Abstract
The classic imaging findings of posterior reversible encephalopathy syndrome (PRES) are of bilateral parietal and occipital subcortical vasogenic oedema, and are well established in the literature. As experience with PRES grows, varied and atypical presentations are being increasingly described. This pictorial review illustrates the variable presentations of PRES, including cases with atypical imaging findings. We illustrate cases of PRES with varying distributions of vasogenic oedema as well as cases with atypical imaging findings, such as variations of haemorrhage and restricted diffusion. Atypical imaging findings should not dissuade the diagnosis of PRES in the appropriate clinical situation, and knowledge of the varied appearance and atypical findings of PRES allows the radiologist to make this diagnosis.
Posterior reversible encephalopathy syndrome (PRES) describes a neurological syndrome characterised by a variety of symptoms, including headache, altered mental status, visual disturbances and seizures, and is accompanied by a unique, potentially reversible imaging pattern [1,2]. Causes of PRES are diverse and include hypertension, eclampsia/pre-eclampsia, sepsis, immunosuppressive agents, chemotherapy, collagen vascular disease and renal failure [2]. Although the pathophysiology of PRES remains unknown, the currently preferred explanation relates to hypertension, impaired autoregulation and hyperperfusion [2]. The classic imaging findings are of vasogenic oedema in the subcortical white matter of the parietal and occipital lobes [3]. As experience with PRES grows in the literature, atypical presentations of PRES are being increasingly described. Authors have demonstrated cases of PRES with atypical vasogenic oedema patterns of distribution, such as frontal lobe, cerebellum, basal ganglia or brain stem involvement [3-6]. Unilateral cases of PRES have also been demonstrated [4]. In addition, cases of PRES with haemorrhage [7] and reversible restricted diffusion [8] have been described. Knowledge of the different presentations of PRES is important, as atypical imaging findings should not dissuade a diagnosis of PRES in the correct clinical context. The purpose of this review is to demonstrate the diverse imaging features of PRES. The cases illustrated in this review demonstrate clinical and imaging presentations characteristic of PRES, with the characteristic clinical and imaging reversibility associated with this diagnosis.
