Abstract
To evaluate comparative efficacy of Samshodhana and Samshamana Chikitsa, the current study is planned in 24 patients of Tamaka Shwasa. Thirteen patients (Group A) were treated with Samshodhana, particularly with Virechana Karma. The patients of this group received Abhyantara Snehana with Tila Taila followed by Bahya Snehana with Tila Taila and Saindhava Lavana. After observations of proper signs of Snehana; Virechana Karma was performed with Aragvadha Phala Majja. Samsarjana Krama was followed for five days. Subsequently all the patients were given the trial drug (powder of Badara). The patients of group B, were treated only with the powder of dried ripe fruits of Badara. In both groups, the dose of Badara powder was 5 g, twice a day, with luke warm water, for a period of 60 days. In group A, maximum number of patients (61.45 %) showed good response, while in group B, 45.45 % patients showed good response. No side effects were observed during the clinical trial. Based on the observations, it was concluded that, group A is more effective than group B.
Keywords: Aragvadha Phala Majja, Badara Phala Majja, Bronchial Asthma, Tamaka Shwasa, Virechana Karma
Introduction
Tamaka Shwasa is a type of Shwasa Roga (respiratory disease) affecting the Pranavaha Srotas and characterized by Pratiloma Vayu (prolonged expiration), Ghurghuraka (wheeze), Ativa Tivra Vagam Ca Shwasam Pranaprapidakam (dyspnoea of exceedingly deep velocity, which was immensely injurious to life) and so on.[1, 2] Tamaka Shwasa, in Ayurvedic classics seems to be identical with the description of bronchial asthma in modern medicine. Bronchial asthma is a major global health problem, which can affect the population irrespective of age, sex, economical status, etc. At present, asthma is reported in 1.2 – 6.3 % adults in most countries.[3] About 300 million people worldwide suffering from asthma and the number has risen by around 50 % in the last decade.[4] There are only a few studies from India on epidemiology of asthma. Overall burden of asthma in India is estimated to be more than 15 million patients.[4] Five percent of children under 11 years have asthma in India.[5] Asthma was diagnosed in 2.28, 1.69, 2.05 and 3.47 % respondents, respectively, at Chandigarh, Delhi, Kanpur and Bangalore with an overall prevalence of 2.38 %.[6]
A number of drugs are available in modern system of medicine to counter this condition, but are known to develop various adverse drug reactions. Considering these reactions, the suffering population is searching certain traditional remedies for better relief that are comparatively safe in nature. Ayurveda can provide promising results in Tamaka Shwasa through a set of treatment modalities. Shodhana and Shamana are some of such modalities. Currently, an attempt has been made to evaluate comparative efficacy of Shodhana and Shamana Chikitsa in case of Tamaka Shwasa.
Materials and Methods
Patients fulfilling the criteria of Tamaka Shwasa (Bronchial Asthma) were registered in the clinical study, irrespective of sex and religion from the Outpatient Department of Kayachikitsa at S.V.S.P hospital attached to the I.P.G.A.E and R, Kolkata.
Inclusion criteria
Age: Patients between 17 to 70 years of age.
Presence of features of Tamaka Shwasa.
Patients not taking any other medicines for Tamaka Shwasa.
Exclusion criteria
Patients suffering from major disorders like hypertension, cardiac asthma, tropical pulmonary eosinophilia, acute and chronic bronchitis, bronchiectasis, spontaneous pneumothorax, complicated bronchial asthma, drug dependent cases and pregnant women were excluded from the study.
Criteria for diagnosis
A detailed history and physical examination was done on the basis of the standard proforma, which included both Ayurvedic and modern methods of examination: Agnibala, Dehabala, Prakriti were recorded. For selection of the patients the diagnosis was based on subjective criteria and objective criteria as follows:
A. Subjective criteria: Presence of symptoms[1] of Tamaka Shwasa. The symptoms were based on textual references like Pratiloma Vayu (prolonged expiration), Ghurghuraka (wheeze), Ativa Tivra Vegam Ca Shwasam Pranaprapidakam (dyspnea of exceedingly deep velocity, which was immensely injurious to life), Shlesmanyamucyamane Tu Bhrsam Bhavati Duhkhita (as the phlegm does not come out, the patient became more restless), Uddhvamsate Kantha (choked throat), Asino Labhate Saukhyam (comfortable in orthopnea position), Tasyaiva Ca Vimoksante Muhurtam Labhata Sukham (patient found momentary relief after the expulsion of phlegm), Shayanah Shwasapiditah (patient had more dyspnea when lying down), Ruksa Bhasana (hoarseness of voice).
