Abstract
Systemic antibiotics in conjunction with scaling and root planing (SRP), can offer an additional benefit over SRP alone in the treatment of periodontitis, in terms of clinical attachment loss (CAL) and pocket depth change, and reduced risk of additional CAL loss. However, antibiotics are not innocuous drugs. Their use should be justified on the basis of a clearly established need and should not be substituted for adequate local treatment. The aim of this review is to discuss the rationale, proper selection, dosage and duration for antibiotic therapy so as to optimize the usefulness of drug therapy.
Keywords: Periodontics, periodontitis, scaling and root planing, systemic antibiotic therapy
INTRODUCTION
During the past two decades, dentists and microbiologists have embraced periodontal antibiotic therapy as a powerful adjunct to conventional mechanical debridement for therapeutic management of the periodontal diseases,[1,2] as the evidence for bacterial specificity in periodontitis has accumulated and strengthened. Antibiotics, are defined as naturally occurring or synthetic organic substances that, in low concentrations, inhibit or kill selective microorganisms.[1]
The concept of antibiotic periodontal therapy centers upon the pathogenic microbiota, the patient, and the drug.[3] There are numerous antibiotics that could be employed to treat periodontal infections, but it is often unclear which antibiotic would provide the greatest benefit to a patient with a specific periodontal infection, with minimal adverse effects.
The discussion below concerns with the rationale, proper selection, dosage and duration for antibiotic therapy so as to optimize the usefulness of drug therapy.
RATIONALE OF ANTIBIOTIC THERAPY
Mechanical and surgical treatment combined with proper oral hygiene measures can arrest or prevent further periodontal attachment loss in most individuals by reducing total supra-subgingival bacterial mass.[4] However, despite diligent dental therapy, some individuals continue to experience periodontal breakdown, may be due to the ability of major periodontal pathogens like Porphyromonasgingivalis, Aggregatibacteractinomycetemcomitans, Fusobacterium-nucleatum, Treponemadenticola, bacteroids, to invade periodontal tissues or to reside in furcations or other tooth structures outside the reach of periodontal instruments, or due to poor host defense mechanisms.[4] In addition, the putative periodontal pathogens (“red complex”) tend to reside in the section of the biofilm attached to the epithelial surface of the periodontal pocket and the patient cannot reach this site during the oral hygiene efforts.[5]
The prime candidates for systemic antimicrobial therapy are those patients exhibiting attachment loss after seemingly adequate conventional therapy, or patients with aggressive forms of periodontitis or associated with predisposing medical conditions or refractory periodontitis.[6] Patients with acute or severe periodontal infections (periodontal abscess, acute necrotizing gingivitis/periodontitis) may also benefit from antibiotic therapy.[3]
Systemic periodontal antibiotic therapy aims to reinforce mechanical periodontal treatment and to support the host defense system in overcoming the infection by killing subgingival pathogens that remain after conventional mechanical periodontal therapy.[4] The susceptibility of bacteria to antibiotics may be the key to the efficacy of systemic antibiotics in the treatment of periodontal diseases.Few chemotherapeutic agents can also reduce collagen and bone destruction through their ability to inhibit the enzyme collagenase. Patients with gingivitis or stable adult periodontitis usually respond well to mechanical periodontal therapy and derive little or no additional benefit from antibiotic therapy.
GUIDELINES FOR USE OF ANTIBIOTICS IN PERIODONTAL DISEASE
The clinical diagnosis and situation dictate the need for possible antibiotic therapy as an adjunct in controlling active periodontal disease as the patient's diagnosis can change overtime.[5]
Continuing disease activity is an indication for periodontal intervention and possible microbial analysis through plaque sampling. Also, cases of refractory or aggressive periodontitis may indicate the need for antimicrobial therapy.
When used to treat periodontal disease, antibiotics are selected based on the patient's medical and dental status, current medications, and results of microbial analysis, if performed.
Microbial samples may be obtained from individual pockets with recent disease activity or from pooled subgingival sites. A pooled subgingival sample may provide a good representation of the range of periodontal pathogens to be targeted for antibiotic therapy.[3]
Plaque sampling can be performed at the initial examination, root planing, reevaluation, or supportive periodontal therapy appointment.
Antibiotics have also been shown to have value in reducing the need for periodontal surgery in patients with chronic periodontitis.
Systemic antibiotic therapy should be an adjunct to a comprehensive periodontal treatment plan. An antibiotic strength 500 times greater than the systemic therapeutic dose may be required to be effective against the bacteria arranged in the biofilms. Therefore, it is important to disrupt this biofilm physically so that the antibiotic agents can have access to the periodontal pathogens.[5]
Slots et al.[7] described a series of steps using anti-infective agents for enhancing regenerative healing. They recommend starting antibiotics 1-2 days before surgery and continuing for a total of atleast 8 days, however, the value of this regimen has not been well documented.
Haffajee et al.[8] concluded that data support similar effects for most antibiotics. Risks and benefits concerning antibiotics as adjuncts to periodontal therapy must be discussed with the patient before the antibiotics are used.
SELECTION OF ANTIBIOTIC
After having established the need for using an antibiotic in a patient, it is often difficult to decide which one to choose from the large number available. The factors governing the decision for selection of antibiotics are:[9]
Age of patient: It may affect pharmacokinetics of many antibiotics e.g. tetracyclines accumulate in the developing teeth and bone.
Renal and hepatic function: Cautious use and modification of the dose of an antibiotic becomes necessary when the organ of its disposal is defective.
Local factors: The conditions prevailing at the site of infection greatly affect the action of antibiotics like the presence of pus and secretions, necrotic material and foreign body, low pH.
Drug allergy: History of previous exposure to an antibiotic and any allergic reaction should be obtained.
