Abstract
Diabetic population is more than 245 million worldwide and expected to be b380 million by 2025. One of the main causes of increasing rate of diabetes is stress and tension in day-to-day life, disturbing the homeostasis of positive and negative emotions to initiate pathophysiology of stress-induced diabetes. In the present study, in Group A of 34 patients, a herbo-mineral compound containing Shuddha Shilajatu, Shuddha Guggulu, Vijayasara Ghana, Saptarangi Ghana, and Triphala Ghana was administered in the dose of 3 gm/day in three divided doses with luke-warm water before meal for the duration of 8 weeks, which significantly relieved symptoms (60.52%) like Prabhuta Mutrata (54.55%), Avila Mutrata (66.67%), Daurbalya (61.36%), Shrama (59.32%), etc. with fasting blood sugar (4.05%) and postprandial blood sugar (9.95%). In another series of 34 patients (Group B), where psychological health promoting drug Shankhapushpi was administered in the dose of 1.5 gm/day in three divided doses for 8 weeks along with herbo-mineral compound. The percentage relief was found to be more better on symptoms (71.13%) like Prabhuta Mutrata (76.92%), Avila Mutrata (83.33%), Daurbalya (75%), Shrama (70.37%), fasting blood sugar (18.04%) and postprandial blood sugar (27.75%). Group B showed better results on psychological parameters like disturbed Manasabhava (29.16%) and Brief Psychiatry Rating Scale (38.28%). The high significance of χ2 (15.50) on overall effect of therapy indicated better results in group B.
Keywords: Herbo-mineral compound, Medhya Rasayana, psychological factors, Shankshapushpi, Type-II diabetes mellitus
Introduction
The dawn of the new millennium is witnessing an unprecedented spread of diabetes in every corner of the globe. Since 1985, the number of people with diabetes worldwide has grown from 30 million to 285 million. It is estimated that 3.5 million people die due to diabetes or its complications annually.[1] While diabetes continues to spread rapidly in the United States and Europe, its impact on the developing world is even more profound and devastating. The World Diabetes Foundation expects 80% of new cases of diabetes to emerge in the developing world due to stressful and sedentary lifestyle as a result of rapid modernization. 90-95% of diabetics have type-II diabetes.[2]
Modern medical science had a spectacular achievement in the control of blood glucose of diabetics; still high risk exists due to its several side effects. The psychological problems associated with diabetes are treated with long-term use of sedatives and anxiolytic drugs which may lead to hazardous effects on psychological health and produce drowsiness, impair motor functions, loss of memory, nonsocial behavior, etc. Moreover, these drugs produce drug dependency and drug resistance. Therefore, it is need of the hour to think from the Ayurvedic point of view for a better management of mental health in diabetes mellitus (DM).
Type-II diabetes can be covered under Avaranajanya Madhumeha described in Ayurveda. In the pathogenesis of Madhumeha, provoked Vata excretes the Dhatus and Ojas with Mutra (urine) from Mutravaha Sotas, involving Medodhatvagni and Meda, Mamsa, Rasa, Kleda, etc.[3] A herbo-mineral compound (HMC) containing Shuddha Shilajatu (Asphaltum punjabinum), Shuddha Guggulu (Commiphora wightii Arn.), Ghana (water-soluble extract) of Triphala (three myrobalan), Vijayasara (Pterocarpus marsupium Roxb.), and Saptarangi (Casearia esculenta Roxb.) and Saptarangi (Casearia esculenta Roxb.) was selected to evaluate the efficacy in type-II DM patients. The ingredients of compound not only have antihyperglycemic effect, but also correct the vitiated Dosha, Dushya, Dhatvagni, and Srotas, along with Rasayana (rejuvination) properties to compensate Dhatukshayatmaka and Ojokshayatmaka effects of the disease.[4]
It is well established that disturbed psychological factors affect the development and progression of type-II DM being a psychosomatic disorder. So, to alleviate worry, sorrow, anger, anxiety, fear, etc., the Medhya Rasayana (MR)-Shankhapushpi[5] (Convolvulus pluricaulis Choisy.) was administered along with HMC to see how far it is capable of potentiating the antidiabetic effect of HMC by counteracting the stress and improving the mental health of diabetic patients.
Materials and Methods
Total 93 patients of type-II diabetes, attending the OPD/IPD of Institute for Post Graduate Teaching and Research in Ayurveda Hospital, Jamnagar, whose blood glucose level was found high and fulfilled the criteria of selection, were randomly distributed in two therapeutic groups.
Group A
HMC was administered to 48 patients in a dose of 3 g/day in three divided doses in pill form for the duration of 8 weeks with lukewarm water before meal.
Preparation of HMC
Ghana (aqueous extract) of Triphala, heart wood of Vijayasara, and roots of Saptarangi, were prepared by following classical guidelines. Shuddha Shilajatu and Shuddha Guggulu in equal proportion was mixed to the Ghana and 500 mg pills were prepared. Ghana (aqueous extract) of Triphala fruits, Vijayasara heart wood, and Saptarangi root were prepared by following classical guidelines; mixed with Shuddha Shilajatu and Shuddha Guggulu in equal proportion and 500 mg pills were prepared.
Group B
HMC as above with MR-Shankhapushpi in a dose of 1.5 g/day in three divided doses was administered to 45 patients for 8 weeks (HMC + MR).
