Abstract
With the increasing tempo of military conflicts in the last decade, much has been learnt about imaging battlefield casualties in the acute setting. Ultrasound in the form of focused abdominal sonography in trauma (FAST) has proven invaluable in emergency triage of patients for immediate surgery. Multidetector CT allows accurate determination of battlefield trauma injuries. It permits the surgeons and anaesthetists to plan their interventions more thoroughly and to be made aware of clinically occult injuries. There are common injury patterns associated with blast injury, gunshot wounds and blunt trauma. While this body of knowledge is most applicable to the battlefield, there are parallels with peacetime radiology, particularly in terrorist attacks and industrial accidents. This pictorial review is based on the experiences of a UK radiologist deployed in Afghanistan in 2010.
Battlefield radiology is almost as old as radiology itself. The first recorded use of radiology near the battlefield was in 1897 in the Greco-Turkish war [1]. In the last decade there has been increasing use of ultrasound and multi detector CT (MDCT) in battlefield hospitals.
In the past, MDCT images from the UK-run military hospitals in Iraq and Afghanistan were reported remotely, as the conflict intensity was low and staffing of military radiology was limited. Using this remote reporting system, authorised results were with the referring clinicians within 1 h, at any time of the day, 7 days a week. Focused abdominal sonography in trauma (FAST) was performed by non-radiologists, usually general surgeons or radiographers who had undergone training.
As the conflict intensity increased in Afghanistan (in 2009) the decision to deploy radiologists was taken, as the 1-h turnaround was not rapid enough and it was difficult to coordinate the imaging of multiple casualties simultaneously.
Currently in Afghanistan the UK military hospital at Camp Bastion treats the armed forces of the NATO international security assistance force, locally employed civilian contractors, captured enemy combatants and some local nationals.
Battlefield radiology is like any other field of radiology in that it requires specific knowledge of aetiology (mechanism of injury), common patterns of disease (injury patterns) and what not to miss. This pictorial review is based on the experiences of working as a consultant radiologist at the UK military hospital at Camp Bastion in the summer of 2010.
Staffing and training
The radiology department at the military hospital at Camp Bastion consists of two consultant radiologists and about six radiographers. There are normally three radiographers on shift during the day and evening. Overnight there is one radiographer in the department, with others on call if help is needed. All the radiographers can do MDCT and plain film. The radiologists alternate between 24 h first on and 24 h second on. The radiographers receive training in CT before deployment to ensure familiarity with the particular scanners they will be using. Both radiologists and radiographers undergo about 1 month of pre-deployment military skills training.
Modalities of imaging
Plain film
Direct digital radiography (DR) is provided by Xograph DaRt (Xograph, Tetbury, UK) portable machines. They are used in the emergency department, in the radiology department and on the wards. The images can be viewed initially on a non-diagnostic built-in screen. The images are subsequently uploaded to a picture archiving and communication system (PACS) system for reporting.
In the primary trauma survey a supine chest radiograph and anteroposterior (AP) pelvic radiograph are performed. Almost all cervical spine imaging is acquired with MDCT because of the significant mechanisms of injury, and the large shoulders of most soldiers make the imaging of the C7/T1 junction difficult on plain film. The trauma series plain films are provisionally reported immediately by the consultant radiologist using a non-reporting-grade thin-film transistor screen on the portable DR machine. Although the screen does not meet diagnostic standards it is uncommon to miss an important finding by using it. All plain films are subsequently reported on diagnostic-quality monitors by consultant radiologists either at Camp Bastion or in the UK remotely.
The supine chest radiograph is evaluated for pneumothorax and haemothorax as these are addressed with a chest drain before MDCT and the operating theatre. The position of any bullets or blast fragments are determined, as this may help identify, in the acute setting, other injuries by evaluating trajectories from skin wounds to the final resting place of the foreign bodies on the chest radiograph.
If the patient has a pelvic binder in place then an AP pelvic radiograph will be performed with the binder on and off. This is because pelvic fractures can be missed if they are completely reduced by the binder.
Plain films can be used to evaluate limb injuries prior to surgery and are also used for standard indications in the emergency department.
Ultrasound
Ultrasound is performed with SonoSite Nanomaxx and M-Turbo machines (SonoSite Inc, Bothell, WA), both with curvilinear abdominal and linear high-frequency probes. These machines are used for ultrasound scanning throughout the hospital. The consultant radiologist performs nearly all of the diagnostic ultrasound scans in the hospital. If other members of staff are trained, such as the emergency medicine doctors, they will perform diagnostic ultrasound scans on their patients and seek a radiological opinion if they feel it is required.
Ultrasound is utilised in the form of FAST [2] at all trauma calls. The ultrasound scan is performed, by the consultant radiologist, in parallel with the primary survey of the patient as part of horizontal resuscitation. A 4- to 6-Mhz curvilinear probe is used to perform the study. The FAST scan is extended to include the pericardium, in addition to the abdomen and pelvis. The benefit of the consultant radiologist performing this rather than another medical or paramedical professional is that they are perceived to be more diagnostically accurate. Placing the radiologist on the trauma team also allows them direct input in the management of the patient, in particular regarding the decision of when to undertake MDCT (pre-operating theatre or post-operating theatre) and, in a multiple casualty situation, the order in which to undertake the MDCT examinations. If the patient is found to have free fluid in a body cavity, and is too unstable clinically to undergo MDCT, he will have surgery prior to imaging with MDCT. Otherwise MDCT imaging is performed before surgery.
