Abstract
Objective
To determine the contribution of infants born at the threshold of viability (defined as <750 g birth weight) and the role of regionalization of perinatal care on the neonatal mortality rate (NMR) in Colorado.
Study Design
We performed a retrospective cohort study, evaluating all live births in Colorado from 1991 to 2003, and comparing the periods 1991 to 1996 versus 1997 to 2003.
Result
The overall unadjusted NMR of the two time periods was 4.3 and 4.4 per 1000 live births, respectively (P=0.42). The contribution of infants with birth weights <750 g to the overall NMR increased from 45.0 to 54.5% (P<0.01). The odds of death for infants <750 g increased between time periods (Odd ratio 1.3, 95% Confidence interval 1.11, 1.61). However, NMR decreased between time periods for all birth weight categories, until infants <600 g. With respect to regionalization, the number of infants <750 g born in a level III care center increased slightly between the two time periods (69.6 versus 73.3%; P=0.04); however, adjusted analysis showed no difference in the practice of regionalization between time periods. Regardless of time period, infants who weighed <750 g born in a level III center had 60% lower mortality risk when compared to <750 g infants born in a non-level III center (P<0.01; 95% CI 0.30, 0.52).
Conclusion
Despite advances in neonatal medicine, the overall NMR in the state of Colorado remained unchanged between the time periods of 1991 to 1996 and 1997 to 2003. Infants at the threshold of viability continue to have a large impact on the Colorado NMR, making up a larger proportion of overall neonatal deaths. While the results demonstrate that the risk of mortality is significantly reduced for <750 g infants born in a level III center, the practice of regionalization has not changed between the two time periods. Improved efforts to standardize the referral practices to ensure delivery of <750 g infants in level III centers could potentially reduce the impact of these infants on the NMR. While the overall NMR in Colorado has not changed between the two time periods, the NMR for infants >600 g has significantly decreased, suggesting that the boundary delineating the threshold of viability needs reevaluation, as it may have been pushed lower than previously defined.
Keywords: neonatal mortality rate, threshold of viability, regionalization, ELBW infants, prematurity
Introduction
In the 30-year period from 1965 to 1995, the Colorado neonatal mortality rate (NMR) had its greatest decline due to advances in obstetrical, neonatal and perinatal care, including new technologies and therapies that allowed for the survivability of more immature, smaller infants.1 In the 1990s, the widespread use of surfactant and antenatal steroids also contributed to increased survivability of extremely low birth weight infants.2 Due in part to these advances, more studies have examined survivability of infants of lower birth weights, with the corollary that the threshold of viability, the birth weight at which infants are expected to have a reasonable chance of survival, continues to trend lower.3,4
In 2000, Hernández, et al.5 examined the impact of infants born at the threshold of viability on the Colorado NMR. The study reviewed neonatal deaths of all liveborn infants <750 g from January 1991 to December 1996, and noted that while these extremely low birth weight infants accounted for 0.31% of all live births, they accounted for 46.3% of the neonatal deaths. The study concluded that further attempts to reduce the Colorado NMR would need to focus on these extremely small infants, and suggested that further improvements in regionalization of high-risk perinatal care would greatly decrease deaths in this group.
The last published examination of the benefits of regionalization in Colorado covered the time period 1971 to 1978. In this study, Bowes showed that a greater proportion of very low birth weight infants (<1500 g) died in level I hospitals rather than level II or III centers, and that the overall NMR decreased from 13.4 to 6.9 per 1000 live births as the concept of regionalization became more widely practiced.6 Since that time, multiple studies in other states have affirmed that regionalization does improve outcomes of extremely premature infants.7–10 In 2004, the American Academy of Pediatrics (AAP) Committee on the Fetus and Newborn presented evidence that the risk-adjusted mortality and morbidities such as intraventricular hemorrhage and chronic lung disease were greater for infants at 27 to 29 weeks gestation born outside level III referral centers as compared to those born in level III centers. Thus, the AAP continues to recommend regionalization as a means to achieve optimal outcomes for these at risk infants.11 The aim of this study was to compare neonatal deaths in Colorado from 1991 to 1996 versus 1997 to 2003, and to explore changes in the impact of infants born at the threshold of viability (<750 g birth weight) on the Colorado NMR. Since regionalization was suggested by Hernández, et al. as a means of improving survivability of these infants, we secondarily analyzed the relationship between neonatal mortality and regionalization for infants at the threshold of viability.