Preparation of MR
To augment the potency, seven Bhavana of Shankhapuspi Swarasa (juice) were given to Churna (powder) of its Panchanga (whole plant) and 500 mg capsules were filled.
Follow-up
After completion of therapy, patients were advised to visit OPD every week for follow-up up to 1 month, and as per the need, routine O.P.D. treatment was given to them.
Inclusion criteria
The new patients fulfilling the diagnostic criteria of World Health Organization for DM described as under were selected:[6]
Symptoms of DM and random blood glucose b200 mg/dl or
Fasting blood glucose b126 mg/dl or
Postprandial (PP) blood glucose b200 mg/dl at an interval of first 2 h during an oral glucose tolerance test.
Criteria for high blood glucose: The diagnosed patients who were taking allopathic medicine but their blood glucose was not under control were included.[7]
Fasting blood glucose b6.0 mmol/l (b108 mg/dl)
2-h PP blood glucose b8.0 mmol/l (b144 mg/dl)
A detailed proforma covering all signs and symptoms of type-II diabetes, supported with positive and negative Manasabhava and Brief Psychiatry Rating Scale (BPRS) was prepared to study the disturbed psychological factors from Ayurvedic as well as modern point of view.
Exclusion criteria
Patients of type-I diabetes.
Endocrinopathies like acromegaly, Cushing’s syndrome, hyperthyroidism, etc.
Drug or chemical (glucocorticoids, thiazides, etc.) induced DM.
Certain genetic syndromes associated with diabetes, e.g., Down’s syndrome, Turner’s syndrome, etc.
Associated with complications like nephropathy, ketoacidosis, etc.
Investigations
Biochemical investigations like routine hematological investigations to rule out pathological conditions, blood sugar (fasting and PP) for the present state of disease, lipid profile [serum cholesterol, serum triglyceride, High Density Lipoprotein (HDL), Low Density Lipoprotein (LDL), Very Low Density Lipoprotein (VLDL)] to evaluate the Dushti of Meda, blood urea and serum creatinine to assess the functional status of kidney, and examination of urine were conducted wherever possible.
Criteria for assessment
-
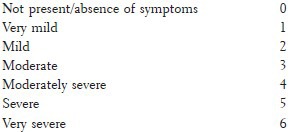
To assess the relief in all symptoms, disturbed Manasabhava and parameters of BPRS were scored depending upon their severity in the following manner before and after the treatment.
Biochemical parameters were investigated before and after the treatment to assess the improvement.
-
The overall effect was assessed on the basis of relief in symptoms, decrease in raised blood sugar level, improvement on disturbed Manasabhava and BPRS. Each criterion has been given equal importance. Thus, the total effect of therapy was marked as:
Control of disease: Fasting blood sugar (FBS) and postprandial blood sugar (PPBS) coming down to normal limits, with 80% and above improvement in overall effect of therapy
Markedly improved: Patient showed improvement between 60% and <80%.
Moderately improved: Improvement between 40% and <60%.
Improved: Improvement between 20% and <40%.
Unchanged: No relief or improvement was less than 20%, was taken as unchanged.
To calculate χ2, the adopted criterion for improvement is equal to or more than 40% of relief from the initial value.
Results and Observations
In group A out of 48 registered patients, 34 had completed the treatment, whereas in group B out of 45 registered patients, 34 had completed therapy.
In group A, highly significant relief was obtained in Prabhuta Mutrata (polyuria), Kshudhadhikya (polyphagia), Trishadhikya (polydipsia), Kara-Pada Tala Suptata (numbness in palm-foot sole), Atisweda (excess sweating), Daurbalya (weakness), and Shrama (fatigue), and significant relief was obtained in Kara-Pada Tala Daha (burning sensation in palm-foot sole), Gala Talu Shosha (dryness of mouth), and Pindikodvestana (leg cramps), while Bhara Hani (loss of weight) got insignificantly relieved. Whereas in group B, highly significant improvement was obtained in Prabhuta Mutrata, Avila Mutrata (turbid urine), Kshudhadhikya, Trishadhikya, Kara-Pada Tala Daha, Kara-Pada Tala Suptata, Atisweda, Gala Talu Shosha, Daurbalya, Shrama, Pindikodvestana, and Bhara Hani, with better percentage achieved in relief [Table 1].
Table 1.
Effect on symptoms of type-II diabetics
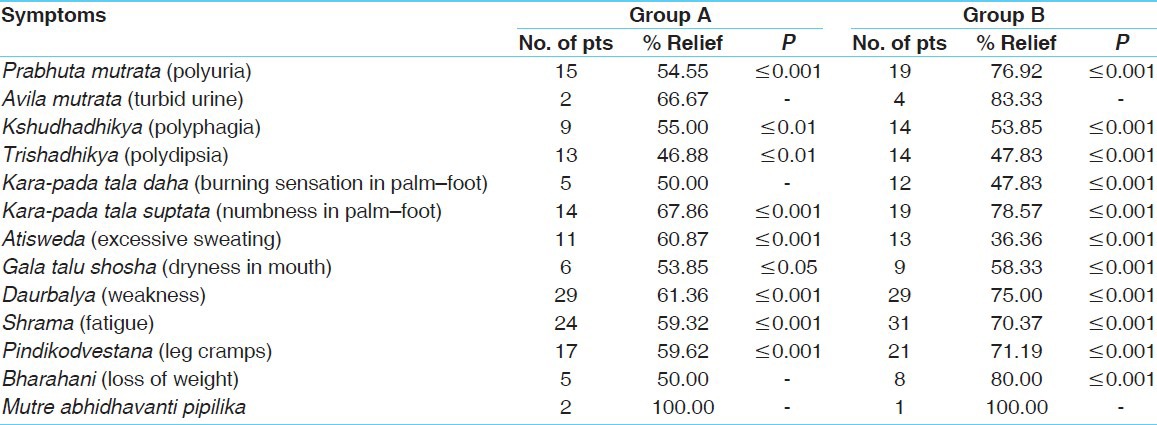
In general, 60.52% in group A reported relief in all the symptoms, whereas in group B better relief (71.13%) was obtained.