When patients arrive who are undergoing cardio-pulmonary resuscitation (CPR), ultrasound of the heart is performed to establish if there is spontaneous cardiac motion and to exclude cardiac tamponade. Ultrasound is occasionally performed intra-operatively to identify sources of haemorrhage distant from the current operative site (e.g. chest and upper abdomen during a pelvic fixation procedure). Ultrasound is not currently used for the evaluation of pneumothorax. This is performed using plain film and MDCT. In forward battlefield situations where no imaging is available, medical staff are taught to perform needle thoracocentesis and chest drain on clinical grounds.
Ultrasound is also used for image-guided chest drain insertion, vascular access and the detection of subcutaneous splinters. Battlefield trauma victims include local women, some of whom are pregnant. Transabdominal ultrasound can be used to confirm foetal viability if the patient is of sufficient gestation.
Ultrasound is performed in patients who do not have battlefield injuries, in other words for “normal” civilian indications such as evaluating testicular lumps and detecting gall stones. Given the larger serving female population in war zones the role for gynaecological ultrasound is increasing, the main indication being pelvic pain.
Multidetector CT
The UK military installed two VCT LightSpeed 64-slice MDCT scanners (General Electric Medical Systems, Milwaukee, WI), with Dual Shot Alpha Nemoto biphasic injectors (Nemoto Kyorindo, Tokyo, Japan), into its hospital at Camp Bastion, Helmand Province, Afghanistan in the summer of 2010. These replaced an older Philips (Philips Medical Systems, Best, The Netherlands) 6-slice MDCT. Having two scanners built in a degree of redundancy and permitted increased scanning throughput at times when multiple casualties arrived at once.
MDCT is undertaken only on stable patients. If patients cannot be stabilised in the emergency department they are taken immediately to the operating theatre and receive damage control surgery [3]. Once stabilised they then undergo MDCT. The most severely injured patients receive an MDCT traumagram. At Camp Bastion this is based on the Baltimore/Geneva protocol [4]. An unenhanced helical head is acquired with 5 mm collimation with an interval of 5 mm (pitch 0.531:1) to below the mandible. 1.25 mm bone and soft tissue reconstructions are also produced. A biphasic intravenous injection of Omnipaque 300 mg I ml−1 (GE Healthcare AS, Oslo, Norway) is administered: 65 ml at 2 ml s−1 followed by 85 ml at 3.5 ml s−1. The scan is triggered at 70 s, while contrast is still flowing in. If there is abnormality on the unenhanced head MDCT then the contrast-enhanced MDCT is acquired from the vertex to the ischial tuberosities. The rationale behind this is to get contrast-enhanced images of the brain abnormality, as these may help management decisions. If the unenhanced head is normal the MDCT is acquired from the supraorbital margin (a bony anatomical landmark that ensures the circle of Willis will be imaged) to the ischial tuberosities. The scan is acquired helically with 5 mm collimation with a 5 mm interval (pitch 1.375:1). 1.25 mm bone and soft tissue reconstructions are also produced.
This biphasic protocol permits a simultaneous arterial phase and portal venous phase study to be acquired. This increases the sensitivity for the detection of arterial injuries, while not significantly decreasing the sensitivity for solid organ parenchymal injuries. These can be missed on arterial phase alone. The inclusion of the neck post-contrast has proved to be particularly useful for evaluating the carotid and vertebral arteries. Neck soft tissue injuries are relatively common in blast injury, given that this is an area of the body not protected by body armour.
Patients are imaged as soon as they are felt to be stable. In practice most imaging occurs between 20 and 60 min after patient arrival at the hospital door. An immediate initial read by a consultant radiologist, identifying potentially life-threatening findings, is provided for the surgical team; this takes about 1–2 min. This report is given verbally. The spine is not cleared at this time. A detailed read is then undertaken after which a report is typed on the radiology information system (RIS) and issued. This takes between 20 and 60 min, depending on the degree of injuries. All MDCT scans are read using axial images and multiplanar reformats on a General Electric Advantage Windows workstation. MDCT is used to exclude immediately life-threatening and less critical injuries that will require treatment later. As with all trauma imaging, reporting the positions of the endotracheal tube, nasal airways, oral airways, venous catheters, arterial catheters, intrasosseous needles, pleural drains and urinary catheters are important as misplaced lines and tubes can cause serious harm to the patient (Figure 1).
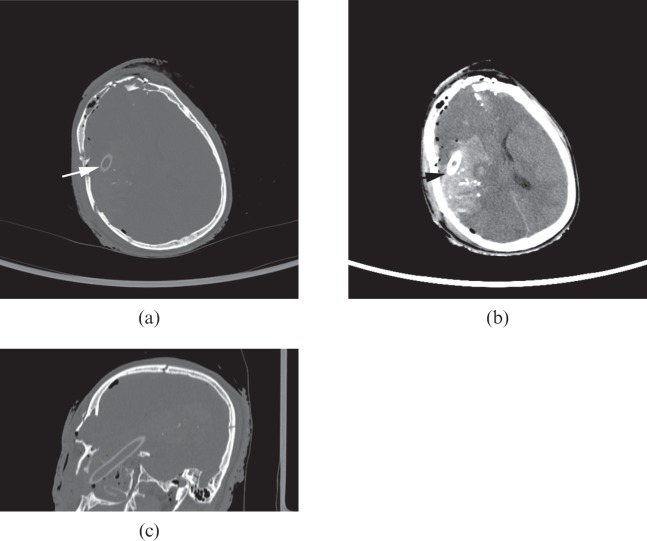
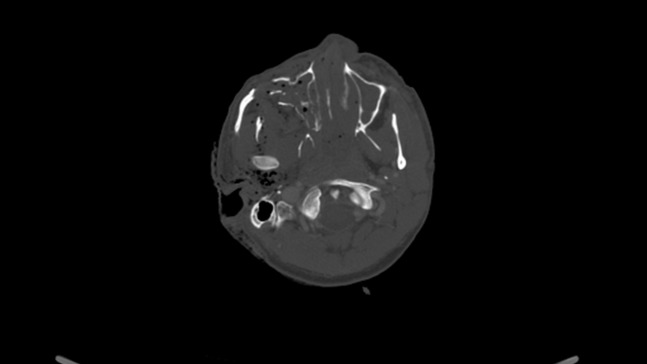
Figure 1.