Impaired host defense: In an individual with normal host defense, a bacteriostatic antibiotic may achieve cure, while intensive therapy with bactericidal drugs is imperative in those with impaired host defense.
Pregnancy: All antibiotics should be avoided in the pregnancy because of risk to the developing foetus.
Organism related considerations: Though the therapy is empirical most of the times, the likelihood of the most probable pathogen must be considered.
Drug factors: This includes the specific properties of antibiotics like spectrum of activity (narrow/broad), type of activity (bactericidal/bacteristatic), sensitivity of the organism (Minimal inhibitory concentration values), relative toxicity, pharmacokinetic profile, route of administration, evidence of clinical efficacy and cost of the drug.
The microbial composition of subgingival plaque varies considerably from patient to patient.
The description of the Gram stain reaction and the anaerobic requirement of the infectious periodontal microbiota provided the first guidelines for selection of antimicrobial therapy.
Delineation of the type of periodontal infection (exogenous/endogenous) may be important in selecting a proper strategy for antimicrobial therapy in periodontics.[4]
Two critical factors should be specifically considered in selecting a systemic antibiotic in periodontal therapy:[10] Gingival fluid concentration and Minimum inhibitory concentration (MIC).
The gingival fluid concentration (CGCF) provides information on the peak levels achieved by systemic delivery at the primary ecological niche for periodontal pathogens, the periodontal pocket.
The 90% minimum inhibitory concentration (MIC90) is an in vitro determination of the concentration that will inhibit growth of 90% of the bacterial strains of a species that are tested. Antimicrobial activity can be defined as a relationship between CGCF and MIC90
100 (CGCF/MIC90) = antimicrobial activity expressed as a percentage for each antibiotic and each organism.
Antibiotics that can achieve 90% inhibition of growth of an organism appear on the 100% line. The most effective antibiotics for treatment of a particular periodontal pathogen are those that equal or exceed the 100% value.
Periodontal diseases in which antibiotics can be used:
-
Chronic periodontitis: Antibiotic therapy is usually recommended for patients showing progressive periodontal breakdown even after conventional mechanical treatment, patients not responding to periodontal therapy (refractory periodontitis) and patients with recurrent disease.[1,4] Reviewing pertinent literature[2–5] use of following antibiotics has been suggested:
Tetracycline, Doxycycline, Metronidazole, Clindamycin, Amoxicillin + Clavulinic acid (Augmentin), Azithromycin, Metronidazole + Amoxicillin, Spiramycin.
-
Aggressive periodontitis: Localized aggressive periodontitis (LAP) mostly involving Aggregatibacteractinomycetemcomitan scan be controlled or eradicated by systemic metronidazole-amoxicillin combination therapy.[1] Other antibiotics recommended for both localized and generalized aggressive periodontitis are:[2,3,5]
Tetracycline, Doxycycline, Minocycline, Metronidazole, Amoxicillin + Clavulinic acid (Augmentin), Metronidazole + Amoxicillin.
Necrotizing periodontal diseases: Patients with moderate or severe NUG or necrotizing ulcerative periodontitis (NUP), local lymphadenopathy and systemic involvement need antibiotic therapy. Antibiotics recommended are amoxicillin, metronidazole and combination of amoxicillin+metronidazole.[1,3,5]
Periodontal abscess: Antibiotic therapy is indicated for periodontal abscesses with systemic manifestations (fever, malaise, lymphadenopathy). Antibiotics for the treatment of abscesses should be prescribed in conjunction with surgical incision and drainage.[3]
Antibiotic regimens for adult patients with acute periodontal abscesses[3]
Amoxicillin: Loading dose of 1.0 g followed by a maintenance dose of 500 mg/t.i.d. for 3 days, followed by a patient evaluation to determine whether further antibiotic therapy or dosage adjustment is required.
With allergy to ß-lactam drugs: Azithromycin: Loading dose of 1.0 g on day 1, followed by 500 mg/q.d. for days 2 and 3; or Clindamycin: Loading dose of 600 mg on day 1, followed by 300 mg/q.i.d. for 3 days.
PRINCIPLES OF ANTIBIOTIC DOSING[11]
Employ high doses for a short duration: Antibiotic success depends on maintaining the blood and tissue concentrations above the minimal inhibitory concentration for the target organism. High concentrations are more critical with aminoglycosides, metronidazole and quinolones (concentration-dependent antibiotics), whereas prolonged exposure of the organism to the antimicrobial agent is more critical with the beta lactams (time-dependent antibiotics).
Use an oral antibiotic loading dose: Without a loading dose, it takes 6-12 hours to achieve maximum therapeutic blood and tissue levels via oral administration.
Achieve blood levels of the antibiotic at 2-8 times the minimal inhibitory concentration: Such blood levels are necessary to compensate for the tissue barriers that impede antibiotic penetration to the site of the infection.
Use frequent dosing intervals: This is important with the older beta-lactam antibiotics such as penicillin V and the first generation cephalosporins (cephalexin, cephradine) so as to maintain relatively constant blood levels.
Determine the duration of therapy by the remission of disease: The antibiotic is terminated when the patient host defenses have gained control of the infection and the infection is reasonably certain to resolve or has resolved. Systemically administered bacteriostatic antibiotics characteristically require longer periods of administration to be effective as compared with their bactericidal counterparts.
COMMONLY USED ANTIBIOTICS IN PERIODONTICS
Eight principle antibiotic groups have been extensively evaluated for treatment of the periodontal diseases; tetracycline, minocycline, doxycycline, erythromycin, clindamycin, ampicillin, amoxicillin and metronidazole.[10] A brief review of these drug groups is as follows:
Tetracycline
Pharmacology
Produced naturally from certain species of Streptomyces or derived semisynthetically.
