Abstract
Background. The pathogenesis of influenza A virus subtype H5N1 (hereafter, “H5N1”) infection in humans is not completely understood, although hypercytokinemia is thought to play a role. We previously reported that most H5N1 viruses induce high cytokine responses in human macrophages, whereas some H5N1 viruses induce only a low level of cytokine production similar to that induced by seasonal viruses.
Methods. To identify the viral molecular determinants for cytokine induction of H5N1 viruses in human macrophages, we generated a series of reassortant viruses between the high cytokine inducer A/Vietnam/UT3028II/03 clone 2 (VN3028IIcl2) and the low inducer A/Indonesia/UT3006/05 (IDN3006) and evaluated cytokine expression in human macrophages.
Results. Viruses possessing the acidic polymerase (PA) gene of VN3028IIcl2 exhibited high levels of hypercytokinemia-related cytokine expression in human macrophages, compared with IDN3006, but showed no substantial differences in viral growth in these cells. Further, the PA gene of VN3028IIcl2 conferred enhanced virulence in mice.
Conclusions. These results demonstrate that the PA gene of VN3028IIcl2 affects cytokine production in human macrophages and virulence in mice. These findings provide new insights into the cytokine-mediated pathogenesis of H5N1 infection in humans.
Keywords: H5N1 virus, Hypercytokinemia, cytokine, human macrophages, virulence, Microarray, Immune response
(See the editorial commentary by Donis and Cox, on pages 208–10 and editorial commentary Hirsch, on page 207.)
Highly pathogenic avian influenza A virus subtype H5N1 (hereafter, “H5N1”) have been circulating among wild birds and domestic poultry worldwide since 2003 [1, 2]. The total number of laboratory-confirmed cases of human H5N1 infection has climbed to >600 cases, with a mortality rate of 60%, posing a true threat to human health [3]. Although the high pathogenicity of these viruses is not completely understood, hypercytokinemia and systemic viral replication have been reported for patients infected with these viruses [4–9].
Alveolar macrophages are considered central players in both innate and adaptive immune responses to respiratory infection and can be infected with H5N1 viruses [10]. In in vitro studies, human monocyte–derived macrophages infected with H5N1 viruses produced higher levels of cytokines than those infected with seasonal viruses, suggesting cytokine production contributes to the high pathogenicity of H5N1 viruses in humans [1, 11–15]. However, we previously found that some H5N1 viruses induce a level of cytokine production similar to that induced by seasonal viruses in human monocyte–derived macrophages [16], indicating that the ability to induce cytokines is virus-strain dependent.
Previous findings regarding the role of nonstructural protein 1 (NS1) in cytokine induction are controversial; in one study, NS1 was shown to affect cytokine production in human macrophages [13], whereas another study was unable to confirm NS1's contribution to cytokine induction in these cells [17]. PB2-E627K, which is widely known as a mutation that enhances viral growth in mammalian cells and some mammals, is reported to enhance cytokine production [13, 18]. Thus, determining the potential molecular markers that enhance cytokine production could extend our knowledge of the basis for the high virulence of H5N1 viruses in humans.
We previously evaluated the ability of several H5N1 viruses to induce cytokines in human macrophages and found that A/Vietnam/UT3028II/03 clone 2 (VN3028IIcl2) was a high cytokine inducer and A/Indonesia/UT3006/05 (IDN3006) a low cytokine inducer [16]. Here, we generated a series of reassortant viruses between these 2 viruses and attempted to identify the viral molecular determinants that confer high cytokine induction in human macrophages. Further, to reveal the molecular networks affected by the virus infection, we examined the entire gene transcriptional profiles in human macrophages by using microarray analysis. To clarify whether differential expression of cytokines mediated by H5N1 viruses contributes to pathogenicity in mammals, we compared the virulence in mice infected with the high cytokine inducer to that in mice infected with the low cytokine inducer.
MATERIALS AND METHODS
Ethics Statement
Our research protocol for the use of human-derived macrophages was approved by the Research Ethics Review Committee of the Institute of Medical Science, the University of Tokyo (approval numbers 18-15-0129 and 19-24-200430). Our research protocol for the use of mice followed the University of Tokyo's Regulations for Animal Care and Use, which was approved by the Animal Experiment Committee of the Institute of Medical Science, the University of Tokyo (approved numbers 19–29).
Cells
A549 and HEK293T cells were maintained in Dulbecco's modified Eagle's medium (DMEM) with 10% fetal calf serum. Madin-Darby canine kidney (MDCK) cells were maintained in minimal essential medium supplemented with 5% newborn calf serum. Human monocyte–derived macrophages were prepared as described previously [16]. Briefly, peripheral blood mononuclear cells were independently separated from the buffy coat of healthy donors. Monocytes were purified by adherence and were allowed to differentiate for 14 days in Roswell Park Memorial Institute (RPMI) 1640 medium supplemented with 5 ng/mL of recombinant human granulocyte-macrophage colony-stimulating factor and 10% human serum derived from the corresponding blood donors. All cells were cultured at 37°C in 5% CO2.