On positive Manasabhava, insignificant improvement was recorded in Harsha (cheerfulness) and Avasthana (stability) in Group A. Whereas in Group B, highly significant improvement was recorded in Harsha, Priti (happiness), Dhairya (fearlessness), and Avasthana. Significant improvement was obtained in Virya (beginning of work) and Shraddha (good attitude), while insignificant improvement was recorded in Dhriti (good control) [Table 2].
Table 2.
Effect on disturbed positive Manasabhava
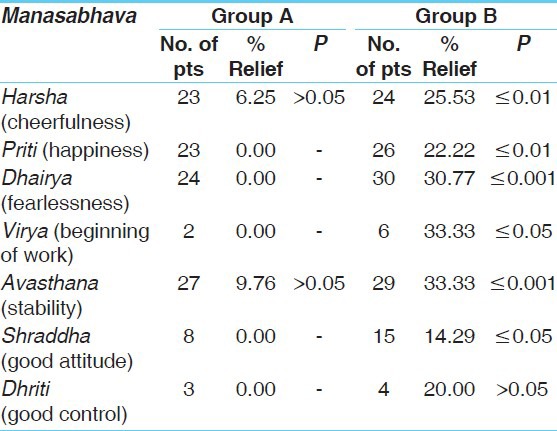
On negative Manasabhava, highly significant decrease was noted in Chinta (worry), Chittodvega (anxiety), and Upadhi (impact). Significant relief obtained in Krodha (anger) and Bhaya (fear), while Shoka (sorrow), Dvesha, Moha, Raga (attachment), and Udvega were insignificantly relieved in group A. Whereas highly significant decrease was observed in Chinta, Vishada, Krodha, Shoka, Bhaya, Upadhi, Udvega, and Chittodvega, while Mana and Raga were insignificantly improved in group B [Table 3].
Table 3.
Effect on disturbed negative Manasabhava
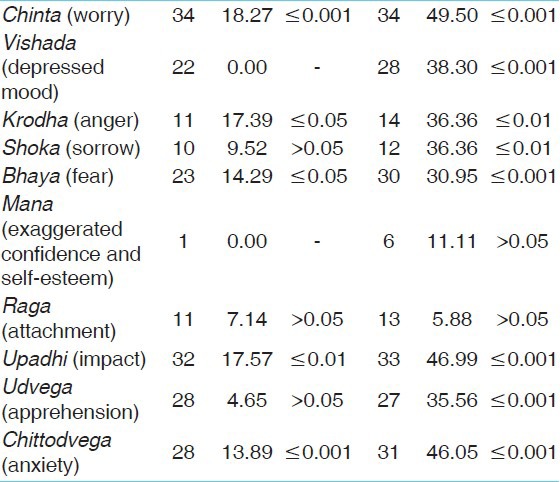
On all disturbed Manasabhavas, Group A demonstrated only 8.27% improvement, whereas Group B demonstrated 29.16% improvement.
On BPRS, Group A showed highly significant relief in fear of physical illness of somatic concern, worry and fear of anxiety, tension, and unusual thought content. Over concern for present or future of anxiety and thought process confusions of conceptual disorganization were significantly reduced. Where as Group B therapy showed highly significant relief in fear of physical illness of somatic concern; worry, fear, and over concern for present or future of anxiety; thought process confusions of conceptual disorganization; overactivation and tension; slow motor retardation; unusual thought content; and heightened emotional tone and increased reactivity of excitement. Strange thought content, reduced emotional tone, and reduction in normal intensity of feelings of blunted affect were significantly reduced [Table 4].
Table 4.