(a–c) Axial (soft tissue and bone) and sagittal bone CT head of a patient with gunshot wound to the head: nasopharyngeal airway with tip within right frontal lobe (arrows). There are parenchymal contusions and cerebral haemorrhages associated, and multiple skull fractures.
MDCT angiography is used to image the great vessels and peripheral vessels. This is incorporated into the body MDCT scan with it being extended distally beyond the area of concern. It is particularly useful in penetrating lower limb injuries (Figure 2). Distal pulses can still be felt in the presence of arterial injury (e.g. a false aneurysm arising from the superficial femoral artery due to a gunshot wound). If there are abnormal pulses or the trajectory of the fragment suggests blood vessel injury then MDCT angiography should be considered.
Figure 2.
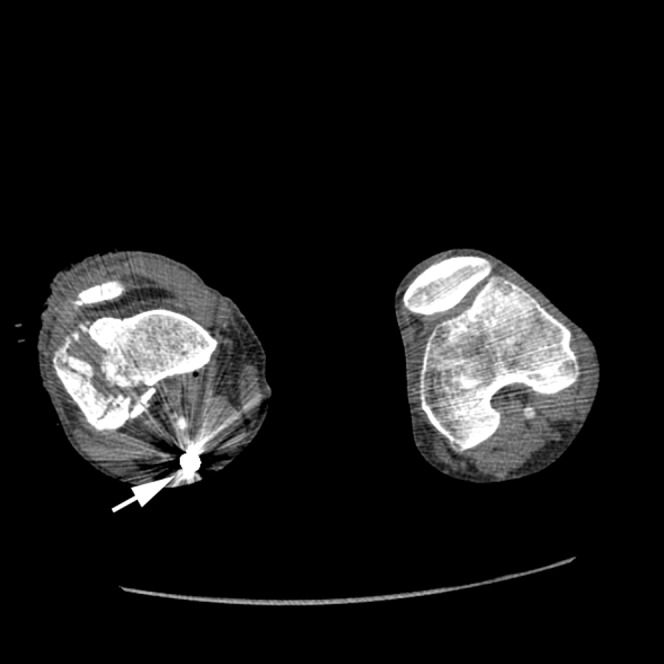
Axial CT angiogram at the level of the popliteal fossa. A bullet (arrow) has fractured the right patella and right lateral femoral condyle coming to rest behind the popliteal vessels. The popliteal artery is patent. This was confirmed at surgery.
At Camp Bastion about two-thirds of all MDCT scans performed are traumagrams. Less severely injured patients and those without battlefield injuries receive MDCT focused to the body region of interest.
Digital subtraction angiography
If arterial injury is discovered intra-operatively, or the surgeon would like to image a repaired vessel, an on-table angiogram can be formed using an image intensifier. The vessel is canulated proximally by the surgeon, and non-ionic vascular contrast is injected. With most image intensifiers a digital subtraction angiogram is possible.
Interventional radiology
There is no vascular interventional radiology service at Camp Bastion. The USA has a vascular interventional radiologist deployed in Kandahar. The UK currently transfers very few patients for interventional procedures. An example would be endovascular stent treatment of a carotid artery false aneurysm. Routine endovascular treatment of traumatic body haemorrhage is not currently undertaken. Further evaluation of interventional radiology in the battlefield situation is needed to fully optimise its role.
Image distribution
The radiological images are archived on a PACS, from which the images are sent electronically to the UK. Non-UK patients are discharged with their images recorded on DVD in Digital Imaging and Communications in Medicine (DICOM) format.
Mechanism of injury
The major mechanisms of injury from battlefield injury are blast, gunshot wound (GSW) and blunt. Each of these mechanisms produces patterns of injury that should be understood by the reporting radiologist to aid accurate diagnosis of the injuries sustained. In addition, there is a group of patients who have contracted disease while on operations but not as a result of battlefield injury. These are known as disease non-battlefield injury (DNBI) patients.
Blast injury
Blast injury has been seen particularly in the conflicts in Iraq and Afghanistan. The injuries are caused by improvised explosive devices (IEDs) [5]. IEDs are “homemade” bombs that are intended to severely injure or kill. They have a number of key components: an initiation system or fuse, explosive material, a detonator, a power supply for the detonator, and a container. These came to pre-eminence in the troubles in Northern Ireland and are now the major threat in Afghanistan.
IEDs are generally triggered by crude pressure sensors, but command wires (allowing remote detonation by an enemy combatant who is observing), radio frequency and mobile phone-based remote detonation devices are also used. Having a command wire can make the IED easier to detect as ground disturbance needed to bury the wire may be identified. Radiofrequency and mobile phone detonation can be jammed, which renders these methods of detonation less effective for the enemy.