Distribution
Hinchey et al [9] originally described a posterior hypertensive encephalopathy syndrome with a predominant posterior distribution of imaging findings on CT or MRI. Typically, PRES presents as widespread, usually reversible vasogenic oedema, predominantly in the subcortical white matter of the occipital and parietal lobes (Figure 1). In large retrospective studies, this is the most common pattern of oedema [3,4,6]. The predilection for the posterior brain is thought to be a result of the better-developed sympathetic regulation in the anterior circulation, with the posterior circulation more susceptible to impaired autoregulation and vasogenic oedema in the setting of hypertension [10].
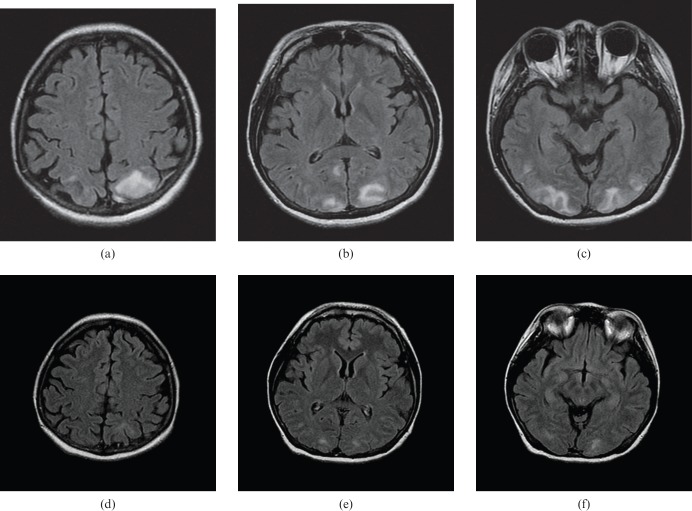
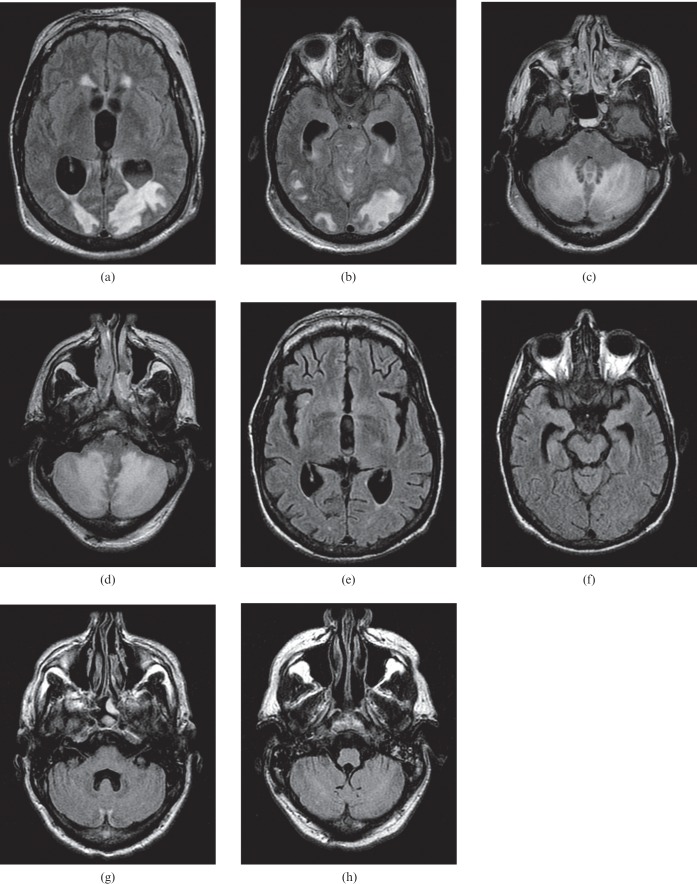
Figure 1.
A 29-year-old female with systemic lupus erythematosus and lupus nephritis, recently started on cyclosporine. She presented with new-onset visual changes and headache, progressing to seizure. (a–c) Brain MRI [fluid attenuated inversion recovery (FLAIR) sequence] obtained on the day of presentation demonstrates moderate vasogenic oedema in the subcortical white matter of the parietal and occipital regions. (d–f) Brain MRI (FLAIR sequence) performed 7 days later demonstrates resolution of the vasogenic oedema seen on the previous MR study.
In addition to the occipital and parietal symmetric pattern of vasogenic oedema, wide variations of distribution have been described in the literature. The pattern of oedema in PRES can be widespread, and can involve the entire brain (Figure 2). Although typically symmetrical and bilateral, asymmetrical or unilateral distributions of vasogenic oedema in PRES can also be seen [4] (Figure 3). Many authors have described cases of PRES with basal ganglia (Figure 4), cerebellar (Figure 5) or brain stem (Figure 6a–d) involvement [2-4,6].
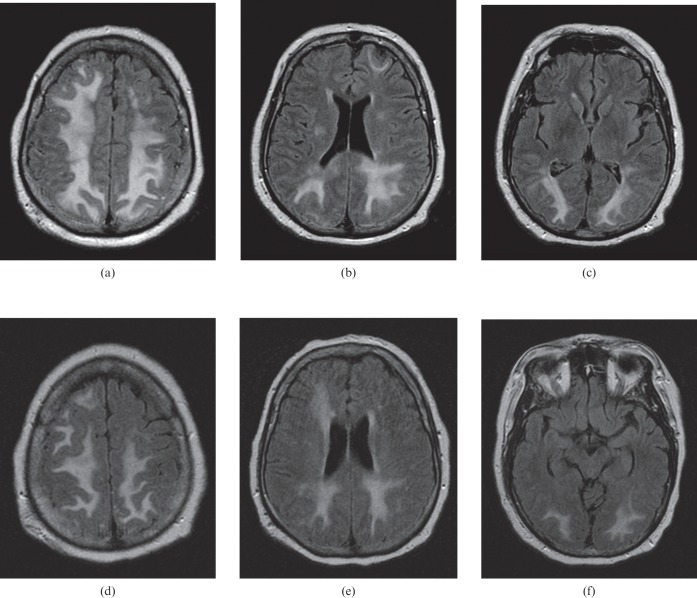
Figure 2.
