Abstract
Birth injury is defined as an impairment of a newborn's body function or structure due to adverse influences that occurred at birth. Phrenic nerve palsy may result from birth trauma during a traumatic neonatal delivery from a stretch injury due to lateral hyperextension of the neck at birth. This could be a rare cause of respiratory distress in the newborn period with irregular respiration. Respiratory distress due to phrenic nerve damage leading to paralysis of the ipsilateral diaphragm may require continuous positive airway pressure or mechanical ventilation and if unresponsive, surgical plication of diaphragm. Herein, we report a case of phrenic nerve palsy in a newborn presenting with respiratory distress.
Keywords: Birth trauma, diaphragmatic paralysis, phrenic nerve palsy, respiratory distress
Introduction
Phrenic nerve damage leading to paralysis of the ipsilateral diaphragm may result from a stretch injury due to lateral hyperextension of the neck at birth. Risk factors include breech and difficult forceps deliveries. Injury to the nerve is thought to occur at the point where it crosses the brachial plexus. Therefore, approximately 75% of the patients also have brachial plexus injury. Phrenic nerve injury with diaphragmatic paralysis must be considered when cyanosis and irregular and labored respirations develop. Diaphragmatic paralysis due to phrenic nerve paralysis may result in significant respiratory compromise, pulmonary infection, growth failure, and even death. This rare cause of respiratory distress of newborn may be missed easily among multiple common etiologies of respiratory distress of newborn if this entity is not kept in mind and thorough examination is not done. These newborn babies may require continuous positive airway pressure (CPAP) or mechanical ventilation and if unresponsive, surgical plication of diaphragm should be performed.
Case Report
Herein, we present the case of a female baby who was preterm, weighed 1.75kg, was appropriate for gestational age, and was born by vaginal delivery with breech presentation. There was no history of the usage of delivery forceps. Antenatal history revealed oligohydramnios. There was a history of second degree consanguineous marriage. The baby cried immediately after birth.
Immediately after birth, the baby developed respiratory distress. Upon examination, it was revealed that cyanosis was present. The baby was started on oxygen and shifted to the Neonatal intensive care unit. Further examination revealed asymmetric Moro reflex. There was Erb's palsy on the right side. The right side of the chest was elevated [Figure 1]. The respiratory movements were diminished on the right side of chest.
Figure 1.

Elevated right side of chest
Sepsis screen was carried out which was negative. X-ray of the chest showed elevation of the right hemidiaphragm [Figures 2 and 3]. Ultrasound abdomen revealed sluggish movements of the right dome of the diaphragm with respiration. The movement of the left dome of the diaphragm was normal.
Figure 2.
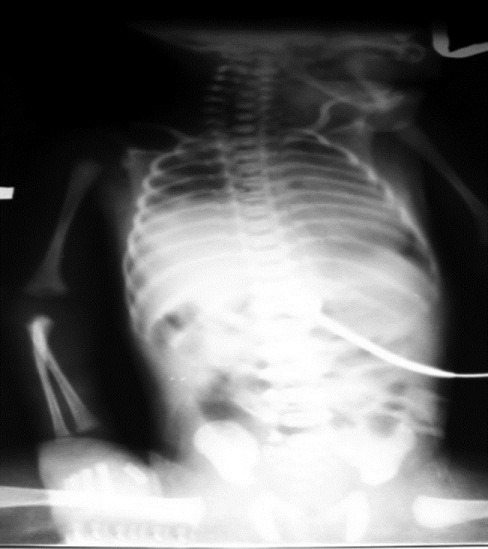
Chest X-ray showing elevated right side of diaphragm
Figure 3.

Another chest X-ray showing elevated right side of diaphragm
The baby was started on CPAP in view of the severe respiratory distress with grunting and cyanosis on the 1st day. Maintenance intravenous fluids were started. The baby was weaned to head box oxygen on the 4th day of life and was started on orogastric tube feeds on the 5th day of life. She required oxygen support for 2 more days. The baby was on complete breast feed by the 7th day of life. She was discharged with advice for physiotherapy and follow-up. The follow-up revealed improvement in the movement of the right upper limb. Normal respiratory movements were present and the baby was feeding normally. X-ray of the chest revealed normal position of the right side of diaphragm and ultrasound showed normal movement of the right hemidiaphragm with respiration.
Discussion
Phrenic nerve damage leading to paralysis of the ipsilateral diaphragm may result from a stretch injury due to lateral hyperextension of the neck at birth. Most cases of diaphragmatic paralysis are unilateral and mostly on the right side. Diaphragmatic paralysis alone in the newborn results in significant respiratory sequelae and failure to thrive.[1] The usual presentation is with respiratory distress, produced largely by over activity of normal hemidiaphragm. In cases of bilateral paralysis, there is cyanosis and poor breathing effort that necessitates mechanical ventilation. Sometimes, diaphragmatic paralysis can be overlooked if thorough examination is not done.[2] Infants are usually large and may have other signs of birth trauma. There is excessive stretching of C3-C5 nerve roots in the neck. Of patients with brachial plexus palsy, a minority had clinically significant diaphragmatic palsy. Majority of the babies with brachial plexus palsy manifested respiratory complications sufficient to warrant diaphragmatic plication (DP). The severity of brachial plexus palsy failed to correlate with the severity of respiratory consequences.[1] Al-Qattan et al. investigated the prognostic value of concurrent phrenic nerve palsy in newborn babies with Erb's palsy. The records of 191 babies with Erb's palsy were reviewed retrospectively in their study. Poor spontaneous return of the motor function of the limb was found for infants both with and without concurrent phrenic nerve palsy. Concurrent phrenic nerve palsy in newborn babies with Erb's palsy has no prognostic value in predicting spontaneous motor recovery of the limb.[3] The diaphragm is an especially important respiratory muscle in the newborn. During sleep, the intercostal muscles are inhibited, because of the supine position of newborn, the diaphragm is pushed upward aggravating respiratory distress.