Viruses
In this study, we used 2 H5N1 viruses with different cytokine induction abilities: A/Vietnam/UT3028II/03 clone 2 (VN3028IIcl2, clade 1) and A/Indonesia/UT3006/05 (IDN3006, clade 2.1.3). Viruses were isolated in MDCK cells, and virus stocks were prepared from the supernatants of MDCK cells.
Plasmid Constructs and Reverse Genetics
Reverse genetics systems for the VN3028IIcl2 and IDN3006 viruses were established as previously described [19]. Briefly, the complementary DNA of genes from these viruses were cloned into the pHH21 vector. The 8 plasmids for the synthesis of viral RNA and 4 expression plasmids for IDN3006 or VN3028IIcl2 virus-derived basic polymerase 2 (PB2), basic polymerase 1 (PB1), acidic polymerase (PA), and nucleoprotein (NP) proteins were transfected into HEK293T cells. Two days later, the supernatant of the transfected cells was harvested and used to infect MDCK cells for the preparation of virus stocks. All virus stocks were sequenced to ensure the absence of unwanted mutations and were titrated by using the plaque assay with MDCK cells prior to use.
Virus Infection of Human Macrophages
Differentiated macrophages were seeded on 24-well plates (BD Falcon), with 1 × 105 cells per well. Cells were infected with viruses at a multiplicity of infection of 2. The virus inoculum was removed, and the cells were washed 3 times and then incubated in serum-free RPMI 1640 medium supplemented with 0.3% bovine serum albumin. At 6, 12, and 24 hours after infection, the supernatant was collected for virus titration and cytokine measurement; the cells were collected for use in viral gene and protein expression assays.
Virus Infection of Human Pulmonary Epithelial Cells
A549 cells were seeded on 6-well plates, with 7.5 × 105 cells per well. Cells were infected with viruses at a multiplicity of infection of 0.0001. The virus inoculum was removed, and the cells were washed 3 times and then incubated in serum-free DMEM supplemented with 0.3% bovine serum albumin. At 6, 12, 24, 48, 72, 96, and 144 hours after infection, viruses in the supernatants were collected and titrated by means of plaque assays in MDCK cells.
Cytokine Measurements
The concentrations of 7 cytokines (interleukin-6 [IL-6], CXCL10 [IP-10], CCL3 [MIP-1α], CCL4 [MIP-1β], CCL5 [RANTES], tumor necrosis factor α [TNF-α], and CXCL9 [MIG]) in supernatants from human macrophages infected with H5N1 viruses were determined by using the Bio-Plex human x-plex (Bio-Rad Laboratories) and by using the Bio-Plex protein array system (Bio-Rad Laboratories) according to the manufacturer's instructions.
RNA Isolation and Integrity
Infected cells were lysed with TRIzol Reagent (Invitrogen), and chloroform-isoamyl alcohol (5:1) was added. The cells were then vortexed and centrifuged for 15 min at 12 000 × g at 4°C. The resulting aqueous layer was subjected to RNA extraction by using RNeasy Mini kit columns (Qiagen) according to the manufacturer's instructions. Isolated total RNA integrity was assessed by determining UV 260/280 absorbance ratios and by examining 28S/18S ribosomal RNA bands with an Agilent 2100 bioanalyzer (Agilent Technologies) according to the manufacturer's instructions. Only samples with high-quality RNA (ie, those with RNA integrity numbers >9.0) were used for microarray analysis.
Microarray Analysis and Bioinformatics
Cy3-labeled complementary RNA probe synthesis was initiated with 50 ng of total RNA by using the Agilent Low Input Quick Amp Labeling kit, one color (Agilent Technologies). The Agilent SurePrint G3 Human GE 8 × 60 K microarrays (G4851) were used according to the manufacturer's instructions. Slides were scanned with an Agilent's High-Resolution Microarray Scanner, and image data were processed by using Agilent Feature Extraction software, version 10.7.3.1. All data were subsequently uploaded into GeneSpring GX, version 11.5, for data analysis. In accordance with proposed MIAME (minimum information about a microarray experiment) standards, microarray data gained in this study are publically available at the Gene Expression Omnibus (GEO) database (http:www.ncbi.nlm.nih.gov/geo/) under the accession number GSE40711. For the microarray data analysis, each gene expression array data set was normalized to the in silico pool for mock-infected cells (n = 3).
Statistically significant differences in gene expression between IDN3006 and VN3028IIcl2 and between IDN3006 and IDN3006/cl2PA were determined by using 1-way analysis of variance (ANOVA) (P < .05) with the Tukey honestly significant difference (HSD) post hoc test and the Benjamini-Hochberg false discovery rate correction. Differentially expressed genes were further filtered to include genes whose expression changed at least 2.0-fold relative to the level in the IDN3006-infected group. Only the genes whose expression showed at least 2.0-fold changes and statistical significance (P < .05) in 2 pairs of comparisons involving IDN3006 versus VN3028IIcl2 and IDN3006 versus IDN3006/cl2PA were assigned to a Gene Ontology group or were uploaded into Ingenuity Pathway Analysis (IPA; Ingenuity Systems) to identify the functions and pathways that were enriched in the gene set. To identify the gene network that enriched the differentially expressed genes, genes were connected in a de novo network based on known interactions in IPA. Genes that were not directly or indirectly connectable to each other were not analyzed further. For all analysis, P values were calculated by using the Fisher exact test to identify biological functions and pathways that were significant (P < .05).