Bacteriostatic drugs, effective against rapidly multiplying bacteria and gram positive bacteria than gram negative bacteria.
Concentration in the gingival crevice is 2-10 times that in serum.[5]
Possess unique non-antibacterial characteristics-collagenase inhibition,[12] inhibition of neutrophil chemotaxis, anti-inflammatory effects,[10] inhibition of microbial attachment[13] and root surface conditioning.[14]
Mode of action
Act by inhibition of protein synthesis by binding to 30 S ribosomes in the susceptible organism.[9]
Clinical use
Adjuncts in the treatment of localized aggressive periodontitis (LAP).
Arrest bone loss and suppress A. actinomycetemcomitans levels in conjunction with scaling and root planing.
Tetracycline, minocycline and doxycycline are semisynthetic members of the tetracycline group that have been used in periodontal therapy.
Tetracycline
Dosage regimen-250 mg four times daily, inexpensive, lesser compliance.
Minocycline
Effective against a broad spectrum of microorganisms.
Suppresses spirochetes and motile rods as effectively as scaling and root planing, with suppression evident up to 3 months after therapy.
Can be given twice daily, thus facilitating compliance.
Although associated with less phototoxicity and renal toxicity than tetracycline, may cause reversible vertigo.
Yields gingival fluid levels 5 times blood levels.[15]
Except for the effect of minocycline on actinomycetes, none of the tetracyclines substantially inhibit the growth of oral gram-positive organisms by systemic delivery.
Doxycycline
Same spectrum of activity as minocycline.
Compliance is favored since it has to be taken once daily, absorption from gastrointestinal tract is only slightly altered by calcium, metal ions, or antacids.[5]
The recommended dosage is 100 mg bid the first day, then 100 mg o.d. To reduce gastrointestinal upset, 50 mg can be taken bid.
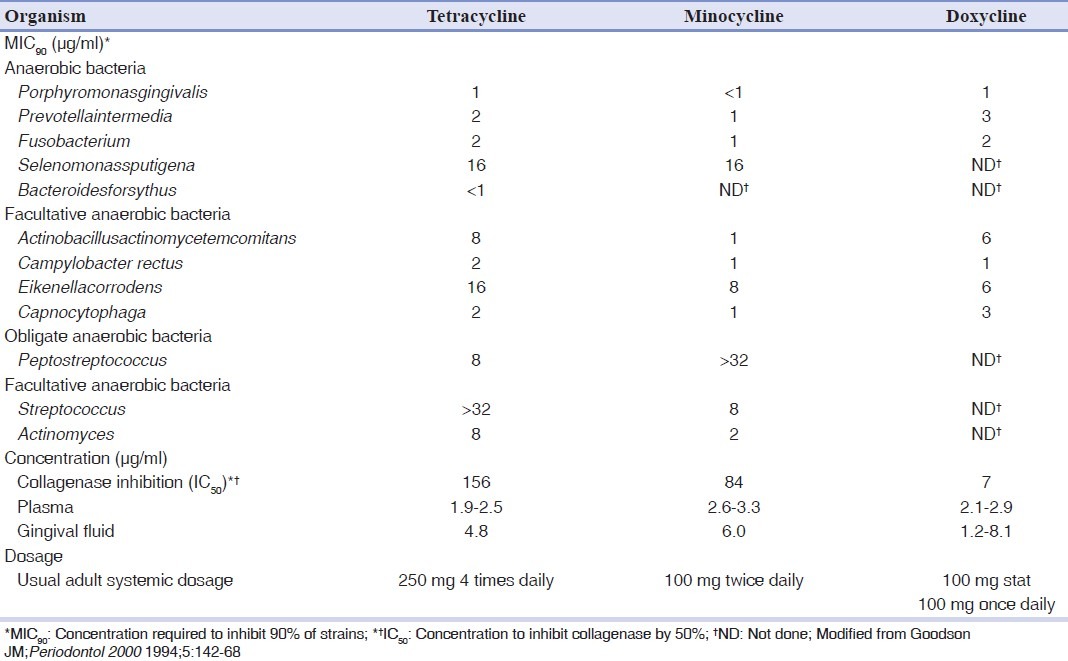
Note: Comparison of biological effects, peak concentrations following systemic administration and usual adult dosage of tetracyclines have been illustrated in Table 1.
Table 1.
Comparison of biological effects, peak concentrations following systemic administration and usual adult dosage of tetracyclines (all values in μg/ml)[10]
Metronidazole
Pharmacology
A synthetic nitroimidazole compound with bactericidal effects primarily exerted on obligate gram-positive and gram-negative anaerobes. Campylobacterrectus is the onlyfacultative anaerobe and probable periodontal pathogen that is susceptible to low concentrations of metronidazole.
Spectrum of activity-outstanding treatment for Fusobacterium and Selenomonasinfections, the best candidate for Peptostreptococcus infections, a reasonable candidate for P. gingivalis, Pintermediaand C. rectus infections, a poor choice for A. actinomycetemcomitansand E. corrodens infections, does not substantially suppress growth beneficial species.[10]
The concentrations measured in gingival fluid are generally slightly less than in plasma.
Mode of action
Metronidazole acts by inhibiting DNA synthesis.
Clinical use
For treating gingivitis, acute necrotizing ulcerative gingivitis, chronic periodontitis, and aggressive periodontitis.
As monotherapy, metronidazole is inferior, should be used in combination with root planing, surgery or with other antibiotics. The most commonly prescribed regimen is 250 mg tid for 7 days.
In a study by Haffajee et al.,[16] sites with initial pocket depth ≥6 mm showed significantly greater pocket depth reduction and greater attachment gain in subjects receiving metronidazole or azithromycin than in subjects who received doxycycline.