Methods
Study design and inclusion criteria
We performed a retrospective cohort study using linked birth certificate and death certificate data on infants born during the years 1991 to 2003 in Colorado, as provided by the Vital Statistics Section of the Colorado Department of Public Health and Environment. We adhered to the State of Colorado definition of live birth: ‘The complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of pregnancy, which, after such separation, breathes or shows any other evidence of life, such as beating of the heart, pulsation of the umbilical cord, or definite movement of voluntary muscles, whether or not the umbilical cord has been cut or the placenta is attached.’12 Furthermore, we included only those birth certificates with complete data for our variables of interest (described below). This criterion resulted in the exclusion of 446 records, or 0.06% of the total birth records for the time period 1991 to 2003. Only one of the 446 exclusions was an infant with a documented birth weight <750 g.
Primary outcomes
The primary outcome measure was neonatal death, defined as death within 28 days after birth. The main subsample of infants we used to test our hypotheses were infants born at the ‘threshold of viability,’ defined as birth weight <750 g. This definition complies with the adopted position of the Committee on the Fetus and Newborn of the AAP, and enabled us to compare more recent data to the findings of Hernández, et al., who used the same cutoff.5,13 The study periods 1991 to 1996 and 1997 to 2003 were used in order to make comparisons to the findings of Hernández, et al.
To test our hypotheses and account for potential confounders, we included the variables: birth weight, gestational age, death, year of birth, maternal education, maternal use of alcohol or tobacco, maternal race, level of care of birth hospital, in utero transport of mother/fetus, initiation and maintenance of mechanical ventilation (which included any respiratory assistance such as continuous positive airway pressure) and presence of congenital anomalies.
To obtain a measure for gestational age that was as accurate as possible, the estimate of gestational age based on last menstrual period was compared to the clinical estimate of gestational age. Employing the algorithm used by Hintz, et al., when there was less than 2 weeks discrepancy, the gestational age based on last menstrual period was used.14 When the discrepancy was greater than 2 weeks, the average was taken and then truncated to indicate completed weeks of gestation. If the discrepancy between the two values was equal to 2 weeks, the lower estimate was chosen.
To test the specific hypothesis regarding the impact of regionalization on NMR, we examined the care levels of healthcare facilities in Colorado where the infants <750 g were born. Eight perinatal facilities were designated status as level III care centers by the Colorado Perinatal Care Council and retained this designation for the full study period 1991 to 2003. All eight centers fulfill the criteria set forth by the AAP for a level III center, including the ability to comprehensively care for extremely low birth weight infants at ⩽28 weeks gestation and ⩽1000 g, and the ability to provide sustained life support with conventional mechanical ventilation.11 Infants <750 g at birth were categorized by a ‘transfer category’: (1) born in a level III center without maternal transport; (2) born in a level III center following maternal transport and (3) born in a level I or II center.
Statistical analysis
Unadjusted differences between the two time periods for our cohorts of infants <750 g were assessed by χ2-tests for all variables except gestational age, maternal age and maternal education level; for these continuous variables, two-sample t-tests were used to assess differences. χ2-tests were also used, as appropriate, to compare the two time periods with respect to our primary outcome, neonatal death.
Using logistic regression, we determined the odds of mortality in the two time periods for each transfer category described above, with the outcome being neonatal death. We adjusted for congenital anomalies, ventilation use, gender, maternal age and education. Statistical analyses were performed with SAS 9.1 (SAS Institute, Cary, NC, USA).
Results
Birth weight distribution of all live births
During the study period, there were 779 385 total live births, with an average of 54 718 births per year from 1991 to 1996, and 64 440 births per year from 1997 to 2003. The male to female ratio in both time periods was 1:0.95. In the earlier time period, there were 1029 infants with birth weights <750 g, accounting for 0.31% of all total live births. Similarly, in the later time period, there were 1664 such infants, representing 0.37% of all total live births (Table 1).
Table 1.
Low birth weight classification groups: Colorado, 1991–1996 vs 1997–2003
| Classification | Birth weight (g) |
1991–1996 No. live births (% of all births) |
1997–2003 No. live births (% of all births) |
|---|---|---|---|
| Threshold of viability | <750 | 1029 (0.31) | 1664 (0.37) |
| Extremely low birth weight | <1000 | 1909 (0.6) | 2907 (0.6) |
| Very low birth weight | <1500 | 4159 (1.3) | 6117 (1.3) |
| Low birth weight | <2500 | 28 288 (8.6) | 39 981 (8.9) |
Rows and totals are not mutually exclusive. P-values are <0.01 for each row comparison between time periods, but this is not inferred to be of practical significance.