Effect on brief psychiatric rating scale
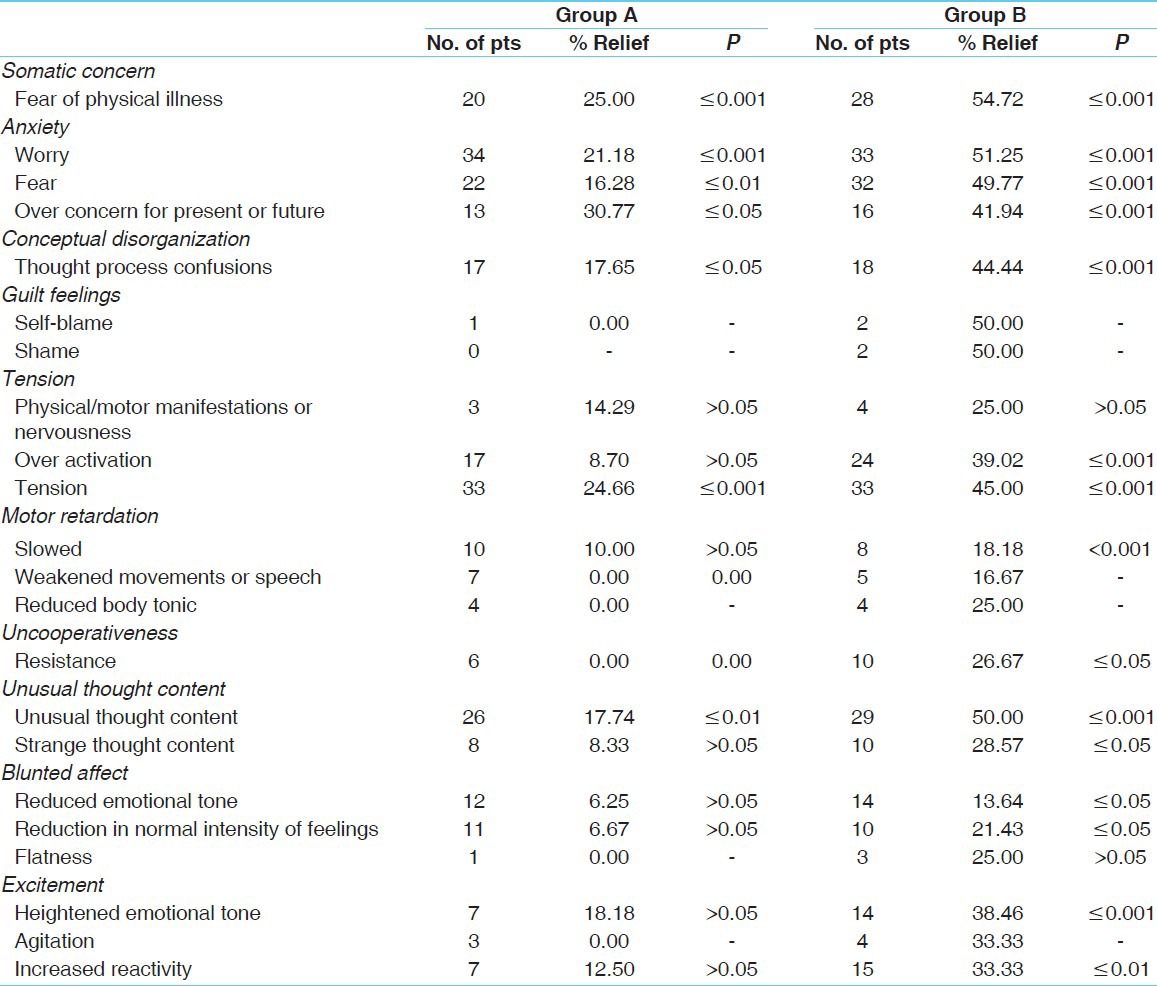
In all the parameters of BPRS, group A showed 14.59% relief while group B showed 38.28% relief.
In the hematological investigations, in both therapeutic groups, hemoglobin was insignificantly increased and erythrocyte sedimentation rate (ESR) was reduced insignificantly. In the lipid profile, serum triglyceride and VLDL were significantly decreased and serum cholesterol was insignificantly reduced, while HDL was insignificantly improved in Group A. In Group B, serum cholesterol and LDL were significantly decreased and serum triglyceride and VLDL reduced insignificantly, while HDL insignificantly increased. In the renal profile, serum creatinine and blood urea were increased in group A, whereas in group B serum creatinine was increased but blood urea was insignificantly decreased [Table 5].
Table 5.
Effect on biochemical investigations
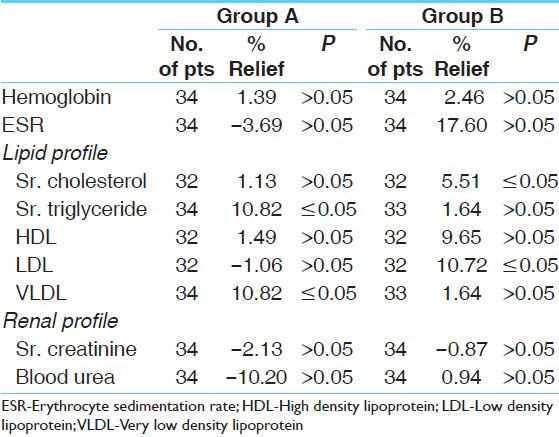
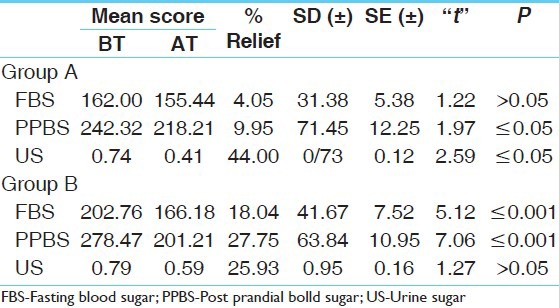
PPBS and urine sugar were significantly decreased and FBS was insignificantly reduced in Group A, whereas in Group B, FBS and PPBS were highly significantly decreased and urine sugar was insignificantly decreased with better percentage relief [Table 6].
Table 6.
