Abstract
Objectives
The purpose of the study was to compare the image generated by a classic panoramic machine equipped with a cadmium telluride sensor capable of digital tomosynthesis and special software with images produced by other popular panoramic X-ray machines using a charge-coupled device and native software for image capture.
Methods
Panoramic images were made using a phantom of a human skull on Planmeca ProMax, Planmeca EC Proline, Kodak 8000 and PC-1000. With the last machine we used the PanoACT® software to adjust the entire arch and to adjust the image in selected regions of interest (ROIs). Ten viewers evaluated the images and provided the viewer data. ANOVA for repeated measures was used to compare the means by pairwise comparisons of means.
Results
The image of the entire arch adjusted by the PanoACT® software was statistically superior to the images produced by other machines. The images generated and individually adjusted by PanoACT® were statistically superior to all other images.
Conclusions
The image generated by the cadmium telluride sensor has great potential and can be processed to create superior images to those taken with other machines. Furthermore, the ROI individual images enhanced by the PanoACT® were superior to the entire arch adjusted by the same software.
Keywords: tomography, X-ray computed, radiography, dental, diagnostic imaging
Introduction
Most digital panoramic X-ray machines use charge-coupled device (CCD) detectors to capture images, which emulate film-based systems for panoramic radiography. This is accomplished by controlling the movement of the CCD charge carriers so that their speed is matched to the speed of the X-ray shadows of objects within the central plane of the image layer. This method, which is directly analogous to the formation of a film-based panoramic image, is described in a patent held by Siemens AG.1 Like conventional film-based panoramic systems, once a CCD-based digital image is produced it is not possible to modify the image layer. If a patient has been incorrectly positioned, a retake may be required, after repositioning the patient, to achieve a satisfactory image.2
An alternative technique, which can be used with narrow two-dimensional (2D) detectors, is digital tomosynthesis of a panoramic image by overlapping and adding a sequential set of frames acquired at regular intervals throughout the scan.3 To achieve this effect it is necessary to use a detector that can acquire a large number of high-resolution images during the course of the X-ray exposure cycle. One detector that meets this requirement is the SCAN 300FP, manufactured by Ajat Oy (Helsinki, Finland), a Finnish company that provides several high-speed 2D X-ray cameras for industrial purposes. This sensor, designed specifically for dental panoramic radiography, uses a cadmium telluride (CdTe) layer for X-ray capture combined with a readout system based on complementary metal oxide semiconductor (CMOS) technology. This CdTe-CMOS technology captures 300 frames per second during the panoramic excursion, resulting in a large number of high-resolution frames (64 × 1510 pixels per frame). Each pixel is square and measures 100 microns on each side.4 The frames are subsequently overlapped and superimposed to produce a panoramic image using the technique of digital tomosynthesis. By changing the degree of overlap in different portions of the image, the layer can be shaped to meet the requirements of panoramic imaging. This is comparable to altering the speed of the film relative to the beam in a conventional system for panoramic radiography, but with this new method it occurs after the data have been acquired. Since the layer is selected by digital image processing, the same frames can be combined in many ways to produce a variety of layer shapes or to move the layer inward or outward should a shift in focus be required. In addition, the image layer can be fitted to correct for the axial inclination of the teeth.
The PC-1000 (Panoramic Corporation, Ft Wayne, IN) is a panoramic X-ray machine that has achieved widespread popularity. The PC-1000 has recently been fitted with the SCAN 300FP sensor.
PanoACT® (AXION Corporation, Tokyo, Japan) is an alternative to the standard software provided with the SCAN 300FP sensor. The software allows the operator to shift the position of the entire layer inward or outward as needed for diagnosis; to select individual regions of interest (ROIs) that resemble periapical images and are located anywhere throughout the dental arch; and to individually adjust the focal depth and tilt of these ROIs (pan periapicals) as required. With this method, a full mouth intraoral survey (FMX) and a panoramic image can be generated from a single panoramic scan with a 3–5 times reduction in the radiation dose compared with digital 20-image FMX.5
The purpose of the present study was to compare the image quality of the digital PC-1000 panoramic machine equipped with the SCAN 300 FP sensor using the PanoACT® software with that of other popular panoramic X-ray machines using their native software for image capture.
