Abstract
A radicular cyst associated with carious teeth is a very common odontogenic lesion in the oral cavity, but calcifications in residual radicular cysts are quite rare. We report one such case where a routine pre-implant radiographic assessment revealed a mixed periapical radiopaque radiolucent lesion in the right maxillary central incisor region. Histological and radiographic studies show that there is a slow increase in the mineralized deposits within the cyst lumen with time. This becomes prominent histochemically in cysts more than 8 years old and radiographically 6 years later, as seen in our case. In this paper we would like to highlight the importance of a residual radicular cyst with calcifications in the differential diagnosis of a mixed periapical radiopaque radiolucent lesion.
Keywords: mixed periapical lesion, dystrophic calcifications, residual cyst, radicular cyst
Clinical presentation
A 24-year-old female reported to the Department of Oral Medicine and Radiology with a chief complaint about a missing tooth in the right maxilla near the midline for the past 3 months. She gave a history of trauma 10 years ago, owing to which the tooth had fractured and discoloured. Following repeated trauma, the tooth was extracted 3 months ago. Her medical history was non-contributory and on extraoral examination no swelling or facial asymmetry could be detected. Intraoral examination revealed a missing right central incisor with a completely healed socket. As part of a routine radiographic pre-implant assessment, an intraoral periapical radiograph (IOPA) was taken. The IOPA revealed the presence of a mixed radiopaque radiolucent lesion in the periapical region of the missing right central incisor. The lesion consisted of a diffuse radiolucency measuring about 7 × 8 mm and three discrete specks of radiopacities within the radiolucency (Figure 1).
Figure 1.
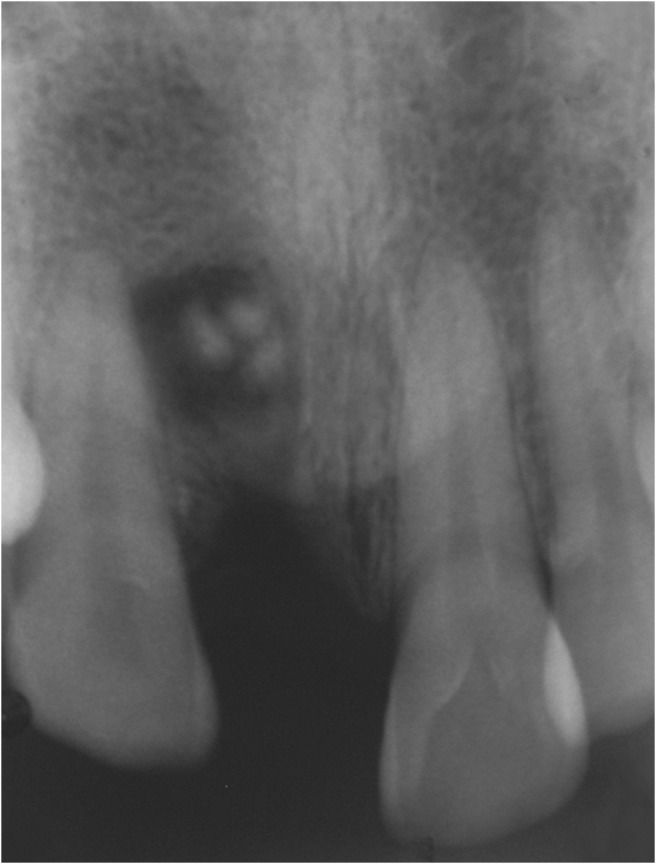
Periapical radiograph revealing mixed radiopaque radiolucent lesion in missing right maxillary central incisor region
A CT scan showed an ill-defined radiolucency about 7 × 8 mm, involving the maxilla near the root of the right central incisor with a central zone of irregular ossification and cortical discontinuity of the anterior margin of the maxilla (Figure 2).
Figure 2.