Effect on blood sugar and urine sugar
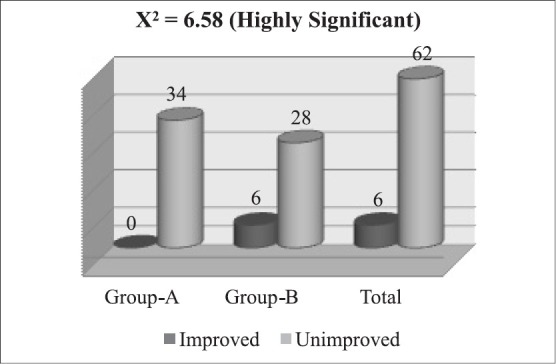
Comparing the effects of both therapies on all symptoms with the statistical parameter χ2 , the result was found to be highly significant (11.96) [Figure 1]. χ2 on all disturbed Manasabhavas was significant (6.58) [Figure 2]. Comparing the efficacies of both groups on BPRS, the effect of Group B was found to be significantly better on χ2 (6.35) [Figure 3].
Figure 1.
Comparison of therapies on symptoms with X2
Figure 2.
Comparison of therapies on Manasabhava with X2
Figure 3.
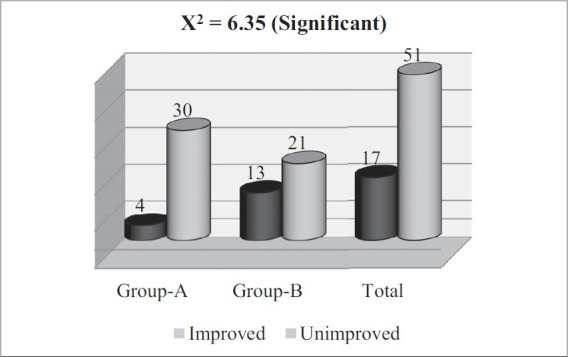
Comparison of therapies on BPRS with X2
On comparison of efficacy in lowering the high blood sugar, the Group B was found to be better with high significance of χ2 (9.68) [Figure 4].
Figure 4.
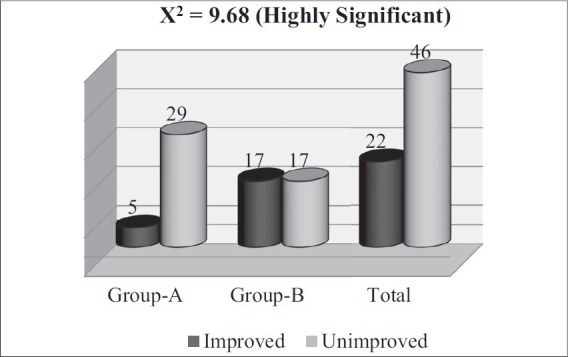
Comparison of therapies on blood sugar with X2
Analysing the overall effect of therapy, 8.82% patients markedly improved, 38.24% moderately improved, 26.47% improved, and 26.47% patients remained unchanged in the Group A. Whereas in Group B, 32.35% patients markedly improved, 58.82% moderately improved, 8.82% improved, and none remained unchanged [Figure 5].
Figure 5.
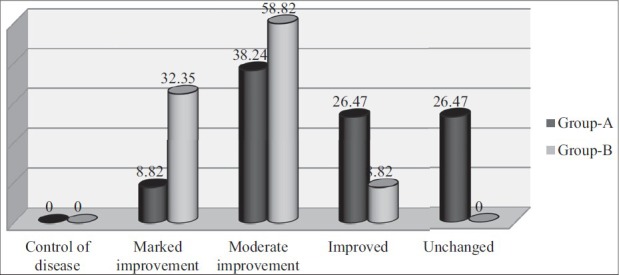
Over all effect of therapy
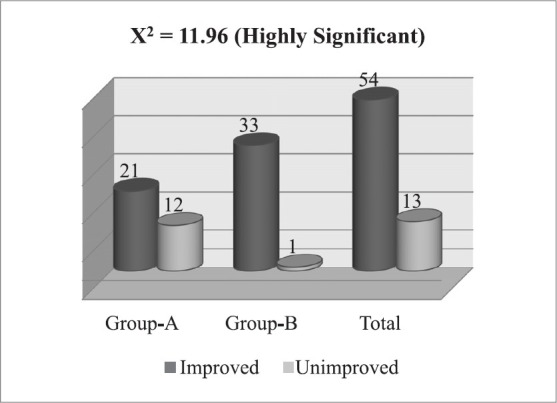
On comparison of overall therapeutic efficacy, only 16 patients of Group A showed improvement, whereas 31 patients in Group B improved, which illustrates that Group B was more effective with highly significant χ2 (15.50) [Figure 6].
Figure 6.