Penicillin
Pharmacology
Natural and semi synthetic derivatives of broth cultures of the penicilliummould.
Narrow spectrum and bactericidal in nature. Major activity in the gram positive spectrum. Only the extended spectrum penicillins, such as ampicillin and amoxicillin, possess substantial antibacterial antimicrobial activity for gram-negative species.[10]
Mode of action
Interfere with the synthesis of bacterial cell wall, inhibit the transpeptidases so that cross linking does not take place.
Clinical use
In the management of patients with aggressive periodontitis, in both localized and generalized forms. Recommended dosage is 500 mg tid for 8 days.
Exhibits high antimicrobial activity at levels that occur in GCF for all periodontal pathogens except E. corrodens, S. sputigena and Peptostreptococcus, inhibits the growth of the gram positive facultative anaerobes.[10]
Studies indicate that more than 60% of adult periodontitis patients sampled harboured periodontal plaque that exhibited β-lactamase activity. For this reason, administration of β-lactamase sensitive penicillins, including amoxicillin alone, is not generally recommended and, in some cases, may accelerate periodontal destruction.
Amoxicillin-Clavulanate (Augmentin) - The generally accepted strategy is to administer amoxicillin with an inhibitor of beta-lactamase such as clavulanic acid. Beta-lactamase-producing strains are generally sensitive to this preparation. Augmentin may be useful in the management of patients with refractory or localized aggressive periodontitis patients.
In guided tissue regeneration, systemic amoxicillin-clavulanic acid therapy has been used to suppress periodontal pathogens and increase the gain of clinical attachment.[3]
Cephalosporins
Pharmacology
Used for infections that might otherwise be treated withpenicillin.
Resistant to a number of β-lactamases normally active against penicillin.
Mode of action
Same mode of action as penicillins, i.e., inhibition of bacterial cell wall synthesis. However, they bind to different proteins than those which bind penicillins.[15]
Clinical use
Cephalexin is a cephalosporin available for administration in an oral dosage form.
Achieves high concentrations in GCF
Effectively inhibits growth of gram-negative obligate anaerobes, fails to inhibit the gram-negative facultative anaerobes.[10]
Newer cephalosporins with extended gram-negative effectiveness could be of value in treatment of periodontal disease conditions.
Clindamycin
Pharmacology
Effective against anaerobic bacteria, and in patients allergic to penicillin.
Mode of action
Inhibition of protein synthesis by binding to 50 S ribosome.
Clinical use
Clindamycin achieves higher levels of antimicrobial activity than other antibiotics.
Gordon et al.[17] observed a mean gain of clinical attachment of 1.5 mm and a decrease of disease activity in patients 24 months after adjunctive clindamycin therapy.
Walker et al.[18] showed that clindamycin assisted in stabilizing refractory patients. Dosage was 150 mg qid for 10 days.
Jorgensen and Slots[19] recommended a regime of 300 mg bid for 8 days.
Ciprofloxacin
Pharmacology
A fluorinated 4-quinolone antibiotic available for oral administration.
A potent inhibitor of gram negative bacteria (all facultative and some anaerobic putative periodontal pathogens), including Pseudomonas aeruginosa, with MIC90 values ranging from 0.2 to 2 μg/ml.[10]
Mode of action
Inhibition of bacterial DNA replication and transcription by inhibiting the enzyme DNA gyrase, an enzyme unique to prokaryotic cells.[9]
Clinical use
Facilitates the establishment of a microflora associated with periodontal health, minimal effects on streptococcus species, which are associated with periodontal health.
At present, ciprofloxacin is the only antibiotic in periodontal therapy to which all strains of A. actinomycetemcomitans are susceptible.
Also used in combination with Nitroimidazoles (metronidazole and tinidazole).
Macrolides
Pharmacology
Contain a poly-lactone ring to which one or more deoxy sugars are attached.
Can be bacteriostatic or bactericidal, depending on the concentration of the drug and the nature of micro organism.
The macrolide antibiotics used for periodontal treatment include erythromycin, spiramycin, and azithromycin.
Principle limitation of erythromycin is its poor tissue absorption. Preparations for systemic administration are available as pro-drugs (erythromycin estolate, erythromycin stearate or erythromycin ethylsuccinate) to facilitate absorption. The pro-drug has little antibacterial activity until hydrolyzed by serum esterases.[10]
Mode of action
Inhibit protein synthesis by binding to the 50 S ribosomal subunits of sensitive microorganisms and interfere with translation.
Erythromycin
Clinical use
An extremely safe drug that has often been recommended as an alternative to penicillin for allergic patients.
Gingival fluid levels suggest that only a small portion reaches the periodontal pocket by oral route.
Spiramycin
It is excreted in high concentrations in saliva.[5] The results of various clinical trials have revealed good efficacy of spiramycin in the treatment of periodontitis and meta-analysis of these studies revealed high levels of evidence supporting its efficacy.[2,4,8] It has been shown to reduce gingival crevicular fluid volume, pocket depth and subgingival spirochete levels.[1] Herrera et al.[6] in ameta analysis evaluating spiramycin, amoxicillin plus metronidazole, andmetronidazole showed a statistically significant additional effect of spiramycin in comparison to other antibiotics with regard to probing pocket depth reduction for sites with initial probing depth of more than 6 mm.
Clinical use
Effective against gram positive organisms, has minimal effect on increasing attachment levels.
Azithromycin
Clinical use
Effective against anaerobes and gram negative bacilli.
After an oral dosage of 500 mg o.d for 3 days, significant levels of azithromycin can be detected in most tissues for 7-10 days.
