Abstract
Vancomycin-resistance in enterococci (VRE) is associated with isolates within ST18, ST17, ST78 Enterococcus faecium (Efm) and ST6 Enterococcus faecalis (Efs) human adapted lineages. Despite of its global spread, vancomycin resistance rates in enterococcal populations greatly vary temporally and geographically. Portugal is one of the European countries where Tn1546 (vanA) is consistently found in a variety of environments. A comprehensive multi-hierarchical analysis of VRE isolates (75 Efm and 29 Efs) from Portuguese hospitals and aquatic surroundings (1996–2008) was performed to clarify the local dynamics of VRE. Clonal relatedness was established by PFGE and MLST while plasmid characterization comprised the analysis of known relaxases, rep initiator proteins and toxin-antitoxin systems (TA) by PCR-based typing schemes, RFLP comparison, hybridization and sequencing. Tn1546 variants were characterized by PCR overlapping/sequencing. Intra- and inter-hospital dissemination of Efm ST18, ST132 and ST280 and Efs ST6 clones, carrying rolling-circle (pEFNP1/pRI1) and theta-replicating (pCIZ2-like, Inc18, pHTβ-like, two pRUM-variants, pLG1-like, and pheromone-responsive) plasmids was documented. Tn1546 variants, mostly containing ISEf1 or IS1216, were located on plasmids (30–150 kb) with a high degree of mosaicism and heterogeneous RFLP patterns that seem to have resulted from the interplay between broad host Inc18 plasmids (pIP501, pRE25, pEF1), and narrow host RepA_N plasmids (pRUM, pAD1-like). TAs of Inc18 (ω-ε-ζ) and pRUM (Axe-Txe) plasmids were infrequently detected. Some plasmid chimeras were persistently recovered over years from different clonal lineages. This work represents the first multi-hierarchical analysis of VRE, revealing a frequent recombinatorial diversification of a limited number of interacting clonal backgrounds, plasmids and transposons at local scale. These interactions provide a continuous process of parapatric clonalization driving a full exploration of the local adaptive landscape, which might assure long-term maintenance of resistant clones and eventually fixation of Tn1546 in particular geographic areas.
Introduction
Since its first description in the late 80’s, vancomycin-resistant enterococci (VRE) have been increasingly reported worldwide, but presenting remarkable geographical and temporal differences in local rates (http://www.cddep.org/ResistanceMap/bug-drug/EFa-VC) [1]-[3]. Vancomycin-resistant Enterococcus faecium (VREfm) became endemic in most North American hospitals since the mid 90′s [1], [2], [4]–[6] while their overall occurrence in Europe remained low until recently, when VRE nosocomial outbreaks started to be increasingly reported in some European countries (Annual Report of the European Antimicrobial Resistance Surveillance Network, EARS-Net, 2009) [1], [3], [7], [8]. Despite E. faecium (Efm) being less frequently found than Enterococcus faecalis (Efs) in clinical isolates, it is far more frequently resistant to vancomycin, one of the last-line intravenous antibiotic resources for therapy. However, although the rate of vancomycin-resistant E. faecalis (VREfs) has remained low, they are steadily increasing in both the US and in EU countries (http://www.cddep.org/ResistanceMap/bug-drug/EFe-VC) [3].
Vancomycin resistance among enterococci is mostly due to the spread of Tn1546 (vanA genotype) and Tn1549 (vanB genotype), which are generally identified on plasmids and chromosome, respectively [3]. The few studies in which plasmids carrying Tn1546 from human or animal isolates were characterized revealed they belong to plasmid families RepA_N (pheromone-responsive plasmids and derivatives of pRUM and pLG1), Inc18 and pHTβ [9]–[18] suggesting an apparent plasmid promiscuity of this transposon influencing its dissemination among enterococcal populations.
Recent analysis of enterococcal populations in the clinical setting depicts a rugged epidemiological profile, with successive waves of isolates causing infections, which belong to specific lineages of E. faecium (ST17, ST18 and ST78, previously considered within the same clonal complex (CC) 17), and E. faecalis (ST6, ST40) [19]–[21]. However, regional differences in the rates of VRE cannot be only explained by clonal replacement dynamics as suggested for other pathogens [22]–[24].
The aim of this study was to address the dynamics of vancomycin resistance among enterococci in Portugal, one of the developed countries with higher rates of both VREfm (21–23%) and VREfs (1.8–4.1%) (www.earss.rivm.nl; http://www.cddep.org/ResistanceMap/bug-drug/EFe-VC), and where VanA is prevalent over VanB [3], [25]–[27], by analyzing the clonal and plasmid backgrounds influencing the spread and persistence of Tn1546. Our study suggests that clonalization, the local selection of distinct clonal variants giving rise to durable bacterial lineages, might result and be modified by the local spread and recombinatorial dynamics of mobile genetic elements, thus providing new clues about the local multi-hierarchical evolutionary biology of vancomycin resistance.
Results
Local dynamic landscape drives the spread and fixation of vancomycin resistance in Portuguese hospitals
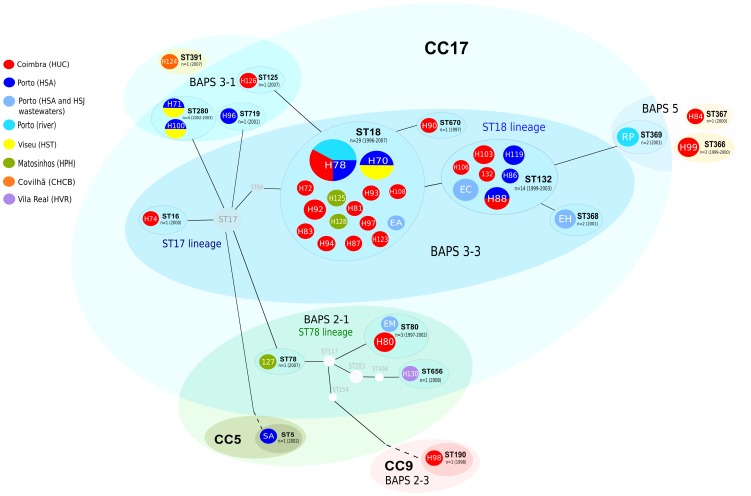
We have determined that the enterococcal population from the Portuguese hospitals is formed by an ensemble of MLST/PFGE clones. Efm isolates fit in three out of six phylogenomic groups recently established by using Bayesian Analysis of Population Structure (BAPS), namely BAPS groups 2, 3 and 5 [19] (Figure 1). Most of the isolates cluster into the predominant BAPS group 3 [subgroup 3–3 comprising main human lineages ST18 (ST18 and ST132) and ST17 (ST16); and subgroup 3–1 comprising ST280], and the BAPS group 2 (including ST80 and ST656/ST78 lineage, ST5/CC5, ST190/CC9), which have been previously associated with isolates from humans and both animals and humans, respectively [10], [19], [25], [28]–[30]. A number of clones cluster in the small Efm BAPS group 5 (ST366, ST367, ST369), which seems to comprise mosaic genomes [19]. Isolates of Efs belong to ST6/CC2, ST30, ST55, ST117, and ST159 lineages although, to the date of this publication, Efs population has not been clustered in different BAPS groups. Among all them, isolates within ST18 Efm and ST6 Efs lineages were predominant, in line with the intra- and interhospital spread of particular highly transmissible Efm and Efs clones recovered in Portuguese hospitals since the late 90s [22], [25], [31], [32]. While ST6 Efs was widely disseminated in all hospitals analyzed in this country [26], specific Efm lineages were overrepresented in Coimbra (ST18) and Oporto (ST132, a single locus variant, SLV, of ST18). Strains belonging to ST18 (showing PFGE types H70 and H78), ST132 (PFGE type H88) and ST280 (with PFGE types 71 and H100) were spread in different hospitals (Figure 1 and Figure 2).
Figure 1. Population of vancomycin resistant Enterococcus faecium.
Abbreviations: ST, sequence types; CC, clonal complex; BAPS, Bayesian Analysis of Population Structure; HUC, Hospital Universitário de Coimbra; HSA, Hospital Santo António; HSJ, Hospital São João; HST, Hospital São Teotónio; HPH, Hospital Pedro Hispano; CHCB, Centro Hospitalar da Cova da Beira; HVR, Hospital S. Pedro. A colored circle represents each PFGE type (white numbers/letters; H for hospital, SW for sewage, R for river and S for swine clones) and each PFGE type is associated with the corresponding sequence type (STs are represented in black letter and in colored elipses grouping different PFGE types) and BAPS group (in colored elipses grouping different STs). The size of the colored circles corresponds to the number of isolates. CC17 (in light blue), CC5 (in light green), CC9 (in light red) and the singletons ST366, ST367 and ST391 (light yellow) are represented according to the eBURST algorithm (download on 26th January 2012) with black lines joining single locus variants (SLV). STs that were not identified in this study are represented as light grey nodes to link the sequence types identified in this study accordingly to eBURST. ST18 strains (H70, H78, H87, H93, H108, H125) and most ST132 strains (H86, H88, H106, SWC) were clonally related by PFGE (< 7 bands difference). Remarkable relationships among PFGE banding patterns of strains belonging to different STs were observed (H125/ST18 and H126/ST125; H124/ST391 and H71/ST280, SWM/ST80 and H86/H88/H106/H119/SWC/ST132, and isolates SWA/ST18 and SWC/ST132 (< 8 bands difference). This figure drawn up was performed in the “Open Source vector graphics editor Inkscape” (version Inkscape-0.48.2–1).
