that shows high concordance with polysomnography results, the results of the present study are also thought to be reliable. Second, the study used a cross-sectional design, making it challenging to prove a causal relationship between poor sleep quality and the related factors. Finally, generalization of the present results to the population at large may be limited since the subjects were mostly patients who had visited the department of family medicine in university hospitals. Nonetheless, the present findings could be helpful in identifying factors related to sleep disorders in patients visiting primary care facilities for chronic diseases such as diabetes, high-blood pressure, and hyperlipidemia.
Evaluation of patients' sleep disorders is paramount because sleep disorders influence physical and mental diseases as well as social functioning. In particular, it should be recognized that the risk of depression is higher in patients complaining of insomnia, and thus patients complaining of sleep disorders must also be assessed for depression.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Simon GE, VonKorff M. Prevalence, burden, and treatment of insomnia in primary care. Am J Psychiatry. 1997;154:1417–1423. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- 2.Ohayon MM, Smirne S. Prevalence and consequences of insomnia disorders in the general population of Italy. Sleep Med. 2002;3:115–120. doi: 10.1016/s1389-9457(01)00158-7. [DOI] [PubMed] [Google Scholar]
- 3.Morin CM, LeBlanc M, Daley M, Gregoire JP, Merette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7:123–130. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R. An epidemiological study of insomnia among the Japanese general population. Sleep. 2000;23:41–47. [PubMed] [Google Scholar]
- 5.Cho YW, Shin WC, Yun CH, Hong SB, Kim J, Earley CJ. Epidemiology of insomnia in korean adults: prevalence and associated factors. J Clin Neurol. 2009;5:20–23. doi: 10.3988/jcn.2009.5.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention? JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 7.Phillips B, Mannino D. Correlates of sleep complaints in adults: the ARIC study. J Clin Sleep Med. 2005;1:277–283. [PubMed] [Google Scholar]
- 8.Kojima M, Wakai K, Kawamura T, Tamakoshi A, Aoki R, Lin Y, et al. Sleep patterns and total mortality: a 12-year follow-up study in Japan. J Epidemiol. 2000;10:87–93. doi: 10.2188/jea.10.87. [DOI] [PubMed] [Google Scholar]
- 9.Park HS, Shin HC, Kim BS, Lee KY, Choi WS, Shin JA, et al. Prevalence and associated factors metabolic syndrome among adults in primary care. J Korean Soc Study Obes. 2003;12:108–123. [Google Scholar]
- 10.Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165:863–867. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 11.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33:414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 13.Chung YC, Rhee MK, Lee YH, Park SH, Sohn CH, Hong SK, et al. A standardization study of Beak Depression Inventory 1-Korean version (K-BDI): reliability and factor analysis. Korean J Psychopathol. 1995;4:77–95. [Google Scholar]
- 14.World Health Organization; International Association for the Study of Obesity; International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment [Internet] Melbourne: Health Communications Australia; c2000. [cited 2013 Jan 17]. Available from: http://www.wpro.who.int/nutrition/documents/docs/Redefiningobesity.pdf. [Google Scholar]
- 15.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. Geneva: World Health Organization; 2001. [Google Scholar]
- 16.Morgan K, Clarke D. Risk factors for late-life insomnia in a representative general practice sample. Br J Gen Pract. 1997;47:166–169. [PMC free article] [PubMed] [Google Scholar]
- 17.Taylor DJ, Lichstein KL, Durrence HH. Insomnia as a health risk factor. Behav Sleep Med. 2003;1:227–247. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- 18.Quan SF, Katz R, Olson J, Bonekat W, Enright PL, Young T, et al. Factors associated with incidence and persistence of symptoms of disturbed sleep in an elderly cohort: the Cardiovascular Health Study. Am J Med Sci. 2005;329:163–172. doi: 10.1097/00000441-200504000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Kim JM, Stewart R, Kim SW, Yang SJ, Shin IS, Yoon JS. Insomnia, depression, and physical disorders in late life: a 2-year longitudinal community study in Koreans. Sleep. 2009;32:1221–1228. doi: 10.1093/sleep/32.9.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res. 2003;37:9–15. doi: 10.1016/s0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- 21.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment: prevalence and correlates. Arch Gen Psychiatry. 1985;42:225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- 22.Lobo LL, Tufik S. Effects of alcohol on sleep parameters of sleep-deprived healthy volunteers. Sleep. 1997;20:52–59. doi: 10.1093/sleep/20.1.52. [DOI] [PubMed] [Google Scholar]
- 23.Kaneita Y, Uchiyama M, Takemura S, Yokoyama E, Miyake T, Harano S, et al. Use of alcohol and hypnotic medication as aids to sleep among the Japanese general population. Sleep Med. 2007;8:723–732. doi: 10.1016/j.sleep.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 24.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 25.Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117:e247–e256. doi: 10.1542/peds.2004-2629. [DOI] [PubMed] [Google Scholar]
- 26.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 27.Statistics Korea. Korea Statistical Information Service [Internet] Daejeon: Statistics Korea; [cited 2013 Jan 17]. Available from: http://www.kosis.kr/ [Google Scholar]
- 28.Hasler BP, Troxel WM. Couples' nighttime sleep efficiency and concordance: evidence for bidirectional associations with daytime relationship functioning. Psychosom Med. 2010;72:794–801. doi: 10.1097/PSY.0b013e3181ecd08a. [DOI] [PMC free article] [PubMed] [Google Scholar]


