Abstract
Objectives
To assess the accuracy of radiographic measurements of infrabony defects and to compare the accuracy with and without individual digital adjustment of brightness and contrast.
Methods
In 41 periodontitis patients (19 females, 22 males; age range 23–73 years), 50 radiographs of 50 infrabony defects were obtained. All radiographs were digitized. Using a personal computer program, the linear distances between cemento-enamel junction (CEJ) and alveolar crest (AC) and between CEJ and bony defect (BD), and the depth of the infrabony defect (INFRA), were measured twice, according to the individual judgement of the radiographic examiner: (1) without digital adjustment (W) and (2) after use of contrast and brightness adjustment (A). Intrasurgical bone measurements served as the gold standard. The accuracy of measurements with or without digital adjustment was compared.
Results
Radiographic measurements underestimated the gold standard for CEJ-BD (W: 1.1 mm ± 1.8 mm, P < 0.001; A: 1.0 mm ± 1.9 mm, P = 0.001). Both CEJ-AC (W: 0.2 mm ± 2.5 mm; A: 0.5 mm ± 2.6 mm) and INFRA (W: −0.4 mm ± 2.4 mm; A: −0.6 mm ± 2.5 mm) measurements came close to the gold standard. Statistically significant differences between W and A regarding accuracy were not observed.
Conclusions
The measurement tool used in this study provided high-accuracy measurements of periodontal bone loss in INFRA. Individual brightness and contrast adjustment failed to improve accuracy.
Keywords: periodontitis, periodontal bone loss, radiology, diagnostic X-ray, radiographic image interpretation, computer-assisted, validity of results
Introduction
Periodontitis is the inflammatory loss of connective tissue attachment and loss of bone. Attachment loss is assessed clinically by probing the distance between the cemento-enamel junction (CEJ) or restoration margin (RM) and the most apical extension of the periodontal pocket; however, the most feasible method to assess periodontal bone loss is by obtaining vertical bitewings or periapical radiographs. Particularly for interproximal defects, radiographs provide information on the defect morphology, i.e. allow the distinction of horizontal from vertical bone loss and the estimation of the depth of the infrabony defects (INFRA). Thus, radiographs are required to identify those defects that may benefit from regenerative therapy.1-3
However, radiographic assessment tends to underestimate the amount of bone loss.1,4-10 Digital processing and manipulation of radiographic images may improve diagnostic interpretation of radiographs in terms of reliability and accuracy. Using a computer-assisted analysing system, the accuracy of linear measurements of periodontal bone loss could be improved compared with conventional methods, such as using a loupe.8 Until now, the accuracy of linear measurements of interproximal bone loss could not be improved by basic digital filtering.9,11 Even digital filters that were developed specifically to image and assess periodontal bone failed to improve accuracy.12
The more precise the radiographs, the better the presurgical judgement of the defect morphology. Improved accuracy of radiographic examination improves treatment planning and prognosis. Digital adjustment of brightness and contrast based on the individual decision of the examiner had not been evaluated before. Thus, we stated the hypothesis that digital adjustment of brightness and contrast based on individual decisions resulted in better accuracy of radiographic measurements of INFRA. The objectives of this study were to assess the accuracy of radiographic measurements of INFRA and to compare the accuracy with and without individual digital adjustment of brightness and contrast based on the individual judgement of the examiner.
Materials and methods
Patients
50 standardized radiographs depicting one INFRA each in a total of 41 patients who had undergone regenerative therapy at the Department of Periodontology, Centre of Dental, Oral and Maxillofacial Medicine (Carolinum), Goethe-University, Frankfurt, were used for analysis. The study had been approved by the Institutional Review Board for Human Studies of the Medical Faculty of the Johann Wolfgang Goethe-University Frankfurt am Main (study #157/08).
Clinical examination
As a clinical routine in defects scheduled for regenerative therapy, the probing pocket depths (PPD) and vertical attachment levels (CAL-V) were measured at six sites per tooth (mesiobuccal, buccal, distobuccal, disto-oral, oral and mesio-oral) to the nearest 0.5 mm using a straight periodontal probe (PCP UNC 15, Hu Friedy, Chicago, IL).13 The CEJ served as a reference for the CAL-V measurements. If the CEJ was destroyed by restorative treatment, the RM was used as reference.