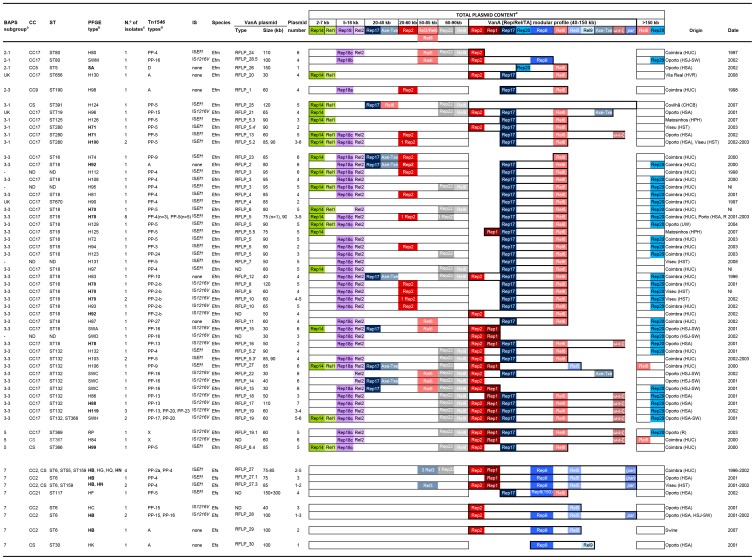
Figure 2. Clonal and plasmid diversity among VREfm and VREFs from Portugal.
Abbreviations: IS, insertion sequence; Efm, Enterococcus faecium; Efs, Enterococcus faecalis; kb, kilobases; BAPS, Bayesian Analysis of Population Structure; ST, sequence type; CC, clonal complex; rep (replicases); rel (relaxases); TA (toxin-antitoxin system); HUC, Hospital Universitário de Coimbra; HSA, Hospital Santo António; HSJ, Hospital São João; HST, Hospital São Teotónio; HPH, Hospital Pedro Hispano; CHCB, Centro Hospitalar da Cova da Beira; HVR, Hospital S. Pedro; SW, sewage wastewaters; UW, urban wastewaters; R, river; ND, not determined; NI, not identified; UK, unknown. aThe distribution of the different isolates is shown by BAPS subgroups as described [19]. bPFGE types shown in bold represented widespread clones in Portuguese hospitals and/or aquatic surroundings over years. cMost Efm isolates expressed resistance to vancomycin, teicoplanin, erythromycin, ampicillin, ciprofloxacin (92–100%) and to a lesser extent to high levels of kanamycin (65%), gentamicin (41%), streptomycin and tetracycline (28% each). While acm was identified in different CC17 and non-CC17 lineages (76%), esp was detected in CC17 isolates (35%, ST132 and its SLVs ST368, ST369) and hyl was sporadically found (9%, ST18, ST125, ST132, SLVs of each other, and ST280 isolates) [25]. Efs isolates (mostly ST6) showed resistance to vancomycin, teicoplanin, erythromycin, ciprofloxacin, high levels of gentamicin and kanamycin (82–100%), tetracycline and chloramphenicol (65% each) and high levels of streptomycin (46%), and mostly contained gelE and agg (>90%), cyl (82%) and esp (46%) [26]. dTn1546 designation is based on the results obtained by a PCR assay described by Woodford et al. consisting on the amplification of overlapped fragments covering the whole Tn1546 [68]. Fragments of unexpected length were further analysed by sequencing (this study) [27]. eThe total rep/rel/TA content of isolates is represented according to its location on plasmids of different size ranges. Rep (normal cells), rel (cells with dots) and TA (cells with diagonal stripes) genes belonging to the same plasmid are represented with the same color and that belonging to the same plasmid family with the same range of colors. The content of VanA plasmids including rep, rel, and TA genes is indicated according to the plasmid type in which they were identified, as well as by the numeric nomenclature used by Jensen et al. [72] for replicases (rep1, rep2, rep9, rep14, rep17, rep18a), given new and consistent designations to replicases non described in reference 72 (rep18b, rep18c, rep20, rep22). Relaxases were designated per numerical order as designed by M. V. Francia (unpublished data). Rolling-Circle plasmids are represented in green (rep14/pRI1-like, rel1/pRI1), small-theta replicating plasmids in violet (rep18a/pEF418, rep18b/pB82, rep18c/pCIZ2, rel2/pCIZ2), Inc18-like plasmids in different red tones (rep1/pIP501, rep2/pRE25/pEF1, rel6/pEF1, TAInc18-ω-ε-ζ), RepA_N plasmids in different blue tones, pRUM in dark blue (rep17/pRUM, rel3/pRUM, TApRUM-Axe-Txe), pLG1 in turquoise (rep20/pLG1), pheromone-responsive plasmids in light blue (rep9/pAD1, rel5/pAD1, rel9/pCF10, par pAD1), and pHTβ/pMG1 plasmids in grey (rep22/pHTβ, rel8//pHTβ). Rep families are named Rep ˝n˝ where ˝n˝ indicates the number assigned to different rep-families according to Jensen et al. [72]. The name of the most representative plasmid of the family is also represented for a better follow-up of the results (e.g. rep17/pRUM, rep17 from pRUM and related plasmids p5753cB and pS177; rep1/pIP501 rep1 linked to Inc18 plasmids as pIP501, pIP816 and pRE25; rep9/pAD1, rep9 linked to pCF10, pAD1, pTEF1, pTEF2, pBEE99, pMG2200; rep14/pRI1-like, rep14 associated with RCR plasmids pEFNP1, pJS42 and/or pRI1; rep18a/pEF418, rep18 from pEF418; and rep22/pHTβ, rep of both pHTβ and pMG1 plasmids). We further specified the name of different plasmids associated with a given group if necessary. For example, it results helpful for Inc18 family given the number of plasmids containing the same rep gene. These plasmids are increasingly identified among isolates of different origins (e.g. rep2/pRE25/pEF1 for designing rep2, as rep and rel modules of pEF1, a plasmid originally identified in olives [35], seems to be widely present in all Efm clinical isolates). Sequencing identified the different variants within these families (see text). Rep18b, rep18c and rep20 were not included in Jensen's scheme [72] and the numbers were assigned in this paper following that numeration (rep18b/pB82, rep from pB82; rep18c/pCIZ2, rep from pCIZ2; rep20/pLG1, rep from pLG1). Rel genes were arbitrarily designated with numbers corresponding to different plasmid types [9] (Francia et al, unpublished data): Rel1, pJS42, pRI1; Rel2, rel from p200B, pCIZ2 and/or pB82 plasmids; Rel3, pRUM; Rel5, rel from pAD1, pTEF1, pAM373 and the pathogenicity island of V583; Rel6, pEF1; Rel8, pHTβ and pMG1; Rel9, pCF10. Toxin-antitoxin systems included Axe-Txe from pRUM, ω-ε-ζ from Inc18 plasmids and par from pAD1. Genes hybridizing in the same band as vanA plasmids appear in bold rectangles.
It is worthwhile to note the possible relatedness between isolates of different STs (Figure 1 and 2). They include some isolates linked to BAPS 3–3 subgroup as ST18, ST80, ST125, ST132, ST368, ST369, all SLVs of each other, with PFGE patterns differing in less than 8 bands difference. Similarly, strains identified as ST280 and ST391, both linked to BAPS group 3–1, showed related PFGE patterns despite being trilocus variants (≤ 8 bands difference).
vanA-Tn1546 is located on highly transferable mosaic plasmids involving narrow host pRUM and pAD1 derivatives
The plasmid content of the isolates studied appears in Figure 2. Efm isolates carried a variable number of plasmids (n = 1–6) which contained specific sequences of different families including rolling-circle plasmids (RCR) related to pRI1 and small theta plasmids related to pCIZ2, RepA_N (pRUM-like, pLG1), pHTβ (present in all ST132 isolates), and Inc18 (pRE25 and pEF1-related). All Efs contained RCR plasmids and pheromone responsive-plasmids.
vanA-Tn1546 was located on plasmids ranging from 30 to 150 kb, successfully transferred by conjugation in 95% (n = 71/75) of Efm and 97% (n = 28/29) of Efs, with a variable frequency (10−1–10−8). Transferable plasmids were identified as members of pRUM and Inc18 families or were mosaic plasmids of pRUM, Inc18 and pheromone plasmids (see sections below). Although some of these mosaic plasmids were detected in both Efm and Efs hosts, species-specific plasmid variants were predominant.
We have classified the enterococcal plasmids according to the content in rep/rel/TA systems, and RFLP profiles (Table 1, Figure 2). For the better interpretation of the results, we should keep in mind that members of the most common plasmid families classified in this and other studies as Inc18-like (pRE25, pIP501, pVEF1, pVEF2, pVEF3, pIP816, pEF1, pWZ909) or pRUM-like (pRUM, p5753cB, pS177) exhibit a high degree of modular dissociability or propensity for independent variation and shuffling, and may contain multiple replicons or be devoid of conjugation systems, thus making it very difficult to establish an accurate classification and to trace the origin of certain elements [9], [33]–[40]. See Clewell et al. for a comprehensive updated revision of enterococcal plasmids [9]. In the following sections we will describe vancomycin resistant plasmids of Efm and Efs.