B. Objective criteria: As objective criteria, the following investigations were carried out –
(a) Blood: Total leucocytes count, differential leucocyte count, hemoglobin percentage, Erythrocyte Sedimentation Rate (ESR), (b) Stool: Routine microscopic examination of the stool., (c) Urine: Routine urine examination, (d) Radiological examination: X-ray of the chest, (e) Pulmonary Function Tests: (i) Breath Holding Time and (ii) Peak Expiratory Flow Rate.
Plan of study: Total 24 patients have been enrolled in the trial and were divided into two groups viz Samshodhana and Samshamana (Group A) and Samshamana (Group B).
(A) 13 Patients in group A, received Samshodhana therapy (Virechana Karma). Snehana (oleation therapy) with Tila Taila in increasing dose (1st day – 40 ml, 2nd day – 80 ml, 3rd day – 120 ml, 4th day – 160 ml and 5th day – 200 ml) was administered to produce the optimum Snehana effects. The duration of intake of Snehapana in all cases was five days. On the 5th day the features of proper oleation were observed. Along with internal oleation, external oleation of the patients was done with Til Taila added with Saindhava Lavana particularly over the chest and back was done.
After observing the features of appropriate oleation like Snigdha Tvaka (smoothness of the skin), Snigdha Purisha (oleous motion) and Utklesha (nausea); Svedana was followed for two days. For Svedana (fomentation), patients were advised to wrap 6 to 10 blankets till perspiration is observed. After observation of the features of proper Snehana and Svedana, the patients were considered ready for the Virechana Karma. On the next day at 9 a.m. (Kaphakala Atigame), the patients were given decoction of Aragvadha Phala Majja on empty stomach for Virechana Karma. Samsarjana Karma was followed for five days for all the 13 patients. Thereafter, dried ripe fruits of Badara were administered in powder form to all the patients, in a dose of 5 g, orally, twice a day, morning and evening after breakfast with luke warm water for a period of 60 days.
11 patients in group B received 5 g of dried fruit pulp of Badara, in powder form, orally, twice a day, morning and evening after breakfast with luke warm water for a period of 60 days.
Criteria for assessment
The improvement in the patients was assessed mainly on the basis of relief in the signs and symptoms of the disease. To assess the effect of therapy objectively, all the signs and symptoms were given a score depending on their severity. Objective parameters like Breath Holding Time (BHT) and, Peak Expiratory Flow Rate (PEFR) were also considered for assessment. The signs and symptoms were recorded from the first day of treatment and then at every 14-day intervals, during the course of treatment. Gradations of the symptoms were made depending on the severity.
Total effect of therapy
Excellent response: The patients were included in the excellent result group when they showed complete relief in the clinical signs and symptoms as well as improvement in investigations.
Good response: The patients were included in the good response group when their clinical features improved more than 50 percent and the investigations like BHT, PEFR, TLC and ESR were improved moderately.
Poor response: The patients were included in the poor response group when the improvement in their signs and symptoms was less than 50 percent, with negligible improvement or no improvement in the investigations like BHT, PEFR, TLC and ESR.
Statistical analysis
Data obtained from the above-mentioned study was statistically analyzed by using the paired and unpaired ‘t’ tests.
