Abstract
The need for consistent and current data describing the true incidence of SCA and/or SCD was highlighted during the most recent Sudden Cardiac Arrest Thought Leadership Alliance’s (SCATLA) Think Tank meeting of national experts with broad representation of key stakeholders including thought leaders and representatives from the American College of Cardiology, American Heart Association, and the Heart Rhythm Society. As such, to evaluate the true magnitude of this public health problem, we performed a systematic literature search in MEDLINE using the MeSH headings, “death, sudden” OR the terms “sudden cardiac death” OR “sudden cardiac arrest” OR “cardiac arrest” OR “cardiac death” OR “sudden death” OR “arrhythmic death.” Study selection criteria included peer-reviewed publications of primary data used to estimate SCD incidence in the U.S. We used Web of Science®’s Cited Reference Search to evaluate the impact of each primary estimate on the medical literature by determining the number of times each “primary source” has been cited. The estimated U.S. annual incidence of SCD varied widely from 180,000 to > 450,000 among 6 included studies. These different estimates were in part due to different data sources (with data age ranging from 1980 to 2007), definitions of SCD, case ascertainment criteria, methods of estimation/extrapolation, and sources of case ascertainment. The true incidence of SCA and/or SCD in the U.S. remains unclear with a wide range in the available estimates, which are badly dated. As reliable estimates of SCD incidence are important for improving risk stratification and prevention, future efforts are clearly needed to establish uniform definitions of SCA and SCD and then to prospectively and precisely capture cases of SCA and SCD in the overall U.S. population.
Keywords: sudden cardiac arrest, sudden cardiac death, incidence
In the United States, cardiovascular disease was the underlying cause of one of every 2.9 deaths occurring in 2006(1). The proportion of these deaths that is sudden has been estimated to be as high as 50%, making sudden cardiac death (SCD) the most common cause of death in this country(2). Studies are available that provide consistent data on survival after sudden cardiac arrest (SCA)(3,4), and several randomized controlled trials offer reliable information on therapies for the prevention of SCD in highly selected, high-risk subgroups(5–11). Nevertheless, data describing the incidence of SCA and/or SCD in the overall U.S. population appear to be inconsistent making it difficult to determine the actual magnitude of this problem. Published estimates of SCA and/or SCD incidence in the U.S. vary widely depending on the source(12). Another major issue limiting the ability to determine the true magnitude of SCD is the lack of consensus on its definition and appropriate designation. Not only are SCD and SCA often used interchangeably despite having two distinct definitions, an agreement on the best definition for these entities is yet to be reached. Subtleties inherent in these clinical definitions have far-reaching public health implications, as they affect the ability to meaningfully discuss these clinical outcomes, and reach any conclusions about their magnitude.
The need for consistent and current data describing the true incidence of SCA and/or SCD was highlighted during the most recent Sudden Cardiac Arrest Thought Leadership Alliance’s (SCATLA) Think Tank meeting in Washington, DC, that convened a group of national experts with broad representation of key stakeholders including thought leaders and representatives from the American College of Cardiology (ACC), American Heart Association (AHA), and the Heart Rhythm Society (HRS). As a result, In this study, we systematically evaluate the sources of the wide range of published estimates for the incidence of SCA and/or SCD. In addition, we propose recommendations to facilitate a more reliable estimation of SCA and/or SCD incidence, which will advance our knowledge and the development of public awareness, education, and prevention.