Blast injuries can be classified as primary, secondary, tertiary and quaternary [6]. Primary blast injury results from the abrupt increase in air pressure due to the explosion. Damage occurs to the organs that have gas/soft tissue interfaces, such as the lungs and gastrointestinal tract. Secondary blast injury results from fragmentation of the IED or from adjacent debris gaining kinetic energy and causing injury by penetrating trauma. Tertiary blast injury occurs when the patient is thrown as a result of the blast injury or collides with objects in the immediate vicinity. Tertiary blast effects are the most significant to troops in vehicles (mounted troops) [6]. Quaternary blast injuries result from thermal effects, toxic effects or any post-incident risks such as drowning or freezing [6].
IEDs produce catastrophic injuries to troops who are on foot (dismounted troops). If the soldier is directly over the blast as it occurs, both lower limbs tend to be traumatically amputated (normally below the knee), as is the right arm and several fingers from the left hand. This pattern of injury in the upper limbs occurs because the right hand is holding the pistol grip of the rifle close to the soldier's body and left hand is further forward holding the rifle, and thus is just outside the centre of the blast wave. Penile and testicular injuries are also fairly common. The blast wave causes variable damage in the trunk, head and neck. The amputees who reach the emergency department alive tend to have relatively few additional injuries other than superficial fragmentation wounds. There is a group which is even more severely injured, with traumatic above-knee amputations, and often pelvic disruption too. While the pelvic disruption can be treated with an external fixator, these patients may have a large soft tissue defect in the perineum, which may later lead to sepsis and can ultimately cause their demise (Figure 3). This group of patients is sometimes treated with hind-quarter amputation. If the energy of the blast is lower, or the soldier is further away from the IED when it is initiated, then the severity of the injuries tends to be less. Again the survivors tend to have relatively few other injuries.
Figure 3.
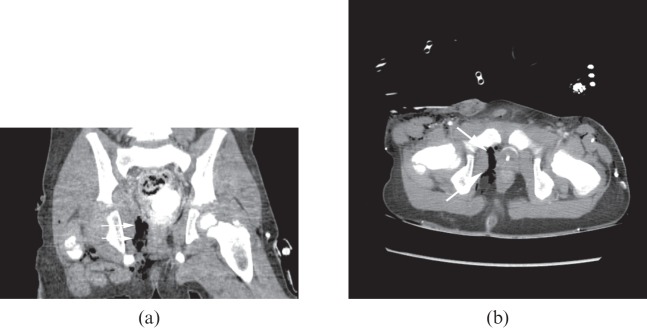
(a) Coronal and (b) axial pelvic CT images demonstrating pelvic and perineal soft tissue injuries in a child injured by an improvised explosive device. Note the large perirectal defect (arrows).
When vehicles are damaged by IEDs there tends to be a combination of tertiary and secondary blast injuries. The vehicle occupants are better protected than dismounted troops from the blast wave, but, as a result of the vehicle being thrown, the occupants are forced (often with significant energy) against the hard surfaces of the vehicle, and sustain compressive injuries. If the vehicle is partially destroyed by the blast then blast fragment injuries can also occur from vehicle debris and the IED [6]. The vehicle occupants frequently have some lower thoracic/upper lumbar spine compression fractures. Calcaneal fractures and skull fractures are also common in these patients. Cervical spine fractures also occur but are less common than the thoracic/lumbar spine fractures. The testes may be crushed between the soldier's leg and the seat of the vehicle. If there is any suspicion of testicular injury early ultrasound is advised to exclude testicular rupture. If the vehicle is turned over as a result of the IED then the injuries tend to be devastating. These soldiers generally have traumatic brain injuries, often with subdural haematomas and skull fractures, unstable spinal fractures (Figure 4), pneumothorax, pulmonary contusions, solid organ intra-abdominal injuries and limb injuries.
Figure 4.

Sagittal CT reformat of the thoracolumbar junction demonstrating burst fracture of L1 (arrow). There is retropulsion of the vertebral body producing significant spinal stenosis. The injury resulted from a vehicle being overturned by an improvised explosive device.
When reporting MDCT in patients who have been exposed to blast injury it is important to evaluate the CT scan thoroughly and systematically. Below is advice on what abnormalities to search for in each body region:
Head and neck
Skull fractures can be of any type. They are usually not subtle and, if of the open variety, there are often fragments of bone within the brain (Figure 5). As with all skull fractures, a small amount of pneumocephalus can alert the reporter to look hard for an occult skull fracture. Scalp haematomas should be reported, and underlying fractures, cerebral contusions and contra-coup injuries sought. When evaluating the facial skeleton it is important to assess the temporomandibular joints, the maxilla and mandible for fractures and/or dislocations. Teeth are often avulsed and can be a potential hazard for aspiration. Foreign bodies in the oral cavity are not infrequent and again may be a hazard for aspiration (Figure 6). Finally, look closely at the external auditory canals as foreign bodies may lodge here.
Figure 5.
Axial CT head of a child injured by improvised explosive device. Complex open skull fracture.
Figure 6.

Axial CT through the maxilla in a blast injury patient. Avulsion of upper left fifth tooth (arrow head) and an oral cavity foreign body (arrow).