Observations and Results
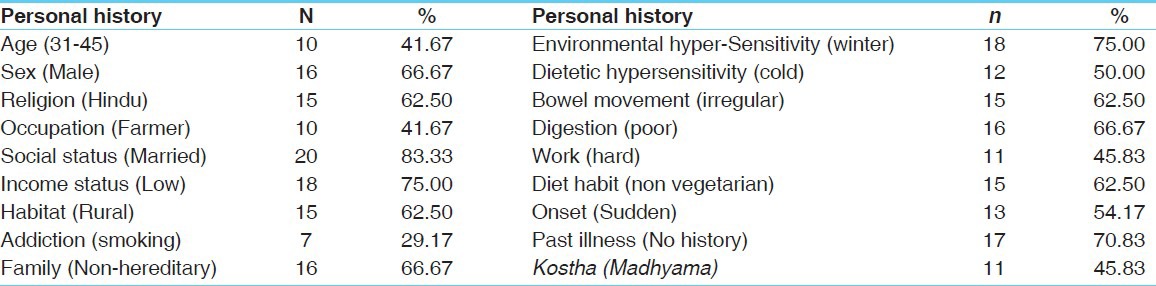
Maximum number of patients (41.67 %) were in the age group of 31 to 45 years, 66.67% were males; 62.50 % were Hindus, and 83.33% were married. Maximum number of patients belonged to the low economic status (75 %), 62.59% from rural habitat, 29.17% were addicted to smoking and 75% had winter sensitivity. Maximum number of patients had dietetic (cold) hypersensitivity, that is increasing of signs and symptoms due to cold drinks (50%), irregular bowel movements (62.50%), poor digestion (66.67%), a non-vegetarian diet (62.50%), no history of past illness (70.83%), no family history of Tamaka Shwasa (66.67%), were hard working (45.83%), Madhyama Koshtha (45.83%), and had a sudden onset (54.17%) [Table 1].
Table 1.
Personal and primary history wise distribution of 24 patients of Tamaka Shwasa
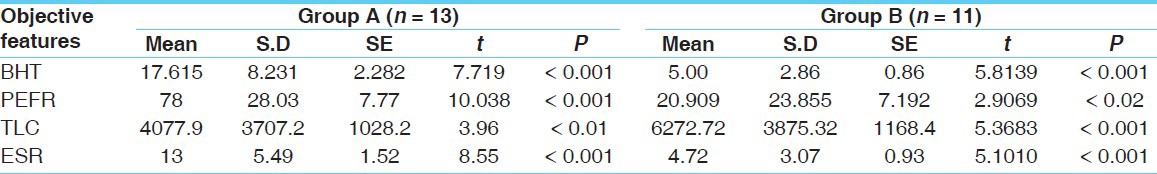
Statistically significant results were found in both groups on all clinical [Table 2] and objective features [Table 3]. On comparison Group A showed significant results than group B.
Table 2.
Effect of therapy on clinical features of Tamaka Shwasa
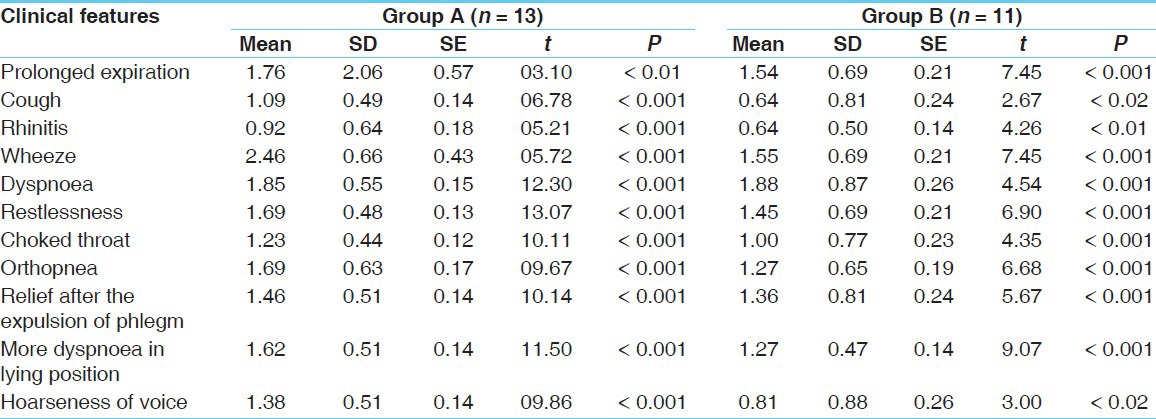
Table 3.
Effect of therapy on objective features
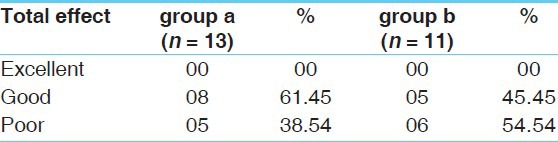
After a period of 60 days, good results observed in group A was 61.45% and 38.54% showed poor response to the treatment, whereas in group B, 38.54% patients showed good response and 54.54% showed poor response to the treatment [Table 4].