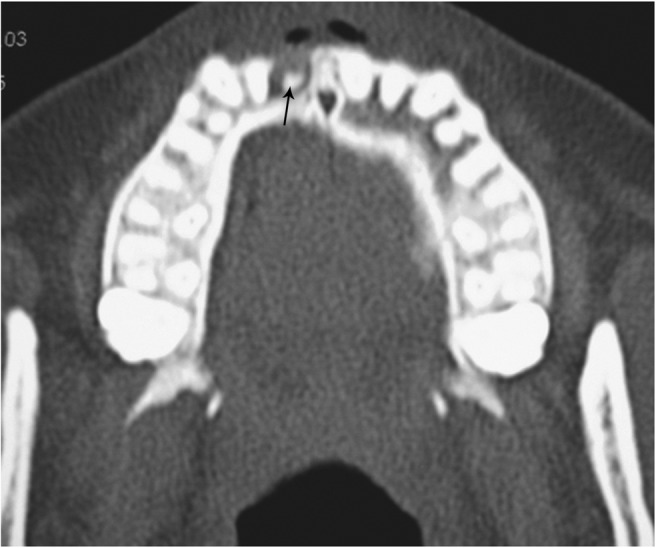
Axial section of CT scan at the level of the maxilla revealing ill-defined radiolucency with a central zone of irregular radiopacity and cortical discontinuity
Diagnosis and management
A biopsy was necessary to establish a definitive diagnosis. Considering the small size of the lesion, following informed consent, an excisional biopsy of the lesion was performed under local anaesthesia. An intraoral crevicular incision was made and mucoperiosteal flap was reflected in the right maxillary central incisor region and the lesion was removed in pieces. The surgical site was debrided and irrigated with saline. The mucoperiosteal flap was reapproximated and the surgical site was closed with 3-0 vicryl sutures.
Histopathologic examination of the biopsy specimen showed dense collagen fibres with chronic inflammatory cell infiltrate; remnants of epithelial lining appeared thin and made up of two to four layers of squamous cells. At the periphery, dystrophic calcifications were seen along with irregular bits of immature bone (Figure 3).
Figure 3.
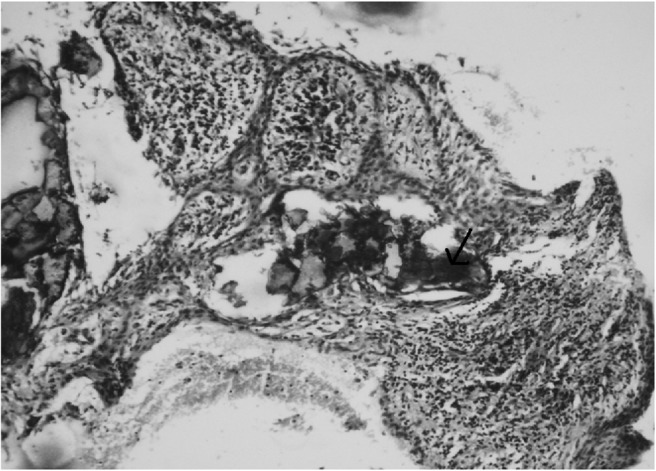
Low-power photomicrograph (10×) showing remnants of thin stratified squamous epithelial lining, about two to four layers thick with dystrophic calcifications, shown by the arrow
Histopathologic examination of the excised specimen confirmed the diagnosis of an infected residual dental cyst with dystrophic calcifications. A 3 month post-operative follow-up revealed normal healing. The patient showed no signs of recurrence over a 2 year follow-up period.
Differential diagnosis
The differential diagnosis of a localized mixed periapical radiopaque, radiolucent lesion in the anterior maxilla includes: residual cyst with calcification; odontomes; fractured root tip/impacted foreign body; intermediate stage of periapical cemento-osseous dysplasia (PCOD); adenomatoid odontogenic tumour (AOT); calcifying epithelial odontogenic tumour; focal cemento-osseous dysplasia; cemento-ossifying fibroma; cementoblastoma; and incisive canal cyst.
Ranking first in our differential diagnosis was a residual cyst with calcifications because of the association of a well-circumscribed radiolucency with a non-vital tooth which was recently extracted.1
Ranking next in our differential diagnosis was an odontome in the intermediate stage of development. Odontomas are composed of dentine and enamel in amorphous conglomeration (complex odontomas) or in rudimentary tooth-like structures (compound odontomas).2 Odontomas are usually discovered incidentally in young adults during routine radiographic examination or during investigation of a missing or displaced tooth.3 The presence of these specks of radiopacities supported this diagnosis.
Fractured root tip or an impacted foreign body surrounded by a reactive radiolucent lesion were also considered because of the associated trauma. However, it is unlikely that multiple fragments of a fractured root tip would be found in the periapical region.
AOT also deserves inclusion in the differential diagnosis because of its characteristic presentation in the anterior maxilla. AOT is the most common benign odontogenic tumour of anterior maxilla presenting in the second decade of life.2,4,5 AOT frequently shows calcifications which further favours this diagnosis.