Table 1. Plasmids identified in this study.
| RFLP type | VanA modular profile | Size | No. isolates | Tn1546 | PFGE type | City | Year |
| RFLP_1 | Rep17.2::Rel6 | 60 | 1 | A | ST190_H98 | Coimbra | 1998 |
| RFLP_2 | Rep17.2::Rel6 | 80 | 1 | A | ST18_H92 | Coimbra | 2000 |
| RFLP_8 c | Rep17.2::Rel6 | 120 | 1 | PP2b | ST18_H70 | Coimbra | 2001 |
| RFLP_9 c | Rep17.2::Rel6 | 60 | 1 | PP2b | ST18_H70 | Viseu | NI |
| RFLP_10 c | Rep17.2::Rel6 | 60 | 3 | PP2b | ST18_H70, H93 | Coimbra, Viseu | 2002 |
| RFLP_11 | Rep17.2::Rel6 | 60 | 1 | PP27 | ST18_H87 | Coimbra | 2002 |
| RFLP_3 b | Rep17.2::Rel6 | 95 | 3 | PP4 | ST18_H108 | Coimbra | 1998–2000-NI |
| RFLP_4 b | Rep17.2::Rel6 | 85 | 2 | PP4 | ST670_H90; ST18_H81 | Coimbra | 1997–2001 |
| RFLP_7 | Rep17.2::Rel6 | 50 | 1 | PP5 | NI | Viseu | 2008 |
| RFLP_6 b | Rep17.2::Rel6 | 80 | 1 | PP5 | ST18_H70 | Coimbra | NI |
| RFLP_5 b | Rep17.2::Rel6 | 90 | 12 | PP3, PP4, PP5, PP24 | ST18_H78, H72, H94, H123, H129 | Coimbra, Porto, Matosinhos | 2001–2007 |
| RFLP_5.2b | Rep17.2::Rel6 | 90 | 2 | PP5 | ST280_ H100 | Porto, Viseu | 2002–2003 |
| RFLP_5.3b | Rep17.2::Rel6 | 90 | 1 | PP5 | ST125_H126 | Matosinhos | 2007 |
| RFLP_5.3’b | Rep17.2::Rep2:: Rel6 | 85 | 2 | PP5 | ST132_H103 | Coimbra | 2002–2003 |
| RFLP_5.2’b | Rep17.2::Rep2:: Rel6 | 90 | 1 | PP4 | ST132_H132 | Coimbra | 2001 |
| RFLP_5.4’b | Rep17.2::Rep2:: Rel6 | 90 | 1 | PP5 | ST280_ H71 | Viseu | 2003 |
| RFLP_5.5b | Rep17.2::Rep2:: Rel6 | 75 | 1 | PP5 | ST18_H125 | Matosinhos | 2007 |
| RFLP_6.4 | Rep17.2::Rep2:: Rel6 | 85 | 1 | PP5 | ST366_H99 | Coimbra | 2000 |
| RFLP_20 | Rep17.2::Rep2:: Rel6 | 30 | 1 | A | ST656_H130 | Vila Real | 2008 |
| RFLP_12 a | Rep17.2::Rep2:: Rel6 | 40 | 1 | PP10 | ST18_H83 | Coimbra | 1996 |
| RFLP_13 b | Rep17.2:: Rel6::TAInc18 a | 60 | 1 | PP5 | ST280_ H71 | Oporto | 2002 |
| RFLP_18 | Rep17.2:: Rep1:: Rel6:: TAInc18 | 50 | 1 | PP13 | ST132_H86 | Oporto | 2001 |
| RFLP_16 | Rep17.2:: Rep1:: Rep2:: Rel6::TAInc18 | 50 | 1 | PP13 | ST18_H78 | Oporto | 2001 |
| RFLP_17 | Rep17.2:: Rep1:: Rep2:: Rel6::TAInc18 | 110 | 1 | PP13 | ST132_H88 | Oporto | 2001 |
| RFLP_19 | Rep17.2:: Rep1:: Rep2:: Rel6::TAInc18 | 60 | 3 | PP13, PP20, PP23 | ST132_H119 | Oporto | 2002 |
| RFLP_19 | Rep17.2:: Rep1:: Rep2:: Rel6::TAInc18 | 60 | 2 | PP17, PP20 | ST368_SWH | Oporto | 2001 |
| RFLP_19.1 | Rep17.2:: Rep1:: Rep2:: Rel6::TAInc18 | 60 | 1 | X | ST369_RP | Oporto | 2003 |
| RFLP_21 | Rep17.2:: Rep2:: Rel6:: TApRUM | 65 | 1 | PP15 | ST719_H96 | Oporto | 2001 |
| RFLP_22 | Rep17.2:: Rep2:: Rel6:: TApRUM | 30 | 1 | PP16 | ST132_SWC | Oporto | 2002 |
| RFPL_27d | Rep9: Rep2: Rep1:: Rel5::TApAD1 | 75–85 | 4 | PP2a, PP4 | ST6_HB, ST55_HG, ST159_HN | Coimbra | 1996–2002 |
| RFPL_27.3d | Rep9: Rep2: Rep1:: Rel5::TApAD1 | 85 | 2 | PP4 | ST6_HB, ST159_HN | Viseu | 2001–2002 |
| RFPL_27.1d | Rep9: Rep1:: Rel5:: TApAD1 | 75 | 1 | PP4 | ST6_HB | Oporto | 2001 |
| RFPL_27d | Rep9: Rep2: Rep1:: Rel5 | 85 | 1 | PP9 | ST132_H106 | Coimbra | 2000 |
| RFPL_28.5 | Rep9: Rep2 | 100 | 1 | PP16 | ST80_SWM | Oporto | 2002 |
| RFPL_28 | Rep9: Rep2: Rel5:: TApAD1 | 100 | 2 | PP15, PP16 | ST6_HB | Oporto | 2001–2002 |
| RFLP_29 | Rep9: Rep2: Rel5 | 100 | 1 | A | ST6_HB | Swine | 2007 |
| RFLP_30 | Rep9: Rel9 | 100 | 1 | A | ST30_HK | Oporto | 2001 |
| RFLP_24 | Rep2 | 110 | 1 | PP4 | ST80_H80 | Coimbra | 1997 |
| RFLP_14 | Rep2 | 40 | 1 | PP16 | ST132_SWC | Oporto | 2002 |
| RFLP_15 | Rep1:: Rep2 | 30 | 2 | PP16 | ST18_SWA, ST132_SWC | Oporto | 2001 |
| RFLP_23 | Rel6 | 85 | 1 | PP9 | ST16_H74 | Coimbra | 2000 |
| RFLP_26 | Rep20:: Rel6 | 150 | 1 | D | ST5_SA | Oporto | 2002 |
| RFLP_25 | – | 120 | 1 | PP5 | ST391_H124 | Covilhã | 2007 |
Abbreviations: RFLP, restriction fragment length polymorphism; ST, sequence type; NI, not identified.
Plasmid type RFLP_12 (Rep17.2/pRUM-like + Rep2/pRE25/pEF1 + Rel6/pEF1) contains a partial sequence of the replication gene of the RCR plasmid pEFNP1 (GenBank accession number AB038522), suggesting the integration of this RCR plasmid on the mobile element carrying Tn1546 involving truncation of the rep14/pRI1/pEFNP1.
Plasmid types RFLP_3, _4, _5, _6 and _13 (Rep17.2/pRUM-like + Rel6/pEF1 and eventually containing Rep1/pIP501, Rep2/pRE25/pEF1 or TAInc18) shared common bands and were identified in the same or different clonal backgrounds in different cities for extended periods of time.
Plasmids types RFLP 8, _9 and _10 also shared a variable number of common bands.
Plasmids showing patterns related to RFLP_27 (75–85 kb; rep9/pAD1 + rel5/pAD1 + rep1/pIP501 + par pAD1 and/or rep2/pRE25/pEF1) initially recovered from the widespread ST6-CC2 Efs clone in Coimbra in 1996 and other Efs (ST55 and ST159) and Efm clones contained similar ISEf1-Tn1546 variants (PP-2a, PP-4, PP-9). Other highly related mosaic Inc18-pAD1-related plasmids carrying IS1216-Tn1546 were recovered from ST6 VREfs and ST80 VREfm isolates (type ˝IIEfs ˝, rep9/pAD1 +rel5/pAD1 + par pAD1 + rep2/pRE25/pEF1 versus type ˝IIEfm ˝, rep9/pAD1 + rep2/pRE25/pEF1).
vanA plasmids of E. faecium
They were classified in two broad groups according to the plasmid replication modules and the background epidemiological context, i) pRUM-like variants (Rep17.2/pRUM-like+ Rel6/pEF1±Rep1/pIP501± Rep2/pRE25/pEF1/TAInc18), ii) mosaics of Inc18-pRUM-like (Rep2/pRE25/pEF1 ± Rep17.2/pRUM/TAAxe-Txe). Highly transmissible pAD1-Inc18 mosaic plasmids from major Efs clones were also identified among Efm but they will be described in the next section.
pRUM derivatives (rep17.2/pRUM-like+rel6/pEF1) of variable size (30–120 kb) were detected since the mid 90 s from a diversity of clonal backgrounds. pRUM plasmids showing different ClaI-digested DNA RFLP patterns were identified carrying a whole copy of Tn1546 (RFLP_1, RFLP_2, RFLP_20, 30–80 kb), IS1216::Tn1546 (RFLP_8–12, 40–120 kb) or ISEf1::Tn1546 (RFLP_3–7, RFLP_13, 50–95 kb). Despite the heterogeneity of plasmid profiles, RFLP_3–6 or RFLP_8–10 shared a variable number of common bands that suggest a relationship among them (see Table 1 and Figure 3 for details about relationships among plasmids). pRUM-like plasmids exhibiting distinct RFLP profiles and carrying different transposon variants were isolated in early and recent isolates of different clonal backgrounds (Figure 2). They include ST190, carrying a 60 kb plasmid RFLP_1 type; ST670 carrying a 85 kb exhibiting a RFLP_4 plasmid type; ST656 carrying a 30 kb plasmid designated as RFLP_20, and ST18, ST132, ST280, carrying different transposon variants. These results suggest multiple independent acquisitions of pRUM-like plasmids and further rearrangements with other elements, some plasmid variants being efficiently transferred among a diversity of different clones. It is of interest to highlight that epidemic ST18 PFGE types H83 (1996) and H92 (2000) harboured two pRUM-like plasmids. One was the rep17.2/pRUM-like::rel6/pEF1 vancomycin resistant plasmid showing RFLP_2 and RFLP_12 and the other was a 25 kb carrying a rep17.1/pRUM gene and a copy of the Axe-Txe toxin-antitoxin system (rep17.1/pRUM+TAAxe-Txe) identical to the pRUM derivatives described to date (pRUM, p5753cB and pS177) (GenBank accession number GQ900487; Figure 2) [12], [38], [39] and other vancomycin resistant plasmids circulating at international level (Freitas et al., unpublished data). Diversification in the Rep sequences of these pRUM-like plasmids (homology of 96% at nucleotide level and 95% at protein level) might have resulted in the compatibility with similar (but not identical) plasmids in the same clonal background along extended periods of time.