Table 4.
Overall effect of therapy
Discussion
Comparative data revealed that the ‘p’ value in almost all the features was highly significant, except Pratiloma Vayu, where the response was moderately significant in group A. On the other hand the response in group B was highly significant in maximum subjective features. The response to Pinasa was moderately significant, whereas that to Kasa and Ruksa Bhasana was less significant in group B. From the data of the objective features, the ‘p’ values were almost highly significant (P`0.001) in the maximum parameters. When the overall effect of therapy was considered, it was found that the response in group A was highly significant when compared to group B [Table 3]. Hence, it can be concluded that the Shodhana with ‘Badara Churna’ is more effective. The results are encouraging and support the classical claim that Badara is effective in alleviating the symptoms of Tamaka Shwasa and can be used extensively in the treatment.
Probable mode of action of the drug
Charaka has advised Samshodhana in Tamaka Svasa & has given more emphasis on Virechana Karma[7] to correct the de-arranged Doshas (Vata and Kapha). In addition, ingredients that alleviate Vata and Kapha (Kapha-Vataghnam), Ushna Virya (hot in potency) and which cause a downward movement of Vata (Vatanulomanam) are useful as medicines (Bhesaja), Pana ( drinks), and Anna (food) for a patient suffering from asthma.[8] A number of drugs are described for Virechana Karma in classical texts. Out of these, for the present study Aragvadha (Cassia fistula Linn) was selected. Charaka has considered it as the best Mridu Virechana Dravya[9] and Badara (Zizyphus jujuba Lam) is considered as useful in Shwasa by Sushruta[10] Govinda Das[11] Aragvadha[12] is Madhura, Tikta Rasa; Guru, Mridu, Snigdha Guna; Shita Virya and Madhura Vipaka. Hence, the drug is useful as Vata-Pitta Shamaka. Due to Madhura, Snigdha Guna it helps in Vatashamana as well as Kaphanihsarana and due to Sransana[13, 14] property it excretes Kosthagata Kapha and Pitta. In Ashtanga Hridaya, Aragvadha is described in the Kaphaghna Gana[15] and in Sushruta Samhita, Aragvadha has been described as the Adhobhagadosahara Dravya.[16] As per Charaka Samhita, Aragvadha is the best Mriduvirecana drug. Therefore, it helps in Kapha Nirharana along with Vatanulomana. Thus, the drug helps in Dosha-Dushya Vighatana in the disease Tamaka Shwasa.
According to different Ayurvedic textual references, Badara Phala Majja possesses Madhura, Amla, Kasaya Rasa; Laghu, Snigdha Guna; Shita Virya and Madhura Vipaka. As per Charaka, Badara has been described in Virechanopaga Mahakasaya[17] as Virechana Dravya[18] and also described in Amla Skandha.[19] As per Sushruta, Badara has been described in Vata Samshamana Varga.[20] Hence, the drug fulfils the criteria[21] of the line of treatment described in Charaka Samhita, Chikitsasthana.
Conclusion
Tamaka Shwasa is a type of Shwasa Roga affecting the Pranavaha Srotas, which is significantly distressing and a fatal disorder of the present-day-life. Tamaka Shwasa has been described in various Ayurvedic classics and seems to be identical to bronchial asthma. On comparative analysis of the data, it appears that Shodhana Chikitsa is more effective than Shamana Chikitsa in Tamaka Shwasa. On the basis of the findings it can be concluded that Virechana Karma, a purification therapy is the potential procedure for the treatment of Tamaka Shwasa. Badara Phala Majja Churna is found to be an effective drug for Tamaka Shwasa. It has also been observed that the drug is found to be more effective in patients after purification. No side effects have been observed during the present study. Further studies in this direction are essential in a good number of cases, for a longer period, to establish probable mechanism of action of the drug.