Cerebral haemorrhage can occur in a tertiary blast injury when a soldier is thrown against a solid object. In our experience, subdural haemorrhage (SDH) is by far the most frequent type (Figure 7). This can be subtle. This should be actively looked for on thin soft tissue section (1.25 mm or less) with widened brain windows to increase the chances of detecting it. There does not need to be a skull fracture for a significant SDH to be present. These haemorrhages can enlarge rapidly in battlefield casualties as they often become coagulopathic. Neurosurgeons should be consulted concerning each case. At Camp Bastion there is no neurosurgeon, and therefore scans are image-linked to the neurosurgical referral centre to inform the discussion regarding the best management of the patient. If the haemorrhage is small and the patient is clinically well, a repeat scan in about 6 h from the initial scan is usually appropriate. If, however, the clinical condition changes, an examination should be performed earlier. Experience in Afghanistan is that it is difficult to predict in whom the haemorrhage will enlarge significantly from the findings on the initial scan. Parenchymal haemorrhages are also common but tend to occur either due to intracranial injury from penetrating foreign bodies or as result of the contused brain hitting the falx or skull. Traumatic subarachnoid haemorrhages are also seen and are most often due to penetrating fragments. Extradural haemorrhages are surprisingly rare in this group of patients. It is worth reviewing the contrast-enhanced brain as vascular injuries and decreased cerebral perfusion can be determined, which can be useful for prognosis (Figure 8).
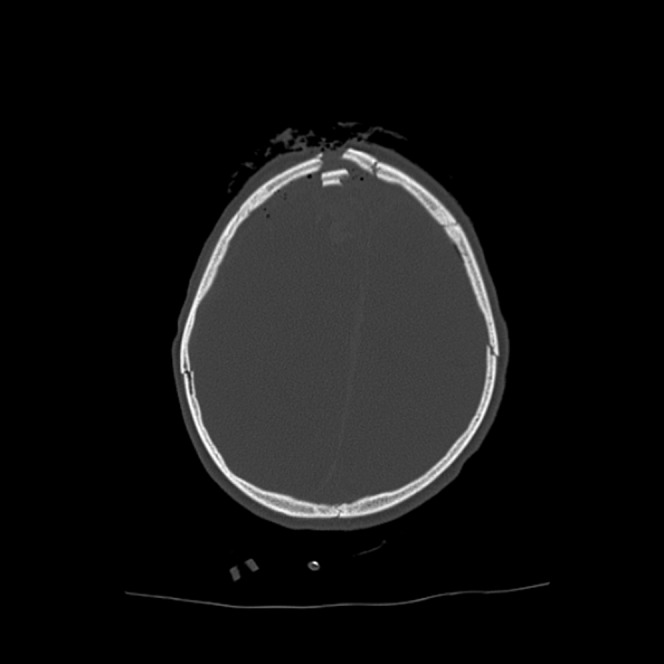
Figure 7.

Axial CT head in a blast injury patient. Traumatic right subdural haematoma (arrows). Note the midline shift and effacement of the right lateral ventricle.
Figure 8.

Axial head CT post-intravenous contrast (arterial phase) in a blast injury patient. Right-sided middle cerebral artery is less apparent than the left, suggesting decreased perfusion. This patient has a right-sided subdural haematoma.
Eye injuries are common. The following should be searched for: intraocular foreign bodies, detached retinas, vitreous haemorrhages, aqueous haemorrhages, dislocated lenses, hyphemas, pre-septal haematomas, periorbital foreign bodies, foreign bodies in the medial and lateral canthi, retro-bulbar haematomas, and foreign bodies (Figures 9 and 10). These soft tissue injuries are generally associated with orbital fractures. In order to detect these important injuries the orbit should be scrutinised on thin sections (1.25 mm or less) on bone, brain and abdominal soft tissue windows. The abdominal soft tissue windows are particular useful for demonstrating intraocular injury.
Figure 9.

Axial CT head of a patient with blast injury to left globe.
Figure 10.

Axial CT head of a child with blast injury. Foreign body within left globe (arrow).
Since soldiers wear helmets and body armour the face and neck are exposed and thus they are often injured with fragments. These can come to rest anywhere in the neck. Vascular injuries such as internal carotid or vertebral dissections occur. It is vital to scrutinise the arteries and veins of the neck on every patient. Bone windows are often the best for demonstrating subtle vascular injury and displaying the internal carotid artery as it traverses the skull base. Fragments are also best seen on bone windows. Sometimes fragments can be the bone of a fellow soldier who was next to the patient at the time of the blast. As these fragments in the affected soldier are the inoculation of foreign biological material, it is important to have a discussion with an infection control specialist to determine if any post-exposure prophylaxis is required. Fragments can enter anywhere in the neck, and traverse from left to right and caudo-cranial or vice versa. The fascial compartments of the neck seem to offer little resistance to the passage of fragments. Salivary gland injuries are common. The submandibular glands are particularly prone to being shattered. The parotid glands may also be injured and the parotid duct should be inspected on soft tissue windows in every patient.
With regard to cervical spine injury, the commonest fractures tend to be flexion, extension and lateral compression fractures of the vertebral bodies. The cervical spine is carefully inspected on multiplanar reformats and axial images in all blast injury victims.