METHODS
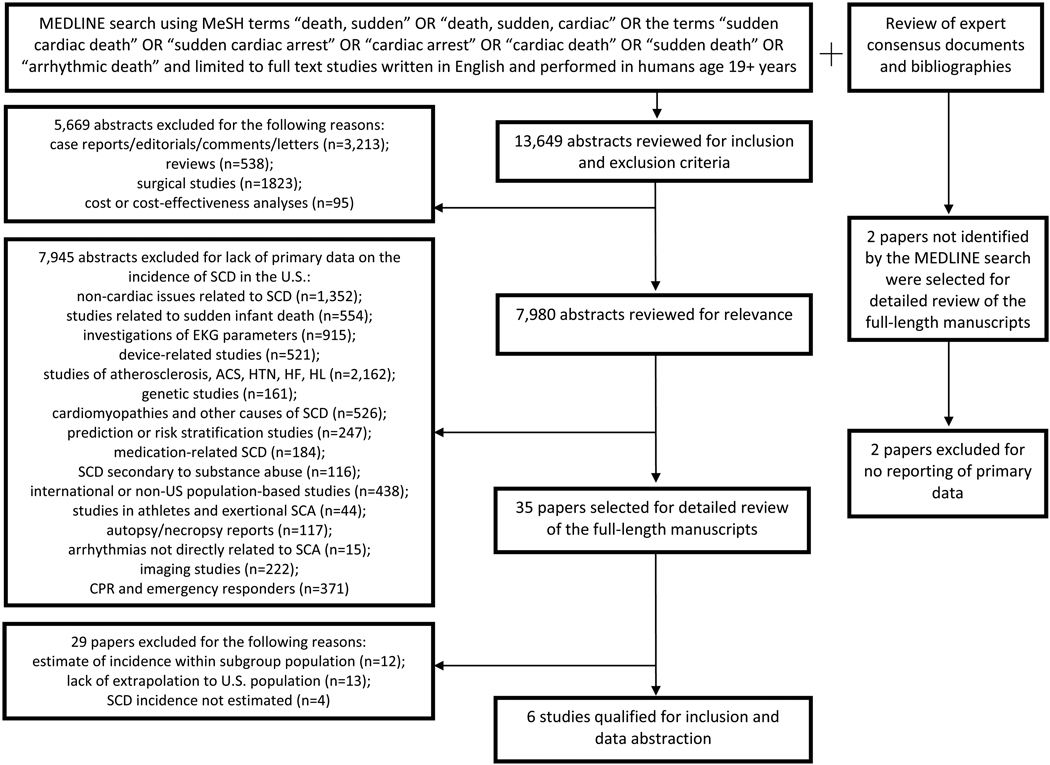
To find estimates of the incidence of SCA and/or SCD, a systematic literature search was performed in MEDLINE using the MeSH headings, “death, sudden” OR “death, sudden, cardiac” OR the terms “sudden cardiac death” OR “sudden cardiac arrest” OR “cardiac arrest” OR “cardiac death” OR “sudden death” OR “arrhythmic death.” Study selection criteria included peer-reviewed publications of primary data used to estimate the incidence of SCD in the U.S. Studies that did not report primary data and/or were not performed in a U.S. population were excluded.
Of the 13,649 abstracts that resulted from the comprehensive search strategy, the vast majority were excluded for the reasons detailed in Figure 1. Thirty-five full-length, peer-reviewed, publications were selected for full review, which yielded 6 studies providing primary data used to derive an estimated annual incidence of SCD in the U.S.(13–18) The study by Chugh et al. published in 2004 provides primary data for a count estimate of SCD; however, an estimated annual incidence of SCD in the U.S. is only presented in a subsequent paper published by Chugh et al. in 2008(16,19). As such, we included the 2004 study and cited additional data from the 2008 study. Review of expert consensus documents including the American College of Cardiology/American Heart Association/European Society of Cardiology (ACC/AHA/ESC) 2006 Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death and bibliographies identified 2 additional sources for the estimate of the incidence of SCA and/or SCD; however both were excluded due to lack of primary data(2,20). Given the wide range of estimated incidences of SCA and/or SCD cited in the literature despite the small number of primary sources providing such estimates, to obtain a sense of the degree of data dissemination in the medical literature we used the Web of Science®’s Cited Reference Search tool to determine the number of times each of these “primary sources” has been cited.
Figure 1.
Systematic Literature Review Search Flow-Diagram
RESULTS
Estimates of SCA and/or SCD Incidence
Despite a very broad search strategy, only 6 publications have reported estimates of the incidence of SCA and/or SCD in the U.S. derived from primary data (Table 1)(13–18). Estimations of SCA and/or SCD incidence ranged widely from 180,000 to >450,000(16,17). The oldest study was published in 1989, using National Center for Health Statistics (NCHS) and death certificate data from 1980–1985(13). The most recent study was published in 2008 using data collected between May 1, 2006 and April 30, 2007 from 10 North American sites (8 US sites) that was subsequently extrapolated to the U.S. population(18).