Quantitative Real-Time Polymerase Chain Reaction (PCR) Analysis
Quantitative real-time PCR was performed to determine the expression levels of viral PA, hemagglutinin (HA), NP, matrix (M), and NS genes. RNA was reverse-transcribed with oligonucleotide dT and SuperScript III reverse transcriptase (Invitrogen). Quantitative real-time PCR was conducted with the SYBR Green PCR master mix (Invitrogen) and performed on the ABI7900HT Fast Real-Time PCR System platform. Target gene messenger RNA (mRNA) levels were normalized to 18S human ribosomal RNA according to the 2−ΔΔCt calculation [20]. Primer sequences are available on request.
Western Blotting
Infected cells were lysed with 2 × sample buffer (Invitrogen), and samples were loaded onto precast gels for 4%–20% sodium dodecyl sulfate–polyacrylamide gel electrophoresis (Bio-Rad Laboratories). Proteins were transferred electrophoretically to polyvinylidene fluoride membrane (Millipore) in transfer buffer (100 mM Tris, 190 mM glycine, and 10% methanol). The membranes were blocked for 1 hour at room temperature with Blocking One (Nacalai Tesque) and were then incubated with primary antibodies for 1 hour at room temperature. Anti-PA and anti-NS1 mouse monoclonal antibodies (1:10 000) and anti-H5N1 rabbit polyclonal antibodies (1:10 000) for detection of HA, NP, and M1 were used. After being washed 3 times with phosphate-buffered saline containing 0.05% Tween-20 (PBS-T), the membranes were incubated with anti-mouse (1:10 000) or anti-rabbit (1:10 000) secondary antibodies conjugated with horse radish peroxidase (GE Healthcare) for 1 hour at room temperature. After 3 more washes with PBS-T, specific proteins were detected by using the ECL Prime Western Blotting Detection System (GE Healthcare). Photography was conducted with the VersaDoc Imaging System (Bio-Rad laboratories).
Minigenome Assay
Human macrophages or A549 cells were transfected with the expression plasmids for PB2, PB1, PA, and NP (0.25 μg each), pPoll-NP(0)luc2(0) [21], and ptkRluc (0.025 μg each) by using the jetPEI-Macrophage DNA transfection reagent (Polyplus transfection) or the Lipofectamine LTX and Plus Reagent (Invitrogen), respectively. The cells were then harvested 48 or 24 hours after transfection, respectively. Luciferase activity was assessed by using a dual-luciferase reporter assay system (Promega) according to the manufacturer's instructions. Photinus luciferase activity was standardized against Renilla luciferase activity.
Animal Experiments
Female BALB/c mice aged 5–6 weeks (Japan SLC) were used in the study. To investigate viral pathogenicity in mice, 4 mice per group were anaesthetized with isoflurane and intranasally infected with 50 μL of serial dilutions of viruses, creating doses ranging from 100 to 103 plaque-forming units (PFU). Mice were monitored daily for morbidity and mortality for up to 14 days after infection. The percentage changes in body weights were calculated by comparing the weight of each mouse at each time point to its weight on day 0. The 50% mouse lethal dose for each virus was calculated by using the Reed-Muench method [22]. To determine virus growth in mouse organs, 9 mice per group were intranasally infected with 102 PFU of IDN3006 or IDN3006/cl2PA. Three mice per group were euthanized on days 2, 4, and 7 after infection, and lungs, nasal turbinates, livers, spleens, kidneys, intestines, and brains were collected. Virus in organs was titrated by using plaque assays in MDCK cells.
Statistical Analysis
Statistically significant differences in cytokine expression, virus growth, luciferase activity, and viral mRNA expression were determined by using 1- or 2-way ANOVA with the post hoc Tukey HSD test. In using 2-way ANOVA, we first confirmed that there were no interaction effects between 2 factors, and then we determined whether there were statistically significant differences in virus growth or viral mRNA levels among the viruses during infection. Statistically significant differences in mouse survival were determined by using the log-rank test. For all statistical tests, values were considered to be significantly different when the P value was <.05.
Accession Numbers
The viral nucleotide sequences described in this study are available from GenBank under the following accession numbers: HM114456 for the PA gene of VN3028IIcl2 and JX235398 for IDN3006.