A 61-year-old male presenting with tonic–clonic seizures, progressing to coma. (a–c) Brain MRI [fluid attenuated inversion recovery (FLAIR) sequence] obtained on the day of presentation demonstrates marked vasogenic oedema involving subcortical, deep and periventricular white matter of the frontal, parietal and occipital regions, while maintaining a predominant posterior pattern. (d–f) Brain imaging (FLAIR sequence) performed 6 days later demonstrates improvement of the vasogenic oedema.
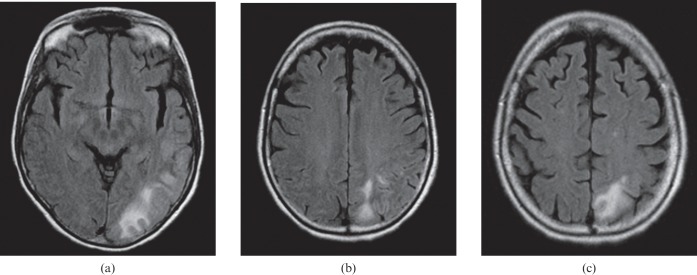
Figure 3.
A 61-year-old female with recent liver transplantation on tacrolimus therapy with new-onset fluent aphasia. (a–c) Brain MRI (fluid attenuated inversion recovery sequence) demonstrated unilateral moderate vasogenic oedema in the white matter of the left posterior temporal, parietal and occipital regions.
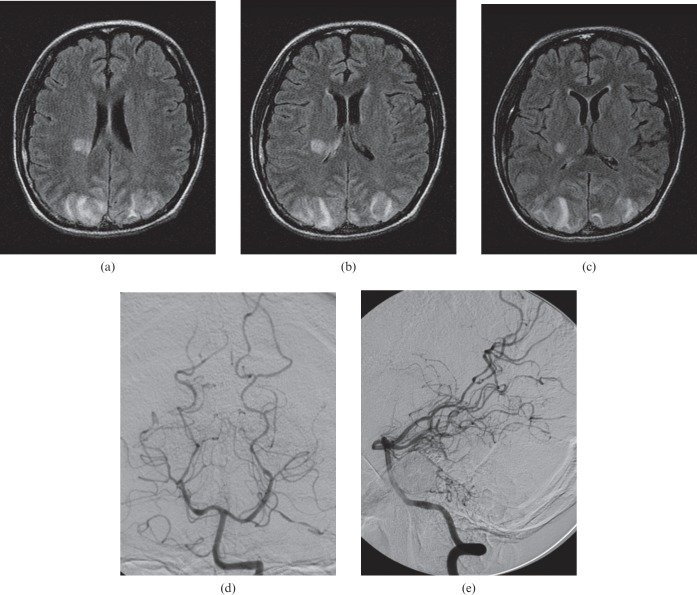
Figure 4.
A 23-year-old female with systemic lupus erythematosus presenting with new-onset seizures. (a–c) Brain MRI (fluid attenuated inversion recovery sequence) obtained on the day of presentation demonstrates vasogenic oedema in the posterior limb of the right internal capsule, extending into the adjacent corona radiata, and subcortical white matter of both parietal lobes. (d, e) Selective digital subtraction angiogram of the left vertebral artery demonstrated multiple areas of vessel calibre irregularity in the secondary and tertiary branches of the left and right posterior cerebral arteries.