Inc18 plasmids and mosaic Inc18-pRUM plasmids. Clonally related ST132 and ST18 Efm isolates from Oporto contained Inc18 plasmids (Rep1/pIP501 ± Rep2/pRE25/pEF1, RFLP_14–15) or mosaic plasmids of Inc18 and pRUM (Rep2/pRE25/pEF1+Rep1/pIP501+TAInc18+Rep17.2/pRUM-like+RelpEF1, RFLP_16–19), all carrying IS1216-Tn1546 variants. Plasmids showing RFLP types 16–19 were highly similar (5 bands/12 bands in common), RFLP_19 being persistently recovered from clonally related ST132, ST368 and ST369 isolates, collected from hospitalized patients of HSA near by sewage plant and the river Douro from 2001 to 2003. This RFLP_19 has been also identified in a VREfm isolate recovered from swine in 2007 (Tn1546 type “PP-31”, RFLP_19.1), highlighting the remarkable stability of particular VanA Inc18 plasmids in ensembles of related clones able to spread in different hosts [10]. A diversity of Tn1546::IS1216 variants (PP-13, PP-17, PP-20, PP-23, PP-31 and X) which differed in the number of IS1216 copies, the presence of insertions identified as short regions of Inc18-like plasmids or duplicated Tn1546 sequence fragments in different orientations, were identified among related plasmids showing the RFLP_19 pattern (Table 1, Figure 4). These results illustrate the possibility of efficient intraclonal and intraplasmid diversification of Tn1546::IS1216 variants. Acquisition of a vanA-Inc18 (rep2/pRE25/pEF1 + rep1/pIP501+ ω-ε-ζ) plasmid carrying a Tn1546::IS1216 “variant”, predominant among poultry from Europe [41] by Portuguese strains containing VanA-pRUM (rep17.2/pRUM-like+rel6/pEF1) plasmids cannot be excluded. Recombination between pRUM::Tn1546 and Inc18::Tn1546 would explain duplicated Tn1546 regions.
Megaplasmids. Tn1546 type “D” was located on a megaplasmid carrying rep20/pLG1 and rel6/pEF1 from isolates of a CC5 Efm clone spreading among swine and humans of different continents. This transposon has been previously associated with isolates from swine which frequently exhibit the G8234T mutation. The variable size (150–190 kb) of vanA megaplasmids linked to CC5 lineage has been previously reported [10].
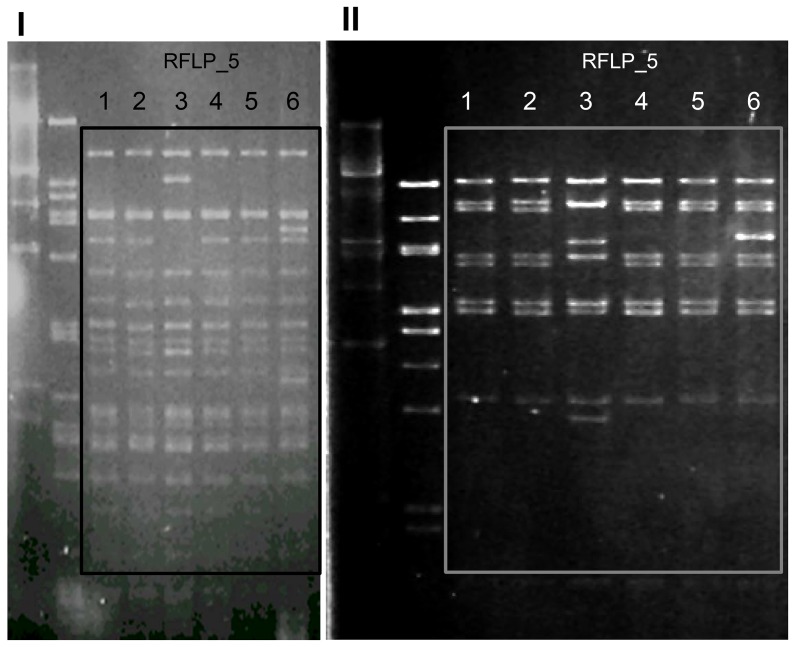
Figure 3. Restriction fragment length polymorphism patterns of plasmids showing RFLP_5 profiles after digestion with ClaI (I) and EcoRI (II) restriction enzymes (New England Biolabs Inc, UK).
Lane 1, RFLP_5 (PFGE H78, ST18 Efm,); lane 2, RFLP_5 (PFGE H72, ST18 Efm); lane 3, RFLP 5.2 (PFGE H100, ST280 Efm), lane 4, RFLP 5 (PFGE H78, ST18 Efm); lane 5, RFLP_5 (PFGE H78, ST18 Efm); lane 6, RFLP_5.2’ (PFGE H132, ST132 Efm).
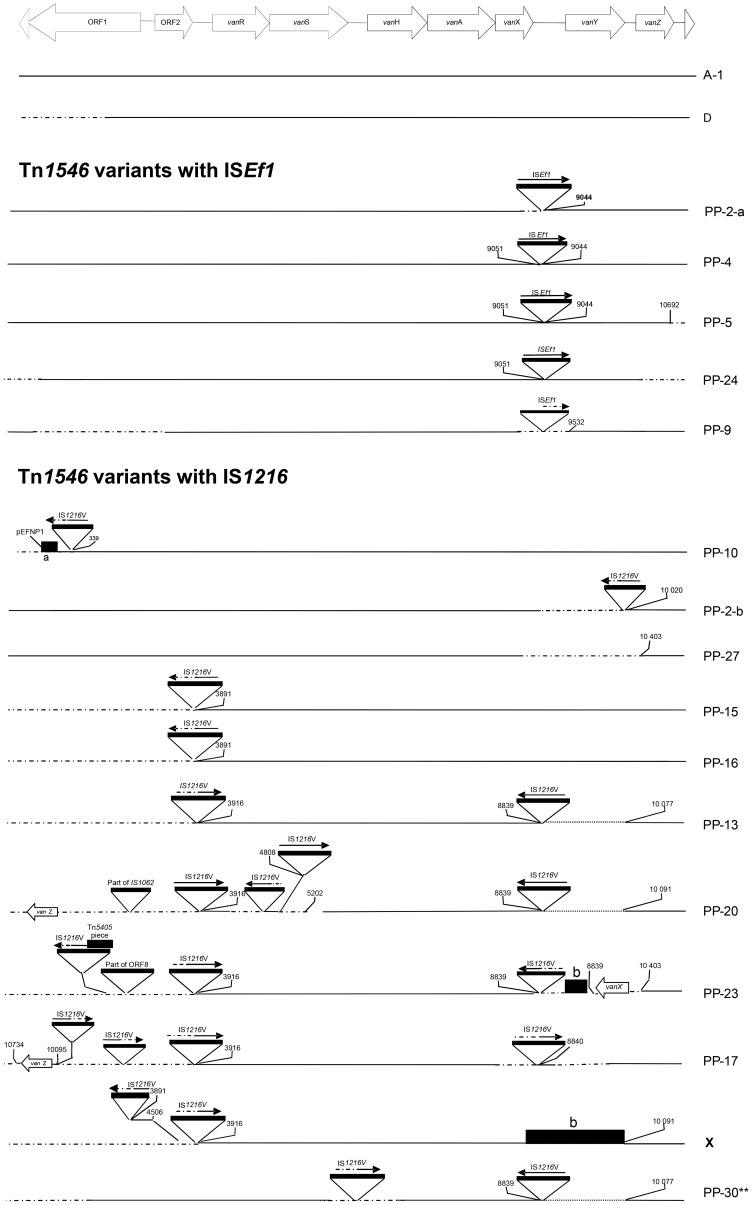
Figure 4. Genetic maps of Tn1546 variants.
Tn1546 variants are represented as previously described by Novais et al. [27] although grouped differently and specific types have been further explored (PP10, PP30): Tn1546 prototype A corresponds to the original sequence described by Arthur et al. [77] and D corresponds to Tn1546 variants from animals. Tn1546 variants with ISEf1 within vanX-vanY intergenic region (PP2a, PP4, PP5, PP9, PP24) and Tn1546 variants with IS1216 insertions at different positions (PP10, PP2b, PP13, PP15, PP16, PP17, PP20, PP23, PP27, PP30, X) are represented. The positions of genes and open reading frames and the direction of transcription are depicted with open arrows. IS elements are represented by triangles; other sequences are designated by rectangles. DNA insertions are represented highlighting the first nucleotide upstream and downstream from the insertion sites whenever known. Deletions are indicated by dots and discontinuous lines indicate sequences that were not characterized. (a) DNA sequence with homology to ORF3 (unknown protein product) and ORF1 (replication protein) of pEFNP1 plasmid (GenBank accession number AB038522). (b) DNA sequence with no match to any sequence available in GenBank. (*) PP23 was identified in an isolate susceptible to teicoplanin; this variant contained an insertion in the vanY gene that would affect the transcription of vanZ and it might explain the susceptibility to this glycopeptide as previously reported [27]. (**) PP30 was identified in an ST78 isolate susceptible to both glycopeptides (MIC against vancomycin and teicoplanin of 4 mg/L) carrying vanA-Tn1546. This variant contained alterations within the vanS-vanH intergenic region (an IS1216 insertion), which is involved in the expression and regulation of the resistance to vancomycin, and it constitutes the first description of a vanA isolate phenotypically susceptible to vancomycin in Portugal.