The teeth scheduled for periodontal surgery underwent a replacement flap procedure. The root surfaces underwent thorough debridement after the complete removal of inflammatory granulation tissue. Surgery was performed by three periodontal surgeons who also performed the intrasurgical measurements. The distances between the CEJ and the alveolar crest (AC), as well as between CEJ and the most apical extension of the bony defect (BD), were measured using the above-mentioned simple manual periodontal probe. Furthermore, INFRA was measured from BD to the most coronal extension of the bony walls. If the CEJ was destroyed by restorative treatment the RM was used as reference.14,15
Radiographic examination
Standardized vertical bitewing radiographs were obtained from teeth exhibiting INFRA by modified film holders (VIP 2 Positioning, UpRad Corp., Fort Lauderdale, FL).8,16 These were done routinely in the clinical setting after anti-infective application and immediately before surgical treatment. The design of these film holders has been extensively described.8 Intraoral size 0 and 2 dental films (Insight, Eastman Kodak Co., Rochester, NY) were exposed using an X-ray source with 7 mA and 60 kVp (Heliodent DS, Sirona, Bensheim, Germany) and developed under standardized conditions (XR24pro, Dürr Dental GmbH, Bietigheim-Bissingen, Germany).
Examiner calibration and radiographic evaluation
Using 20 radiographs of INFRA unrelated to this study, the examiner was calibrated prior to evaluating the study radiographs. The principal investigator instructed and trained the examiner in locating the anatomical landmarks and measuring the respective distances. The principal investigator had already measured the 20 radiographs (measurement of distances between CEJ/RM and BD, between CEJ/RM and AC and of depth of INFRA). Measurements of both the principal investigator and the examiner were then compared. An agreement within 1 mm in 90% of all measurements should be achieved. If this agreement was not achieved all discrepancies were discussed and all measurements repeated until the desired agreement was reached. The radiographic examiner was not involved in the clinical measurements and was blinded to the clinical parameters. The examiner was a periodontal specialist with 8 years professional experience as a dentist and 5 years experience as a university teacher. The principal investigator was a periodontologist at Heidelberg and Frankfurt University and had worked as a dentist for more than 20 years.
From a bigger pool of radiographs of INFRA, 50 were selected that allowed clear identification of the anatomical landmarks and defects. All 50 radiographs were numbered from 1 to 50. While numbering the radiographs, the principal investigator of the radiographic evaluation determined the coronal landmark (CEJ or RM). Thereafter they were digitized and analysed in chronological order by one examiner who was blinded to the clinical results.2,3,16 Each radiograph was identified by its number. Each defect was characterized by its defect number, tooth number, site of defect (mesial: M; distal: D) and the coronal landmark of measurement (CEJ; RM) (e.g. 01_36 Mszg: defect 1, tooth 36, defect site mesial, landmark CEJ).
All radiographs were digitized using a computer program (SIDEXIS next Generation 1.51, Sirona, Bensheim, Germany) and a flatbed scanner (Microtek ScanMaker 4, Microtek, Hsinchu, Taiwan) with 600 dpi resolution and 8-bit grey values. The image files were stored as tagged image file format (TIFF) files and analysed by the calibrated examiner using the computer program SIDEXIS and a 19-inch flat LCD monitor (Totoku CCL 192 plus, Totoku Electric, Ueda, Japan) in the same room with no natural or artificial light.
For evaluation, the analysing tool of the program SIDEXIS was used. All image files were opened and magnified using the zoom function once. Thus, all radiographs were analysed under the same six-fold magnification. The length of the image of a wire orientated parallel to the film on the film holder was measured. The actual length of this wire was entered into the program and all subsequent measurements were adjusted automatically for any magnification (Figure 1). Afterwards the distances between CEJ/RM and AC, between CEJ/RM and BD as well as depth of INFRA were measured. In the first round of evaluation, for every second radiograph the examiner was allowed to adjust the image for brightness and contrast according to the examiner’s best judgement (Figure 1b). The degree of adjustment was documented as a percentage. In the second round of evaluation adjustment was allowed for all radiographs assigned an odd number.
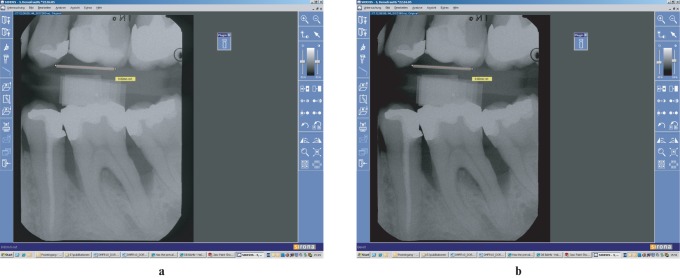
Figure 1.