Neonatal death and unadjusted NMR
During the period spanning 1991 to 2003, there were 3398 neonatal deaths among all live born infants. From 1991 to 1996, there were 1408 neonatal deaths, for an overall unadjusted NMR of 4.3 per 1000 live births. Similarly, in 1997 to 2003, there were 1990 neonatal deaths, for an overall unadjusted NMR of 4.4 per 1000 live births. This small increase in overall NMR was not statistically significant (χ2=0.66, d.f.=1, P=0.42).
Characteristics of infants at the threshold of viability (<750 g)
Neonatal death and unadjusted NMR
Characteristics of the infants born at the threshold of viability (birth weight <750 g) are provided in Table 2. There were no significant differences between the two time periods for the number of neonatal deaths, infant gender, transfer status, presence of congenital anomalies, maternal education and maternal race. However, statistically significant differences existed between the two time periods for gestational age, the use of mechanical ventilation, maternal age and the mother’s use of tobacco or alcohol during pregnancy.
Table 2.
Characteristics of infants born at the threshold of viability (<750 g): Colorado, 1991–1996 vs 1997–2003
| 1991–1996 | 1997–2003 | P-value | |
|---|---|---|---|
| N (%) | N (%) | ||
| No. live births | 1029 | 1664 | |
| No. neonatal deaths | 633 (61.5) | 1084 (65.1) | 0.06 |
| Characteristics of birth | |||
| Male infants | 515 (50.1) | 867 (52.1) | 0.36 |
| Gestational age (mean ± s.d.) | 24.2 ± 3.24 | 23.7 ± 3.14 | <0.01 |
| Ventilation status | 0.02 | ||
| >30 min | 266 (22.0) | 437 (26.3) | |
| <30 min | 54 (5.3) | 67 (4.0) | |
| Not ventilated | 749 (72.8) | 1160 (69.7) | |
| Presence of congenital anomalies | 124 (12.1) | 162 (9.7) | 0.06 |
| Characteristics of mother | |||
| Age (mean ± s.d.) | 26.1 ± 6.8 | 26.7 ± 6.6 | 0.02 |
| Race and ethnicity | 0.28 | ||
| Caucasian, non-Hispanic | 639 (62.1) | 1046 (62.9) | |
| Caucasian, Hispanic | 181 (17.6) | 314 (18.9) | |
| African American, non-Hispanic | 168 (16.3) | 229 (13.8) | |
| Other | 41 (4.0) | 75 (4.5) | |
| Education, highest grade complete (mean ± s.d.) | 12.6 ± 2.8 | 12.6 ± 2.8 | 0.64 |
| Alcohol use | <0.01 | ||
| Yes | 43 (4.2) | 51 (3.1) | |
| No | 955 (92.8) | 1613 (96.9) | |
| Unknown | 31 (3.0) | 0 (0) | |
| Tobacco use | <0.01 | ||
| Yes | 186 (18.1) | 214 (12.9) | |
| No | 815 (79.2) | 1450 (87.1) | |
| Unknown | 28 (2.7) | 0 (0) |
Neonatal deaths and unadjusted NMR are summarized per birth weight group in Table 3 for infants <750 g. As a group, infants <750 g had an overall mortality rate of 61.5% (633 of 1029) from 1991 to 1996, as compared to 65.1% (1084 of 1664) from 1997 to 2003 (χ2=3.62, d.f.=1, P=0.06). No differences between time periods for any 100 g increment subgroup were statistically significant. As noted by Hernández, et al., mortality in the <500 g group when compared to the 500 to 749 g group continues to be almost double: 89.0 versus 46.4% in the earlier time period and 89.2 versus 49.5% in the later time period. The lowest mortality rate continued to be observed in infants of 600 to 749 g, at 35.9% in the earlier time period and 38.2% in the later time period.
Table 3.