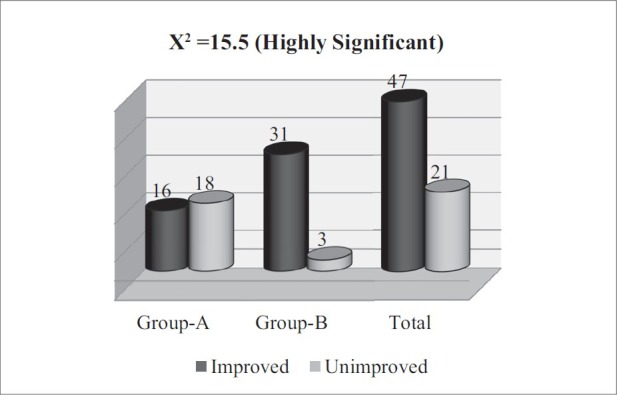
Comparison of therapies on over all effect with X2
Discussion
The HMC is able to correct provoked Dosha, vitiated Dushya, hampered Agni, and affected Srotas involved in the pathophysiology of type-II DM by its potent ingredients. Shilajatu with its Tikta Rasa (bitter taste), Katu Vipaka, and Lekhana property decreases excess of Kapha and Meda, as well has a curative effect on disease of Mutravaha Srotas.[8] Guggulu with its Tikta-Katu Rasa and Ushna Virya reduces increased Meda and Kapha and pacifies Vata. Triphala with its Kashaya Rasa, Laghu-Ruksha property causes a decline in excess of Sharira Kleda, Vasa, and Meda.[9] Vijaysara with its Tikta-Katu-Kashaya Rasa and Laghu-Ruksha property diminishes excessive Kapha,[10] and Saptarangi with its Kashaya-Tikta Rasa and Laghu-Ruksha property not only decreases Kapha and Pitta, but also improves Rakta.[11] The Rasayana effect of Shilajatu, Guggulu, and Triphala improves all Dhatus and provides relief in Dhatukshayatva and Ojokshayatva of disease.[12] Hence, significant relief was obtained with HMC. Diabetes, being a psychosomatic disease, both Sharirika and Manasika Dosha are vitiated and affect each other mutually[13] as sorrow and fear provoke Vata and anger provokes Pitta.[14] Medhya drug calms the mind and normalizes vitiated Manasa Dosha, which subsequently improves vitiation of Sharirika Dosha and related symptoms. Therefore, MR-Shankhapushpi, when added to principal therapy HMC, provided better relief in symptoms with highly significant result on χ2 (11.96).
The root cause of disturbance of psychological factors is various types of Ichchha, i.e., desire, and Dvesha, i.e., hatred.[15] When one cannot get the desired thing or one gets unwanted thing, it produces stress,[16] causing disturbance of positive psychological and negative psychological factors leading to vitiation of Raja and Tama. Due to these, Manasa Vikaras are produced.[17] When Shankhapushpi with proven stress relieving psychotropic effect in experimental rats[18,19] was administered, it improved the disturbed psychological factors and re-established the balance of Rajas and Tamas. That’s why, HMC + MR therapy (29.16%) was significantly better than single administration of HMC (8.27%) on χ2 (6.58) to improve disturbed Manasabhava.
The pharmacological studies proved that Shankhapushpi enhances neuropeptide synthesis in the brain. Moreover, it reduces the level of acetylcholine and catecholamine in the brain tissue,[20] which are elevated because of disturbed psychological factors. This way Shankhapushpi as an MR provides psycho-stimulant and psycho-tranquilizer effects in animal experiments.[21] In clinical study also, it had shown significant anxiety relieving results.[22] That’s why when Shankhapushpi was administered along with HMC, better results (χ2 = 6.35) were obtained in BPRS adopted for evaluating the improvement in psychological factors.
Hemoglobin and ESR were within normal limits in both the groups before treatment and remained normal after completion of therapy. The slight increase noted in hemoglobin was due to hemoglobin increasing effect of Amalaki[23] and Shilajatu.[24] The ESR came down slightly due to anti-infective activities of Guggulu.[25]
In diabetic patients of both therapeutic groups, the mean scores of lipid profile were within the physiological range. Also, most of the patients had normal lipid profile before and after treatment. Therefore, it was obvious to obtain insignificant results for lipid profile in both the groups, although positive effect was noticed in those diabetic patients whose lipid profile was abnormally high. The contents of HMC-Triphala,[26] Shilajatu,[27] and Guggulu[28] -have Medohara/antihyperlipidemic effect. That’s why antihyperlipidemic action was seen in the present study. Similarly in the renal profile, the mean scores of serum creatinine and blood urea were increased or decreased within their physiological range by therapy.
The main diagnostic object of diabetes is elevated blood sugar, which came down by clinically proven ingredients of HMC. Shilajatu is effective in controlling the blood glucose level by its fulvic acid.[26] Oral administration of the extracts of Triphala significantly reduced the blood sugar level in normal and in alloxan diabetic rats.[29] Pterostilbene, marsupsin, and epicatechin present in the bark of Vijaysara are reported to significantly lower the blood glucose and reverse the damage of β-cells.[30,31] Saptarangi showed potent antihyperglycemic effects.[32] The impulses of disturbed psychological factors release epinephrine and norepinephrine, which increase glycogenolysis and lipolysis. Furthermore, stress and tension increases the level of neurotransmitters like catecholamines, epinephrine and norepinephrine, which work as an insulin antagonist.[33] When mental health promoting MR was administered together with HMC to normalize the disturbed psychological factors, it takes better care of neuroendocrine changes related to insulin antagonism.[33] Therefore, HMC + MR showed better relief on high blood sugar (χ2 = 9.68).
In nutshell, HMC improved the symptoms and elevated blood sugar, but it did not have significant effect on disturbed Manasabhava-induced pathophysiology of Madhumeha. So, when Shankhapushpi, having Medhakrita, Medhya, Smruti Vardhak, and Manasarogahara effects,[34,35] was administered along with the antidiabetic HMC, it showed better improvement in the overall health including relief in symptoms (group A = 60.52%, group B = 71.13%), decrease in high blood sugar (group A = 4.48%, group B = 21.13%), and improvement in mental health based on BPRS (group A = 14.59%, group B = 38.28%) and Manasabhava (group A = 8.27%, group B = 29.16%).