Table 1.
Published estimates of the annual incidence of SCD in the U.S.
| Source | Definitional equivalents of SCA and/or SCD |
Estimated annual incidence of SCD |
Proportion of sudden deaths considered SCD |
Method of estimation |
Dates data collected for estimate |
Publicati on Date |
|---|---|---|---|---|---|---|
| Gillum, RF(13) |
SCD = sudden coronary death, defined as “deaths attributed to ischemic heart disease occurring out-of-hospital or in emergency rooms.” |
223,864 | 56% | Based on national level data (from 40 states) |
1980–1985 | 1989 |
| Escobed o, et al.(14) |
SCD = sudden coronary death, defined as “coronary heart disease deaths in persons dying within 1 hour of onset of cardiovascular symptoms.” |
251,000 | 48% | Based on national level data (except Oregon) |
1980 and 1986 |
1996 |
| Zheng, et al.(17) |
SCD = sudden cardiac death, defined as “the sudden, unexpected natural death from a cardiac cause a short time (generally ≤1 hour) after the onset of symptoms in a person without any previous condition that would seem fatal” or “any cardiac death occurring out of the hospital or taking place in the emergency room or dead on arrival in the emergency room.” |
456,076 | 63.3% | Based on national level data |
1989–1998 | 2001 |
| Cobb, et al.(15) |
All cardiac arrest cases with presumed cardiac etiology who received advanced life support from Seattle Fire Department emergency medical services. |
184,000 | NR | Extrapolated from community study (Seattle, Washington) |
During specified periods between 1979–2000 |
2002 |
| Chugh, et al 2004 (16) and Chugh, et al 2008 (19)* |
SCD = sudden cardiac death, defined using the World Health Organization criteria as “sudden unexpected death either within 1 h of symptom onset (event witnessed), or within 24 h of having been observed alive and symptom free (unwitnessed).” Survivors of cardiac arrest were also included under SCD cases. |
180,000– 250,000 |
NR | Extrapolated from community study (Multnomah County, Oregon) |
2002–2003 | 2004 |
| Nichol, et al 2008(18) |
Cardiac arrest cases that occurred outside the hospital, were evaluated by EMS and either (1) received attempts at external defibrillation or chest compressions by organized EMS or (2) were pulseless but did not receive CPR or attempts to defibrillate by EMS. |
294,851 (quasi confidence interval, 236,063 – 325,007) |
NR | Extrapolated from 8 US sites (Alabama, Iowa, Dallas, Texas, Milwaukee, Wisconsin, Pittsburgh, Pennsylvania, Portland, Oregon, Seattle, Washington) |
2006–2007 | 2008 |
CPR = cardiopulmonary resuscitation; EMS = emergency medical services; NR = not reported
A count estimate is not provided in Chugh, et al., 2004, but is extrapolated and reported in Chugh, et al., 2008.
Methods of estimation differed among studies. Two studies extrapolated estimates of national annual incidence of SCA and/or SCD based on smaller community-based studies(15,16). One study used registry data from 8 different sites in the US to extrapolate a national annual incidence(18). The 3 remaining studies used national level data to provide estimates(13,14,17); however, one of these studies reported only data from the 40 states that reported data to the NCHS(13).
Differences in Definitions
The stated definitions of SCA and/or SCD varied across the 6 studies (Table 1). Three studies included time constraints in their case definitions for SCD(14,16,17). Four sources included a geographical location of the event as part of the case definition(13,15,17,18). While 2 studies specifically defined SCD as death attributable to ischemic or coronary heart disease(13,14), the other studies broadened their criteria to include death from a cardiac or cardiovascular etiology(15–18). One study included “survivors of cardiac arrest” in their case definition of SCD(16) and the most recent study also specifically examined out-of-hospital cardiac arrest and included deaths as well as patients who survived to hospital discharge(18).
Differences in Case Ascertainment
Reflecting the variation in definitions of SCA and SCD among these primary sources, the derivation methodologies for each study were also different (Table 2). The age cut-off for the studied population was highly variable. Two studies used an age cut-off ≥25 years(13,14); one study used an age cut-off ≥35 years(17); and another study used age ≥20 years(15). The two most recent studies did not specify any age criteria(16,18).