Infants born at the threshold of viability (<750 g) and neonatal mortality rate: Colorado, 1991–1996 vs 1997–2003
| Birth weight (g) | 1991–1996 |
1997–2003 |
||||||
|---|---|---|---|---|---|---|---|---|
| Live births | Neonatal deaths | NMR (%) | Survival rate (%) | Live births | Neonatal death | NMR (%) | Survival rate (%) | |
| <300 | 75 | 71 | 94.7 | 5.3 | 186 | 181 | 97.3 | 2.7 |
| 300–399 | 130 | 115 | 88.5 | 11.5 | 204 | 189 | 92.6 | 7.4 |
| 400–499 | 160 | 139 | 86.9 | 13.1 | 267 | 216 | 80.9 | 19.1 |
| <500 | 365 | 325 | 89.0 | 11.0 | 657 | 586 | 89.2 | 10.8 |
| 500–699 | 255 | 161 | 63.1 | 36.9 | 397 | 265 | 66.8 | 33.2 |
| 600–749 | 409 | 147 | 35.9 | 64.1 | 610 | 233 | 38.2 | 61.8 |
| 500–749 | 664 | 308 | 46.4 | 53.6 | 1007 | 498 | 49.5 | 50.5 |
| <750 | 1029 | 633 | 61.5 | 38.5 | 1664 | 1084 | 65.1 | 34.9 |
| ⩾750 | 327 277 | 775 | 0.2 | 99.8 | 449 415 | 906 | 0.2 | 99.8 |
Abbreviation: NMR, neonatal mortality rate.
Infants born <500 g accounted for 23.1% of all neonatal deaths in the first period, and 29.6% of all neonatal deaths in the second period (χ2=17.0, d.f.=1, P<0.01). The <750 g cohort comprised 45.0% of all neonatal deaths in the first time period (633 of 1408), as compared to 54.5% of all neonatal deaths in the second time period (1084 of 1990) (χ2=29.9, d.f.=1, P<0.01).
Birth weight aggregation and NMR
To further explore the boundary which represents the threshold of viability for low birth weight infants, we constructed aggregate birth weight groups and compared changes in NMR between the two time periods. In each successive group, we lowered the cutoff for the inclusion of lower birth weights. These groups are depicted in Table 4.
Table 4.
Birth weight aggregate group NMR comparisons: Colorado, 1991–1996 vs 1997–2003
| Birth weight aggregate | 1991–1996 | 1997–2003 | P-value |
|---|---|---|---|
| NMR (per 1000 births) | NMR (per 1000 births) | ||
| >2500 | 1.0 | 0.9 | 0.07 |
| >1500 | 1.6 | 1.4 | <0.01 |
| >1000 | 2.0 | 1.6 | <0.01 |
| >750 | 2.4 | 2.0 | <0.1 |
| >600 | 2.8 | 2.5 | 0.02 |
| >500 | 3.3 | 3.1 | 0.15 |
| >300 | 4.1 | 4.0 | 0.67 |
| Overall | 4.3 | 4.4 | 0.42 |
Abbreviation: NMR, neonatal mortality rate.
As described previously, the overall NMR did not change significantly from 1991 to 1996 to 1997 to 2003 (4.3 versus 4.4 per 1000). However, the aggregations shown in Table 4 demonstrate that, in fact, NMR decreased between the two time periods when considering only infants >1500 g (χ2=8.6, d.f.=1, P<0.01), >1000 g (χ2=14.0, d.f.=1, P<0.01) and >750 g (χ2=10.9, d.f.=1, P<0.01). Furthermore, a significant reduction in NMR was noted for infants >600 g, from 2.8 to 2.5 per 1000 (χ2=5.7, d.f.=1, P=0.02). No improvements in NMR, however, were noted when including birth weights from <600 g or for birth weight infants >2500 g.
Delivery room interventions
As noted in Table 2, there was a statistically significant difference in the use of mechanical ventilation for infants <750 g between the two time periods. In the time period 1997 to 2003, the percentage of infants mechanically ventilated >30 min increased to 26.3 from 22.0% in 1991 to 1996 (χ2=7.73, d.f.=2, P=0.02).
Of the 3398 infants with birth weight <750 g who eventually died, 85.5% in 1991 to 1996 and 84.9% in 1997 to 2003 received no mechanical ventilation. In both periods, 11.9% received mechanical ventilation for >30 min, likely indicating that they responded to delivery room resuscitation and were admitted to the neonatal intensive care unit. Death occurred despite attempted resuscitation in 2.7% of the infants in 1991 to 1996 and 3.2% of the infants in 1997 to 2003. None of these findings reached a level of significance.