Materials and methods
A digital PC-1000 unit was installed at the Dental School of the University of Texas Health Science Center at San Antonio (UTHSCA) and provided with the PanoACT® software and SCAN 300 FP CdTe sensor. Panoramic exposures were made using a 3M phantom consisting of a human skull and cervical spine encased in tissue-equivalent acrylic. The skull is completely dentate; however, the mouth area cannot be opened as the area is sealed by the tissue-equivalent acrylic. The phantom is fitted with hardware so that it may be attached to a tripod and positioned in the panoramic machine. Images were constructed with the PanoACT® software using both available options (processing the entire dental arch and processing selected ROIs). Radiographs of the phantom were also made using the Planmeca ProMax (Planmeca Oy, Helsinki, Finland), the Planmeca EC Proline and the Kodak 8000 (Kodak Dental Systems, Rochester, NY) panoramic machines.
This resulted in a total of five modalities:
Planmeca ProMax;
Planmeca EC Proline;
Kodak 8000;
PC-1000 with PanoACT® software used to adjust the entire arch; and
PC-1000 with PanoACT® software used to adjust the image in selected ROIs.
The 11 anatomical structures designated as ROIs were as follows: sites 1 and 11 consisted of the visualization of a narrow root canal space in the maxillary right second molar and in the mandibular left central incisor, respectively. These sites were selected as the structures may be difficult to fully visualize, especially on panoramic radiographs, if they are being assessed for root canal treatment. Visualization may also be difficult because of the superimposition of anatomical structures such as the zygomatic arch or maxillary sinus.6 Sites 2 and 3 consisted of a vertical crack in the crowns of the maxillary right and left central incisors, respectively. These sites were selected as cracked teeth may represent a difficult diagnostic challenge for dental practitioners. The localization of pain and the visualization of cracks may sometimes be difficult clinically, and to confirm on intraoral and panoramic images.7 Site 4 consisted of the distal lamina dura of the mandibular left second premolar. This site was selected because subtle lamina dura changes can be seen in periodontitis, which is a common condition, as well as in less common disorders such as fibrous dysplasia, Paget's disease,8 hyperparathyroidism, renal osteodystrophy,9 osteopetrosis and socket sclerosis.10 Sites 5 and 7 consisted of the mesial periodontal ligament (PDL) space of the mandibular left first premolar and the apical PDL space and lamina dura of the mandibular right first premolar, respectively. These sites were selected as they are often affected in diseases such as malignant metastatic disorders, gingival carcinoma, scleroderma, orthodontic tooth movement and ankylosis.11,12 The lamina dura and PDL space may be slightly enlarged or more prominent in hyperocclusion. The earliest changes occurring in abscess formation are seen as a widening of the apical PDL space and resorption of the lamina dura. Some of these problems may be painless, and the diagnosis is made serendipitously upon reviewing the panoramic radiograph.13 Site 6 consisted of an area of the bony floor of the maxillary sinus in the left maxillary premolar region. This site was selected as primary disorders of the maxillary sinus may result in regional odontalgia; conversely, dental and periodontal infections can cause sinus infections producing symptoms such as headache and odontalgia. One of the most significant structures affected by these processes is the thin bony floor of the sinus. Changes can include resorptive, additive and remodelling of the bony sinus floor.14 Sites 8, 9 and 10 consisted of the apical portion of a mandibular central incisor root, the apical half of the root outline and root canal space of the mandibular left lateral incisor, and a maxillary left first premolar root, respectively. These sites were selected as apical regions of teeth, which are important in the diagnosis of an abscess developing from advanced pulp disease.15 Other disorders, such as in focal cemento-osseous dysplasia and periapical cemental dysplasia, produce similar changes in this region. These are seen on vital teeth and do not require root canal therapy. Also, the orthodontic movement of teeth can cause resorption of the apices of teeth, an important sign of excessive orthodontic forces being applied to the teeth.16
In summary, the selected ROIs represent structures that must be visualized for common diagnoses made in the dental office. (Figure 1) The reason for selecting this sample of ROIs is to create the maximum challenge for the panoramic equipment or its accompanying software to better visualize these structures. In further clinical studies involving actual patients it will be necessary to see if such improved visualization of structures (if any) will be diagnostically significant.