It has been proposed that azithromycin penetrates fibroblasts and phagocytes in concentrations 100-200 times greater than that of extracellular compartment. The azithromycin is actively transported to sites of inflammation by phagocytes, then directly released into the sites of inflammation as phagocytes rupture during phagocytosis.[5]
Therapeutic use requires a single dose of 250 mg/day for 5 days after initial loading dose of 500 mg.
Aminoglycosides
Inhibit protein synthesis by binding irreversible to a particular protein or proteins of the 30 S ribosomal subunit.
Are inactive under anaerobic conditions because intracellular transport is severely impaired in the absence of oxygen. Therefore, all anaerobic bacteria are markedly resistant even though they contain ribosomes that are sensitive to these antibiotics.[15]
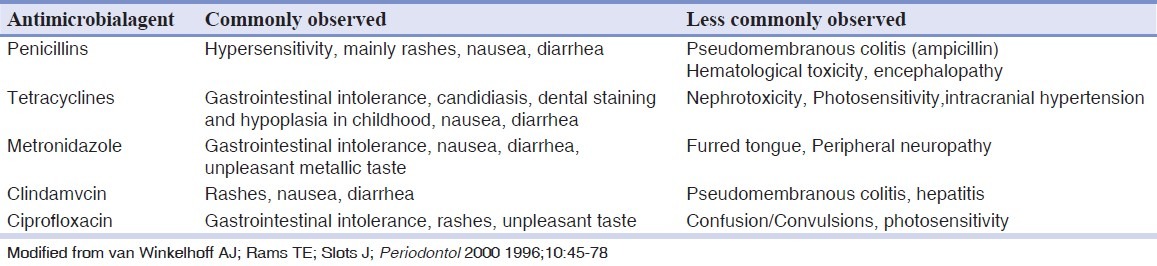
Note: Adverse effects of selected antibiotics used in the treatment of periodontal diseases have been given in Table 2.
Table 2.
Selected adverse effects of antibiotics used in the treatment of periodontal diseases[4]
There are five daunting problems that have slowed progress of antibiotic therapy are:[2]
Periodontal diseases are heterogeneous;
Clinical diagnoses are made on the basis of clinical signs, not molecular pathology;
The actual causal factor(s) have not been definitively identified;
No microbiological sampling.
There are many different antibiotic protocols but few well designed, randomized controlled trials that test the efficacy of these protocols.
Periodontal infections may be considered as mixed infections, in which a variety of aerobic, microaerophilic, and anaerobic bacteria, both gram negative and gram positive, sensitive to different drugs are involved. Therefore, it seems better to use more than one antibiotic to cover all the periodontal pathogens in some clinical situations.
Combination of antibiotics may help[4]
To broaden the antimicrobial range of the therapeutic regimen beyond that attained by any single antibiotic.
To prevent or forestall the emergence of bacterial resistance by using agents with overlapping antimicrobial spectra.
To lower the dose of individual antibiotics by exploiting possible synergy between two drugs against targeted organisms.
The disadvantages of combining antibiotics are:[4]
Increased adverse reactions
Antagonistic drug interactions with improperly selected antibiotics.
SEQUENTIAL SYSTEMIC ANTIBIOTICS
Antibiotics that are bacteriostatic (e.g., tetracycline) generally require rapidly dividing microorganisms to be effective. They do not function well if a bactericidal antibiotic (e.g., amoxicillin or metronidazole) is given concurrently. When both types of drug are required, they are best given serially, not in combination, to avoid unfavourable interaction yet derive the benefit of both.[5]
In one such study, six patients with recurrent progressive periodontitis were given the usual adult dosage of doxycycline for 4 days followed by amoxicillin with clavulanate for 5 days. Five similar patients were given doxycycline alone for 10 days. After 25 weeks, patients receiving the sequential combination had significantly greater pocket depth reduction than those receiving doxycycline alone.[2]
In another study, all patients with recurrent periodontitis received regular bimonthly scaling and sequential dose of doxycycline and metronidazole. In the combined antibiotic group, 9% were observed to have recurrent periodontitis, whereas 42% of the placebo group showed signs of recurrent disease. Although these differences appear statistically significant, by 7 months after metronidazole, no difference in microbiota between groups could be detected.[2]
COMBINATION THERAPY
A combination of metronidazole and amoxicillin (MA) has shown to be an effective antibiotic regime to combat Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis-associated periodontal infections.[20]
One important clinical finding in a study by Winkel et al.,[21] was the observation that patients with subgingival P. gingivalis at baseline who were treated with metronidazole+amoxicillin showed approximately half the number of >5 mm pockets after therapy compared with P. gingivalis positive patients treated with placebo. Guerreo et al.[22] used a comparable treatment protocol in patients with aggressive periodontitis and showed significantly better improvement of all periodontal parameters in the antibiotic treated patients compared to placebo treated subjects 6 months post-treatment.
These studies have revealed that, in chronic as well as in aggressive periodontitis, the antibiotics result in better resolution of the periodontal inflammation, better probing depths, and attachment loss reduction.