E. faecalis vanA plasmids
The vanA Efs plasmids were Inc18-pheromone-responsive mosaics, further classified in four main types on the basis of their RFLP patterns (RFLP_27–30), rep-rel/TA content, and replicase sequences. These plasmids have been documented in different Portuguese hospitals since the mid 90 s [26].
Plasmids showing highly related patterns designated as RFLP_27 (carrying ISEf1-Tn1546) or RFLP_28 (carrying IS1216-Tn1546) were recovered from both Efs (ST6, ST55, ST159) and Efm (ST80, ST132). However, despite the similarity of their RFLP patterns, they differed in the rep/rel/TA content and transposon variant content (Table 1). Conversely, the finding of an ST117 Efs isolate from Oporto with two different vanA plasmids of 150 kb and 300 kb indicates acquisition and further recombination of widespread pRUM-vanA plasmids from Efm with narrow host pheromone responsive plasmids of Efs.
The observed differences in transposon variants and plasmid modules reflect frequent rearrangements during transfer of plasmids between Efs and/or Efm clonal backgrounds and also highlight the connectivity of these enterococcal populations resulting in the acquisition and generation of plasmids with enhanced host range.
Fixation of vanA-Tn1546 variants is associated with plasmid connectivity
Tn1546 backbones were classified in three main groups corresponding to Tn1546 with no insertion sequences (“type A” and “type D”) and variants containing ISEf1 (5 types) or IS1216 (11 types) at different locations of the Tn1546 backbone (Figure 4). Variants with a single copy of ISEf1 within the vanX-vanY region at nt 9044 were located on early (1996–1997) Efm plasmids identified as Inc18 and pRUM lacking Axe-Txe, and also on early (1996) Efs Inc18-pAD1 mosaics. Some of them were isolated from strains for more than one decade, which can be explained by their successful long-term recovered clonal and plasmid backgrounds.
Variants containing IS1216 were mostly located on Inc18 plasmids or on mosaic plasmids Inc18-pRUM or Inc18-pAD1. Most variants contained the IS1216 at 8839nt of the transposon (PP13, PP17, PP20, PP23, PP30) similarly to other Tn1546 variants previously described in Europe [42]. Some of them also harboured different insertions corresponding to unknown sequences (X, PP23) or RCR plasmid sequences (PP10) [43] suggesting frequent recombination between acquired genes/plasmids and housekeeping Efm and Efs plasmids (Figure 4). Tn1546 type D was specifically linked to megaplasmids from CC5 Efm from swine of different continents (Figure 2, Figure 4).
The presence of early plasmids carrying Tn1546 belonging to different families suggests independent acquisitions of the transposon by pRUM and Inc18 plasmids, which would have been acquired by diverse Efm and Efs populations. Local fixation would be influenced by connectivity of plasmid and population backgrounds enabling further evolvability of transposon variants.
Discussion
This paper shows the local dynamics of Tn1546-vanA among Enterococci is shaped by horizontal genetic transfer of pRUM and Inc18 plasmids and by recombination-driven evolution of them within and between Efs and Efm clones. The clonal diversity reported in this study has also been observed in areas where the spread of VRE has been documented [44]. Recent retrospective analysis of enterococcal populations suggests that the temporal evolution of the population biology of Enterococci is driven by a succession of epidemic waves of enterococcal human specific lineages, Efm ST78 and Efs ST6 emerging in the last decade at global scale similarly to that reported for other pathogens [19], [23], [24]. In Portugal, the population structure of VRE analysed in this study comprises isolates of main human Efm lineages, ST18 (ST18, ST132) being much more abundant than ST17 (represented by a single isolate of early ST16 lineage) [31], or ST78 (represented by sporadic ST80 and ST656, the first one linked to early VRE outbreaks) [25], [29]. It is worthwhile highlighting the recent detection of isolates of another Efm lineage in hospitals of the Oporto area (http://www.mlst.net) as ST117 Efm (ST78 lineage), which would reflect the increasing trend of isolates belonging to the ST78 lineage at international level. However, regional differences in the rates of VRE cannot be fully explained by clonal replacement dynamics since similar enterococcal clones appear widely distributed in areas with high and low rates of VRE (Tedim AP et al., unpublished data). Instead, local conditions, including type and density of hosts, antibiotic usage, and transmission facilities, may influence regional differences in the proportions of VRE, as suggested by mathematical modelling studies on local trends of antibiotic resistance [45], [46]. Clones can locally evolve by variation, drift and short-distance migration, leading to changes in colonization ability, pathogenicity or even host range, the fittest clonal variants being able to facilitate the spread of antibiotic resistance [23], [47]–[50]. The observed clonal heterogeneity of the predominant ST18 lineage which comprises particular ST18 and ST132 strains widespread in different cities, highlights the role of certain efficiently transmissible clones in the dissemination of antibiotic resistance. Succesful clones can eventually be able to disseminate at international level as strains of ST6 Efs or ST280 Efm within main Efm human lineages driving or contributing the spread of different traits as Tn1546 or Tn1549 [51]. One remarkable fact is the similarity among PFGE patterns of isolates with different STs. Given the high content of plasmids and transposons of the isolates studied, and the frequent rearrangements identified among Efm and/or Efs isolates [21], chromosomal transfer can not be discarded. Recent phylogenomic analysis based on the degree of admixture among a diversity of isolates studied suggests that recombination is restricted to isolates within specific BAPS groups [19]. Most plasmids coding for vancomycin resistance are found in similar clonal backgrounds. This observation suggests that recombination does occur within isolates of similar BAPS groups as recently described [19]. However, the observed mosaicism and enhanced host range of particular plasmid variants indicates the existence of an unexpectedly high degree of connectivity between phylogenetically distant enterococcal populations and/or in bacterial genetic exchange communities integrating enterococci.
Broad host and narrow host plasmids carrying vancomycin resistance would have a high “betweenness centrality”, which is a pivotal index in network theory useful for measuring the load placed on the given node in the network as well as the node's importance to the network than just connectivity [52]. A recent in silico network analysis of all plasmid sequences available at the GenBank databases confirms very high ˝betweenness ˝ values for some Inc18 plasmids as pVEF3 (an Inc18 derivative highly spread among Efm from animals in Europe) [13], [37], and also for a pheromone-responsive plasmid pTEF1 (a plasmid recovered from ST6_Efs strain V583, highly related to the ST6 described in this work) [53] (unpublished data). Other plasmids with a high degree of modular dissociability, would be pRUM-like elements, which may enhance their complexity resulting in new configurations with enhanced betweenness. It is tempting to suggest that plasmid variability has contributed to intra-clonal diversification both in Efm and Efs, giving rise to a local wealth of clonal variants able to fully explore the local adaptive landscape. In fact, this and other studies demonstrate that selected variants of Inc18, pAD1, and pRUM plasmids can determine differences in the dynamics of VRE in different areas, further influencing the plasmid host range and the selection of specific clones within human adapted lineages. Examples of widespread plasmid variants of Inc18 or pRUM plasmids coding for vancomycin resistance have been reported recently. They included Inc18 widespread among Efm poultry isolates from Europe [13] or among Efs clinical isolates from the USA, the last one being able to transfer Tn1546 to S. aureus [15]; and mosaics of pRUM variants containing Axe-Txe and Inc18 from humans in different continents (Freitas AR et al. unpublished data). The identification of chimeric pRUM-Inc18 plasmids containing rep/rel/TA of Inc18 sequences and Tn1546 variants widely observed in poultry, hospitals and hospital sewage in the Oporto area reflects genetic exchanges between enterococci from different origins and highlights the need to enforce barriers to avoid the spread of multidrug resistance human pathogens to the environment and viceversa.
In this scenario, the genetic context of Tn1546 seems to greatly influence the evolvability of the transposon and explains the high diversity of variants found in this and other studies [1], [27], [42], [54]. The frequent presence of insertions in the backbone of Tn1546 and the abundance of IS1216 and ISEf1 in enterococcal genomes [9], [55] makes homoplasic evolution of Tn1546 in different backgrounds possible. However, other IS (IS1251, IS1542, IS1476, IS19 and IS1485) linked to different plasmid and clonal backgrounds [9], [40] have been identified at different sites of Tn1546, thus suggesting that chance and selection are responsible to differences in variants collected in different areas. The widespread of Inc18 plasmids with a common origin in Europe [13], [56] indicates local fixation of Tn1546 influenced by a founder effect and further connectivity of plasmid and population backgrounds enabling further evolvability of transposon variants as reported in this study.