Figure 5.
A 31-year-old male intravenous drug abuser found unconscious. Blood pressure at presentation was 180/110 mmHg. (a–d) Brain MRI [fluid attenuated inversion recovery (FLAIR) sequence] demonstrated marked vasogenic oedema in the white matter of the parietal and occipital regions, most severe in the cerebellum, with resultant obstructive hydrocephalus. (e–h) Brain MRI (FLAIR sequence) performed 6 weeks later demonstrates resolution of the vasogenic oedema seen on the previous MR study.
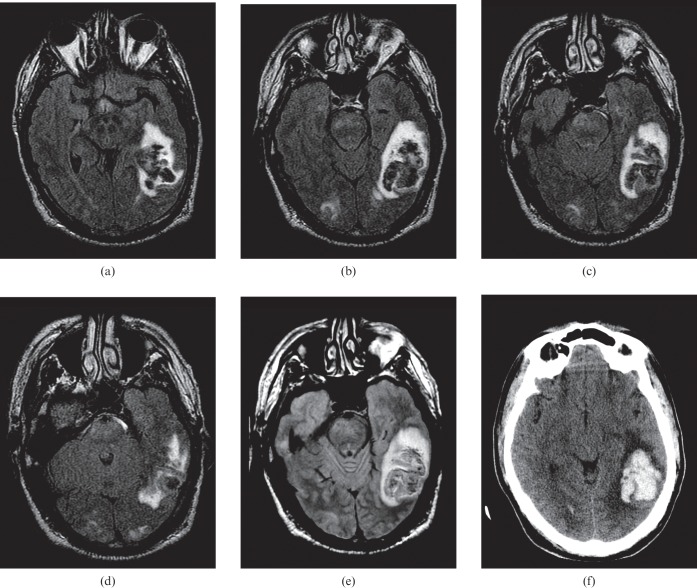
Figure 6.
A 39-year-old male with an appendiceal carcinoid tumour treated with chemotherapy complicated by haemolytic uraemic syndrome. Systolic blood pressure at the time of the study was >220 mmHg. (a–d) Brain MRI (fluid attenuated inversion recovery sequence) demonstrates numerous foci of vasogenic oedema in the occipital regions, cerebellum and brain stem. A large haematoma is seen in the left temporal lobe. (e) Proton density image demonstrates a haematoma in the left temporal lobe. (f) Non-contrast CT again demonstrates the known haematoma with surrounding vasogenic oedema.
Haemorrhage
Intracranial haemorrhage is known to occur in PRES with an incidence of approximately 15% [7]. The pathological mechanism is still not well understood but is thought to relate to hypertension and hyperperfusion or vasculopathy with resulting hypoperfusion. Varying patterns of haemorrhage have been identified, including large focal haematomas (Figure 6d–f), subarachnoid haemorrhage (Figure 7) or multiple minute foci of haemorrhage (Figure 8).
Figure 7.
A 70-year-old with metastatic hepatocellular carcinoma presenting with new-onset seizures 7 days after commencing a trial chemotherapeutic agent, brivanib. (a–c) Brain MRI (fluid attenuated inversion recovery sequence) demonstrates vasogenic oedema in the subcortical and deep white matter of the parietal and occipital regions. (d–g) T2* gradient sequence demonstrates subarachnoid haemorrhage in the interhemispheric fissure, right ambient cistern and occipital horn of the left lateral ventricle.