PCOD also merits inclusion in the differential diagnosis. It starts as a periapical radiolucency that may mature over time into a circumscribed radiopacity surrounded by a radiolucent rim. It is generally asymptomatic and usually discovered on routine radiographic examination.6,7 However, approximately 70% of cases are found in close proximity to the apices of vital teeth, commonly the mandibular teeth of middle-aged women.7 The association of our case with a non-vital tooth argued somewhat against this diagnosis.
Calcifying epithelial odontogenic cyst and calcifying epithelial odontogenic tumour were also considered because of the radiographic evidence of internal calcifications, although they are more common in the posterior mandible.8,9 The absence of jaw expansion or an associated unerupted tooth were against this diagnosis.
Although an incisive canal cyst could be considered in the differential diagnosis of periapical radiolucencies in maxillary central incisor, the lesion in our case had radiopaque foci, which argued against the possibility. Focal cemento-osseous dysplasia, a condition similar to PCOD, was also considered. However, it occurs more commonly in the mandibular premolar and molar regions and the margins are not so discrete. Cemento-ossifying fibroma was considered unlikely as it is more commonly seen in the mandibular posterior region and tends to be more extensive.10 Cementoblastoma was considered highly unlikely as it occurs almost exclusively at the periapices of mandibular molars.11 Rarities such as a squamous odontogenic tumour occasionally present as anterior maxillary radiolucencies.12 It was considered highly unlikely because of the presence of the lesion in the periapical region and also the calcifications. The patient's history and the well-circumscribed character of the lesion practically ruled out the rare possibility of this being a malignancy at the periapical region.
In summary, our case involves a young adult female with a 10-year history of trauma and an asymptomatic mixed periapical lesion in the anterior maxilla associated with a recently extracted non-vital upper central incisor. Clinical and radiographic features of this case are more consistent with the diagnosis of residual cyst with calcifications, fractured root tip or foreign body, odontome or AOT.
Discussion
Residual cysts are inflammatory periodontal cysts that are periapical in position and persist after removal of the associated tooth. They represent approximately 10% of all odontogenic cysts.13,14 Panoramic radiographic studies of asymptomatic patients suggest a prevalence for residual cysts of up to 2%.15 Residual radicular cysts are slowly resolving lesions and those that persist or increase in size are more likely secondarily infected.16 These lesions can persist for long periods owing to the mechanism which prolongs the process. The squamous epithelium, because of its apparent thinness, will act as a semi-permeable membrane and also continue to shed some cellular material into the lumen. Both these mechanisms could delay resolution. Browne17 reported that most dental cysts are found in the maxillary incisor/canine region and High et al found that most of the cysts in their study were found in the mandibular premolar region, suggesting that the site of the primary lesion is important and may influence its possible persistence as an uninfected residual cyst.1
Intrinsic calcification in odontogenic cysts was first reported by Lovestadt and Bruce in 195418 and later by Browne et al in 1984.19 Molyneux studied inflammatory changes along with epithelial atrophy in residual cysts and summarized that repair followed removal of inflammatory irritant.20 Oehlers made a radiographic study of 168 presumed residual cysts, left in situ for periods up to 7 years, and concluded that most lesions resolved while a small percentage remained static and none increased in size.16 Browne et al noted mineralized deposits in odontogenic cyst aspirates by X-ray diffraction and noted a 10% incidence, but did not specify residual cyst types.19
High et al reported in their study of 33 cases that histological and radiographic study show that there is a slow increase in the mineralized deposits within the cyst lumen with time. This becomes prominent histochemically in those cysts that are more than 8 years old and radiographically 6 years later. There is also an overall decrease in cyst size with increase in cyst age. He also demonstrated the presence of dystrophic calcification in residual cyst contents.1
Dystrophic calcification refers to calcification that forms in degenerating, diseased and dead tissue despite normal serum calcium and phosphate levels. The soft tissue may be damaged by blunt trauma, inflammation, infections, soft tissue changes arising from the disease and many other causes. This calcification is usually localized to the site of injury. Dystrophic calcification is the precipitation of calcium salts into primary sites of chronic inflammation or dead and dying tissue. This process is usually associated with a high local concentration of phosphatase, an increase in local alkalinity and anoxic conditions within the inactive or devitalized tissue.21
A longstanding, chronically inflamed cyst is a common location of dystrophic calcification, as seen in our case. Dystrophic calcifications usually do not produce any signs or symptoms. The radiographic appearance of dystrophic calcification varies from barely perceptible, fine grains of radiopacities to large, irregular particles that rarely exceed 0.5 cm in diameter. One or more of these radiopacities may be seen and the calcification may be homogeneous or may contain punctate areas. The outline of the calcified area is usually irregular or indistinct.21
In conclusion, a mixed periapical radiopaque radiolucent lesion in the anterior maxilla with a missing tooth should prompt the clinician to include a residual cyst with dystrophic calcifications in the differential diagnosis.