RESULTS
Contribution of the PA Gene to Cytokine Induction in Human Macrophages
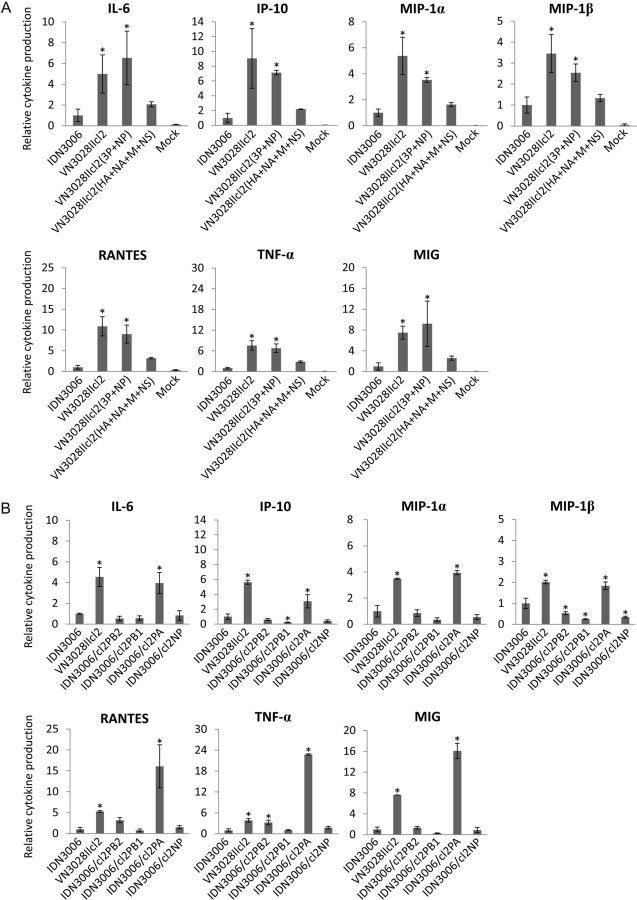
To determine the molecular basis for the induction of cytokines in human macrophages, we used 2 H5N1 viruses that differed in their ability to induce cytokines in human macrophages. We first generated wild-type VN3028IIcl2 (high cytokine inducer) and IDN3006 (low cytokine inducer) by using reverse genetics and confirmed the difference in their abilities to induce cytokines by infecting human monocyte–derived macrophages with them and measuring the expression levels of 7 cytokines (IL-6, IP-10, MIP-1α, MIP-1β, RANTES, TNF-α, and MIG; Figure 1). VN3028IIcl2 induced significantly higher expression levels of all of the cytokines tested than did IDN3006 in human macrophages. To identify the gene segments responsible for the difference in cytokine induction between these 2 viruses, we generated 2 reassortant viruses: VN3028IIcl2(3P + NP), which possesses the polymerase complex genes (PB2, PB1, and PA) and the NP gene from VN3028IIcl2 and its remaining genes from IDN3006, and VN3028IIcl2(HA + NA + M + NS), which possesses the HA, neuraminidase (NA), M, and NS genes from VN3028IIcl2 and its remaining genes from IDN3006. VN3028IIcl2(3P + NP) induced statistically significantly higher expression levels of all of cytokines tested than did IDN3006, whereas VN3028IIcl2(HA + NA + M + NS) did not (Figure 1A). These results indicate that the PB2, PB1, PA, and NP genes contribute to the high cytokine induction property of the VN3028IIcl2 virus in human macrophages.
Figure 1.
Cytokine production in human macrophages. Human monocyte–derived macrophages were infected with a series of reassortants between IDN3006 and VN3028IIcl2 at a multiplicity of infection of 2. At 12 hours after infection, the supernatants of the infected cells were collected, and the concentrations of 7 cytokines (interleukin-6 [IL-6], CXCL10 [IP-10], CCL3 [MIP-1α], CCL4 [MIP-1β], CCL5 [RANTES], tumor necrosis factor α [TNF-α], and CXCL9 [MIG]) were measured. All values were normalized to the value of IDN3006. A, Contributions of a set of 4 viral genes to the cytokine production were evaluated. B, Single viral gene segments responsible for the cytokine induction were determined. The values are means ± SD (n = 3). *P < .05, compared with the IDN3006 group (1-way analysis of variance with the post hoc Tukey honestly significant difference test). Abbreviations: HA, hemagglutinin; M, matrix; NA, neuraminidase; NP, nucleoprotein; NS, nonstructural.
To identify the gene segments responsible for the high cytokine induction among those that encode the proteins in the ribonucleoprotein complex (ie. PB2, PB1, PA, and NP), we generated a series of reassortants possessing a single gene segment derived from VN3028IIcl2 in the IDN3006 backbone (eg, IDN3006/cl2PB2 indicates a virus that possesses the PB2 gene from VN3028IIcl2 and its remaining 7 genes from IDN3006) and evaluated the cytokine expression levels (Figure 1B). The reassortants that possessed the single PB2, PB1, or NP gene from VN3028IIcl2 did not induce cytokine levels similar to those produced by the parental VN3028IIcl2. However, the cytokine expression induced by IDN3006/cl2PA was as high as that induced by VN3028IIcl2; the expression levels of RANTES and TNF-α induced by IDN3006/cl2PA were even statistically significantly higher than those induced by VN3028IIcl2. Thus, the PA gene of VN3028IIcl2 was responsible for the high cytokine induction in human macrophages.