Our results suggest that VRE spread is facilitated by selected clones of different lineages through strong interactive processes of clonalization and plasmid diversification that might occur at local scales. Despite the maintenance of significant gene flow, a sympatric, or more probably, parapatric bacterial clonalization process (when diverging populations share a common or neighbouring environment), might contribute to the formation of temporary genetic mosaics and the preservation of ecologically important genomic traits [57]. Such micro-evolutionary process will result in an array of clonal complexes forming a population structure able to exploit the local spatio-temporal patch heterogeneities [58]. Note that exploitation of connected microenvironments should accelerate evolution of antibiotic resistance [59]. The expected result of such a successful population structure is the local persistence of antibiotic resistant clones, and eventually the local fixation [60] of vancomycin-resistance [46].
In summary, this study highlights the relevance of studying the local microecology of genes, elements, lineages and populations to decipher the robustness of the trans-hierarchical networks connecting these evolutionary elements in order to describe and predict the local evolvability of vancomycin-resistance [61]. Traditional surveillance studies are one-off cross sectional surveys focused on single traits as epidemic strains, genes or mobile genetic elements over limited periods of time which only gives one shot view that precludes addressing the long-term dynamics of antibiotic resistance. The more comprehensive approach described in this study is needed for understanding in depth the evolution of complexity in multihierarchical systems as those involved in the spread of antibiotic resistance among the populations of bacterial human pathogens.
Materials and Methods
Bacterial strains and epidemiological background
One hundred four VRE clinical isolates carrying Tn1546 from different regions of Portugal, 75 VREfm and 29 VREfs, were analyzed in this study. They included: i) clinical isolates from hospitals of Coimbra (Hospital Universitário de Coimbra, HUC), Oporto (Hospital Santo António, HSA), Viseu (Hospital de São Teotónio, HST); Matosinhos (Hospital Pedro Hispano, HPH), Vila Real (Hospital S. Pedro, HVR) and Covilhã (Centro Hospitalar da Cova da Beira, CHCB) located in Northern and Central Portugal (62 Efm and 26 Efs; 1996–2008); ii) isolates from waste waters of hospitals (HSA and Hospital de São João, HSJ) (10 Efm and 3 Efs), and iii) isolates from the estuary of the River Douro (3 Efm) recovered in the Oporto area during 2001–2003. Part of the isolates analyzed in this work corresponds to strains from previous surveillance studies [25]–[27], [62]; this paper constitutes the first description of isolates obtained during 2007 and 2008. Contemporary Portuguese VRE isolates of animal origin were used for comparative analysis of lateral transfer events [10].
Susceptibility against 15 antibiotics was determined by the agar dilution method following CLSI standard guidelines. Clonal relatedness was established by pulsed-field gel electrophoresis (PFGE), banding patterns were interpreted according to criteria previously suggested for long-term studies, and multilocus sequence typing (MLST) as described elsewhere (http://efaecium.mlst.net) [25], [63]–[65].
The presence of putative virulence traits [collagen-binding adhesin (acm), enterococcal surface protein (esp), hyaluronidase (hylE. faecium), cytolysin/hemolysin (cyl), gelatinase (gelE) and aggregation substance (agg)] was searched by using PCR as described [66], [67].
Genetic context of Tn1546
Characterization of Tn1546 backbone was determined by amplification of overlapping transposon fragments and further sequencing of PCR products [27], [68]. We have accomplished the analysis for the isolates not studied in previous surveys and have interpreted the resulting transposon diversity (this study) [27], under the light of the plasmid and clonal backgrounds identified in this geographical area.
Plasmid analysis
Isolates (n = 62 Efm and n = 13 Efs) representing the clonal diversity observed in both species were selected for plasmid characterization (Table 1, Figure 2). The content and size of plasmids from transconjugants obtained by filter mating were determined by using either the technique described by Barton et al. (plasmids >10 kb) or the alkaline lysis extraction method of Kado & Liu (plasmids <10 kb) [51], [69], [70]. Classification of E. faecium plasmids was based on the presence of specific modules for replication (rep-initiator proteins), mobilization (relaxases) and stability (toxin-antitoxin systems). Relaxases (rel) were sought by a multiplex-PCR-based relaxase typing method which differentiates relaxases of the MOBQ, MOBP, MOBC and MOBV families related to 27 known plasmids [9], [71] (Francia MV, unpublished data). Replication initiator proteins (rep) were investigated by amplification of 24 replicons, which allows discriminating among DNA sequences from more than 100 published Gram-positive plasmids [9], [72]. Designation of rep sequences pointed out the plasmid type in which they were initially identified, as well as the numeric nomenclature originally used by Jensen et al. (Figure 2 ´s footnote) [72]. Toxin-antitoxin systems (TA) previously identified among streptococci and enterococci (Axe-Txe, ω-ε-ζ par, mazEF) or Gram-negative bacteria (relBE) were detected by PCR [73]. PCR products were sequenced in order to confirm the specificity of the method and to analyze similarities with other well-characterized plasmids. Genomic location of the Tn1546 and the rel/rep/TA sequences was determined by hybridization of vanA and rel/rep/TA specific probes obtained by PCR from DNA from reference plasmids with S1 or I-CeuI digested genomic DNA from representative strains [51], [69]. Structural relationship between plasmids of similar size was established by comparison of their RFLP patterns obtained after digestion with different restriction enzymes (EcoRI, HindIII and ClaI; see Figure 3). Plasmid DNA was obtained by using a modified protocol based on the alkaline lysis method described by Handwerger et al. [74] consisting of increasing two-fold the volume of lysozyme, SDS/NaOH and acetate potassium solutions, extending the incubation period in potassium acetate solution for at least three hours, precipitating the supernatant obtained after extraction with phenol-chloroform using ethanol-acetate potassium solution (2∶0.1 vol/vol) at 25°C for at least 2 hours, and resuspending final DNA pellets in 30 µl of water for further enzyme digestion analysis.
Molecular techniques
Southern blot DNA transfer and hybridization were performed by standard procedures [75]. The vanA and rep/rel/TA/bac probes used in the hybridization assays were generated by PCR using well known positive controls as template DNA. Labelling and detection were carried out using Gene Images Alkphos Direct Labelling system kit, following the manufacturer's instructions (Amersham GB/GE Healthcare Life Sciences UK Limited). PFGE was performed as described previously [76] using the following conditions: switch time of 5 s to 25 s for 6 h, followed by 30 s to 45 s for 18 h (S1 nuclease); 5 s to 30 s for 22 h, 14°C, and 6 V/cm2 (I-CeuI) and 1 s to 20 s for 26 h, 14°C, and 6 V/cm2 (SmaI).
Plasmid sequences
Analysis of nucleotide and aminoacid sequences revealed two types of sequences amplified with primers used for identification of rep17/pRUM. They were 100% (designated as Rep17.1/pRUM) or 97% (96% identity at amino acid level; designated as Rep17.2/pRUM-like) homologous to that of RepA_pRUM (GenBank accession number AF507977). Most Rep1/pIP501 aminoacid sequences were 98%–100% identical to RepE_pIP816, a member of the Inc18 family (GenBank accession number AM932524), and to a lesser degree to pRE25, pTEF1 or pSM19035; and Rep2/pRE25/pEF1 showed 96%–100% amino acid identity to that of pEF1 (GenBank acc. no. DQ198088). Sequences identified as Rel6/pEF1 showed 98%–100% homology to orf34_pEF1. Relaxases of the E. faecalis pheromone-responsive plasmids identified in this study displayed a high homology with those of known enterococcal pheromone plasmids pAD1, pAM373 and pTEF1 (orf57_pAD1, GenBank acc. no. AAL59457; EFA0025_pTEF1, GenBank AE016833; and EP0019_pAM373, GenBank acc. no. NC_002630). That of plasmid showing RFLP_27 showed a 67–84% homology with the above mentioned pheromone enterococcal plasmids but 94% identity with a MobC relaxase (annotated as a hypothetical protein) from a vancomycin-resistant S. aureus strain (GenBank acc. no. EIK35827).
Acknowledgments
We are grateful to the personal involved in the gift of the strains from the different Portuguese healthcare institutions: HSA (Hospital Santo António, Porto), HPH (Hospital Pedro Hispano, Matosinhos), CHCB (Centro Hospitalar da Cova da Beira, Covilhã), HST (Hospital S. Teotónio, Viseu), and HVR (Hospital S. Pedro, Vila Real). We are grateful to Lars B. Jensen, Ewa Sadowy, Arnfinn Sundsjford, Guido Werner, and Rob Willems for providing suitable control strains.