Figure 1.
11 regions of interest selected and enhanced with PanAct® software
The images were captured and exported from the native software of each machine without any compression and viewed using Microsoft Image Viewer (Microsoft Corporation, Redmond, WA) on a flat panel monitor (Dell 1707 with a dot pitch of 0.264 mm and a maximum resolution of 1280 × 1024/75 Hz, Dell Inc. Austin, Tx).
Ten viewers were chosen from the departments of Dental Diagnostic Science, General Dentistry and Periodontics to evaluate the panoramic images and provide the viewer data for the study. Viewers were asked to examine images representing the five modalities under optimal conditions for viewing digital images. The same computer was used throughout the study. The monitor brightness and contrast were not altered throughout the viewing sessions. All viewing was done in a quiet room with reduced illumination. Each reader attended an initial orientation session to become familiar with his or her task and with the different techniques. A standardized answer sheet was provided to the viewers, who were instructed to examine the 11 specific ROIs on the images from each of the 5 modalities. The ROIs to be studied were not selected randomly but were chosen based on their importance in making common dental diagnoses as related to every-day dental patient problems and complaints in the dental office. For each examined area viewers were asked to rate their confidence level of the decision using the following scale: 1, not seen; 2, difficult to see; 3, can be seen; 4, good visualization; and 5, excellent visualization. These five choices were typed on the viewer answer sheet for easy reference throughout the viewing sessions. 10 answer sheets were generated, and on each one 11 ROIs were evaluated for each of the 5 modalities. Altogether, 550 data were analysed.
Since the scores are expressed as an ordered scale from 1 to 5, they may not be normally distributed. However, when comparing modalities and/or locations the data were averaged over 11 locations and 10 raters, or 5 modalities and 10 raters. The means are more normally distributed and the residuals from an ANOVA for repeated measures were expected to be nearly normally distributed as well.
ANOVA for repeated measures was used with factors for modality (5 modalities) and ROIs (11 clinically important areas) and their interaction. Each effect was tested against its interaction with the random effect of raters (sample of 10 raters). Pairs of means were tested using the least significant difference with the appropriate error term for each pair of means tested. Residuals from the model were plotted to examine their distribution and homogeneity of variance at different predicted values (Table 1).
Table 1. ANOVA table.
| Source of variation | df | SS | MS | F | P-value |
| Modality | 4 | 145.5 | 36.4 | 26.6 | <0.0001 |
| E1: reader* modality | 36 | 49.3 | 1.4 | ||
| AOI | 10 | 160.7 | 16.1 | 10.9 | <0.0001 |
| E2: reader* ROI | 90 | 133.2 | 1.5 | ||
| Modality* ROI | 40 | 222.6 | 5.6 | 12.4 | <0.0001 |
| E3: reader* modality* ROI | 360 | 161.3 | 0.4 |
E1, the error variance term for testing modality differences; E2, the error variance term for testing ROI differences; E3, the error variance term for testing modality*ROI interaction; df, degrees of freedom; SS, sum of squares; MS, mean squared deviations
Results
The means over the 10 raters for machines and locations varied from 1.0 to 4.7, indicating a good range of evaluations for these locations and modalities.
The five modalities were significantly different overall (F(5, 45) = 23.08, P < 0.0001). The mean ratings for the modalities were 2.82, 2.55, 2.40, 3.32 and 3.75, respectively (Figure 2). Modalities 2 and 3 were not significantly different in mean ratings overall. Modalities 3 and 1 were different (P < 0.01), with Modality 1 better. Modality 4 was significantly different from all other modalities (better than Modalities 1–3 and not as good as Modality 5) in overall mean score (P < 0.007), as was Modality 5 (P < 0.007). Modality 5 was statistically superior to all other modalities (Figure 2).
Figure 2.