Metronidazole and clindamycin appear to be more efficient in eradicating the anaerobic periodontopathic bacteria than doxycycline or mechanical therapy alone.[23]
Metronidazole ciprofloxacin combination is effective against A. actinomycetemcomitans. Metronidazole targets obligate anaerobes, and ciprofloxacin targets facultative anaerobes. This is a powerful combination against mixed infections. Studies of this drug combination in the treatment of refractory periodontitis have documented marked clinical improvement.[24]
MEDICAL CONDITIONS THAT NEED PRE-OPERATIVE ANTIBIOTIC USE
Patients having uncontrolled diabetes, organ transplantation, bone marrow transplantation, prosthetic joint replacement, leukemia, neutropenia, thrombocytopenia are at greater risk of developing infection after dental procedures due to immunosuppression or decreased number of immune cells.[25,26] Chronic renal disease patients also need antibiotic prophylaxis to prevent endarteritis of the arteriovenous fistula or shunt.[25] To prevent infective endocarditis in patients having previous history of infective endocarditis, prosthetic cardiac valves, major congenital heart disease (tetralogy of Fallot, transposition of great arteries, surgically constructed systemic pulmonary shunts or conduits), acquired valvular function (e.g., rheumatic heart disease), hypertrophic cardiomyopathy, mitral valve prolapsed with valvular regurgitation, thickened leaflets or both, antibiotic prophylaxis is recommended.[25]
The periodontal procedures considered as high risk procedures in these patients are probing, scaling, root planing, subgingival placement of antibiotic fibers or strip, intraligamentary local anesthetic injections, prophylactic cleaning of teeth or implants with anticipated bleeding, periodontal surgery, dental implant placement.[27] Amoxicillin is used most commonly used for antibiotic prophylaxis. The recommended dosage is 2 g in adults and 50 mg/kg in children, orally one hour before procedure. For the patients who cannot use oral medication, ampicillin is given intramuscularly or intravenously at dose of 2.0 gm in adults and 50 mg/kg in children within 30 minutes before procedure. In patients allergic to penicillin, the antibiotics preferred are clindamycin (adults, 600 mg; children, 20 mg/kg orally one hour before procedure), Cephalexin or cefadroxil (adults, 2.0 g; children, 50 mg/kg orally one hour before procedure), Azithromycin or clarithromycin (adults, 500 mg; children, 15 mg/kg orally one hour before procedure). The patients allergic to penicillin and unable to take oral medications are given clindamycin (adults, 600 mg; children, 15 mg/kg IV one hour before procedure) or cefazolin (adults, 1.0 g; children, 25 mg/kg IM or IV within 30 minutes before procedure).[27]
CLINICAL REASONS FOR ANTIBIOTIC FAILURE
The clinical reasons for antibiotic failure are as follows:[11]
Inappropriate choice of antibiotic
Emergence of antibiotic-resistant microorganisms
Too low a blood concentration of the antibiotic
Slow growth rate of microorganisms
Impaired host defenses
Patient noncompliance
Antibiotic antagonism
Inability of the antibiotic to penetrate to the site of the infection
Limited vascularity or decreased blood flow
Unfavorable local factors (decreased tissue pH or oxygen tension)
Failure to eradicate thesource of the infection (lack of incision and drainage)
SUMMARY
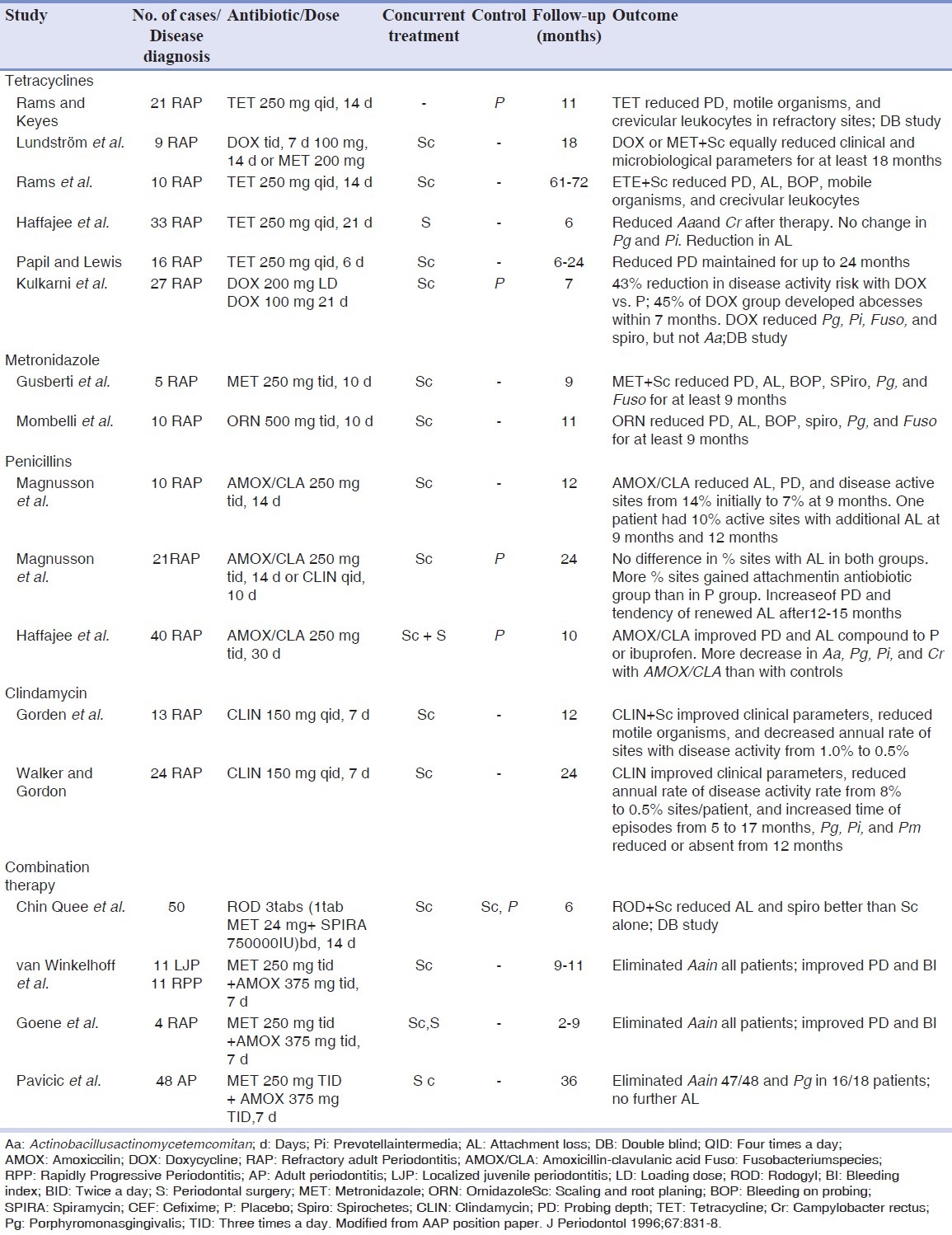
It has been established that systemic antibiotics can significantly enhance the effects of mechanical periodontal therapy in conjunction with measures that improve the oral hygiene. Clinical studies of systemic antibiotic therapy in adult periodontitis, refractory periodontitis, aggressive periodontitis patients have been given in Table 3. As suggested by Herrera et al.[6] and Haffajee et al.[8] the mean “gain” in attachment of 0.3-0.4 mm may appear small, but it was based on change throughout the mouth including sites with shallow probing depths whose post-therapy improvement would be expected to be modest. As a bench mark, periodontitis subjects monitored after treatment and on supportive periodontal therapy for about 12 years only experienced an average annual full mouth mean attachment loss of 0.042 mm (normal susceptibility subjects) to 0.067 mm (high susceptibility subjects).[28] Thus, attachment level “gain” of 0.3 mm would be equivalent to reversing 4-7 years of disease progression in a treated and maintained population.[8]
Table 3.