The diagnosis is suggested on chest radiograph if the right hemidiaphragm is two intercostal spaces higher than left or if the left hemidiaphragm is one intercostal space higher than right. Paradoxical motion or limitation of motion of involved diaphragm may be seen on fluoroscopy or ultrasound examination. Ultrasound examination of the diaphragm and phrenic nerve conduction studies are the diagnostic methods of choice.[4] Basal atelectasis of the lung may be present. This is the reason why some newborn babies improve markedly with CPAP. According to Escande et al., non-invasive nasal CPAP should be proposed for the treatment of phrenic nerve obstetrical palsy before introducing more invasive ventilation techniques.[5] If both the hemidiaphragms are paralyzed, these babies require prolonged mechanical ventilation. These babies improve over a period of 2-3 weeks and further improvement is possible over a period of 2 months. If there is no further improvement and if the newborn cannot be weaned from the ventilator, surgical plication of the diaphragm should be performed. Surgery should be considered after an adequate trial of expectant management in symptomatic patients.[6] Stramrood et al. in his study showed that a minority of infants suffering from diaphragmatic paralysis due to perinatal phrenic nerve injury recover spontaneously. Infants who fail to wean from ventilatory support and undergo early plication have a quick recovery and can be extubated successfully within a few days.[7] Plication of the diaphragm is a safe and useful procedure to improve ventilation in infants with a paralyzed diaphragm. Since this technique does not prevent return of the diaphragmatic function, it should be employed prior to the development of sequelae of prolonged assisted ventilation and sooner if the phrenic nerve is permanently injured.[8] According to de Vries et al., if after 1 month, no spontaneous recovery of the diaphragmatic paralysis caused by a phrenic nerve injury occurs, plication of the diaphragm is indicated. This operation proved to be successful for relief of symptomatic phrenic nerve injury in all cases. If the condition of the patient clinically deteriorates during the 1st month of life, the patient should be operated upon immediately.[9] Traditionally, DP is performed via a thoracotomy that includes incision of the lower intercostal muscles, which are involved in respiratory movement. This may adversely affect ventilation by causing deterioration of respiratory function and making ventilation less efficient. These problems do not occur with thoracoscopic DP, since the lower intercostal muscles are left intact.[10]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Bowerson M, Nelson VS, Yang LJ. Diaphragmatic paralysis associated with neonatal brachial plexus palsy. Pediatr Neurol. 2010;42:234–6. doi: 10.1016/j.pediatrneurol.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Karabiber H, Ozkan KU, Garipardic M, Parmaksiz G. An overlooked association of brachial plexus palsy: Diaphragmatic paralysis. Acta Paediatr Taiwan. 2004;45:301–3. [PubMed] [Google Scholar]
- 3.Al-Qattan MM, Clarke HM, Curtis CG. The prognostic value of concurrent phrenic nerve palsy in newborn children with Erb's palsy. J Hand Surg Br. 1998;23:225. doi: 10.1016/s0266-7681(98)80179-4. [DOI] [PubMed] [Google Scholar]
- 4.Zifko U, Hartmann M, Girsch W, Zoder G, Rokitansky A, Grisold W, et al. Diaphragmatic paresis in newborns due to phrenic nerve injury. Neuropediatrics. 1995;26:281–4. doi: 10.1055/s-2007-979774. [DOI] [PubMed] [Google Scholar]
- 5.Escande B, Cerveau C, Kuhn P, Astruc D, Daemgen F, Messer J. Phrenic nerve paralysis of obstetrical origin: Favorable course using continuous positive airway pressure. Arch Pediatr. 2000;7:965–8. doi: 10.1016/s0929-693x(00)90012-5. [DOI] [PubMed] [Google Scholar]
- 6.Bowman ED, Murton LJ. A case of neonatal bilateral diaphragmatic paralysis requiring surgery. Aust Paediatr J. 1984;20:331–2. doi: 10.1111/j.1440-1754.1984.tb00106.x. [DOI] [PubMed] [Google Scholar]
- 7.Stramrood CA, Blok CA, van der Zee DC, Gerards LJ. Neonatal phrenic nerve injury due to traumatic delivery. J Perinat Med. 2009;37:293–6. doi: 10.1515/JPM.2009.040. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz MZ, Filler RM. Plication of the diaphragm for symptomatic phrenic nerve paralysis. J Pediatr Surg. 1978;13:259–63. doi: 10.1016/s0022-3468(78)80397-2. [DOI] [PubMed] [Google Scholar]
- 9.de Vries TS, Koens BL, Vos A. Surgical treatment of diaphragmatic eventration caused by phrenic nerve injury in the newborn. J Pediatr Surg. 1998;33:602–5. doi: 10.1016/s0022-3468(98)90325-6. [DOI] [PubMed] [Google Scholar]
- 10.Shimizu M. Bilateral phrenic nerve paralysis treated by thoracoscopic diaphragmatic plication in a neonate. Pediatr Surg Int. 2003;19:79–81. doi: 10.1007/s00383-002-0737-z. [DOI] [PubMed] [Google Scholar]