Funding Statement
Ana Freitas was supported by a fellowship from Fundação para a Ciência e Tecnologia (SFRH/BD/24604/2005) and from the European Union (LSHE-CT-2007-037410). This work was funded by grants from the European Union (6FPEU-LSHE-CT-2007-037410_ACE and 7FPEU-HEALTH-F3-2011-282004_EvoTAR), the Ministry of Economy and Competitiveness of Spain-Instituto de Salud Carlos III (PS09/02381, PI10/01081, PI12/01581), and Fundação para a Ciência e Tecnologia of Portugal (PTDC/AAC-AMB/103386/2008 and PEst-C/EQB/LA0006/2011). Work in MVFs lab is funded by the the Ministry of Economy and Competitiveness of Spain-Instituto de Salud Carlos III (PI10/01081 and CES08/008) and the Spanish Network for the Research in Infectious Diseases (REIPIRD06/0008/0031). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Bonten MJM, Willems RJ, Weinstein RA (2001) Vancomycin resistant enterococci: why are they here, and where do they come from? Lancet Infect Dis 1: 314–325. [DOI] [PubMed] [Google Scholar]
- 2. Murray BE (2000) Vancomycin-resistant enterococcal infections. N Engl J Med 342: 710–721. [DOI] [PubMed] [Google Scholar]
- 3.Werner G, Coque TM, Hammerum AM, Hope R, Hryniewicz W, et al. (2008) Emergence and spread of vancomycin resistance among enterococci in Europe. Euro Surveill 13: :pii = 19046. [PubMed] [Google Scholar]
- 4. De Lencastre H, Brown AE, Chung M, Armstrong D, Tomasz A (1999) Role of the transposon Tn5482 in the epidemiology of vancomycin-resistant Enterococcus faecium in the pediatric oncology unit of a New York City hospital. Microb. Drug Resist 5: 113–129. [DOI] [PubMed] [Google Scholar]
- 5. Martone WJ (1998) Spread of vancomycin resistant enterococci: why did it happen in the United States? Infect Control Hosp Epidemiol 19: 539–545. [DOI] [PubMed] [Google Scholar]
- 6. Thal L, Donabedian S, Robinson-Dunn B, Chow JW, Dembry L, et al. (1998) Molecular analysis of glycopeptide-resistant Enterococcus faecium isolates collected from Michigan hospitals over a 6-year period. J Clin Microbiol 36: 3303–3308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kawalec M, Gniadkowski M, Hryniewicz W (2000) Outbreak of vancomycin-resistant enterococci in a hospital in Gdansk, Poland, due to horizontal transfer of different Tn1546-like transposons variants and clonal spread of several strains. J Clin Microbiol 38: 3317–3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stampone L, Del Grosso M, Boccia D, Pantosti A (2005) Clonal spread of a vancomycin-resistant Enterococcus faecium strain among bloodstream-infecting isolates in Italy. J Clin Microbiol 43: 1575–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clewell DB, Weaver KE, Dunny GM, Coque TM, Francia MV, et al. (2013) Extrachromosomal and Mobile Elements in Enterococci. Transmission, Maintenance, and Epidemiology. In: Clewell DB, Shankar N, Ike Y, and Gilmore M, editors. The Enterococci: Pathogenesis, Molecular Miology and Antibiotic Resistance. In revision. [PubMed]
- 10. Freitas AR, Coque TM, Novais C, Hammerum AM, Lester CH, et al. (2011) Human and swine hosts share vancomycin-resistant Enterococcus faecium CC17, CC5, and Enterococcus faecalis CC2 clonal clusters harboring Tn1546 on indistinguishable plasmids. J Clin Microbiol 49: 925–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Laverde Gomez JA, Van Schaik W, Freitas AR, Coque TM, Weaver KE, et al. (2010) A multiresistance megaplasmid pLG1 bearing a hylE. faecium genomic island in hospital Enterococcus faecium isolates. Int J Med Microbiol 301: 165–175. [DOI] [PubMed] [Google Scholar]
- 12. Rosvoll TC, Pedersen T, Sletvold H, Johnsen PJ, Sollid JE, et al. (2010) PCR-based plasmid typing in Enterococcus faecium strains reveals widely distributed pRE25-, pRUM-, pIP501- and pHTbeta-related replicons associated with glycopeptide resistance and stabilizing toxin-antitoxin systems. FEMS Immunol Med Microbiol 58: 254–268. [DOI] [PubMed] [Google Scholar]
- 13. Sletvold H, Johnsen PJ, Wikmark OG, Simonsen GS, Sundsfjord A, et al. (2010) Tn1546 is part of a larger plasmid-encoded genetic unit horizontally disseminated among clonal Enterococcus faecium lineages. J Antimicrob Chemother 65: 1894–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tomita H, Pierson C, Lim SK, Clewell DB, Ike Y (2002) Possible connection between a widely disseminated conjugative gentamicin resistance (pMG1-like) plasmid and the emergence of vancomycin-resistance in Enterococcus faecium . J Clin Microbiol 40: 3326–3333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhu W, Murray PR, Huskins WC, Jernigan JA, McDonald LC, et al. (2010) Dissemination of an Enterococcus Inc18-Like vanA plasmid associated with vancomycin-resistant Staphylococcus aureus . Antimicrob Agents Chemother 54: 4314–4320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Valdezate S, Miranda C, Navarro A, Freitas AR, Cabrera JJ, et al. (2012) Tn1546 plasmid in a haemo-oncology ward of a Spanish hospital. J Antimicrob Chemother 67: 832–836. [DOI] [PubMed] [Google Scholar]
- 17. Garcia-Migura L, Sanchez-Valenzuela AJ, Jensen LB (2011) Presence of glycopeptides-encoding plasmids in enterococcal isolates from food and humans in Denmark. Foodborne Pathog Dis 8: 1191–1197. [DOI] [PubMed] [Google Scholar]
- 18. Qu TT, Yang Q, Shen P, Wei ZQ, Yu YS (2012) Novel vancomycin-resistance transposon, plasmid replicon types, and virulence factors of vancomycin-resistant Enterococci in Zhejiang, China. Microb Drug Resist 18: 183–188. [DOI] [PubMed] [Google Scholar]
- 19. Willems R, Top J, van Schaik W, Leavis H, Bonten M, et al. (2012) Restricted gene flow among hospital subpopulations of Enterococcus faecium . MBio 3(4): e00151–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McBride SM, Fischetti VA, Leblanc DJ, Moellering RC Jr, Gilmore MS (2007) Genetic diversity among Enterococcus faecalis . PLoS One 2(7): e582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Manson JM, Hancock LE, Gilmore MS (2010) Mechanism of chromosomal transfer of Enterococcus faecalis pathogenicity island, capsule, antimicrobial resistance, and other traits. Proc Natl Acad Sci U S A 107(27): 12269–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leavis HL, Bonten MJ, Willems RJ (2006) Identification of high-risk enterococcal clonal complexes: global dispersion and antibiotic resistance. Curr Opin Microbiol 9: 454-460. Review. [DOI] [PubMed]
- 23. Wyllie D, Paul J, Crook D (2011) Waves of trouble: MRSA strain dynamics and assessment of the impact of infection control. J Antimicrob Chemother 66: 2685–2688. [DOI] [PubMed] [Google Scholar]
- 24.Chambers HF, Deleo FR (2009) Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat Rev Microbiol 7(9):629-41. Review. [DOI] [PMC free article] [PubMed]
- 25. Freitas AR, Novais C, Ruiz-Garbajosa P, Coque TM, Peixe L (2009) Dispersion of multidrug-resistant Enterococcus faecium isolates belonging to major clonal complexes in different Portuguese settings. Appl Environ Microbiol 75: 4904–4908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Freitas AR, Novais C, Ruiz-Garbajosa P, Coque TM, Peixe L (2009) Clonal expansion within clonal complex 2 and spread of vancomycin-resistant plasmids among different genetic lineages of Enterococcus faecalis from Portugal. J Antimicrob Chemother 63: 1104–1111. [DOI] [PubMed] [Google Scholar]
- 27. Novais C, Freitas AR, Sousa JC, Baquero F, Coque TM, et al. (2008) Diversity of Tn1546 and its role in the dissemination of vancomycin-resistant enterococci in Portugal. Antimicrob Agents Chemother 52: 1001–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Willems RJ, Hanage WP, Bessen DE, Feil EJ (2011) Population biology of Gram-positive pathogens: high-risk clones for dissemination of antibiotic resistance. FEMS Microbiol Rev 35: 872–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mato R, Almeida F, Pires R, Rodrigues P, Ferreira T, et al. (2009) Assessment of high-level gentamicin and glycopeptide-resistant Enterococcus faecalis and E. faecium clonal structure in a Portuguese hospital over a 3-year period. Eur J Clin Microbiol Infect Dis 28: 855–859. [DOI] [PubMed] [Google Scholar]
- 30. Araújo C, Torres C, Gonçalves A, Carneiro C, López M, et al. (2011) Genetic detection and multilocus sequence typing of vanA-containing Enterococcus strains from mullets fish (Liza ramada). Microb Drug Resist 17: 357–361. [DOI] [PubMed] [Google Scholar]
- 31. Galloway-Peña JR, Nallapareddy SR, Arias CA, Eliopoulos GM, Murray BE (2009) Analysis of clonality and antibiotic resistance among early clinical isolates of Enterococcus faecium in the United States. J Infect Dis 200: 1566–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Willems RJ, van Schaik W (2009) Transition of Enterococcus faecium from commensal organism to nosocomial pathogen. Future Microbiol 4: 1125–1135. [DOI] [PubMed] [Google Scholar]
- 33. Weaver KE, Kwong SM, Firth N, Francia MV (2009) The RepA_N replicons of Gram-positive bacteria: a family of broadly distributed but narrow host range plasmids. Plasmid 61: 94–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schwarz FV, Perreten V, Teuber M (2001) Sequence of the 50-kb conjugative multiresistance plasmid pRE25 from Enterococcus faecalisRE25. Plasmid 46: 170–187. [DOI] [PubMed] [Google Scholar]
- 35. Ruiz-Barba JL, Floriano B, Maldonado-Barragán A, Jiménez-Díaz R (2007) Molecular analysis of the 21-kb bacteriocin-encoding plasmid pEF1 from Enterococcus faecium 6T1a. . Plasmid. 57: 175–181. [DOI] [PubMed] [Google Scholar]
- 36. Sletvold H, Johnsen PJ, Simonsen GS, Aasnaes B, Sundsfjord A, et al. (2007) Comparative DNA analysis of two vanA plasmids from Enterococcus faecium strains isolated from poultry and a poultry farmer in Norway. Antimicrob Agents Chemother 51: 736–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sletvold H, Johnsen PJ, Hamre I, Simonsen GS, Sundsfjord A, et al. (2008) Complete sequence of Enterococcus faecium pVEF3 and the detection of an omega-epsilon-zeta toxin-antitoxin module and an ABC transporter. Plasmid 60: 75–85. [DOI] [PubMed] [Google Scholar]
- 38. Grady R, Hayes F (2003) Axe-Txe, a broad-spectrum proteic toxin- antitoxin system specified by a multidrug-resistant, clinical isolate of Enterococcus faecium . Mol Microbiol 47: 1419–1432. [DOI] [PubMed] [Google Scholar]
- 39. Halvorsen EM, Williams JJ, Bhimani AJ, Billings EA, Hergenrother PJ (2011) Txe, an endoribonuclease of the enterococcal Axe-Txe toxin-antitoxin system, cleaves mRNA and inhibits protein synthesis. Microbiology 157: 387–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Coque TM, Freitas AR, Novais C, Peixe L, Baquero F (2012) Mobile Genetic Elements and Lateral Genetic Transfer in Enterococci. In: Enterococcus and Safety Series: Advances in Food Safety and Food Microbiology. Semedo-Lemsaddek T, Barreto-Crespo MT, Tenreiro R (eds). Nova Publishers. ISBN: 978-1-61470-569-7.