Chest
Blast lung is demonstrated on MDCT as pulmonary haemorrhage. In our experience it is of no particular lobar predilection. In the more severe cases traumatic pneumatocoeles and pneumothoracies are also present (Figure 11). The body armour that soldiers wear has ceramic plates anteriorly, posteriorly and laterally protecting the thorax. The axillae are potentially vulnerable laterally; therefore most chest penetrating injuries enter in the region of the axilla or traverse the lateral chest soft tissues tangentially from this region. Of course, local nationals who are injured do not have body armour and therefore frequently have anterior and posterior chest fragment injuries. Many of the injuries are simply the deposition of subcutaneous fragments. If fragments traverse through the chest wall they can cause pneumothorax, haemothorax, bronchopleural fistulae, parenchymal lung contusion, pneumomediastinum, great vessel injury and cardiac injury. Cardiac and great vessel injury is uncommon among those who reach hospital alive. Patients with these injuries tend to die at the scene or in transit. There are several “fortunate” individuals who have penetrating fragments that have lodged in their epicardial fat that did not progress to their myocardium. It is important to scrutinise the heart for foreign bodies. Fragments may traverse through the diaphragm from the chest to the abdomen or vice versa (Figure 12). Penetrating fragment injuries to the axilla are very common. A careful evaluation of the subclavian and axillary vessels should be made. It is often difficult to exclude venous injury as the veins are frequently collapsed. Secondary signs such as surrounding haematoma should be sought.
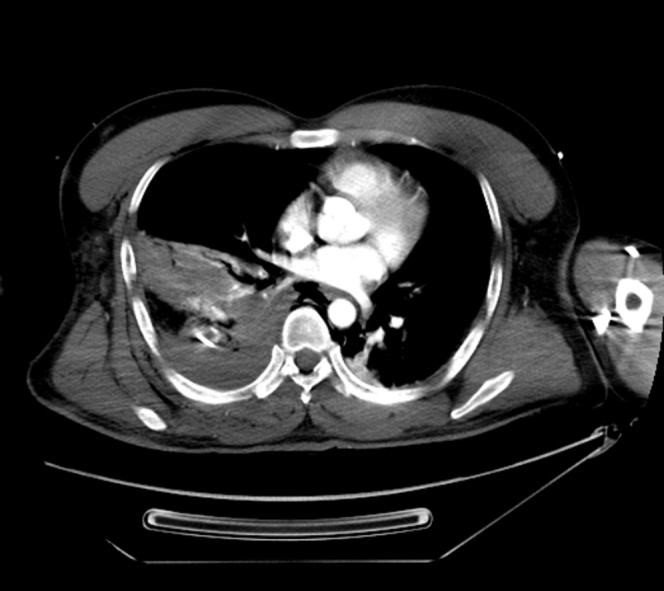
Figure 11.

(a, b) Axial CT thoracic images demonstrating haemorrhagic pulmonary contusion, traumatic pneumatocoeles and a right-sided pneumothorax (arrow). Note the double-lumen endotracheal tube.
Figure 12.
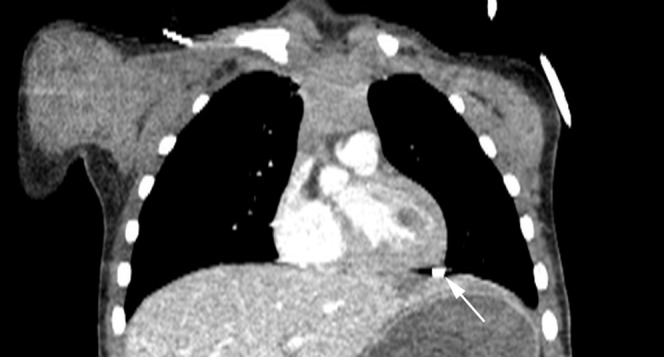
Coronal thoracic CT reformat demonstrating blast fragment lodged between epicardium and diaphragm (arrow). Note the left liver lobe laceration. This fragment traversed the diaphragm from the abdomen into the chest.
Abdomen and pelvis
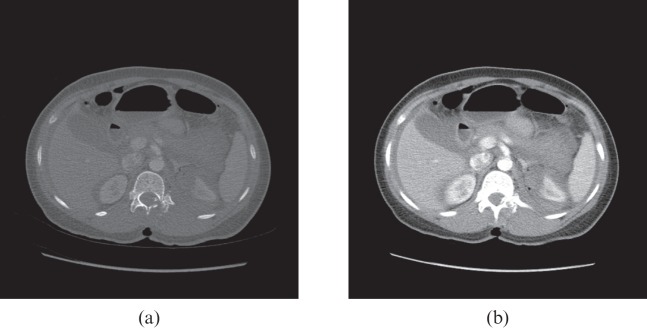
Blast bowel manifests itself as small bowel thickening. This can be restricted to, for example, the left upper quadrant or can affect the entire small bowel. Lacerations to the liver and spleen are common with penetrating fragments. Often with very sick patients it is difficult for the arms to be raised above their heads and as a result they have to be scanned with their arms by their sides. This produces streak artefact, which reduces the sensitivity of the scan for small splenic and liver lacerations. Secondary signs such as adjacent free fluid should be sought to aid detection. Small and large bowel perforations are common. These are usually associated with free fluid and free gas. Renal injuries can occur due to fragments passing through the peritoneal cavity or may simply be isolated retroperitoneal injuries (Figure 13). Vascular injuries are uncommon in those who make it to the emergency department alive. Pancreatic and adrenal injuries are rare.
Figure 13.