Table 2.
Case Ascertainment Criteria and Sources
| Case ascertainment criteria |
|||||||
|---|---|---|---|---|---|---|---|
| Source | Time | Geograph y |
Disease Attributio n |
Witnessed or Unwitness ed |
Age | SCA include d |
Sources for case ascertainment |
| Gillum, RF(13) |
Not specified |
Out-of- hospital or in the emergenc y room |
Ischemic heart disease |
Not specified |
≥25 years old |
no | 1) National Center for Health Statistics (NCHS) data from the 40 states that reported data 2) US standard certificate of death, item 7c* |
| Escobedo, et al.(14) |
≤ 1 hr of onset of cardio- vascular symptoms |
Not specified |
Coronary heart disease |
Not specified |
≥25 years old |
no | 1) 1986 National Mortality Followback Survey (did not include data from Oregon or patients < 25 years old)† 2) 1980 US Bureau of the Census data 3) Death certificates (death considered to have resulted from coronary heart disease if death certificate listed rubrics 410 through 414 International Classification of Diseases, 9th revision) 4) Additional information obtained through questionnaire/interview of person identified as the informant on death certificate (89% of informants responded) |
| Zheng, et al.(17) |
≤1 hour of symptoms |
Out-of- hospital or in the emergenc y room or “dead on arrival” with underlying cause of death reported as cardiac disease |
Cardiac disease death |
Not specified |
≥ 35 years old |
no | 1) NCHS data 2) Death certificates (death considered to have resulted from cardiac disease if underlying cause of death classified using ICD-9 codes 390–398, 402, or 404–429) |
| Cobb, et al.(15) |
Not specified |
Out-of- hospital |
Cardiac cause |
Witnessed or unwitnesse d |
≥ 20 years old |
no | 1)Medical incident reports submitted by fire department paramedics for all patients who received advanced life support by Seattle Fire Department/EMS personnel 2) Any missing data from above obtained from death certificates or hospital admission forms* |
| Chugh, et al,. 2004(16) and Chugh, et al., 2008(19) |
≤1 hour of symptoms if witnessed or ≤24 hrs if unwitness ed |
Not specified |
Cardiac cause |
Witnessed or unwitnesse d |
No age criteria |
yes | 1) Case ascertainment from EMS system (78%), county medical examiner’s office (20%), and 16 area hospitals (2%). Of 353 cases, 280 identified by EMS; 68 by medical examiner; and 5 by hospital or provider 2) Postmortem exam performed at discretion of medical examiner or physician 3) Death certificate data from Oregon State Health Division 4) Available medical records |
| Nichol, et al., 2008(18) |
Not specified |
Out-of- hospital |
Cardiac cause |
Not specified |
No age criteria (infants , childre n, and adults all include d) |
yes | 1) Resuscitation Outcomes Consortium (ROC), a clinical research network consisting of 11 sites and 1 central coordinating center, conducting clinical research on cardiopulmonary arrest and traumatic injury. ROC created a registry, ROC Epistry-Cardiac Arrest, which is a prospective, multicenter, observational registry of out-of-hospital arrests in EMS agencies and 11 institutions (8 US, 3 Canadian) 2) Multiple case ascertainment strategies used: telephone notification of each incident defibrillator use or CPR by EMS, hand sorting through paper EMS charts, electronic queries of EMS records using various data fields such as dispatch type, vital signs, or diagnosis, |
CPR = cardiopulmonary resuscitation; EMS = emergency medical services; ICD = International Classification of Diseases
% of data from each source not provided
The National Mortality Followback Survey is described as a random sample of 1% of U.S. resident deaths (except residents of Oregon) age 25 years or older in 1986(27).
Five studies used death certificate data in addition to other survey or report data including the NCHS, the National Mortality Followback Survey, U.S. Bureau of the Census data, and emergency medical services reports(13–17). In contrast, the study by Nichol, et al. assesses out-of-hospital cardiac arrest incidence and outcomes and did not use death certificates to determine mortality, but used case-fatality rates from a registry(18). When vital status data were missing, the authors used multiple imputation methods to determine mortality rates(18). Only two studies used prospective case ascertainment(16,18).