Clinical studies of systemic antibiotic therapies in adult periodontitis patients with recent disease activity prior to antibiotic therapy[29]
All the antibiotics used in periodontal therapy, inhibit growth of the major periodontal pathogens P. gingivalis, C. rectus and Capnocytophaga. In direct contrast, none are particularly effective in the inhibition of E. corrodens (minocycline and doxycycline being best). Minocycline appears to be the most effective antibiotic, which achieves levels that should be completely inhibitory (antibiotic activity = 600%) to most of the periodontal pathogens but may inhibit the growth of beneficial species as well.[10] Amoxicillin appears almost as effective as minocycline. Tetracycline, the most commonly used antibiotic, but appears to be a relatively poor choice for A. actinomycetemcomitans infections, for which it has been used most commonly. Erythromycin appears to be a poor choice for any pathogenic oral infection. Metronidazole is uniquely effective in treating Selenomonassputigena and Peptostreptococcus infections and equal to minocycline in treating Fusobacterium infections.
CONCLUSION
Periodontal infections can involve a variety of pathogens with different antimicrobial sensitivities and resistance patterns. In periodontal infections, tissue barriers and biofilms should be removed, by mechanical debridement prior to or with antibiotics. The periodontal disease status and the antimicrobial regimen must be determined carefully to succeed with antimicrobial periodontal therapy. Unless antimicrobial agents against periodontal disease are used intelligently, we may soon face a new breed of oral microorganisms with heightened defenses that will ensure the survival of the species, allows for greater pathogenicity and transfer genetic material coding for increased virulence and antibiotic resistance to other oral and nonoral microorganisms.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Slots J, Ting M. Systemic antibiotics in the treatment of periodontal disease. Periodontol 2000. 2002;28:106–76. doi: 10.1034/j.1600-0757.2002.280106.x. [DOI] [PubMed] [Google Scholar]
- 2.Ellen RP, Mcculloch CA. Evidence versus empiricism: Rational use of systemic antimicrobial agents for treatment of periodontitis. Periodontol 2000. 1996;10:29–44. doi: 10.1111/j.1600-0757.1996.tb00067.x. [DOI] [PubMed] [Google Scholar]
- 3.Slots J. Research, Science and Therapy Committee. Systemic Antibiotics in Periodontics. J Periodontol. 2004;75:1553–65. doi: 10.1902/jop.2004.75.11.1553. [DOI] [PubMed] [Google Scholar]
- 4.van Winkelhoff AJ, Rams TE, Slots J. Systemic antibiotic therapy in periodontics. Periodontol 2000. 1996;10:45–78. doi: 10.1111/j.1600-0757.1996.tb00068.x. [DOI] [PubMed] [Google Scholar]
- 5.Jolkovsky DL, Ciancio S. Chemotherapeutic agents. In: Carranza FA, Newman MG, Takei HH, Klokkevold PR, editors. Clinical periodontology. 10th ed. Philadelphia: WB Saunders; 2006. pp. 798–812. [Google Scholar]
- 6.Herrera D, Sanz M, Jepsen S, Needleman I, Roldan S. A systematic review on the effect of systemic antimicrobials as an adjunct to scaling and root planing in periodontitis patients. J Clin Periodontol. 2002;29:136–59. doi: 10.1034/j.1600-051x.29.s3.8.x. [DOI] [PubMed] [Google Scholar]
- 7.Slots J, MacDonald ES, Nowzari H. Infectious aspects of periodontal regeneration. Periodontol 2000. 1999;19:164–72. doi: 10.1111/j.1600-0757.1999.tb00154.x. [DOI] [PubMed] [Google Scholar]
- 8.Haffajee AD, Socransky SS, Gunsolley JC. Systemic anti-infective periodontal therapy.A systematic review. Ann Periodontol. 2003;8:115–81. doi: 10.1902/annals.2003.8.1.115. [DOI] [PubMed] [Google Scholar]
- 9.Tripathi KD. Antimicrobial drugs: General considerations. In: Tripathi KD, editor. Essentials of medical pharmacology. 5th ed. New Delhi: Jaypee Publishers; 2003. pp. 627–40. [Google Scholar]
- 10.Goodson JM. Antimicrobial strategies for treatment of periodontal diseases. Periodontol 2000. 1994;5:142–68. doi: 10.1111/j.1600-0757.1994.tb00022.x. [DOI] [PubMed] [Google Scholar]
- 11.Pallasch TJ. Pharmacokinetic principles of antimicrobial therapy. Periodontol 2000. 1996;10:5–11. doi: 10.1111/j.1600-0757.1996.tb00065.x. [DOI] [PubMed] [Google Scholar]