- 41. Sørum M, Johnsen PJ, Aasnes B, Rosvoll T, Kruse H, et al. (2006) Prevalence, persistence, and molecular characterization of glycopeptide-resistant enterococci in Norwegian poultry and poultry farmers 3 to 8 years after the ban on avoparcin. Appl Environ Microbiol 72: 516–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schouten MA, Willems RJ, Kraak WA, Top J, Hoogkamp-Korstanje JA, et al. (2001) Molecular analysis of Tn1546-like elements in vancomycin-resistant enterococci isolated from patients in Europe shows geographic transposon type clustering. . Antimicrob Agents Chemother. 45: 986–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Garcia-Migura L, Hasman H, Jensen LB (2009) Presence of pRI1: a small cryptic mobilizable plasmid isolated from Enterococcus faecium of human and animal origin. Curr Microbiol 58: 95–100. [DOI] [PubMed] [Google Scholar]
- 44. Zheng B, Tomita H, Xiao YH, Wang S, Li Y, et al. (2007) Molecular characterization of vancomycin-resistant Enterococcus faecium isolates from mainland China. J Clin Microbiol 45: 2813–2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. McCormick AW, Whitney CG, Farley MM, Lynfield R, Harrison LH, et al. (2003) Geographic diversity and temporal trends of antimicrobial resistance in Streptococcus pneumoniae in the United States. Nat Med 9: 424–430. [DOI] [PubMed] [Google Scholar]
- 46. Johnsen PJ, Townsend JP, Bøhn T, Simonsen GS, Sundsfjord A, et al. (2009) Factors affecting the reversal of antimicrobial-drug resistance. . Lancet Infect Dis. 9: 357–364. [DOI] [PubMed] [Google Scholar]
- 47.Price LB, Stegger M, Hasman H, Aziz M, Larsen J, et al. (2012) Staphylococcus aureus CC398: Host Adaptation and Emergence of Methicillin Resistance in Livestock. MBio 3 : pii = e00305-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Robinson DA, Kearns AM, Holmes A, Morrison D, Grundmann H, et al. (2005) Re-emergence of early pandemic Staphylococcus aureus as a community-acquired meticillin-resistant clone. Lancet 365: 1256–1258. [DOI] [PubMed] [Google Scholar]
- 49. de Regt MJ, van Schaik W, van Luit-Asbroek M, Dekker HA, van Duijkeren E, et al. (2012) Hospital and community ampicillin-resistant Enterococcus faecium are evolutionarily closely linked but have diversified through niche adaptation. PLoS One 7: e30319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Li M, Du X, Villaruz AE, Diep BA, Wang D, et al. (2012) MRSA epidemic linked to a quickly spreading colonization and virulence determinant. Nat Med 18: 816–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Freitas AR, Tedim AP, Novais C, Ruiz-Garbajosa P, Werner G, et al. (2010) Global spread of the hyl (Efm) colonization-virulence gene in megaplasmids of the Enterococcus faecium polyclonal subcluster. Antimicrob Agents Chemother 54: 2660–2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Freeman LC (1977) A set of measures of centrality based on betweenness. Sociometry 40: 35–41. [Google Scholar]
- 53. Tamminen M, Virta M, Fani R, Fondi M (2012) Large-scale analysis of plasmid relationships through gene-sharing networks. Mol Biol Evol 29: 1225–1240. [DOI] [PubMed] [Google Scholar]
- 54. Willems RJ, Top T, van den Braak N, Van Belkum A, Mevius DJ, et al. (1999) Molecular diversity and evolutionary relationships of Tn1546-like elements in enterococci from humans and animals. Antimicrob Agents Chemother 43: 483–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Paulsen IT, Banerjei L, Myers GS, Nelson KE, Seshadri R, et al. (2003) Role of mobile DNA in the evolution of vancomycin-resistant Enterococcus faecalis . Science. 299: 2071–2074. [DOI] [PubMed] [Google Scholar]
- 56. Garcia-Migura L, Hasman H, Svendsen C, Jensen LB (2008) Relevance of hot spots in the evolution and transmission of Tn1546 in glycopeptide-resistant Enterococcus faecium (GREF) from broiler origin. J Antimicrob Chemother 62: 681–687. [DOI] [PubMed] [Google Scholar]
- 57. Via S (2009) Natural selection in action during speciation. Proc Natl Acad Sci U S A 106: 9939–9946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Levin SA, Paine RT (1974) Disturbance, patch formation, and community structure. Proc Natl Acad Sci U S A 71: 2744–2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Zhang Q, Lambert G, Liao D, Kim H, Robin K, et al. (2011) Acceleration of emergence of bacterial antibiotic resistance in connected environments. Science 333: 1764–1767. [DOI] [PubMed] [Google Scholar]
- 60. Aguilée R, Claessen D, Lambert A (2009) Allele fixation in a dynamic metapopulation: founder effects vs refuge effects. Theor Pop Biol 76: 105–117. [DOI] [PubMed] [Google Scholar]
- 61.Baquero F, Tedim AP, Coque TM (2013) Antibiotic resistance shaping multilevel population biology of bacteria. Frontiers in Antimicrobials, Resistance and Chemotherapy. In press. ISSN:664-302. [DOI] [PMC free article] [PubMed]
- 62. Novais C, Coque TM, Ferreira H, Sousa JC, Peixe L (2005) Environmental contamination with vancomycin-resistant enterococci from hospitalsewage in Portugal. Appl Environ Microbiol 71: 3364–3368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Novais C, Sousa JC, Coque TM, Peixe LV (2005) Molecular characterization of glycopeptide-resistant Enterococcus faecium isolates from Portuguese hospitals. Antimicrob Agents Chemother 49: 3073–3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, et al. (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33: 2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Morrison D, Woodford N, Barrett SP, Sisson P, Cookson BD (1999) DNA banding pattern polymorphism in vancomycin-resistant Enterococcus faecium and criteria for defining strains. J Clin Microbiol 37: 1084–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Nallapareddy SR, Weinstock GM, Murray BE (2003) Clinical isolates of Enterococcus faecium exhibit strain-specific collagen binding mediated by Acm, a new member of the MSCRAMM family. Mol Microbiol 47: 1733–1747. [DOI] [PubMed] [Google Scholar]
- 67. Vankerckhoven V, van Autgaerden T, Vael C, Lammens C, Chapelle S, et al. (2004) Development of a multiplex PCR for the detection of asa1, gelE, cylA, esp and hyl genes in enterococci and survey for virulence determinants among European hospital isolates of Enterococcus faecium . J Clin Microbiol 42: 4473–4479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Woodford N, Adebiyi AMA, Palepou MFI, Cookson BD (1998) Diversity of VanA glycopeptide resistance elements in enterococci from humans and nonhuman sources. Antimicrob Agents Chemother 42: 502–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Barton BM, Harding GP, Zuccarelli AJ (1995) A general method for detecting and sizing large plasmids. Anal Biochem 226: 235–240. [DOI] [PubMed] [Google Scholar]
- 70. Kado CI, Liu ST (1981) Rapid procedure for detection and isolation of large and small plasmids. J Bacteriol 145: 1365–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Garcillan-Barcia MP, Francia MV, de la Cruz F (2009) The diversity of conjugative relaxases and its application in plasmid classification. FEMS Microbiol Rev 33: 657–687. [DOI] [PubMed] [Google Scholar]
- 72. Jensen LB, Garcia-Migura L, Valenzuela AJ, Løhr M, Hasman H, et al. (2010) A classification system for plasmids from enterococci and other Gram-positive bacteria. J Microbiol Methods 80: 25–43. [DOI] [PubMed] [Google Scholar]
- 73. Moritz EM, Hergenrother PJ (2007) Toxin-antitoxin systems are ubiquitous and plasmid-encoded in vancomycin-resistant enterococci. Proc Natl Acad Sci U S A 104: 311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Handwerger S, Skoble J (1995) Identification of chromosomal mobile element conferring high-level vancomycin resistance in Enterococcus faecium . Antimicrob Agents Chemother 39: 2446–2453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sambrook J, Frisch E, Maniatis T (1989) Molecular cloning: a laboratory manual. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY.
- 76.Kaufmann ME (1998) Pulsed-Field Gel Electrophoresis. In: Woodford N and Johnson AP, editors. Molecular Bacteriology: protocols and clinical applications. Humana Press: Inc Totowa NJ. pp. 17-31.
- 77. Arthur M, Molinas C, Depardieu F, Courvalin P (1993) Characterization of Tn1546, a Tn3-related transposon conferring glycopeptide resistance by synthesis of depsipeptide peptidoglycan precursors in Enterococcus faecium BM4147. J Bacteriol 175: 117–127. [DOI] [PMC free article] [PubMed] [Google Scholar]