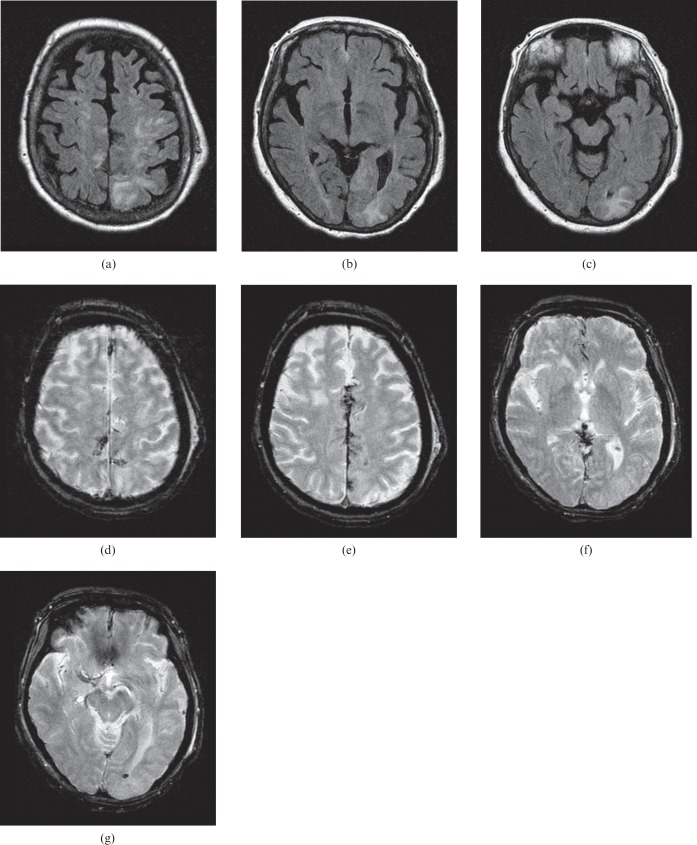
Figure 8.
An 87-year-old female presenting with a 15 min episode of visual changes and slurred speech. Blood pressure at the time of presentation was 176/99 mmHg. (a–d) Brain MRI (fluid attenuated inversion recovery sequence) demonstrates vasogenic oedema in the subcortical white matter of the left post-central gyrus, the right parietal lobe, right temporal lobe and bilateral occipital lobes. (e–g) T2* gradient sequence demonstrates haemosiderin in a petechial cortical gyral distribution.
Restricted diffusion
Restricted diffusion as an associated finding has been described in PRES and has been shown to be potentially reversible [8]. Benziada-Boudour et al [8] demonstrated a case of PRES with foci of restricted diffusion that resolved on follow-up imaging with no abnormal imaging sequelae. Similar reversibility of restricted diffusion abnormalities has been seen in patients with transient cerebral ischaemia [10] and vasospasm after subarachnoid haemorrhage [11]. The patient in Figure 9 demonstrates a region of restricted diffusion that resolved on follow-up imaging. Another patient demonstrates restricted diffusion in the splenium of the corpus callosum, which resolved on follow-up imaging (Figure 10).
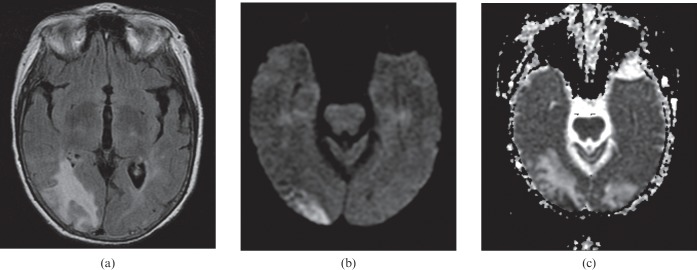
Figure 9.
A 65-year-old female with thrombotic thrombocytopenic purpura presenting with acute renal failure and generalised seizures. Her systolic blood pressure was 200 mmHg at presentation. (a) Brain MRI (fluid attenuated inversion recovery sequence) demonstrates vasogenic oedema in the white matter of the occipital lobes. (b) Diffusion-weighted imaging and (c) apparent diffusion coefficient map demonstrate a region of restricted diffusion in the right occipital cortex.