References
- 1.High AS, Hirschmann PN. Age changes in residual radicular cysts. J Oral Pathol 1986;15:524–528 [DOI] [PubMed] [Google Scholar]
- 2.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology (2nd edn) Philadelphia: W.B. Saunders, 2002: 553–571 [Google Scholar]
- 3.Stavrou E, Tosios KI, Stavrou I. Globular radiopacity around the apex of an impacted third molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:594–598 [DOI] [PubMed] [Google Scholar]
- 4.Regezi JA, Sciubba JJ. Oral pathology: Clinical pathologic correlations (3rd edn) Philadelphia: W.B. Saunders, 1999: 339 [Google Scholar]
- 5.Olgac V, Koseoglu BG, Kasapoglu C. Adenomatoid odontogenic tumor: A report of unusual maxillary lesion. Quintessence Int 2003;34:686–688 [PubMed] [Google Scholar]
- 6.Su L, Weathers DR, Waldron CA. Distinguishing features of focal cemento-osseous dysplasias and cemento-ossifying fibromas I. A pathological spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;84:301–309 [DOI] [PubMed] [Google Scholar]
- 7.Su L, Weathers DR, Waldron CA. Distinguishing features of focal cemento-osseous dysplasia and cemento-ossifying fibromas II. A clinical and radiological spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;84:540–549 [DOI] [PubMed] [Google Scholar]
- 8.Buchner A. The central (intraosseous) calcifying odontogenic cyst: an analysis of 215 cases. J Oral Maxillofac Surg 1991;49:330339 [DOI] [PubMed] [Google Scholar]
- 9.Tanimoto K, Tomita S, Aoyama M, Furuki Y, Fujita M, Wada T. Radiographic characteristics of calcifying odontogenic cyst. Int J Oral Maxillofac Surg 1988;17:29–32 [DOI] [PubMed] [Google Scholar]
- 10.Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg 1993;51:828–835 [DOI] [PubMed] [Google Scholar]
- 11.Wood NK, Goaz PW. Differential diagnosis of oral and maxillofacial lesions (5th edn) St Louis: Mosby, 1997: 269 [Google Scholar]
- 12.Krithika C, Vardhan BG, Saraswathy K, Koteeswaran D, Sivapathasundaram B. Radiolucency in the anterior maxilla associated with an impacted tooth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:164–168 [DOI] [PubMed] [Google Scholar]
- 13.Main DM. Epithelial jaw cysts: A clinicopathological reappraisal. Br J Oral Maxillofac Surg 1970;8:114–125 [DOI] [PubMed] [Google Scholar]
- 14.Killey HC, Kay LW, Seward GR. Benign cystic lesions of the jaws, their diagnosis and treatment (3rd edn) Edinburgh: Churchill Livingstone, 1977: 169 [Google Scholar]
- 15.Perrelet LA, Bernhard DMD, Spirgi M. Panoramic radiography in the examination of edentulous patients. J Prosthet Dent 1977;37:494–498 [DOI] [PubMed] [Google Scholar]
- 16.Oehlers FA. Periapical lesions and residual dental cysts. Br J Oral Maxillofac Surg 1970;8:103–113 [DOI] [PubMed] [Google Scholar]
- 17.Browne RM. Metaplasia and degeneration in odontogenic cysts in man. J Oral Pathol 1972;1:145–158 [DOI] [PubMed] [Google Scholar]
- 18.Lovestadt SA, Bruce KW. Cysts of the incisive canal with concrements. J Oral Surg 1954;12:48. [PubMed] [Google Scholar]
- 19.Browne RM, Rowles SL, Smith AJ. Mineralized deposits in odontogenic cysts. IRCS Med Sci 1984;12:642 [Google Scholar]
- 20.Molyneux GS. Observations on the structure and growth of periodontal and residual cysts. Oral Surg 1964;18:80. [DOI] [PubMed] [Google Scholar]
- 21.White SC, Pharoah MJ. Oral radiology — Principles and interpretation (5th edn) St Louis: Mosby, 2006: 597–598 [Google Scholar]