Dissemination of Data from Primary Sources
Despite the markedly heterogeneous SCA- and/or SCD-equivalent definitions and methods of estimation, all of these articles have been cited as sources of estimates for the incidence of SCA and/or SCD in the U.S. Four of the six source articles identified by our MEDLINE search were also referenced in the ACC/AHA/ESC 2006 Guidelines(12–15,17); however, the Guidelines cited 2 additional studies as primary data sources for the wide ranging estimates of SCD incidence in the U.S.(2,20) As these citations were selected by the Writing Committee to Develop Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death, they represent expert consensus on the best source documents providing information on the incidence of SCA and/or SCD. The oldest reference was published in 1989(13) and the most current source was published in 2004(20); however, two of the sources cited by the guidelines were not primary derivations of the estimated incidence of SCA and/or SCD(2,20).
These documents have been widely cited in the published body of peer-reviewed literature (Table 3). The most often cited source was published almost a decade ago using U.S. vital statistics and death certificate data from 1989 to 1998(17), but has been cited 400 times from March 2002–most recently in November 2009. The next most cited source was published in 1993 and does not provide primary data from which an estimated incidence of SCD was derived, but instead states that “estimates are based on published epidemiologic and clinical data”(2). Finally, the third most often cited source was published in 1989 based on death certificates and data from the NCHS collected from 1980 to 1985—thirty years ago(13).
Table 3.
Additional sources cited by the ACC/AHA/ESC 2006 Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death
| Source | Definitional equivalents of SCA or SCD |
Estimated incidence of SCD (no primary data presented)* |
Sources for estimate | Publicati on Date |
|---|---|---|---|---|
| Myerburg et al.(2) |
Sudden cardiac death defined as “cardiovascular deaths that are sudden and unexpected.” |
300,000 | 1) Reported “estimates are based on published epidemiologic and clinical data” with two citations: a) Myerburg RJ, Castellanos A. Cardiac arrest and sudden cardiac death. In: Braunwald E: ed. Heart Disease: A Textbook of Cardiovascular Medicine, 4th ed. Philadelphia: W.B. Saunders; 1992:756–89; b) Myerburg RJ, Kessler KM, Castellanos A. Sudden cardiac death. Structure, function, and time-dependence of risk. Circulation. 1992;85(Suppl 1):I2–10. |
1993 |
| AHA Heart Disease and Stroke(20) |
SCD = sudden cardiac death, defined as “sudden cardiac deaths from coronary disease.” |
335,000 | 1) Only sources listed are ICD-9 codes 427.4 and ICD-10 code I49.0* |
2004 |
ICD = International Classification of Diseases
No primary data presented in publication.
DISCUSSION
There are 2 main findings for this study: 1) definitions of SCA and SCD are not standardized across the medical community; and 2) the true incidence of SCA and/or SCD in the U.S. population remains unclear.
The widely ranging estimates published in the few studies that have tackled this question highlight the lack of clarity about the true annual incidence of SCA and/or SCD in the U.S. By extension, discrepancies in published estimates reflect inconsistencies in the medical community’s knowledge and understanding of SCD.
Multiple and sometimes discordant case definitions are used to describe SCA, which is often incorrectly used interchangeably with SCD in the literature. To date, there is no standardized, universal definition used uniformly across the large numbers of studies of this clinical entity. Confusion surrounding the definition of “sudden cardiac death” starts with the fundamentally complex nature of the entity we are attempting to capture within the constraints of the English lexicon, i.e., what counts as “sudden”? What qualifies as “cardiac”? Does “sudden” and “cardiac” refer to “death” and/or resuscitated “death”? These definitional issues have been recognized and numerous definitions have been put forth over the last half century; however, no single, “all-purpose” definition has emerged in light of the myriad, often multifactorial, etiologies of SCD(21,22). Rather than propose a universal definition of SCD, the World Health Organization Scientific Group on SCD wrote in 1985 that it is “more meaningful to define the specific characteristics surrounding cardiac arrest, and register and collect data in a standardized way, than to try to define the word ‘sudden’ in the context of death.”(21) According to the ACC/AHA/ESC 2006 Guidelines, SCA is defined as “death from an unexpected circulatory arrest, usually due to a cardiac arrhythmia occurring within an hour of the onset of symptoms, in whom medical intervention (e.g., defibrillation) reverses the event”(12). SCD is defined as “death from an unexpected circulatory arrest, usually due to a cardiac arrhythmia occurring within an hour of the onset of symptoms”(12).