- 12.Golub LM, Ramamurthy N, McNamara TF, Gomes B, Wolff M, Casino A, et al. Tetracyclines inhibit tissue collagenase activity. Anew mechanism in the treatment of periodontal disease. J Periodontal Res. 1984;19:651–5. doi: 10.1111/j.1600-0765.1984.tb01334.x. [DOI] [PubMed] [Google Scholar]
- 13.Lantz MS, Ray T, Krishanasami S, Perrson DE. Subinhibitory concentrations of tetracycline alter fibrinogen binding by Bucferoidesinterrnedius. Antimicrob Agents Chemother. 1987;31:1915–8. doi: 10.1128/aac.31.12.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wikesjö UM, Baker PJ, Christersson LA, Genco RJ, Lyall RM, Hic S, et al. A biochemical approach to periodontal regeneration: Tetracycline treatment conditions dentin surfaces. J Periodont Res. 1986;21:322–9. doi: 10.1111/j.1600-0765.1986.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 15.Walker CB. Selected antimicrobial agents: Mechanisms of action, side effects and drug interactions. Periodontol 2000. 1996;10:12–28. doi: 10.1111/j.1600-0757.1996.tb00066.x. [DOI] [PubMed] [Google Scholar]
- 16.Haffajee AD, Torresyap G, Socransky SS. Clinical changes following four different periodontal therapies for the treatment of chronic periodontitis: 1 year results. J Clin Periodontol. 2007;34:243–53. doi: 10.1111/j.1600-051X.2006.01040.x. [DOI] [PubMed] [Google Scholar]
- 17.Gordon J, Walker C, Lamster I, West T, Socransky S, Seiger M, et al. Efficacy of clindamycin hydrochloride in refractory periodontitis - 12 month results. J Periodontol. 1985;56:75–80. doi: 10.1902/jop.1985.56.11s.75. [DOI] [PubMed] [Google Scholar]
- 18.Walker CB, Gordon JM, Magnusson I, Clark WB. A role for antibiotics in the treatment of refractory periodontitis. J Periodontol. 1993;64:772–81. doi: 10.1902/jop.1993.64.8s.772. [DOI] [PubMed] [Google Scholar]
- 19.Jorgenson MG, Slots J. Responsible use of antimicrobials in periodontics. J Calif Dent Assoc. 2000;28:185–93. [PubMed] [Google Scholar]
- 20.van Winkelhoff AJ, Winkel EG. Antibiotics in periodontics: Right or wrong? J Periodontol. 2009;80:1555–8. doi: 10.1902/jop.2009.090276. [DOI] [PubMed] [Google Scholar]
- 21.Winkel EG, van Winkelhoff AJ, Timmerman MF, Van der Velden U, van der Weijden GA. Amoxicillin plus metronidazole in the treatment of adult periodontitis patients.A double-blind placebo-controlled study. J Clin Periodontol. 2001;28:296–305. doi: 10.1034/j.1600-051x.2001.028004296.x. [DOI] [PubMed] [Google Scholar]
- 22.Guerrero A, Griffiths GS, Nibali L, Suvan J, Moles DR, Laurell L, et al. Adjunctive benefits of systemic amoxicillin and metronidazole in non-surgical treatment of generalized aggressive periodontitis: A randomized placebo controlled clinical trial. J Clin Periodontol. 2005;32:1096–107. doi: 10.1111/j.1600-051X.2005.00814.x. [DOI] [PubMed] [Google Scholar]
- 23.Sigusch B, Beier M, Klinger G, Pfister W, Glockmann E. A 2-step non-surgical procedure and systemic antibiotics in the treatment of rapidly progressive periodontitis. J Periodontol. 2001;72:275–83. doi: 10.1902/jop.2001.72.3.275. [DOI] [PubMed] [Google Scholar]
- 24.Rams TE, Feik D, Slots J. Ciprofloxacin/metronidazole treatment of recurrent adult periodontitis. J Dent Res. 1992;71:319. [Google Scholar]
- 25.Mealey BL, Klokkevold PR, Otomo-Corgel J. Periodontal treatment of medically compromised patients. In: Carranza FA, Newman MG, Takei HH, Klokkevold PR, editors. Clinical periodontology. 10th ed. Philadelphia: WB Saunders; 2006. pp. 650–64. [Google Scholar]
- 26.Little JW, Falace DA, Miller CS, Rhodus NL. 7th ed. St. Louis: Mosby Elsevier; 2008. Dental management of the medically compromised patient; pp. 1–40. [Google Scholar]
- 27.Tong DC, Rothwell BR. Antibiotic prophylaxis in dentistry: A review and practice recommendations. J Am Dent Assoc. 2000;131:366–74. doi: 10.14219/jada.archive.2000.0181. [DOI] [PubMed] [Google Scholar]
- 28.Rosling B, Serino G, Hellstrom MK, Socransky SS, Lindhe J. Longitudinal periodontal tissue alterations during supportive therapy.Findings from subjects with normal and high susceptibility to periodontal disease. J Clin Periodontol. 2001;28:241–9. doi: 10.1034/j.1600-051x.2001.028003241.x. [DOI] [PubMed] [Google Scholar]
- 29.AAP position paper. J Periodontol. 1996;67:831–8. [Google Scholar]