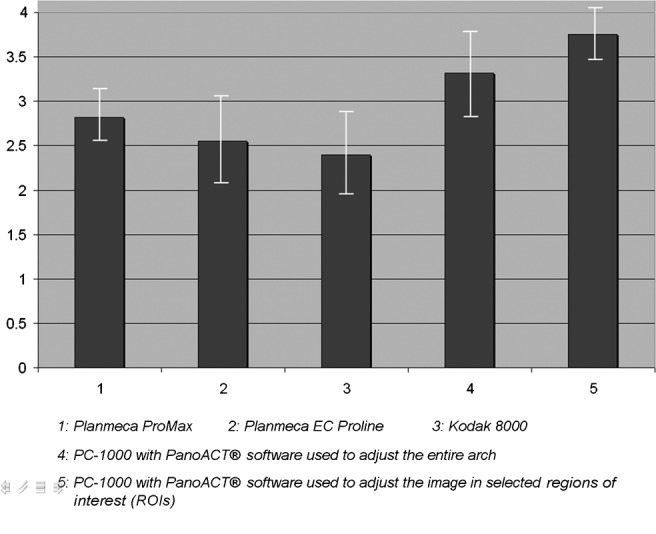
Mean ratings with standard deviation for all modalities. X-axis represents the five modalities; y-axis is the average score of each modality
The magnitude of comparison of the modalities varied slightly over the 11 locations (F(50, 450) = 10.44, P < 0.0001). Details of this variability are given in Figure 3. The figure numbers correspond to the ROIs defined in the Materials and Methods section. While Modalities 4 and 5 were not always the highest at each ROI, one can see from the graphs that they were generally among the highest at each site and therefore were superior over all sites, on average.
Figure 3.
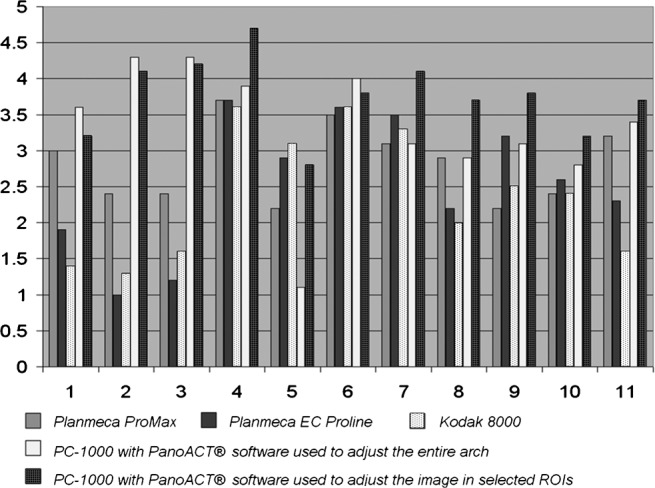
Mean score for each modality in evaluating the 11 regions of interest (ROIs); X-axis represents the 11 ROIs; y-axis is the average score of each machine per ROI
Discussion
The design of the PC-1000, which has been stable over a number of years, is that of the older generation of panoramic machines developed before the adoption of direct current X-ray generators, programmable stepper motors and digital sensors. In spite of this older design, the PC-1000 images acquired with the Axion PanoACT® software and Ajat sensor were statistically superior to all of the more advanced and more expensive machines in the comparison test.
PanoACT® software, which can be used to modify the entire image, can also be used to process individual ROIs resembling periapical images in size and quality. For the points of comparison used in this study, the software-treated ROIs were rated statistically superior even to the whole arch option. This means that the practitioner can obtain a panoramic image as usual, but with superior image quality; individual ROIs can then be processed and exported from the original panoramic scan and further details sought by probing and tilting the layer. No other panoramic imaging system permits this capability. The reader is reminded that this is regular panoramic equipment and not related in any way to cone beam CT machines, which have a pan configuration and can also generate standard digital panoramic images. When compared with digital intraoral radiography, this new technology means far less infection control supplies, procedures and disinfection time, less potential for delicate sensor damage, less time to acquire the image(s), less patient discomfort, less radiation than a 16- to 20- image full mouth survey and potentially more diagnostic information than previous systems. Of course, intraoral radiography will still be needed on occasion, for example in endodontic procedures. In addition, this technology cannot correct for the overlap of the interproximal surfaces in the premolar region.