There are a number of possible reasons that the annual incidence of SCA and/or SCD in the U.S. remains unclear. To begin, there are few studies focused on answering this question, and among this handful of studies, most are old, dependent on death certificate data, and not prospective. Across studies there was significant variation in case definitions of SCD and methods of case ascertainment.
Instead of prospective case ascertainment, most of the available estimates are based on retrospective death certificate-based methodology. Death certificate data do not account for survived SCA and have been demonstrated in validation studies to overestimate the incidence of SCD(23–25). The study providing the highest estimate of annual SCD incidence (>450,000) used only death certificate-based retrospective surveillance(17) compared with the more recent prospective study that provides a range that included the lowest estimate (180,000–250,000) and employed multiple methods of case ascertainment(16). Additional difficulties stemming from these estimates’ dependence on death certificate data are the lack of uniform designation of cause of death on the certificate(26). On death certificates, SCD is often listed as the primary cause of death even when the patient had multiple comorbidities that may have directly contributed to death. Like death certificate data, other sources of retrospective case ascertainment such as vital statistics and census data also misclassify and can overestimate SCD(26). Finally, the prospective, community-based studies, used data from first-responders, which results in the inherent exclusion of unwitnessed SCA and/or SCD.
From a public health perspective, the ability to reliably estimate the incidence of SCA and/or SCD in the U.S. is important because it informs our efforts to prevent SCD, to improve risk stratification techniques, and to direct future research that may save lives. Based on our findings from this review of the literature, we recommend three actionable next-steps toward addressing our knowledge and data gaps:
- Establish precise, uniform definitions of SCA and of SCD, to be agreed upon and adopted by the major stakeholders in the medical/scientific community. SCA and SCD should have two distinct definitions that should not be used interchangeably, as SCA includes a subset of potentially lethal events that are reversed with medical intervention. We support the definitions put forth by the ACC/AHA/ESC 2006 Guidelines that state:
- Sudden cardiac arrest: “an unexpected circulatory arrest, usually due to a cardiac arrhythmia occurring within an hour of the onset of symptoms, in whom medical intervention (e.g., defibrillation) reverses the event”(12).
- Sudden cardiac death: “death from an unexpected circulatory arrest, usually due to a cardiac arrhythmia occurring within an hour of the onset of symptoms”(12).
Perform larger, multicenter, prospective studies in the general population as well as across different geographic regions and races, using the above definitions to facilitate optimal case ascertainment. The Resuscitation Outcomes Consortium (ROC) is a clinical research network of 11 sites and 1 central coordinating center in addition to its companion prospective, multicenter, observational registry of the 11 sites (ROC Epistry-Cardiac Arrest) established to evaluate out-of-hospital cardiac arrest and resuscitation outcomes in the participating geographic regions.(18) One potential approach for achieving more reliable national estimates of SCA and SCD could be based on an expansion of the ROC and ROC-ECA design, establishing a national SCA and SCD research network comprised of 40–50 emergency medical services agencies with a central receiving institution selected to be nationally representative.
Integrate multiple source methods for case ascertainment to capture more cases and rule out those cases that do not meet strict criteria according to the definitions determined above. Using multiple sources to confirm cases of SCA and/or SCD will help to minimize dependence on death certificate data.
It is hoped this initial framework will help to put in place the necessary elements enabling us to fill in data gaps on this important public health issue. Establishing definitional agreement in the medical community and in the literature will facilitate the more reliable evaluation and comparisons of therapies, utilization, and outcomes, which will ultimately enhance our strategies for risk stratification and prevention of SCD. Given the paucity of studies providing current data on the annual incidence of SCD in the U.S., these findings highlight the need for additional contemporaneous studies to be performed prospectively and to integrate multiple methods of case ascertainment to determine the true incidence of SCD in the U.S. Consideration should be given to create a national surveillance system to assess the characteristics, treatments, and outcomes of patients with SCA; facilitate efforts to improve the quality of resuscitation and SCA patient care; and implement research findings and evidence-based recommendations into clinical practice.