Evaluation of the Effect of Viral Replicative Properties on Cytokine Induction
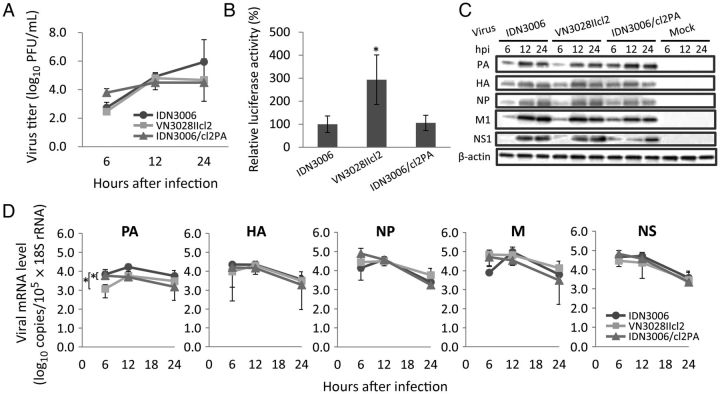
The PA subunit plays a role in virus replication in infected cells [23, 24]. To evaluate whether the high cytokine induction phenotype of VN3028IIcl2 is linked to high viral replication in infected cells, as observed with viruses possessing the PB2-E627K mutation [13], we compared the replication in human macrophages of IDN3006, VN3028IIcl2, and IDN3006/cl2PA (Figure 2) by determining virus titers, polymerase activity, viral protein (PA, HA, NP, M1, and NS1) expression, and viral mRNA gene (PA, HA, NP, M, and NS) expression. Among the 3 viruses tested, there were no statistically significant differences in the virus titers in the supernatants of infected cells, although IDN3006/cl2PA replicated slightly better than IDN3006 or VN3028IIcl2 at 6 hours after infection (Figure 2A). Although VN3028IIcl2 showed statistically significantly higher polymerase activity as compared to IDN3006 (Figure 2B), IDN3006/cl2PA exhibited polymerase activity similar to that of IDN3006, suggesting that the PA gene of VN3028IIcl2 did not substantially affect the polymerase activity. While only PA gene expression was statistically significantly higher in the IDN3006-infected cells as compared to cells infected with VN3028IIcl2 or IDN3006/cl2PA, there were no substantial differences in the expression levels of other viral proteins or genes tested among the 3 viruses (Figures 2C and 2D). Thus, we found no appreciable differences in the viral replicative properties of these 3 viruses even though they differed in their cytokine-inducing abilities in human macrophages. These results indicate that the high cytokine induction by VN3028IIcl2 was not related to efficient virus growth in human macrophages.
Figure 2.
Viral growth properties in human macrophages. Human monocyte–derived macrophages were infected with IDN3006, VN3028IIcl2, or IDN3006/cl2PA at a multiplicity of infection of 2. A, At 6, 12, and 24 hours after infection, the virus titers in the supernatants were determined by means of plaque assays in Madin-Darby canine kidney cells. B, The 4 viral protein expression plasmids (basic polymerase 2 [PB2], basic polymerase 1 [PB1], acidic polymerase [PA], and nucleoprotein [NP]) of IDN3006, VN3028IIcl2, or IND3006/cl2PA together with pPollNP(0)luc2(0) for the production of virus-like RNA encoding the reporter luciferase gene were transfected into human monocyte–derived macrophages and assayed for luciferase activities 48 hours after transfection at 37°C. The values were standardized to the value for the ribonucleoprotein complex protein activity of IDN3006. C and D, Viral proteins (PA, hemagglutinin [HA], NP, matrix [M], matrix 1 [M1], nonstructural [NS], and nonstructural 1 [NS1]; C) and messenger RNA (mRNA; PA, HA, NP, M, and NS; D) expression levels were measured by means of Western blotting and quantitative real-time polymerase chain reaction, respectively. The values are means ± SD (n = 3). *P < .05 among the 3 groups (2-way analysis of variance with the post hoc Tukey honestly significant difference test).
The Role of the PA Gene of VN3028IIcl2 in the Differential Regulation of Host Genes Involved in Hypercytokinemia
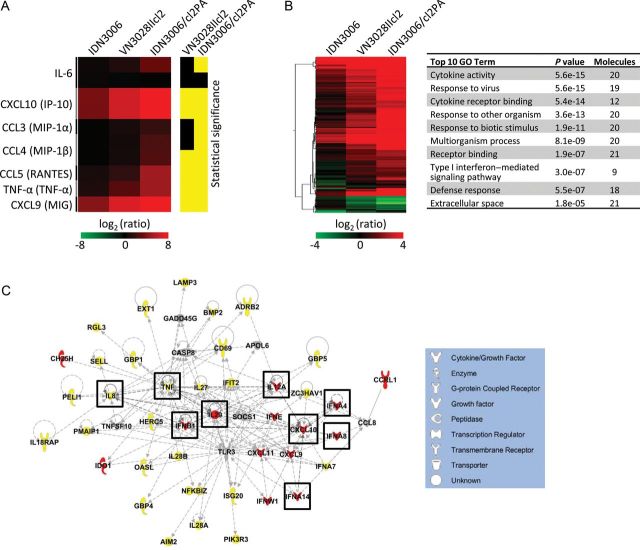
To gain further insights into how the PA gene of VN3028IIcl2 affects cytokine production in human macrophages, we examined all of the gene expression levels in the cells infected with IDN3006, VN3028IIcl2, and IDN3006/cl2PA. The gene expression of IP-10, MIP-1β, RANTES, TNF-α, and MIG confirmed the differential upregulation at the transcriptional level in cells infected with VN3028IIcl2 or IDN3006/cl2PA, compared with those infected with IDN3006 that was observed at the protein level, although the differential upregulation of IL-6 and MIP-1α was confirmed only in cells infected with IDN3006/cl2PA, compared with IDN3006 (Figures 1 and 3A). Microarray analyses further identified 129 genes that were statistically significantly differentially expressed in the human macrophages infected with VN3028IIcl2 and IDN3006/cl2PA as compared to IDN3006 (Supplementary Table 1). Gene Ontology analysis revealed that these genes were enriched with cytokine-related genes (Figure 3B). IPA network analyses identified a gene network composed of 48 genes that were significantly differentially expressed in the macrophages infected with VN3028IIcl2 and IDN3006/cl2PA as compared to IDN3006 (Figure 3C). Of note, this network was enriched with genes related to hypercytokinemia, represented by IFNA4, IFNA8, IFNA14, IFNB1, IL12A, IL29, and CXCL10. These results indicate that the PA amino acid differences are responsible for the differential expression of the various cytokines related to hypercytokinemia at the gene transcriptional level in human macrophages.