References
- 1.Chakrapani . Charaka Samhita of Charaka with Ayurveda Dipika commentary Chikitsasthana 17/55-60. Delhi: Rastriya Sanskrit Sansthana; 2006. p. 533, 535. [Google Scholar]
- 2.Murthy K, Srikantha R. Madhava Nidana of Madhavakara, 12/17-34. Varanasi: Chaukhambha Orientalia; 1993. pp. 50–1. [Google Scholar]
- 3.Agarwal AN, Chaudhry K, Chhabra SK, D’Souza GA, Gupta D, Jindal SK, et al. Prevalence & Risk Factors for Bronchial asthma in Indian Adults: A multicentre study. Indian J Chest Dis Allied Sci. 2006;48:13–22. [PubMed] [Google Scholar]
- 4.Viswanathan R, Prasad M, Thakur AK. Epidemiology of asthma in an urban population: Random morbidity survey. J Indian Med Assoc. 1996;46:480–3. [PubMed] [Google Scholar]
- 5.Peat JK, Gray EJ, Mellis CM, Leeder SR, Woolcock AJ. Differences in airway responsiveness between children & adults living in the same environment: An epidemiological study in two regions of New South Wales. Eur Respir J. 1994;7:1805–13. doi: 10.1183/09031936.94.07101805. [DOI] [PubMed] [Google Scholar]
- 6.Peat JK, Haby M, Spijker J, Berry G, Woolcock AJ. Prevalence of asthma in adults in Busselton, Western, Australia. BMJ. 1992;305:1326–9. doi: 10.1136/bmj.305.6865.1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chakrapani . Charaka Samhita of Charaka with Ayurveda Dipika commentary Chikitsasthana 17/121. Delhi: Rastriya Sanskrit Sansthana; 2006. p. 538. [Google Scholar]
- 8.Ibidem. Charaka samhita, Chikitsasthana, 17/147. p. 539.
- 9.Ibidem. Charaka samhita, Sutrasthana, 25/40. p. 131.
- 10.Acharya Jadavji Trikamji. Sushruta Samhita with Nibandhasangraha commentary of Dalhanacharya, Uttaratantra, 51/39. Varanasi: Chaukhambha Orientalia; 2009. p. 764. [Google Scholar]
- 11.Mishra S. Bhaisajya Ratnavali of Govinda Das, 16/38. 1st ed. Varanasi: Chaukhamba Surbharati Prakashan; 2005. p. 461. [Google Scholar]
- 12.Chakrapani . Charaka Samhita of Charaka with Ayurveda Dipika commentary, Kalpasthana, 8/4. Delhi: Rastriya Sanskrit Sansthana; 2006. p. 666. [Google Scholar]
- 13.Pandye R. Bhavaprakasha Nighantu of Bhavamishra, Haritakyadi Varga, 252. 3rd ed. Varanasi: Chaukhamba Surbharati Prakashan; 2003. p. 34. [Google Scholar]
- 14.Shastri P. Sharangadhara Samhita with the commentaries of Adhamalla’s Dipika and Kashiram’s Gurartha Dipika, Prathamakhanda, 4/4,5. 1st ed. Varanasi: Chaukhamba Surbharati Prakashan; 2006. p. 35. [Google Scholar]
- 15.Kunta A. Moreswara. Ashtanga Hridaya of Vagbhata, Sutrasthana, 15/7. Reprint, 9th ed. Varanasi: Chaukhambha Orientalia; 2005. p. 232. [Google Scholar]
- 16.Acharya Jadavji Trikamji. Sushruta Samhita with Nibandhasangraha commentary of Dalhanacharya, Sutrasthana 39/4. Reprint. Varanasi: Chaukhambha Orientalia; 2009. p. 170. [Google Scholar]
- 17.Chakrapani . Charaka Samhita of Charaka with Ayurveda Dipika commentary, Sutrasthana 4/13. Reprint. Delhi: Rastriya Sanskrit Sansthana; 2006. p. 33. [Google Scholar]
- 18.Ibidem. Charaka samhita, Vimanasthana, 8/136. p. 283.
- 19.Ibidem. Charaka samhita, Vimanasthana, 8/140. p. 284.
- 20.Acharya Jadavji Trikamji. Sushruta Samhita with Nibandhasangraha commentary of Dalhanacharya, Sutrasthana, 39/7. Reprint. Varanasi: Chaukhambha Orientalia; 2009. p. 171. [Google Scholar]
- 21.Chakrapani . Charaka Samhita of Charaka with Ayurveda Dipika commentary, Chikitsasthana, 17/148. Reprint. Delhi: Rastriya Sanskrit Sansthana; 2006. p. 539. [Google Scholar]