Conclusions
The true incidence of SCA and/or SCD in the U.S. remains unclear with a wide range in available estimates. In order to advance knowledge and understanding of the epidemiology of SCD and improve risk stratification and prevention, there needs to be a focused effort to create a standard definition of SCA and SCD and expand national research efforts to precisely capture cases of SCA and SCD prospectively and more broadly across communities.
Supplementary Material
Table 4.
Measure of Impact and Data Dissemination
| References | Number of citations found by Web of Science®’s Cited Reference Search (dates of publications citing each reference) |
|---|---|
| Sources with estimate derived from primary data | |
| Gillum, RF (1989)(13) | 197 (Jan 1990 – Nov 2009) |
| Escobedo, et al. (1996)(14) | 59 (Apr 1997 – Sept 2009) |
| Zheng, et al. (2001)(17) | 400 (Mar 2002 – Nov 2009) |
| Cobb, et al. (2002)(15) | 161 (Dec 2002 – Nov 2009) |
| Chugh, et al. (2004)(16) Chugh, et al. (2008)(19) |
74 (Jan 2005 – Nov 2009) 9 (Jun 2009 – Nov 2009) |
| Nichol, et al., (2008)(18) | 67 (Sept 2008 – April 2010) |
| Sources with estimates not derived from primary data, but cited by the 2006 ACC/AHA/ESC Guidelines | |
| Myerburg, et al. (1993)(2) | 207 (Dec 1993 – Dec 2009) |
| AHA Heart Disease and Stroke (2004)(20) | Not available |
ABBREVIATIONS
- ACC
American College of Cardiology
- AHA
American Heart Association
- ESC
European Society of Cardiology
- NCHS
National Center for Health Statistics
- SCA
sudden cardiac arrest
- SCD
sudden cardiac death
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
Melissa H. Kong: Receives research funding from Biotronik and was supported by a Ruth L. Kirschstein-National Research Service Award (Kirschstein-NRSA) National Institutes of Health (NIH) [grant number 5-T32-DK-007731-15]. The contents of this work are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Gregg C. Fonarow: Receives research funding from National Heart Lung and Blood Institute; serves as a consultant for Novartis, Medtronic, and St. Jude Medical; and receives honorariums from GlaxoSmithKline, St. Jude Medical, and Medtronic.
Eric D. Peterson: None reported.
Anne B. Curtis: Receives research funding from Medtronic and St. Jude Medical; consulting, speakers’ bureau, and/or fellowship support from Medtronic, St. Jude Medical, Biotronik, Sanofi-Aventis, and Biosense Webster.
Adrian F. Hernandez: Receives research funding from Johnson & Johnson and honorarium from Medtronic.
Gillian D. Sanders: None reported.
Kevin L. Thomas: None.
David L. Hayes: Serves on an advisory board for St. Jude Medical, Boston Scientific, and Pixel Velocity and receives honoraria for speaking from St. Jude Medical, Boston Scientific, Medtronic, Sorin Medical, Biotronik, Blackwell-Futura.
Sana M. Al-Khatib: None.