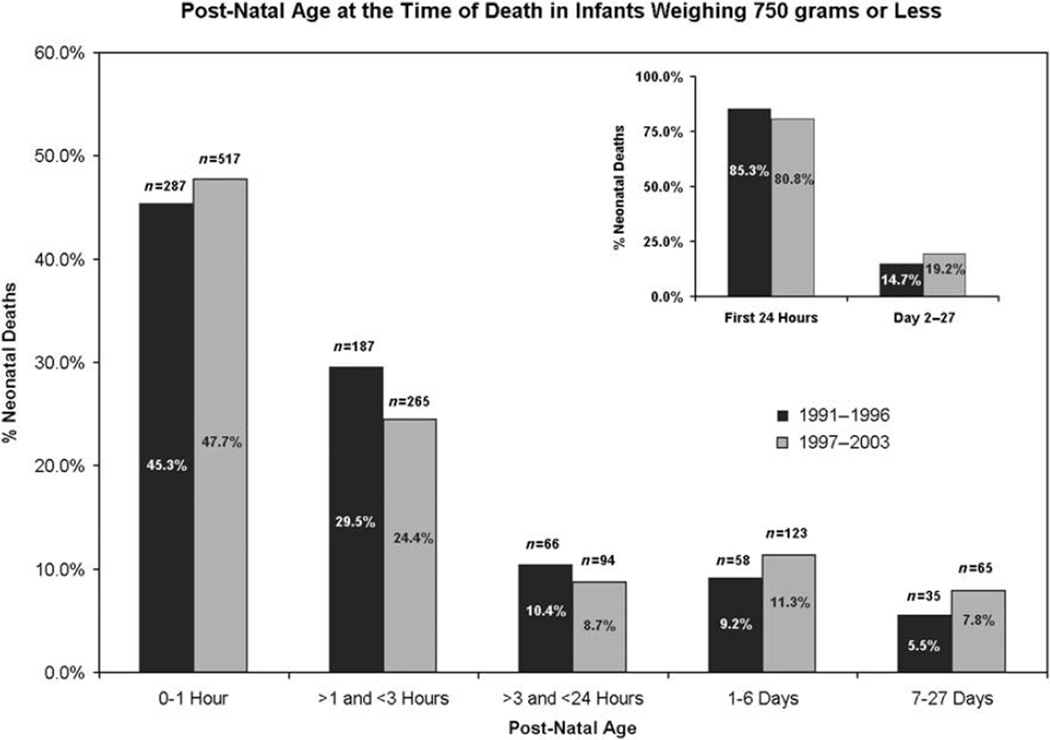
Timing of neonatal deaths
As shown in Figure 1, among infants born at the threshold of viability, the majority of neonatal deaths occurred on the first day of life in both time periods, although the percentage of deaths in the first 24 h was less in 1997 to 2003. In total 85.3% of neonatal deaths of infants <750 g in the time period 1991 to 1996 occurred within the first 24 h after birth, while only 80.8% of similar infants died in the first 24 h after birth in the time period 1997 to 2003 (χ2=5.59, d.f.=1, P=0.02).
Figure 1.
Postnatal age at the time of death in infants weighing <750 g.
Neonatal deaths according to level of perinatal center
For the entire study period, 1936 of 2693 infants <750 g were born in level III perinatal centers. Overall, 69.6% of these infants were born in level III facilities in the first time period, as compared to 73.3% in the second time period (χ2=4.39, d.f.=1, P=0.04). As stated previously, infants were further categorized as having been born in a level III care center without maternal transport, born in a level III care center following maternal transport, or born in a I or II care center. These data are summarized in Table 5. Percentages of infants born in each of these transfer categories were similar across both time periods, with the majority being born in a level III care center (χ2=5.04, d.f.=2, P=0.08).
Table 5.
Infants born at the threshold of viability (<750 g) and in utero transfer status: Colorado residents, 1991–1996 vs 1997–2003
| Transfer category | 1991–1996 | 1997–2003 |
|---|---|---|
| No. births (%) | No. births (%) | |
| Born in level III center, no maternal transport | 547 (53.2) | 912 (54.8) |
| Born in level III center following maternal transport | 169 (16.4) | 308 (18.5) |
| Born in a level I or II center | 313 (30.4) | 444 (26.7) |
Adjusted analysis
When we examined the outcome of neonatal death using logistic regression analyses, and adjusting for significant covariates (presence of congenital anomalies, ventilation use, infant gender age, and education of the mother), interactions between birth period and transfer status were not statistically significant at α=0.05. However, there was a significant difference between the odds of death regardless of transfer status when comparing the two study periods; the odds of death for <750 g infants born in 1997 to 2003 were 1.3 times higher than similar infants born in 1991 to 1996 (95% CI 1.11, 1.61).
Regardless of time period, the mortality risk for infants who were transported to a level III care facility was 60% lower than that of infants who were born outside a tertiary facility (P<0.01; 95% CI 0.30, 0.52). For infants who were already in a tertiary care facility and thus did not need transfer, the mortality risk was 46% lower than for infants born outside a level III hospital (P<0.01; 95% CI 0.43, 0.67).