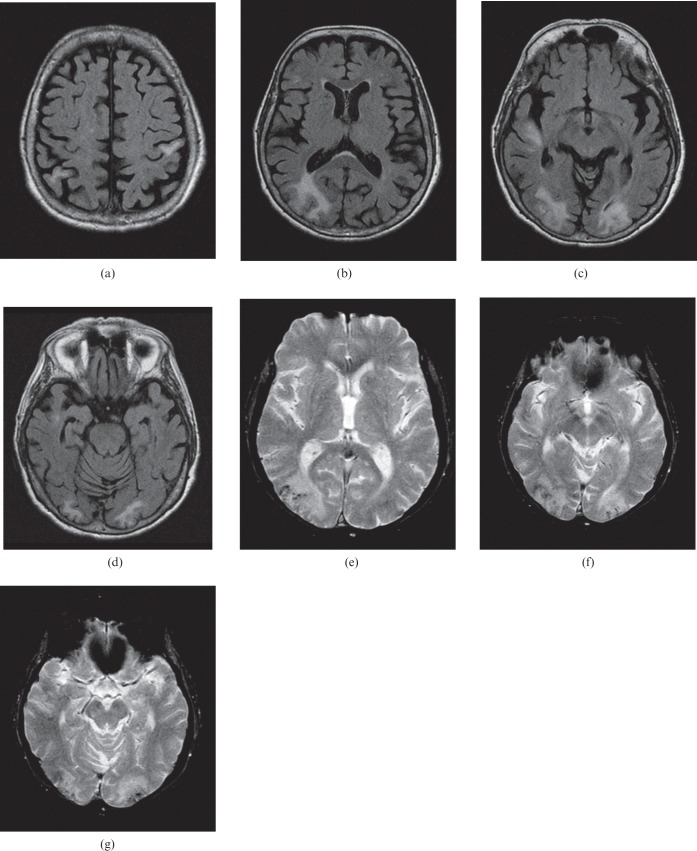
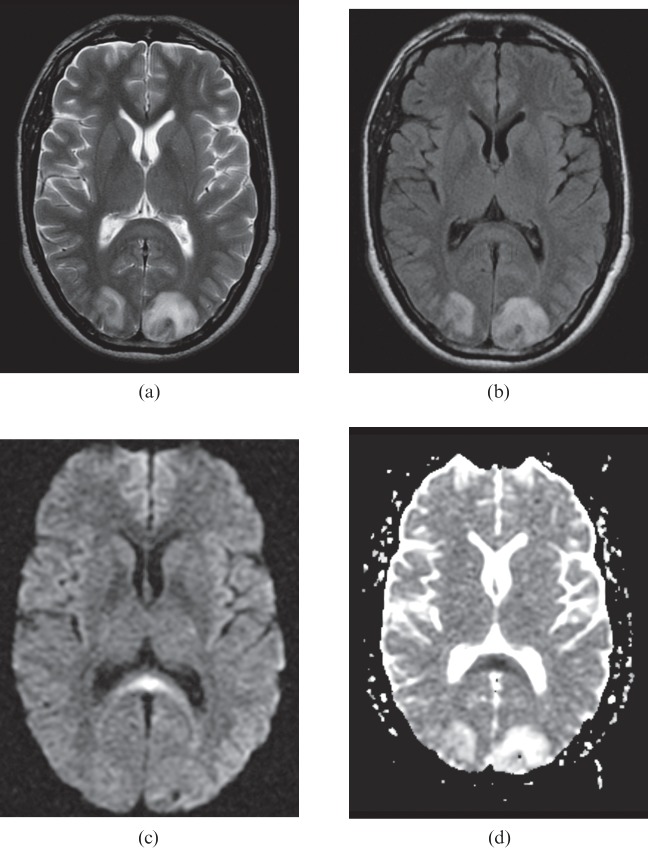
Figure 10.