Menu of Sidexis viewer with radiograph number 44. (a) After the actual length (9.8 mm) of the film holder wire has been entered. (b) After brightness (−5%) and contrast (+4%) had been adjusted
Definition of radiographic landmarks
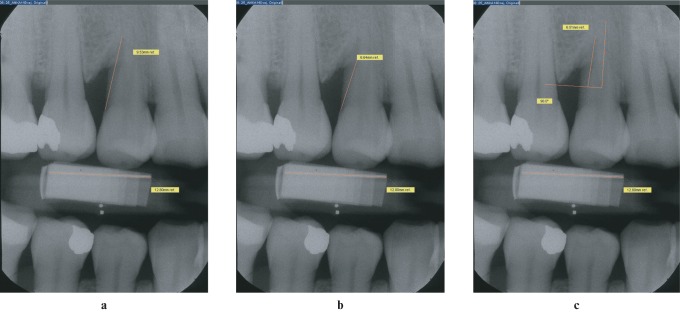
The radiographic landmarks were defined as follows: if the CEJ was destroyed by restorative treatment, the RM was taken as the coronal landmark; BD was defined as the most coronal point where the periodontal ligament space showed a continuous width (Figure 2a); if no periodontal ligament space could be identified, the point where the projection of the AC crossed the root surface was used as the landmark;17 if both structures could be identified at one defect, the point defined by the periodontal ligament was used as BD and the crossing of the silhouette of the alveolar crest with the root surface was defined as AC (Figure 2b); if several bony contours could be identified, the most apical one that crossed the root was defined as the BD and the most coronal one as AC.8 For all INFRA the distances between CEJ/RM and AC as well as between CEJ/RM and BD were measured using the measurement tool (Figure 2a,b). Using the angle tool the first leg of an angle was drawn to represent the tooth axis (Figure 2c). Then the second leg was drawn in a 90° angle to the first leg. This angle was moved along the tooth axis until the second leg ran through the most coronal margin of the intrabony defect (Figure 2c). INFRA was measured as the distance between BD and the crossing of the silhouette of the root surface and the second leg (Figure 2c).
Figure 2.
Unadjusted radiograph number 25 depicting a right first maxillary premolar with a distal infrabony defect. (a) Distance between cemento-enamel junction and bony defect: 9.53 mm. (b) distance between cemento-enamel junction and alveolar crest: 6.64 mm. (c) Infrabony defect: 6.51 mm
Statistical analysis
To show a clinically relevant mean difference of 0.25 mm between the accuracy of unadjusted and adjusted radiographs for a standard deviation of differences of 0.613 mm11 with a Type 1 error α < 0.05 and a test power of 80%, a sample of 50 radiographs was required. The main outcome variable was the accuracy of the radiographic measurements (distance between CEJ/RM and BD, distance between CEJ/RM and AC, depth of INFRA), i.e. radiographic measurements compared with the gold standard of the respective intrasurgical measurements. The differences between the intrasurgical and radiographic measurements were used as a measure for accuracy.
The sample was described by age at the time of radiographic examination (mean±standard deviation, range), sex and the number of defects that were contributed by the different patients. Further, the defects are described by PPD, CAL-V (interproximal site with most pronounced CAL-V), intrasurgical and radiographic (distance between CEJ/RM and BD, distance between CEJ/RM and AC, depth of INFRA) parameters. The distribution of defects according to jaw (maxilla/mandible) and tooth type (anterior (incisors and canines), premolars and molars) was assessed.
Accuracy of the radiographic measurements of the distances between CEJ/RM and BD, between CEJ/RM and AC, and the depth of INFRA with adjusted and unadjusted radiographic images were compared using the paired t-test or the Wilcoxon test. To detect differences in accuracy related to location of the defect in the maxilla or mandible, accuracy of the radiographic measurements of the distances between CEJ/RM and BD, between CEJ/RM and AC, and the depth of INFRA with adjusted and unadjusted radiographic images were compared using the unpaired t-test or the Mann–Whitney U-test. Statistical analysis was performed using a personal computer program (Systat™ for Windows Version 10, Systat Inc., Evanston, IL).