References
- 1.Pfeiffer J, Guenther W, Muether M, Heubeck E. Dental X-ray diagnostics installation for producing panorama slice exposures of the jaw of a patient. US Patent No. 4878234. [Google Scholar]
- 2.McDavid WD, Welander U, Dove B, Tronje G. Digital imaging in rotational panoramic radiography. Dentomaxillofac Radiol 1995;24:68–75 [DOI] [PubMed] [Google Scholar]
- 3.Guenther W, Muether M, Heubeck E, Doebert M, Werner L. Dental X-ray diagnostics installation for producing panorama slice exposures of the jaw of a patient. US Patent No. 4823369. [Google Scholar]
- 4.Internet publication http://www.ajat.fi/index.php. [Google Scholar]
- 5.Underhill TE, Chilvarquer I, Kimura K, Langlais RP, McDavid WD, Preece JW, et al. Radiobiologic risk estimation from dental radiology. Part I. Absorbed doses to critical organs. Oral Surg Oral Med Oral Pathol 1988;66:111–120 [DOI] [PubMed] [Google Scholar]
- 6.Kim-Park MA, Baughan LW, Hartwell GR. Working length determination in palatal roots of maxillary molars. J Endod 2003;29:58–61 [DOI] [PubMed] [Google Scholar]
- 7.White SC, Pharoah MJ. Oral radiology, principles and interpretation, 5th edn. St Louis: Mosby; 2004: 623 [Google Scholar]
- 8.Theodorou SJ, Theodorou DJ, Sartoris DJ. Imaging characteristics of neoplasms and other lesions of the jawbones Part 2. Odontogenic tumor-mimickers and tumor-like lesions. Clinical Imaging 2007;31:120–126 [DOI] [PubMed] [Google Scholar]
- 9.Asaumi J, Aiga H, Hisatomi M, Shigehara H, Kishi K. Advanced imaging in renal osteodystrophy of the oral and maxillofacial region. Dentomaxillofac Radiol 2001;30:59–62 [DOI] [PubMed] [Google Scholar]
- 10.Petrikowski CG, Pharoah MJ, Lee L, Grace MG. Radiographic differentiation of osteogenic sarcoma, osteomyelitis, and fibrous dysplasia of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80:744–750 [DOI] [PubMed] [Google Scholar]
- 11.Auluck A, Pai KM, Shetty C, Shenoi SD. Mandibular resorption in progressive systemic sclerosis: a report of three cases. Dentomaxillofac Radiol 2005;34:384–386 [DOI] [PubMed] [Google Scholar]
- 12.Soares Ade J, Gomes BP, Zaia AA, Ferraz CC, de Souza-Filho FJ. Relationship between clinical-radiographic evaluation and outcome of teeth replantation. Dent Traumatol 2008;24:183–188 [DOI] [PubMed] [Google Scholar]
- 13.Noujeim M, Prihoda TJ, Langlais R, Nummikoski P. Evaluation of high-resolution cone beam computed tomography in the detection of simulated interradicular bone lesions. Dentomaxillofac Radiol 2009;38:156–162 [DOI] [PubMed] [Google Scholar]
- 14.Sharan A, Madjar D. Maxillary sinus pneumatization following extractions: a radiographic study. Int J Oral Maxillofac Implants 2008;23:48–56 [PubMed] [Google Scholar]
- 15.Willershausen B, Kasaj A, Röhrig B, Marroquin BB. Radiographic investigation of frequency and location of root canal curvatures in human mandibular anterior incisors in vitro. J Endod 2008;34:152–156 [DOI] [PubMed] [Google Scholar]
- 16.Lv T, Kang N, Wang C, Han X, Chen Y, Bai D. Biologic response of rapid tooth movement with periodontal ligament distraction. Am J Orthod Dentofacial Orthop 2009;136:401–411 [DOI] [PubMed] [Google Scholar]