On overall effect of therapy, more patients showed marked (group A = 8.82%, group B =32.35%) or moderate improvement (group A = 38.24%, group B =58.82%), whereas less patients were under the category of unchanged (group A = 26.47%, group B = 00%) or improved (group A = 32.35%, group B = 8.82%) in HMC + MR-Shankhapushpi group. Furthermore, it was proved by statistical parameter χ2 (15.50) with a high significance, which showed that combined therapy improved the patients in a more pronounced manner.
Conclusion
Stress plays an important role in the etiopathogenesis of type-II DM, which is well comparable to Avaranajanya Madhumeha. Though the disease is Tridoshik in nature, in the initial stage there is dominancy of Kapha (Bahudrava Sleshma) followed by Pitta and Vata in association with Dushya at various levels. All these changes lead to hyperglycemia, imbalance lipid profile with high level of catecholamine and other insulin antagonists. The trial drug HMC has antipyperglycemic/hypoglycemic and hypolipidemic properties is a drug of choice for Samprapti Vighatana of disease. Simultaneous administration of Medhya drug like Shankhapushpi has further potentiated the therapeutic efficacy of the principal antidiabetic compound by counteracting stress and due to its antioxidant and immunomodulatory properties.
References
- 1.Worlddiabetesfoundation.org [Diabetes facts] 4th edition. Lyngby, Denmark: The World Diabetes Foundation, Source: IDF, Diabetes Atlas; [Last updated on 2010 May 02 by bisl.wdf; cited September 04]. Available from http://wwwworlddiabetesfoundationorg/composite-35htm . [Google Scholar]
- 2.E-News letter of American Diabetes Association. Nov, Original Source: IDF Diabetes Atlas. 2nd and 3rd edition. 2007. Professional Edition, American Diabetes Association. [Updated on 2006 Nov]
- 3.Agnivesha . Charaka Dridhabala, Charaka samhita, Sutra Sthana, Kiyantahshirseeyo Adhyaya, 17/78-80. reprint ed 2000. [Google Scholar]; Jadavaji Vaidya, Aacharya Trikamji, Prakashana Chaukhamba Surbharati. Varanasi: p. 103. [Google Scholar]
- 4.Chakrapanidutta . Commnetator. Charaka Samhita, Nidana Sthana, Prameha Nidana Adhyaya, 4/38-46. Varanasi: Chaukhamba Surbharati Prakashana; 2000. p. 215. [Google Scholar]
- 5.Agnivesha . Charaka, Dridhabala, Charaka samhita, Chikitsa Sthana, Rasayana Adhyaya, Karprachiteeyo Rasayanapada, 1-3/31. reprint ed 2000. [Google Scholar]; Vaidya Jadavaji, Aacharya Trikamji. Varanasi: Chaukhamba Surbharati Prakashana; p. 385. [Google Scholar]
- 6.Diabetes Mellitus Chapter: 323 by Alvin C. Powers. Harrision’s principles of internal medicine. 16th ed 2005. [Google Scholar]; Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. New York: McGraw-Hill Medical Publishing Division; p. 2153. [Google Scholar]
- 7.http://www.diabetes.ca. [Clinical Practice Guidelines] Canada: Canadian Diabetes Association; 2008. [Retrieved 2008 July 19]. Available from http://www.diabetes.ca/cpg2003/chapters.aspx.htm . [Google Scholar]
- 8.Bhava Prakasha. Bhava Prakasha Nighantu, Purvakhanda, Shilajatu. 1963 [Google Scholar]; Shastri GM. Ahmedabad: Sastu Sahitya Mudranalaya; p. 592. [Google Scholar]
- 9.Ibidem. Bhava Prakasha Nighantu, Guggulu. pp. 245–47.
- 10.Ibidem. Bhava Prakasha Nighantu, Vijaysara. p. 349.
- 11.Ibidem. Bhava Prakasha Nighantu, Saptarangi. p. 686.