REFERENCES
- 1.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Myerburg RJ, Kessler KM, Castellanos A. Sudden cardiac death: epidemiology, transient risk, and intervention assessment. Ann Intern Med. 1993;119:1187–1197. doi: 10.7326/0003-4819-119-12-199312150-00006. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg RJ, Gorak EJ, Yarzebski J, et al. A communitywide perspective of sex differences and temporal trends in the incidence and survival rates after acute myocardial infarction and out-of-hospital deaths caused by coronary heart disease. Circulation. 1993;87:1947–1953. doi: 10.1161/01.cir.87.6.1947. [DOI] [PubMed] [Google Scholar]
- 4.Chan PS, Nichol G, Krumholz HM, et al. Racial differences in survival after in-hospital cardiac arrest. JAMA. 2009;302:1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. N Engl J Med. 1997;337:1576–1583. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]
- 6.Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 7.Connolly SJ, Gent M, Roberts RS, et al. Canadian implantable defibrillator study (CIDS) : a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation. 2000;101:1297–1302. doi: 10.1161/01.cir.101.11.1297. [DOI] [PubMed] [Google Scholar]
- 8.Kadish A, Dyer A, Daubert JP, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004;350:2151–2158. doi: 10.1056/NEJMoa033088. [DOI] [PubMed] [Google Scholar]
- 9.Moss AJ, Hall WJ, Cannom DS, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N Engl J Med. 1996;335:1933–1940. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 10.Kuck KH, Cappato R, Siebels J, Ruppel R. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest : the Cardiac Arrest Study Hamburg (CASH) Circulation. 2000;102:748–754. doi: 10.1161/01.cir.102.7.748. [DOI] [PubMed] [Google Scholar]
- 11.Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 12.Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e385–e484. doi: 10.1161/CIRCULATIONAHA.106.178233. [DOI] [PubMed] [Google Scholar]
- 13.Gillum RF. Sudden coronary death in the United States: 1980–1985. Circulation. 1989;79:756–765. doi: 10.1161/01.cir.79.4.756. [DOI] [PubMed] [Google Scholar]
- 14.Escobedo LG, Zack MM. Comparison of sudden and nonsudden coronary deaths in the United States. Circulation. 1996;93:2033–2036. doi: 10.1161/01.cir.93.11.2033. [DOI] [PubMed] [Google Scholar]
- 15.Cobb LA, Fahrenbruch CE, Olsufka M, Copass MK. Changing incidence of out-of-hospital ventricular fibrillation, 1980–2000. JAMA. 2002;288:3008–3013. doi: 10.1001/jama.288.23.3008. [DOI] [PubMed] [Google Scholar]
- 16.Chugh SS, Jui J, Gunson K, et al. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–1275. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 17.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–2163. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 18.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chugh SS, Reinier K, Teodorescu C, et al. Epidemiology of sudden cardiac death: clinical and research implications. Prog Cardiovasc Dis. 2008;51:213–228. doi: 10.1016/j.pcad.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Heart Association. Heart Disease and Stroke Statistics-2005 Update. Dallas, TX: American Heart Association; 2004. [Google Scholar]
- 21.WHO Scientific Group on Sudden Cardiac Death Technical Report Series 726 (World Health Organization) Geneva: World Heatlh Organization; 1985. p. 28. [PubMed] [Google Scholar]
- 22.Roberts WC. Sudden cardiac death: definitions and causes. Am J Cardiol. 1986;57:1410–1413. doi: 10.1016/0002-9149(86)90229-8. [DOI] [PubMed] [Google Scholar]
- 23.Iribarren C, Crow RS, Hannan PJ, Jacobs DR, Jr, Luepker RV. Validation of death certificate diagnosis of out-of-hospital sudden cardiac death. Am J Cardiol. 1998;82:50–53. doi: 10.1016/s0002-9149(98)00240-9. [DOI] [PubMed] [Google Scholar]
- 24.Every NR, Parsons L, Hlatky MA, et al. Use and accuracy of state death certificates for classification of sudden cardiac deaths in high-risk populations. Am Heart J. 1997;134:1129–1132. doi: 10.1016/s0002-8703(97)70035-8. [DOI] [PubMed] [Google Scholar]
- 25.Goraya TY, Jacobsen SJ, Belau PG, Weston SA, Kottke TE, Roger VL. Validation of death certificate diagnosis of out-of-hospital coronary heart disease deaths in Olmsted County, Minnesota. Mayo Clin Proc. 2000;75:681–687. doi: 10.4065/75.7.681. [DOI] [PubMed] [Google Scholar]
- 26.Fox CS, Evans JC, Larson MG, Kannel WB, Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: the Framingham Heart Study. Circulation. 2004;110:522–527. doi: 10.1161/01.CIR.0000136993.34344.41. [DOI] [PubMed] [Google Scholar]
- 27.Seeman I, Poe GS, McLaughlin JK. Design of the 1986 National Mortality Followback Survey: considerations on collecting data on decedents. Public Health Rep. 1989;104:183–188. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.