Figure 3.
Genes differentially expressed between low and high cytokine inducer H5N1 viruses in human macrophages. Human monocyte–derived macrophages were infected with IDN3006, VN3028IIcl2, or IDN3006/cl2PA at a multiplicity of infection of 2. At 6 hours after infection, the cells were harvested and subjected to microarray analysis. A, Gene expression levels determined by microarray are shown for the 7 cytokines tested in Figure 1. Yellow indicates P < .05, compared with the IDN3006-infected group (1-way analysis of variance [ANOVA] with the Tukey honestly significant difference (HSD) post hoc test). All values were normalized to the values of the mock group. B, A total of 129 genes were selected by 1-way ANOVA with the Tukey HSD post hoc test (P < .05) and by filtering the genes whose expression changed at least 2.0-fold relative to the level in the IDN3006-infected group. The set of genes differentially regulated in both pairs of VN3028IIcl2 and IDN3006/cl2PA as compared to IDN3006 was functionally annotated by means of Gene Ontology (GO) grouping. Statistical significance was determined by using the Fisher exact test (P < .05). C, The differentially expressed genes were connected in a de novo network based on known interactions in the Ingenuity Pathway Analysis (IPA) knowledgebase and functionally annotated by use of IPA canonical pathways. Red indicates genes whose expression showed a change of >4.0-fold for both VN3028IIcl2 and IDN3006/cl2PA, relative to IDN3006. Yellow indicates genes whose expression showed a change of >4.0-fold for IDN3006/cl2PA, relative to IDN3006. The genes enriched with the top canonical pathway of "Role of Hypercytokinemia/hyperchemokinemia in the Pathogenesis of Influenza" are boxed.
Contribution of Cytokine Induction to Pathogenicity in Mice
To examine whether the VN3028IIcl2 PA gene that conferred high cytokine induction is associated with pathogenicity in mammals, we compared the pathogenicity in mice of IDN3006 with that of IDN3006/cl2PA. Four mice per group were infected with 100–103 PFU of each virus, and mortality and morbidity were observed for 14 days after infection (Figure 4). Mice infected with 102 PFU of IDN3006/cl2PA exhibited 100% mortality, whereas 75% of mice infected with IDN3006 survived. However, there were no statistically significant differences in mouse survival at any infectious dose tested. The 50% mouse lethal doses of IDN3006 and IDN3006/cl2PA were 2.1 × 102 and 5.9 PFU, respectively. Thus, there was a trend toward increased virulence in mice for IDN3006/cl2PA, compared with IDN3006, indicating that the VN3028IIcl2 PA contributed to virus pathogenicity in mice. These results suggest that the high cytokine induction phenotype contributes to high pathogenicity in mammals.
Figure 4.
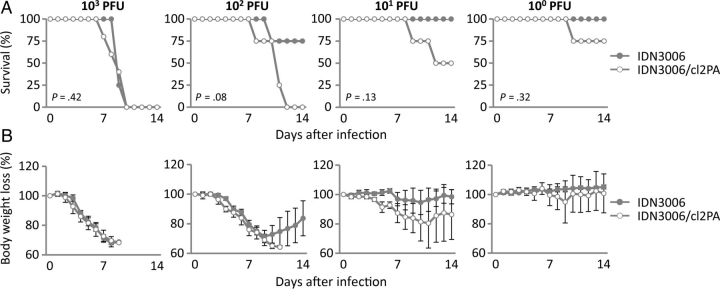
Contribution of the acidic polymerase of VN3028IIcl2 to pathogenicity in mice. Four mice per group were intranasally infected with serially diluted viruses ranging from 100 to 103 plaque-forming units (PFU) of IDN3006 or IDN3006/cl2PA, and survival (A) and body weight changes (B) were monitored daily for 14 days after infection. The values are means ± SD (n = 4) for the mice that were alive at each time point. P values were determined by using the log-rank test for each pair.