Discussion
Despite prenatal efforts to improve outcomes for infants born at the threshold of viability, these infants continue to present a challenge to obstetricians and neonatologists alike. Since the 1990s, surfactant, antenatal steroids, antenatal antibiotics and noninvasive forms of ventilatory support (continuous positive airway pressure) have influenced further reduction of the NMR, as has been shown in other studies.8 However, despite these advances in neonatal medicine, the results of this study indicate that the overall NMR in Colorado did not significantly change between the time periods. This lack of improvement in the Colorado NMR since the mid-1990s mirrors the stasis in NMR in the United States.15
Our results also show that the <750 g infants have increased odds of death in the second time period as compared to the first, despite the advances in neonatal medicine. This finding prompts the question: which infants are benefiting from these innovations? Our analysis indicates that infants <750 g accounted for 45.1% of total neonatal deaths in the first time period, and this proportion increased significantly to 54.4% in the second time period. Likely, infants >750 g benefit most from the advances in neonatal medicine described above. Indeed, the <500 g infants had significantly greater mortality, from 23.1 to 29.5% (P<0.01) between time periods; this increased mortality may be reflective of the more premature infants <750 g born in the second time period. As shown in the birth weight aggregation analysis, infants weighing <600 g may be heavily influencing these contributions to overall NMR, disproportionately accounting for the lack of improvement in NMR between time periods.
In the birth weight aggregate analysis, NMR improved for infants weighing 600 g or more, until birth weights reached >2500 g, where no improvement in NMR was seen. This finding suggests that continuing advances in neonatal intensive care have made an impact, especially for infants slightly below the currently accepted definition of the threshold of viability (<750 g). In addition, while advances in neonatal medicine have improved the opportunities for successful live births of infants at the currently defined threshold of viability, these advances may be insufficient for long-term survival of infants below 600 g.
Neonatologists vary in their care of infants at the extremes of viability. As documented in the literature, some neonatologists are more pessimistic about the viability of these infants and do not initiate resuscitation at all.16 Indeed, some neonatologists have concluded that perhaps the threshold of viability has been reached; investigators place this cutoff at approximately 23 to 24 weeks gestation, although they note that survivability has improved at these gestational ages.17,18 In reviewing our results on postnatal age at the time of death, in the second time period, fewer babies who eventually died did so in the first 24 h after birth, indicating that medical interventions may sustain life slightly longer for these infants, but not alter the eventual outcome of death. This supports results from Hintz et al.14 that medical advances may convey an early advantage, but these infants surviving >12 h may have no significant mortality differences between early and later time periods.
As a whole, the practice of regionalization did not appear to change between the two time periods. However, the data clearly indicated that infants <750 g born in a level III referral center, regardless of time period, had decreased risk of mortality, confirming the results documented in other studies. Based on the preponderance of data, the importance of regionalization in the care of extremely low birth weight infants cannot be overstated; efforts to further standardize and improve the safety of transfers appear critical to improve survivability for these infants.
Our analysis did not examine the timing of or decisions surrounding maternal or neonatal transfer, as obstetricians and neonatologists make crucial decisions, which could play an important role in survivability of infants. Interpretation of viability for extremely low birth weight infants can affect the timing of heroic measures, such as cesarean delivery or maternal transport for a higher level of perinatal care. Ideally, pregnant women would be transferred safely well in advance of the onset of labor, rather than incur the risk for transport of an unstable mother/fetus.
A delay in transfer that resulted in a death could skew the results if attributed to the referral hospital; therefore, attributing early neonatal death and adverse neonatal outcomes to the referral hospital rather than the hospital of origin may be inappropriate. In fact, Dooley, et al.19 suggest attributing perinatal deaths to the hospital of origin in order to better identify specific institutions that are lacking in personnel or resources and to further demonstrate that regionalization can play a more significant role in the reduction of neonatal mortality than what has been previously realized. While our data support that birth in a level III referral center does decrease the risk of mortality, the means of referral was outside the scope of this study; we did not examine if the infants were referred to the correct center, nor do we know why specific births took place at specific centers. Further studies could examine in greater detail the relationship between each level III referral center and the level I and II centers that it supports to further clarify the chain of referrals.