Results
A total of 50 standardized radiographs of INFRA originating from 41 patients were included in the analysis. The patients ranged in age from 23 to 73 years (51.7 ± 11.6 years), 19 patients were female and 22 were male. Mean PPD at the most severe site of INFRA was 8.15 mm ± 1.82 mm and mean CAL-V was 9.48 mm ± 1.91 mm. 2 patients contributed 3 INFRA, 5 contributed 2 defects and 34 patients contributed 1 defect each. The distribution of defects according to tooth type (anterior/posterior) and jaw (maxilla/mandible) is given in Table 1. 25 (50%) of all INFRA were located on the distal surface of the tooth.
Table 1. Number and distribution of examined defects according to jaw and tooth type.
| Type of tooth | Maxillary | Mandibular | Total |
| Anterior | 8 | 6 | 14 |
| Posterior | 18 | 18 | 36 |
| Total | 26 | 24 | 50 |
Both radiographic measurements underestimated the intrasurgical gold standard for the distance between CEJ/RM and BD (without adjustment (W): 1.1 mm ± 1.8 mm, P < 0.001; adjustment (A): 1.0 mm ± 1.9 mm, P = 0.001; Table 2). For the distance between CEJ/RM and AC (W: 0.2 mm ± 2.5 mm, P = 0.588; A: 0.5 mm ± 2.6 mm, P = 0.212; Table 3) and the depth of INFRA (W: −0.4 mm ± 2.4 mm, P = 0.236; A: −0.6 mm ± 2.5 mm, P = 0.110; Table 4), both measurements came close to the gold standard. However, INFRA accuracy was statistically significantly different according to the jaw for W (P = 0.025) and A (P = 0.002). While INFRA came close to the gold standard for maxillary defects, it was overestimated in the mandible (Table 4).
Table 2. Accuracy of radiographic measurements with and without brightness and contrast adjustment of the distance between cemento-enamel junction/restoration margin and most apical extension of bony defect for all defects, as well for maxillary and mandibular defects separately, and amount of adjustments.
| Intrasurgical (mm) | Radiographic without adjustment (mm) | Radiographic with adjustment (mm) | P-value |
| 10.44 ± 2.67 | 9.38 ± 2.63 | 9.47 ± 2.72 | |
| Difference to intrasurgical | 1.06 ± 1.81 | 0.97 ± 1.91 | 0.450 |
| P | <0.001 | 0.001 | |
| Maxilla | 1.05 ± 2.00 | 1.20 ± 2.00 | 0.341 |
| Mandible | 1.08 ± 1.62 | 0.72 ± 1.82 | 0.059 |
| P | 0.949 | 0.376 | |
| Adjustment | Mean/% | Increase/n | Decrease/n |
| Brightness | −1.30 ± 3.14 | 10 | 27 |
| Contrast | 3.78 ± 4.26 | 36 | 4 |
Table 3. Accuracy of radiographic measurements with and without brightness and contrast adjustment of the distance between cemento-enamel junction/restoration margin and alveolar crest for all defects, as well for maxillary and mandibular defects separately, and amount of adjustments.
| Intrasurgical (mm) | Radiographic without adjustment (mm) | Radiographic with adjustment (mm) | P-value |
| 5.04 ± 2.66 | 4.85 ± 1.79 | 4.57 ± 1.83 | |
| Difference to intrasurgical | 0.19 ± 2.53 | 0.47 ± 2.63 | 0.046 |
| P | 0.588 | 0.212 | |
| Maxilla | −0.39 ± 1.94 | −0.11 ± 2.14 | 0.136 |
| Mandible | 0.83 ± 2.96 | 1.10 ± 3.00 | 0.199 |
| P | 0.097 | 0.113 | |
| Adjustment | Mean/% | Increase/n | Decrease/n |
| Brightness | −1.12 ± 3.55 | 12 | 27 |
| Contrast | 2.68 ± 3.74 | 30 | 7 |
Table 4. Accuracy of radiographic measurements with and without brightness and contrast adjustment of the infrabony defect for all defects as well for maxillary and mandibular defects separately and amount of adjustments.