A 30-year-old male with uncontrolled hypertension presenting with a 2-week history of paroxysmal headaches and visual changes. His blood pressure was 198/120 mmHg on presentation. (a, b) Brain MRI with (a) T2 and (b) fluid attenuated inversion recovery sequence demonstrated white matter vasogenic oedema in the occipital lobes. (c) Diffusion-weighted imaging and (d) apparent diffusion coefficient map demonstrated a transient splenial lesion, a region of reversible restricted diffusion in the splenium of the corpus callosum. This resolved on subsequent imaging (not shown).
Angiography
Findings of PRES on catheter angiography include focal or diffuse vasoconstriction, vasodilation or a “string-of-beads” appearance. This vessel irregularity can also be seen on CT angiography or MR angiography [2]. These findings may be confused for other diagnoses, such as vasospasm or vasculitis [2]. The patient in Figure 4d,e demonstrates these characteristic angiographic findings.
Summary
As demonstrated, PRES can present with a variety of imaging findings on CT, MRI and angiography. Although originally described as a bilateral symmetrical pattern of vasogenic oedema in the posterior parenchyma, other distributions of vasogenic oedema can be seen, including a unilateral pattern and involvement of the cerebellum and brain stem. The typical findings of patchy discontinuous vasoconstriction on angiography are well recognised. Furthermore, haemorrhage is increasingly being recognised in PRES and does not exclude the diagnosis. This can be anatomically located in the brain parenchyma as a focal haematoma or petechial gyral pattern, or in the subarachnoid space. Restricted diffusion is an atypical finding in PRES, but has been described and should not preclude the diagnosis of PRES in the appropriate clinical context.
References
- 1.Bartynksi WS. Posterior reversible encephalopathy syndrome. Part 2. Controversies surrounding pathophysiology of vasogenic edema. AJNR Am J Neuroradiol 2008;29:1043–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartynksi WS. Posterior reversible encephalopathy syndrome. Part 1. Fundamental imaging and clinical features. AJNR Am J Neuroradiol 2008;29:1036–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartynksi WS, Boardman JF. Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol 2007;28:1320–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, et al. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol 2007;189:904–12 [DOI] [PubMed] [Google Scholar]
- 5.Decker DA, Falchook AD, Yachnis AT, Waters MF. Radiographic and pathologic findings in an atypical brainstem variant of reversible posterior leukoencephalopathy syndrome. Neurologist 2009;15:364–6 [DOI] [PubMed] [Google Scholar]
- 6.Ni J, Li-Xin Zhou , Hao H-L, Liu Q, Yao M, Li M, et al. The clinical and radiological spectrum of posterior reversible encephalopathy syndrome: a retrospective series of 24 patients. J Neuroimaging 2011;21:219–24 [DOI] [PubMed] [Google Scholar]
- 7.Hefzy HM, Bartynski WS, Boardman JF, Lacomis D. Hemorrhage in posterior reversible encephalopathy syndrome: imaging and clinical features. AJNR Am J Neuroradiol 2009;30:1371–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benziada-Boudour A, Schmitt E, Kremer S, Foscolo S, Riviere A-S, Tisserand M, et al. Posterior reversible encephalopathy syndrome: a case of unusual diffusion-weighted MR images. J Neuroradiol 2009;36:102–5 [DOI] [PubMed] [Google Scholar]
- 9.Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med 1996;334:494–500 [DOI] [PubMed] [Google Scholar]
- 10.Kidwell CS, Ager JR, Di Salle F, Starkman S, Villablanca P, Bentson J, et al. Diffusion MRI in patients with transient ischemic attacks. Stroke 1999;30:1174–80 [DOI] [PubMed] [Google Scholar]
- 11.Condette-Auliac S, Bracard S, Anxionnat R, Schmitt E, Lacour JC, Braun M, et al. Vasospasm after subarachnoid hemorrhage: interest in diffusion-weighted MR imaging. Stroke 2001;32:1818–24 [DOI] [PubMed] [Google Scholar]