DISCUSSION
Here, we demonstrated that the PA gene of an H5N1 virus confers high levels of cytokine expression in human monocyte–derived macrophages. We also showed that PA enhances pathogenicity in mammals without altered virus growth properties in human macrophages.
There are 8 amino acid differences in the PA protein between IDN3006 (low cytokine inducer) and VN3028IIcl2 (high cytokine inducer) (Table 1). Yet, we did not find any PA amino acid residues common to either the high or low cytokine inducers examined in our previous study (Table 1) [16]. Although we attempted to identify the amino acid substitutions responsible for the high cytokine production in macrophages, a single amino acid mutation did not substantially change the cytokine induction level (data not shown), suggesting a synergistic effect among the PA amino acids on cytokine induction. The influenza polymerase complex has a role in inhibiting type I interferon in infected cells [25]. Since the PA amino acid differences tested here did not affect the polymerase activity in human macrophages, the host responses in the infected cells may have been affected by the altered anti-interferon activity of the polymerase complex, possibly mediated by PA or by some as yet unknown function of PA.
Table 1.
Amino Acid Differences in Acidic Polymerase Between IDN3006 and VN3028IIcl2
| Amino Acid | IDN3006 | VN3028IIcl2 | Low Cytokine Inducersa | High Cytokine Inducersa | Known Functionb |
|---|---|---|---|---|---|
| 90 | V | M | V | V/M | … |
| 94 | L | I | L/I | I | … |
| 163 | I | L | I/L | L | cRNA interaction [26] |
| 327 | A | E | A/E | E | … |
| 391 | T | R | T/K | K/R | … |
| 520 | Y | F | Y/F | F | … |
| 594 | G | S | G/S | S | … |
| 653 | S | P | S/P | P | PB1 binding [26] |
Abbreviations: cRNA, complementary RNA; PB1, basic polymerase 1.
a Cytokine induction phenotype was determined in our previous study [16]. Low cytokine inducers include IDN3006 and A/Vietnam/UT31203A/07; high cytokine inducers include VN3028IIcl2 and A/Hong Kong/483/97.
b Functions previously reported to be associated with these amino acid positions.
Virus growth assay revealed that PA was not responsible for the differences between the high and low cytokine inducers with respect to viral transcription, translation, and replication in human macrophages. Interestingly, IDN3006 showed statistically significantly higher growth than IDN3006/cl2PA in human pulmonary epithelial cells (Supplementary Figure 1). Viruses with efficient viral replication in epithelial cells are generally highly pathogenic to mice, represented by viruses with the PB2-E627K mutation, which enhances viral replication in human pulmonary epithelial cells [18]. When we investigated the virus titers in mouse organs, there were no substantial differences between IDN3006 and IDN3006/cl2PA in terms of virus growth in any mouse organ tested (Supplementary Figure 2). Our results, including virus growth, cytokine production, and gene expression in human macrophages, indicate that the ability to induce high levels of cytokines in macrophages, rather than viral replication efficiency in respiratory epithelial cells, may be responsible for enhanced pathogenicity in mice.
In patients infected with H5N1 viruses, high levels of cytokines, represented by MCP-1, MIG, IL-8, IL-10, IL-6, IFN-γ, and RANTES, are generally observed in their sera [6, 9]. Since the PA of a high cytokine inducer was responsible for high levels of these cytokines in macrophages, PA may be a factor in the increased mortality mediated by hypercytokinemia in humans infected with H5N1 viruses. However, both viruses used in this study were isolated from patients who had lethal outcomes, suggesting the involvement of other unknown virulence determinants in the high pathogenicity of H5N1 viruses in humans. Nevertheless, our results have clinical implications for cytokine-mediated pathogenesis in humans infected with H5N1 viruses.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online (http://jid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Acknowledgments. We thank Susan Watson for editing the manuscript.