| Intrasurgical (mm) | Radiographic without adjustment (mm) | Radiographic with adjustment (mm) | P-value |
| 5.65 ± 2.72 | 6.06 ± 2.76 | 6.22 ± 2.81 | |
| Difference to intrasurgical | −0.41 ± 2.40 | −0.57 ± 2.48 | 0.236 |
| P | 0.236 | 0.110 | |
| Maxilla | 0.36 ± 0.90 | 0.51 ± 1.11 | 0.412 |
| Mandible | −1.23 ± 3.16 | −1.74 ± 3.00 | 0.010 |
| P | 0.025 | 0.002 | |
| Adjustment | Mean/% | Increase/n | Decrease/n |
| Brightness | −1.28 ± 3.15 | 11 | 27 |
| Contrast | 2.90 ± 3.75 | 33 | 5 |
Statistically significant differences between W and A regarding accuracy could only be observed for the distance between CEJ/RM and AC when analysing all defects (P = 0.046; Table 3) and for the depth of INFRA when analysing mandibular defects separately (P = 0.01; Table 4). On average the examiner chose reduction of brightness and increased contrast for adjustment of the radiographic images when assessing all three linear distances (between CEJ/RM and BD, between CEJ/RM and AC, depth of INFRA; Tables 2–4). For 41 of all 50 radiographs, the examiner chose the same adjustments for all 3 measurements. In two radiographs no adjustment was chosen at all.
Discussion
Intraoral radiographs are generally used to assess the extent of periodontal alveolar bone. However, these radiographs provide only two dimensional (2D) images of three dimensional (3D) structures. Hence, the radiographic image of interproximal bone loss may change with changing projection geometry. Additionally, evaluation of radiographs tends to underestimate the extent of alveolar bone loss compared with the gold standard of intrasurgical measurements.1,3,5-8 In some cases where 3D imaging is required (e.g. complex implant cases), cone beam volume tomography may overcome the limitations of intraoral radiographs; however, this results in higher exposure.18
Using a computer-assisted analysing system to evaluate digitized conventional radiographs, the accuracy of linear measurements of periodontal bone loss could be improved compared with measurements of the conventional radiographs using a loupe.8 Similar findings were reported when comparing computer-assisted measurements on direct digital radiographs with calliper measurements of conventional radiographs.19,20 Comparison of the interproximal distance between CEJ and AC on conventional and direct digital radiographs showed statistically significant differences depending on tooth location. However, the study did not compare radiographic measurements to a gold standard.21 It seems that the measurement tools of computer-assisted analysis of digitized or directly digitally obtained radiographs provided better sensitivity and accuracy in most cases. This may be due to higher magnification or easier on-screen viewing compared with a calliper or loupe. For the assessment of caries lesions, better accuracy had been shown for 18-fold than for 7-fold magnification.22
Digital processing and filtering of radiographic images may further enhance diagnostic interpretation of radiographs. However, the accuracy of linear measurements of interproximal bone loss could not be improved by basic digital filtering until now.9,11,20 The human eye can better discriminate between colours than between grey values. Thus, it was attempted to improve accuracy of radiographic assessments by transferring grey values into colours. However, the use of a colour-coding algorithm failed to improve accuracy of radiographic assessments of interproximal bone loss. Underestimation of bone loss ranged from 1.2 mm in canines to 2.8 mm in incisors.23 Even digital filters that had been developed to image and assess periodontal bone failed to improve the accuracy of radiographic measurements.12 The distance between CEJ and AC was slightly and statistically insignificantly overestimated by 0.35 mm to 0.68 mm. The distances between CEJ and BD and the depth of INFRA were underestimated by 0.84 mm to 1.12 mm and 0.66 mm to 0.76 mm, respectively. However, all these deviations from the intrasurgical gold standard failed to reach statistical significance.12
In earlier investigations it had been demonstrated that the underestimation of bone loss is less pronounced for the distance between CEJ/RM and AC than for the distance between CEJ/RM and BD.9,11 This tendency was confirmed in this study. However, the examiner tended to underestimate the distance between CEJ/RM and BD this time and to come quite close to the gold standard for the distances between CEJ/RM and BD as well as the depth of INFRA.