Our study was also limited by the uncertainty of birth certificate data. Birth weight is an objective criterion that allowed our study to be comparable to previous work and the position of the Committee on the Fetus and Newborn of the AAP. However, antenatal assessment of birth weight is sometimes unreliable. Gestational age is a clinically more relevant measure of prematurity and more often the basis on which medical decisions, such as initiation of resuscitation and withdrawal of life support are made.20,21 However, due to the relative unreliability of the measures of gestational age in the birth dataset, which included a clinical estimate and an estimate based on the mother’s last menstrual period, it was improbable that gestational age and birth weight could accurately be combined.
In addition, we were unable to evaluate important characteristics of the infants for whom resuscitation was not performed. If a mother were pregnant with a fetus at the threshold of viability, if she or her physician decided not to undertake aggressive resuscitation for that infant, transfer of that mother/baby dyad would be unnecessary, and the infant would likely die outside of a referral center. If these infants were preferentially overrepresented in one of the transfer categories, it would have affected the estimates of the mortality risk based on facility level of care. A chart review of these infants who died outside of level III facilities may elucidate this further.
The impact of infants at the threshold of viability on the NMR in Colorado is significant, further compounded by their effect on personnel, resources and health care systems. Not only do these infants require a prolonged course of neonatal intensive care, but as more of these extremely vulnerable and premature infants survive, they potentially contribute to increased incidence of co-morbidities such as chronic lung disease, severe neurodevelopmental disability, cerebral palsy and poor growth, which require continued chronic and specialized care. Hack and Fanaroff17 cite a 30 to 50% incidence of severe neurodevelopmental disability at 18 to 30 months in survivors born at 23 to 25 weeks gestation. Chronic lung disease is the most prevalent morbidity, from 86 to 100% in infants born at 23 weeks or less gestation.18 For many parents and medical practitioners, such outcomes stimulate medical and ethical discussion.
As demonstrated by the increase in contribution to the overall neonatal mortality of infants <750 g in the State of Colorado between the time periods 1991 to 1996 and 1997 to 2003, we continue to face challenges presented by these extremely vulnerable infants. Large gaps still exist in our knowledge about these infants and the threshold of viability. Indeed, the extent to which we can use neonatal intensive care technology at the extreme degrees of viability are unknown, or as Lucey, et al.3 appropriately described, ‘a big uncontrolled experiment’. Some studies suggest that the threshold of viability has been reached at 23 to 24 weeks gestation, although infants more immature than this continue to be resuscitated with varying results, and more often than not, suffer severe morbidities with which families must cope for years to come.
We continue to face ethical, medical, and economic dilemmas in how our efforts should be focused to improve survivability and decrease morbidity in these extremely vulnerable infants at the threshold of viability. Further research is needed to explore the costs and benefits associated with heroic care and transport of extremely small, immature infants. In addition, our data suggest a need for more in-depth survival analysis of infants weighing 600 g or less, with the potential that the threshold of viability remains a dynamic boundary we may continue to push lower with improved technologies. As data lend even greater support to the concept of regionalization, pooled allocation of resources and personnel, antenatal referral to level III centers and transport of high-risk mothers and infants prior to delivery, we may provide these infants at the threshold of viability the best chance of survival.
Acknowledgments
We thank Dr Dennis Lezotte, Dr Ned Calonge and Dr Jill Norris for their assistance in study design and development of this work. We also thank Dr Meica Efird, Dr Gerald Merenstein and Dr Daniel Hall for their insightful comments and suggestions.
Footnotes
We have no financial support to disclose.
References
- 1.Colorado Department of Public Health Environment. Colorado Vital Statistics 1999 May. 2001 http://www.ext.colostate.edu/cis/health-ch1.pdf.