Financial support. This work was supported by a grant-in-aid for Specially Promoted Research and by the Japan Initiative for Global Research Network on Infectious Diseases from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; by a grant-in-aid of Scientific Research from the Ministry of Health, Labor, and Welfare, Japan; by a grant-in-aid for Exploratory Research for Advanced Technology (ERATO) from Japan Science and Technology Agency (JST), Japan; and by National Institute of Allergy and Infectious Diseases Public Health Service Research grants. S. S. and R. T. were supported by Research Fellowships from the Japan Society for the Promotion of Science for Young Scientists.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Guan Y, Poon LL, Cheung CY, et al. H5N1 influenza: a protean pandemic threat. Proc Natl Acad Sci U S A. 2004;101:8156–61. doi: 10.1073/pnas.0402443101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li KS, Guan Y, Wang J, et al. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature. 2004;430:209–13. doi: 10.1038/nature02746. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Cumulative number of confirmed human cases of avian influenza A(H5N1) reported to WHO. 2012 Geneva: WHO, http://www.who.int/influenza/human_animal_interface/H5N1_cumulative_table_archives/en/index.html . Accessed 10 September 2012. [Google Scholar]
- 4.Hui DS. Review of clinical symptoms and spectrum in humans with influenza A/H5N1 infection. Respirology. 2008;13(Suppl 1):S10–3. doi: 10.1111/j.1440-1843.2008.01247.x. [DOI] [PubMed] [Google Scholar]
- 5.de Jong MD, Bach VC, Phan TQ, et al. Fatal avian influenza A (H5N1) in a child presenting with diarrhea followed by coma. N Engl J Med. 2005;352:686–91. doi: 10.1056/NEJMoa044307. [DOI] [PubMed] [Google Scholar]
- 6.de Jong MD, Simmons CP, Thanh TT, et al. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat Med. 2006;12:1203–7. doi: 10.1038/nm1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdel-Ghafar AN, Chotpitayasunondh T, Gao Z, et al. Update on avian influenza A (H5N1) virus infection in humans. N Engl J Med. 2008;358:261–73. doi: 10.1056/NEJMra0707279. [DOI] [PubMed] [Google Scholar]
- 8.Yuen KY, Chan PK, Peiris M, et al. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet. 1998;351:467–71. doi: 10.1016/s0140-6736(98)01182-9. [DOI] [PubMed] [Google Scholar]
- 9.Peiris JS, Yu WC, Leung CW, et al. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet. 2004;363:617–9. doi: 10.1016/S0140-6736(04)15595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Riel D, Munster VJ, de Wit E, et al. H5N1 virus attachment to lower respiratory tract. Science. 2006;312:399. doi: 10.1126/science.1125548. [DOI] [PubMed] [Google Scholar]
- 11.Cheung CY, Poon LL, Lau AS, et al. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet. 2002;360:1831–7. doi: 10.1016/s0140-6736(02)11772-7. [DOI] [PubMed] [Google Scholar]
- 12.Lee SM, Gardy JL, Cheung CY, et al. Systems-level comparison of host-responses elicited by avian H5N1 and seasonal H1N1 influenza viruses in primary human macrophages. PLoS One. 2009;4:e8072. doi: 10.1371/journal.pone.0008072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mok KP, Wong CH, Cheung CY, et al. Viral genetic determinants of H5N1 influenza viruses that contribute to cytokine dysregulation. J Infect Dis. 2009;200:1104–12. doi: 10.1086/605606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woo PC, Tung ET, Chan KH, Lau CC, Lau SK, Yuen KY. Cytokine profiles induced by the novel swine-origin influenza A/H1N1 virus: implications for treatment strategies. J Infect Dis. 2010;201:346–53. doi: 10.1086/649785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hui KP, Lee SM, Cheung CY, et al. H5N1 influenza virus-induced mediators upregulate RIG-I in uninfected cells by paracrine effects contributing to amplified cytokine cascades. J Infect Dis. 2011;204:1866–78. doi: 10.1093/infdis/jir665. [DOI] [PubMed] [Google Scholar]
- 16.Sakabe S, Iwatsuki-Horimoto K, Takano R, et al. Cytokine production by primary human macrophages infected with highly pathogenic H5N1 or pandemic H1N1 2009 influenza viruses. J Gen Virol. 2011;92:1428–34. doi: 10.1099/vir.0.030346-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monteerarat Y, Sakabe S, Ngamurulert S, et al. Induction of TNF-alpha in human macrophages by avian and human influenza viruses. Arch Virol. 2010;155:1273–9. doi: 10.1007/s00705-010-0716-y. [DOI] [PubMed] [Google Scholar]
- 18.Hatta M, Gao P, Halfmann P, Kawaoka Y. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science. 2001;293:1840–2. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- 19.Neumann G, Watanabe T, Ito H, et al. Generation of influenza A viruses entirely from cloned cDNAs. Proc Natl Acad Sci U S A. 1999;96:9345–50. doi: 10.1073/pnas.96.16.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–8. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 21.Octaviani CP, Goto H, Kawaoka Y. Reassortment between seasonal H1N1 and pandemic (H1N1) 2009 influenza viruses is restricted by limited compatibility among polymerase subunits. J Virol. 2011;85:8449–52. doi: 10.1128/JVI.05054-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reed LJ, Muench H. A simple method of estimating fifty percent end points. Am J Hyg. 1938;27:493–7. [Google Scholar]
- 23.Honda A, Ishihama A. The molecular anatomy of influenza virus RNA polymerase. Biol Chem. 1997;378:483–8. [PubMed] [Google Scholar]
- 24.Huang TS, Palese P, Krystal M. Determination of influenza virus proteins required for genome replication. J Virol. 1990;64:5669–73. doi: 10.1128/jvi.64.11.5669-5673.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iwai A, Shiozaki T, Kawai T, et al. Influenza A virus polymerase inhibits type I interferon induction by binding to interferon beta promoter stimulator 1. J Biol Chem. 2010;285:32064–74. doi: 10.1074/jbc.M110.112458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naffakh N, Tomoiu A, Rameix-Welti MA, van der Werf S. Host restriction of avian influenza viruses at the level of the ribonucleoproteins. Annu Rev Microbiol. 2008;62:403–24. doi: 10.1146/annurev.micro.62.081307.162746. [DOI] [PubMed] [Google Scholar]