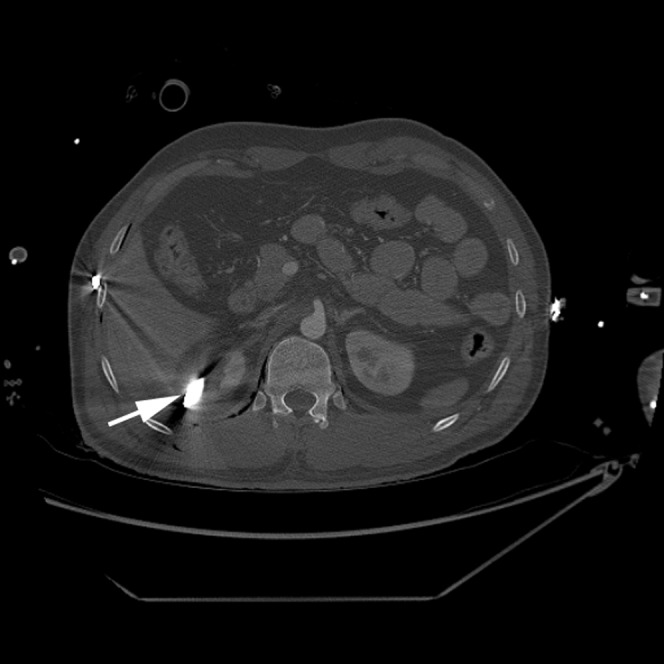
Axial abdominal CT (bone windows). Penetrating fragment in right kidney (arrow) from blast injury. The fragment entered posteriorly. At surgery there was no breach of the peritoneum.
Spine
Penetrating spinal injuries are rare in blast injury. When they do occur they can result in small fragments coming to lie in the neural foramina or epidural space. The entire spine should be evaluated for fractures, which are usually the result of tertiary blast injuries.
Gunshot wounds
The helmets and body armour that soldiers wear protect the anterior, posterior and lateral chest, as well as the head from the forehead to the occiput. Injuries therefore tend to occur in the face, axilla and abdomen/pelvis, buttocks and limbs. Local nationals without body armour can of course have GSWs anywhere.
As with blast injury, systematic evaluation of the CT scan is advised in patients who have sustained gunshot injury. Below is advice on what abnormalities to search for in each body region.
Head and neck
Patients with facial injuries who reach the emergency department alive usually have not had their cranial fossae breached, and their injuries normally involve just the facial skeleton (Figure 14). Basal skull and skull vault fractures are commonly associated, but tend to be simple fractures rather than depressed fractures or large holes in the skull. These facial fractures tend to be complex, involving the maxilla, mandible and zygoma. As with blast injuries, the eyes should be carefully evaluated for ocular trauma. Oral fragments are common, and should be reported, as they herald a risk of aspiration.
Figure 14.
Axial head CT (bone windows). Complex right-sided facial fracture. The bullet entered just below the right orbit and exited anterior to the right exterior auditory meatus.
Skull injuries from GSW tend to be devastating. Generally, there is a small entry wound and a large exit wound. Sometimes the bullet does not exit and remains within the brain tissue. Multiple bone fragments are normally introduced into the brain substance from the entry wound. The bullet may fragment after passing into the skull. As one would expect there is a track of haemorrhagic contusion following the bullet. The bullet produces cavitation of the brain as it travels and there is normally significant pneumocephalus (Figure 15). There are often small traumatic subarachnoid and subdural haemorrhages. If the bullet just traverses the frontal lobe the remainder of the brain often appears relatively normal. More posterior injuries tend to be associated with cerebral oedema with uncal and eventually tonsillar herniation. Transmitting the images to a neurosurgical centre is again a matter of urgency to select those patients who have a survivable injury.
Figure 15.

Axial head CT. Gunshot wound to head. Left frontal exit wound. Bullet fragments (arrows) are present within the right cerebral hemisphere. Haemorrhage is present within and around the bullet track.
In the neck the bullet can injure any structure. Careful evaluation of the neck vessels and bones is required.
Chest
Those patients with chest injuries who reach the emergency department alive often have tangential lateral soft tissue injuries that do not breach the parietal pleura. Normally these are associated with peripheral lung contusions. Fractures of the scapula are common from bullet injuries. GSWs that breach the parietal pleura result in haemopneumothorax. In significant haemothorax an intercostal artery is often the source of the haemorrhage (Figure 16). Again, in patients who reach the emergency department alive, great vessel and cardiac injuries are rare. Rib fractures and clavicle fracture are common in penetrating injuries. GSWs to the axilla are frequent. Careful evaluation of the subclavian and axillary vessels should be made. The bullet can lodge deep to the scapula.
Figure 16.
Axial CT thorax. Traumatic right pulmonary contusion and haemopneumothorax. This was secondary to a penetrating blast fragment to the chest.
Abdomen and pelvis
In the abdomen and pelvis, as with the chest, lateral entry wounds rather than anterior or posterior wounds are more likely in soldiers due to the body armour they wear. Obviously, patients not wearing body armour can have injuries anywhere. As with penetrating blast injuries the commonest organs to be injured are liver, spleen, small bowel and large bowel. Bullets can travel through the iliac wings into the pelvis, often injuring the bowel and occasionally injuring the urinary bladder. Dilute non-ionic contrast media can be instilled through a urinary catheter prior to MDCT to aid diagnosis of urinary bladder injury. Soft tissue injuries traversing the buttocks are common. These patients often do not have any internal pelvic or abdominal injuries.
Spine
Bullets may injure any part of the spine. Injuries tend to involve the spine and organs deep to the spine such as the kidneys or lungs (Figure 17). Again, body armour limits the spinal injuries seen in soldiers. In soldiers these tend to have lateral entry wounds with the bullet traversing a body cavity before injuring the spine on the way out of the body. Obviously the cervical spine is exposed and any penetrating injury can occur here.