The means of all radiographic measurements reported came quite close to the results reported for computer-assisted measurements of INFRA on digitized radiographs.11,12 The differences between the radiographic measurements and the intrasurgical gold standard reported (distance between CEJ/RM and BD: W: 1.06 mm; A: 0.97 mm) are less pronounced than those reported by other working groups: distance between CEJ/RM and BD: approximately 2.0 mm,19 distance between CEJ/RM and BD: 1.5 mm to 1.7 mm.20 This is noteworthy because the present study assessed INFRA exclusively while Li et al19 measured horizontal and vertical bone loss. Jorgensen et al20 selected only radiographs of mandibular teeth to provide easy paralleling of film and teeth. However, the accuracy of measurements of the distances between CEJ/RM and BD as well as between CEJ/RM and AC was not influenced significantly by the jaw in this study. Exclusively for INFRA measurements, a statistically significant difference was found between maxillary (slight underestimation) and mandibular (clear overestimation) defects. However, the statistical significance of this difference between maxillary and mandibular defects for measurements without adjustment may be due to multiple testing. After Bonferroni correction this significance disappears. Jorgensen et al20 did not adjust the radiographic measurement for radiographic distortion and magnification. After such adjustment the differences between radiographic measurements and gold standard may have been even larger.20 In a study assessing radiographs with vertical and horizontal bone loss, underestimation of the distance between CEJ/RM and BD of 0.45 mm to 0.83 mm, depending on digital adjustment, was reported.9 It has been demonstrated before that INFRA is measured with less accuracy than horizontal bone loss.8,9
Overall, the digital brightness and contrast adjustments used in this study failed to improve accuracy of linear measurements on radiographic images compared with assessments on digitized but unmanipulated images. For the distance between CEJ/RM and AC, adjustment led to a statistically significant greater underestimation of the gold standard (P = 0.046). For INFRA measurements in mandibular defects, adjustment resulted in statistically significant greater overestimation (P = 0.01). After correction, according to multiple testing, both significances disappear. However, the conditions for computer-assisted analysis of radiographs have to be taken into account. These were high-resolution digitization and good-quality films with mostly optimal contrast. This observation has been made several times before using different modes of adjustments.9,11,12 In contrast to earlier studies that had used high-resolution dental films (D-speed), the present trial investigated modern F-speed film with less resolution. To the best of our knowledge this is the first report on computer-assisted measurements on images of digitized F-speed radiographs. Digital adjustment of radiographs cannot increase information. Digital adjustment may increase detectability of structures or landmarks by decreasing information, which may compensate for lack of quality (e.g. low contrast, under or over exposure). Thus, further work should address the evaluation of low quality radiographs.
Within the limits of the present study the following conclusions may be drawn:
The digital adjustment of brightness and contrast of digitized radiographic images used in this study failed to increase the accuracy of the radiographic assessment of alveolar bone loss regarding intrasurgical measurements.
Overall, the measurements on the digitized unmanipulated and filtered images of the radiographs came quite close to the gold standard of intrasurgical measurements. This indicates that after digitization the radiographic image can be used reliably for periodontal diagnosis.
Acknowledgments
We wish to thank Dr Almut von Schwedler, mbbs (Tas), Matcham, NSW, Australia, for her valuable and competent support in the preparation of this manuscript.
The authors declare that they have no conflict of interests. This study was funded by the authors and their institutions.
References
- 1.Tonetti MS, Pini Prato G, Williams RC, Cortellini P. Periodontal regeneration of human infrabony defects. III. Diagnostic strategies to detect bone gain. J Periodontol 1993;64:269–277 [DOI] [PubMed] [Google Scholar]
- 2.Klein F, Kim T-S, Hassfeld S, Staehle HJ, Reitmeir P, Holle R, et al. Radiographic defect depth and width for prognosis and description of periodontal healing of infrabony defects. J Periodontol 2001;72:1639–1646 [DOI] [PubMed] [Google Scholar]