- 2.Schwartz RM, Luby AM, Scanlon JW, Kellogg RJ. Effect of surfactant on morbidity, mortality, and resource use in newborn infants weighing 500–1500 g. New Engl J Med. 1994;330(21):1476–1480. doi: 10.1056/NEJM199405263302102. [DOI] [PubMed] [Google Scholar]
- 3.Lucey JF, Rowan CA, Shiono P, Wilkinson AR, Kilpatrick S, Payne NR, et al. Fetal infants: the fate of 4172 infants with birth weights of 401–500 grams—the Vermont Oxford Network Experience (1996–2000) Pediatrics. 2004;113(6):1559–1566. doi: 10.1542/peds.113.6.1559. [DOI] [PubMed] [Google Scholar]
- 4.Lemons JA, Bauer CR, Oh W, Korones SB, Papile L, Stoll BJ, et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1995 through December 1996. Pediatrics. 2001;107:1–8. doi: 10.1542/peds.107.1.e1. [DOI] [PubMed] [Google Scholar]
- 5.Hernández JA, Hall DM, Goldson EJ, Chase M, Garrett C. Impact of infants born at the threshold of viability on the neonatal mortality rate in Colorado. J Perinatol. 2000;1:21–26. doi: 10.1038/sj.jp.7200300. [DOI] [PubMed] [Google Scholar]
- 6.Bowes WA. A review of the perinatal mortality in Colorado, 1971–1978, and its relationship to the regionalization of perinatal services. Am J Obstet Gynecol. 1981;141(8):1045–1052. doi: 10.1016/s0002-9378(16)32696-5. [DOI] [PubMed] [Google Scholar]
- 7.Bode MM, O’Shea TM, Metzguer KR, Stiles AD. Perinatal regionalization and neonatal mortality in North Carolina, 1968–1994. Am J Obstet Gynecol. 2001;184(6):1302–1307. doi: 10.1067/mob.2001.114484. [DOI] [PubMed] [Google Scholar]
- 8.Clement MS. Perinatal care in Arizona 1950–2002: a study of the positive impact of technology, regionalization and the Arizona Perinatal Trust. J Perinatol. 2005;25:503–508. doi: 10.1038/sj.jp.7211337. [DOI] [PubMed] [Google Scholar]
- 9.Yeast JD, Poskin M, Stockbauer JW, Shaffer S. Changing patterns in regionalization of perinatal care and the impact on neonatal mortality. Am J Obstet Gynecol. 1998;178:131–135. doi: 10.1016/s0002-9378(98)70639-8. [DOI] [PubMed] [Google Scholar]
- 10.Hein HA. Regionalized perinatal care in North America. Semin Neonatol. 2004;9:111–116. doi: 10.1016/j.siny.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 11.American Academy of Pediatrics Committee on the Fetus Newborn. Levels of neonatal care. Pediatrics. 2004;114(5):1341–1347. doi: 10.1542/peds.2004-1697. [DOI] [PubMed] [Google Scholar]
- 12.Colorado Department of Public Health and Environment. Colorado Vital Statistics 1996. Denver, CO: Vital Statistics Section; 1997. pp. 239–246. [Google Scholar]
- 13.American Academy of Pediatrics Committee on Fetus and Newborn. Perinatal care at the threshold of viability. Pediatrics. 1995;96:974–976. [PubMed] [Google Scholar]
- 14.Hintz SR, Poole WK, Wright LL, Fanaroff AA, Kendrick DE, Laptook AR, et al. Changes in mortality and morbidities among infants born at less than 25 weeks during the post-surfactant era. Arch Dis Child Fetal Neonatal Ed. 2005;90:F128–F133. doi: 10.1136/adc.2003.046268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.March of Dimes. http://search.marchofdimes.com/peristats/.
- 16.Shankaran S, Fanaroff AA, Wright LL, Stevenson DK, Donovan EF, Ehrenkranz RA, et al. Risk factors for early death among extremely low birth weight infants. Am J Obstet Gynecol. 2002;186:796–802. doi: 10.1067/mob.2002.121652. [DOI] [PubMed] [Google Scholar]
- 17.Hack M, Fanaroff AA. Outcomes of extremely low birthweight and gestational age in the 1990’s. Early Hum Dev. 1999;53:193–218. doi: 10.1016/s0378-3782(98)00052-8. [DOI] [PubMed] [Google Scholar]
- 18.Ho S, Saigal S. Current survival and early outcomes of infants of borderline viability. NeoReviews. 2005;6(3):e123–e131. [Google Scholar]
- 19.Dooley SL, Freels SA, Turnock BJ. Quality assessment of perinatal regionalization by multivariate analysis: Illinois, 1991–1993. Obstet Gynecol. 1997;89(2):193–198. doi: 10.1016/S0029-7844(96)00450-4. [DOI] [PubMed] [Google Scholar]
- 20.Allen MC, Donohue PK, Dusman AE. The limit of viability—Neonatal outcome of infants born at 22–25 weeks gestation. N Engl J Med. 1993;329(22):1597–1601. doi: 10.1056/NEJM199311253292201. [DOI] [PubMed] [Google Scholar]
- 21.MacDonald H the American Academy of Pediatrics Committee on the Fetus and Newborn. Perinatal care at the threshold of viability. Pediatrics. 2002;110(5):1024–1027. doi: 10.1542/peds.110.5.1024. [DOI] [PubMed] [Google Scholar]