Figure 17.
(a, b) Axial CT abdomen (bone and soft tissue windows) gunshot wound entering through the L1 lamina and pedicle, then traversing the left renal upper pole, small bowel and colon before exiting through the left anterolateral abdominal wall.
Limbs
Bullet wounds to limbs are common as these are unprotected. Frequently they do not involve major vessels or bones. If there is concern of vascular injury an MDCT angiogram can be performed in a stable patient or an on-table digital subtraction angiogram in an unstable patient.
Blunt trauma
Battlefield blunt trauma resembles civilian blunt trauma. Road traffic collisions and falls from height are similar to those seen in civilian practice.
Disease and injury not occurring on the battlefield
Since the majority of soldiers are males, 18–40 years old, the diseases that manifest themselves in an operational environment that require imaging are relatively few. The commonest are renal tract stone disease, appendicitis and epididymo-orchitis. As in civilian practice non-renal diagnoses are frequently demonstrated on MDCT KUB (kidneys, ureters and bladder; Figure 18).
Figure 18.
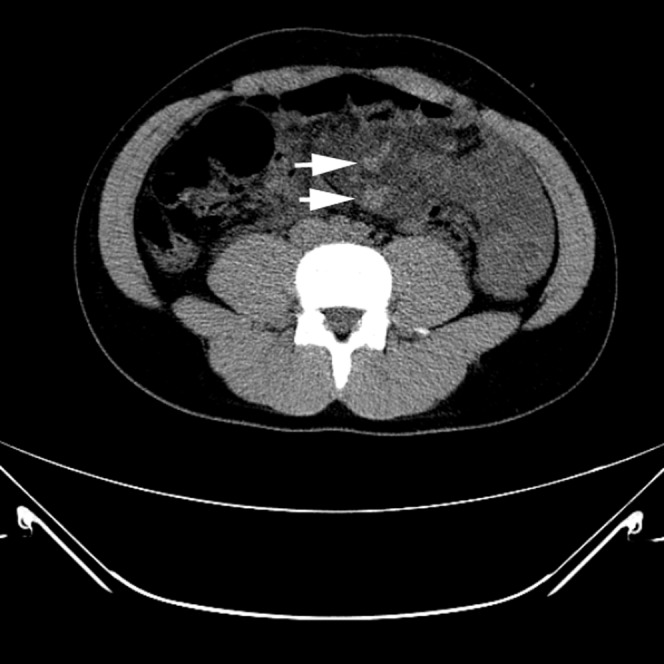
Unenhanced axial abdominal CT performed as CT KUB (kidneys, ureters and bladder) demonstrating oedematous small bowel mesentery and dilated mesenteric veins (arrows). This was confirmed as small bowel volvulus at surgery.
With increasing numbers of women serving in war zones, ovarian cysts, pelvic inflammatory disease, acute cholecystitis and pregnancy are being diagnosed more often.
The ability to offer definitive imaging in the operation environment for disease or non-battlefield injury allows troops to be managed locally and stay on deployment rather than having to be repatriated for diagnostic work-up.
Conclusion
Battlefield radiology is an old branch of radiology that has recently rapidly advanced due to the conflicts in Iraq and Afghanistan. Plain film and ultrasound are useful modalities for imaging battlefield injuries. Deployed MDCT, however, has significantly increased the clinical input that radiologists can offer in battlefield trauma. It is extremely difficult to manage battlefield trauma well without MDCT, as many non-clinically obvious injuries will go undiagnosed or patients will suffer from unnecessary exploratory surgery. Interventional vascular radiology is being used in Afghanistan. It is not known whether it produces enough benefit to justify the resources required to provide it as a deployed service. Further work is required to determine its usefulness in the battlefield environment. The days of radiologists not deploying to operational theatres are hard to imagine. Remote reporting of MDCT images is too slow and is not fit for purpose with the operational tempo we see today. Radiology, radiologists and radiographers are firmly in the centre of battlefield trauma care, and are a vital component of the deployed clinical team.
References
- 1.Ramoutsaki IA, Giannacos EN, Livadas GN. Birth of battlefield radiology: Greco-Turkish War of 1897. Radiographics 2001;21:263–6 [DOI] [PubMed] [Google Scholar]
- 2.Patel NY, Riherd JM. Focused assessment with sonography for trauma: methods, accuracy, and indications. Surg Clin North Am 2011;91:195–207 [DOI] [PubMed] [Google Scholar]
- 3.Holcomb JB, Helling TS, Hirshberg A. Military, civilian, and rural application of the damage control philosophy. Mil Med 2001;166:490–3 [PubMed] [Google Scholar]
- 4.Nguyen D, Platon A, Shanmuganathan K, Mirvis SE, Becker CD, Poletti PA. Evaluation of a single-pass continuous whole-body 16-MDCT protocol for patients with polytrauma. AJR Am J Roentgenol 2009;192:3–10 [DOI] [PubMed] [Google Scholar]
- 5.Ramasamy A, Harrisson SE, Clasper JC, Stewart MP. Injuries from roadside improvised explosive devices. J Trauma 2008;65:910–14 [DOI] [PubMed] [Google Scholar]
- 6.Ramasamy A, Hill AM, Hepper AE, Bull AM, Clasper JC. Blast mines: physics, injury mechanisms and vehicle protection. J R Army Med Corps 2009;155:258–64 [DOI] [PubMed] [Google Scholar]