- 3.Eickholz P, Hörr T, Klein F, Hassfeld S, Kim T-S. Radiographic parameters for prognosis of periodontal healing of infrabony defects: Two different definitions of defect depth. J Periodontol 2004;75:399–407 [DOI] [PubMed] [Google Scholar]
- 4.Theilade J. An evaluation of the reliability of radiographs in the measurement of bone loss in periodontal disease. J Periodontol 1960;31:143–153 [Google Scholar]
- 5.Suomi JD, Plumbo J, Barbano JP. A comparative study of radiographs and pocket measurements in periodontal disease evaluation. J Periodontol 1968;39:311–315 [DOI] [PubMed] [Google Scholar]
- 6.Shrout MK, Hildebolt CF, Vannier MW. The effect of alignment errors on bitewing-based bone loss measurements. J Clin Periodontol 1991;18:708–712 [DOI] [PubMed] [Google Scholar]
- 7.Åkesson L, Håkansson J, Rohlin M. Comparison of panoramic and intraoral radiography and pocket probing for the measurement of marginal bone level. J Clin Periodontol 1992;19:326–332 [DOI] [PubMed] [Google Scholar]
- 8.Eickholz P, Benn DK, Staehle HJ. Radiographic evaluation of bone regeneration following periodontal surgery with or without expanded polytetrafluoroethylene barriers. J Periodontol 1996;67:379–385 [DOI] [PubMed] [Google Scholar]
- 9.Eickholz P, Riess T, Lenhard M, Hassfeld S, Staehle HJ. Digital radiography of interproximal bone loss. Validity of different filters. J Clin Periodontol 1999;26:294–300 [DOI] [PubMed] [Google Scholar]
- 10.Eickholz P, Hausmann E. Accuracy of radiographic assessment of interproximal bone loss in infrabony defects using linear measurements. Eur J Oral Sci 2000;108:70–73 [DOI] [PubMed] [Google Scholar]
- 11.Wolf B, von Bethlenfalvy E, Hassfeld S, Staehle HJ, Eickholz P. Reliability of assessing interproximal bone loss by digital radiography: intrabony defects. J Clin Periodontol 2001;28:869–878 [DOI] [PubMed] [Google Scholar]
- 12.Hörr T, Kim T-S, Hassfeld S, Staehle HJ, Klein F, Eickholz P. Accuracy of assessing infrabony defects using a special digital filter for periodontal bone loss. Am J Dent 2005;18:50–56 [PubMed] [Google Scholar]
- 13.Eickholz P. The reproducibility and validity of furcation measurements as related to class of furcation invasion. J Periodontol 1995;66:984–989 [DOI] [PubMed] [Google Scholar]
- 14.Eickholz P, Krigar D-M, Kim T-S, Reitmeir P, Rawlinson A. Stability of clinical and radiographic results after guided tissue regeneration in infrabony defects. J Periodontol 2007;78:37–46 [DOI] [PubMed] [Google Scholar]
- 15.Pretzl B, Kim T-S, Steinbrenner H, Dörfer C, Himmer K, Eickholz P. Guided tissue regeneration with bioabsorbable barriers III 10 years results in infrabony defects. J Clin Periodontol 2009;36:349–356 [DOI] [PubMed] [Google Scholar]
- 16.Duckworth JE, Judy PF, Goodson JM, Socransky SS. A method for the geometric and densitometric standardisation of intraoral radiographs. J Periodontol 1983;54:435–440 [DOI] [PubMed] [Google Scholar]
- 17.Benn DK. A computer-assisted method for making linear radiographic measurements using stored regions of interest. J Clin Periodontol 1992;19:441–448 [DOI] [PubMed] [Google Scholar]
- 18.Grimard BA, Hoidal MJ, Mills MP, Mellonig JT, Nummikoski PV, Mealey BL. Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J Periodontol 2009;80:48–55 [DOI] [PubMed] [Google Scholar]
- 19.Li G, Engström P-E, Nasström K, Lü ZY, Sanderink G, Welander U. Marginal bone levels measured in film and digital radiographs corrected for attenuation and visual response: an in vivo study. Dentomaxillofacial Radiol 2007;36:7–11 [DOI] [PubMed] [Google Scholar]
- 20.Jorgensen T, Masood F, Beckerley JM, Burgin C, Parker DE. Comparison of two imaging modalities: F-speed film and digital images for detection of osseous defects in patients with interdental vertical bone defects. Dentomaxillofac Radiol 2007;36:500–505 [DOI] [PubMed] [Google Scholar]
- 21.Khocht A, Janal M, Harasty L, Chang K-M. Comparison of direct digital and conventional intraoral radiographs in detecting alveolar bone loss. J Am Dent Assoc 2003;134:1468–1475 [DOI] [PubMed] [Google Scholar]
- 22.Eickholz P, Kolb I, Lenhard M, Hassfeld S, Staehle HJ. Digital radiography of interproximal caries: effect of different filters. Caries Res 1999;33:234–241 [DOI] [PubMed] [Google Scholar]
- 23.Li G, Engström P-E, Welander U. Measurement accuracy of marginal bone level in digital radiographs with and without color coding. Acta Odontol Scand 2007;65:254–258 [DOI] [PubMed] [Google Scholar]