- 12.Agnivesha, Charaka, Dridhabala . Charaka samhita, Chikitsa Sthana, Rasayana Adhyaya, Karprachiteeyo Rasayanapada, 1-3/6,31,64,65. reprint ed 2000. [Google Scholar]; Vaidya Jadavaji, Aacharya Trikamji. Varanasi: Chaukhamba Surbharati Prakashana; pp. 384–86. [Google Scholar]
- 13.Ibidem. Charaka Samhita, Sharira Sthana, Garbhavkranti Sharira. 4(36):323. [Google Scholar]
- 14.Ibidem. Charaka Samhita, Chikitsa Sthana, Jwara Chikitsa. 3(115):407. [Google Scholar]
- 15.Jadavaji Trikamaji Acharya. Dalhana Commnetator, Sushruta Samhita, Chaukhambha Surbharti Prakashana, Varanasi. Purvardha Sutra Sthana, Vedana Adhyaya, 2008;1(4):6. [Google Scholar]
- 16.Agnivesha . Charaka, Dridhabala, Charaka samhita, Sutra Sthana, Tistraishaneeya Adhyay, 11/45. reprint ed 2000. [Google Scholar]; Vaidya Jadavaji, Trikamji Aacharya. Varanasi: Chaukhamba Surbharati Prakashana; p. 76. [Google Scholar]
- 17.Ibidem. Charaka Samhita, Vimana Sthana, Roganeekam Vimana. 6(5):254. [Google Scholar]
- 18.Khare CP. Indian Herbal Therapy. 2nd ed. Delhi: Vishv Vijay Publication; 2003. p. 87. [Google Scholar]
- 19.Dandekar UP, Chandra RS, Dalvi SS, Joshi MV, Gokhale PC, Sharma AV, et al. Analysis of clinically important interaction between phenytoin and Shankhapushpi, an Ayurvedic preparation. J Ethnopharmacol. 1992;35:285–88. doi: 10.1016/0378-8741(92)90026-n. [DOI] [PubMed] [Google Scholar]
- 20.Bihaqi SW, Sharma M, Singh AP, Tiwari M. Neuroprotective role of Convolvulus pluricaulis on aluminium induced neurotoxicity in rat brain. J Ethnopharmacol. 2009;124:409–15. doi: 10.1016/j.jep.2009.05.038. Available from: http://wwwsciencedirectcom/science_ob=ArticleURL and_udi=a. [cited 2009 July 30] [DOI] [PubMed] [Google Scholar]
- 21.Bhowmik D, Sampath Kumar KP, Paswan S, Srivatava S, Yadav A, Dutta A. Traditional Indian herbs Convolvulus pluricaulis and its medicinal importance. J Pharmacogn Phytochem. 2012;1:50. [Google Scholar]
- 22.Parsaniya S, Singh G. I.P.G.T. and R.A., G.A.U. Jamnagar: 2001. A clinical study on the role of Jaladhara and Sankhapuspi (Convolvulus Puricaulis Chois) in the management of Chittodvega (Anxiety Disorders)-MD (Ayu.) [Google Scholar]
- 23.Khan KH. Role of Emblica officinalis in Medicine - A Review. Bot Res Int. 2009;2:218–28. [Google Scholar]
- 24.Goel RK, Banerjee RS, Acharya SB. Antiulcerogenic and antiinflammatory Studies with Shilajit. J Ethnopharmacol. 1990;29:95–103. doi: 10.1016/0378-8741(90)90102-y. [DOI] [PubMed] [Google Scholar]
- 25.Saeed MA, Sabie AW. Antibacterial activities of some constituents from oleo-gum-resin of Commiphora mukul. Filoterpia. 2004;75:204–8. doi: 10.1016/j.fitote.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Modak M, Dixit P, Londhe J, Ghaskadbi S, Paul A Devasagayam T. Indian herbs and herbal drugs used for the treatment of diabetes. J Clin Biochem Nutr. 2007;40:163–73. doi: 10.3164/jcbn.40.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nair R, Chanda SV. Antibacterial activities of some medicinal plants of the western region of India. Turk J Biol. 2007;31:231–4. [Google Scholar]
- 28.Kuppurajan K, Rajagopalan SS, Rao TK, Sitaraman R. Effect of guggulu (Commiphora mukul--Engl.) on serum lipids in obese, hypercholesterolemic and hyperlipemic cases. J Assoc Physicians India. 1978;26:367–73. [PubMed] [Google Scholar]
- 29.Dobrowolski JW, Vohora SB, Sharma K, Shah SA, Naqvi SA, Dandiya PC. Antibacterial, antifungal, antiamoebic, antiinflammatory and antipyretic studies on propolis bee products. J Ethnopharmacol. 1991;35:77–82. doi: 10.1016/0378-8741(91)90135-z. [DOI] [PubMed] [Google Scholar]
- 30.Ahmad F, Khalid P, Khan MM, Chaubey M, Rastogi AK, Kidwai JR. Hypoglycemie activity of Pterocarpus marsupium wood. J Ethnopharmacol. 1991;35:71–5. doi: 10.1016/0378-8741(91)90134-y. [DOI] [PubMed] [Google Scholar]
- 31.Grover JK, Yadav S, Vats V. Hypoglycemic and antihyperglycemic effect of Brassica juncea diet and their effect on hepatic glycogen content and the key enzymes of carbohydrate metabolism. Mol Cell Biochem. 2002;241:95–101. doi: 10.1023/a:1020814709118. [DOI] [PubMed] [Google Scholar]
- 32.Yoshikawa M, Morikawa T, Matsuda H, Tanabe G, Muraoka O. Absolute stereostructure of potent alpha-glucosidase inhibitor, Salacinol, with unique thiosugar sulfonium sulfate inner salt structure from Salacia reticulata. Bioorg Med Chem. 2002;10:1547–54. doi: 10.1016/s0968-0896(01)00422-9. [DOI] [PubMed] [Google Scholar]
- 33.E-news latter from: www.mendosa.com , update-102, how diabetes works stress and DM. [Last accessed on 2007 Jan]. Available from http://www.mendosa.com/diabetes_update_102.htm .
- 34.Prakasha B, Nighantu BP. Purvakhanda, Shankhapushpi. 1963. [Google Scholar]; Shastri G.M. Ahmedabad: Sastu Sahitya Mudranalaya; p. 327. [Google Scholar]
- 35.Sharma PV, Vijnana Dravya Guna. Shankhapushpi, Chaukhamba Bharati Akadami. Varanasi: BHU; 1990. pp. 9–10. [Google Scholar]


