Abstract
Background:
Composite resin restorations may have a short lifespan due to the degradation of resin–dentin interface. Ethanol wet bonding technique may extend the longevity of resin–dentin bond. The purpose of this one year randomized clinical trial was to compare clinical performance of two adhesives with ethanol wet bonding technique.
Materials and Methods:
This randomized clinical trial was performed on 36 non-carious cervical lesions in 12 patients restored with composite resin using one of the following approaches: 1. OptiBond FL (Kerr, USA); 2. Clearfil SE Bond (Kuraray, Japan) with enamel etching and 3. Ethanol wet bonding technique with the part of adhesive of OptiBond FL. The clinical success rate was assessed after 24 h, 6, 9 and 12 months according to the United States Public Health Service (USPHS) criteria: Marginal discoloration, marginal defect, retention rate, caries occurrence, and postoperative sensitivity. The tooth vitality was also assessed.
Results:
The retention rate was 100% at baseline and at 6 months follow up for all types of bonding protocols and was 91.67% at 9 and 12 months follow up for ethanol wet bonding group. None of the restorations in three groups showed marginal defects, marginal discoloration or caries occurrence and were vital after 12 months. There was no statistically significant difference between three groups after 12 months follow up (p value = 0.358).
Conclusions:
Composite restorations placed using ethanol wet bonding technique presented equal performance to the other groups.
Keywords: Clearfil SE Bond, clinical success rate, ethanol wet bonding, in vivo, OptiBond FL
INTRODUCTION
There have always been concerns about the long-term durability of composite resin restorations. These restorations may have a short lifespan due to the degradation of resin–dentin interface. Water wet bonding technique was introduced in the beginning of 1990s with the aim of preventing collapse of collagen fibrils after acid etching, improving the penetration of resin into the etched dentin and increasing the durability of resin–dentin bond.[1] The etched dentin is kept moist in this technique. Consequently, manufacturers increased the concentration of ionic and hydrophilic monomers in order to produce more suitable adhesives to bond to water-saturated etched dentin.[2] The increased concentration of acidic and hydrophilic resin monomers may reduce durability of resin–dentin bond due to more water adsorption of hydrophilic resins.[3] In addition to hydrolysis, insufficient penetration of resin into the collagen fibrils due to residual water decreases the durability of resin–dentin bond.[1,4] Recent studies have demonstrated that dentin adhesives cannot replace free and loosely bound water from the interfibrillar spaces, even when resin monomers are able to encapsulate the collagen fibrils.[5,6] Another reason which reduces the resin–dentin bond durability is collagenolysis by endogenous matrix metalloproteinase (MMP) enzymes. Acid etching releases and activates pro-MMPs of the mineralized dentin.[7] Also, acidic resin monomers of self-etch and etch and rinse adhesives increase collagenolytic and gelatinolytic activity in collagen matrix.[8,9] Several approaches are available to overcome these problems and to achieve the main goal of bonding process which is the complete infiltration of resin monomers into the demineralized collagen fibrils and displacement of water of these spaces.[10] Ethanol wet bonding technique is based on the concept of water replacement from interfibrillar and intrafibrillar spaces. There are two versions of the ethanol wet bonding technique. In the progressive method, water is gradually substituted with ethanol by means of ascending ethanol concentration. While in the simplified method ethanol with 100% concentration is applied to water saturated acid etched dentin for one minute prior to the application of ethanol–solvated hydrophobic resin comonomer blend.[5,6] In ethanol wet bonding technique, water is replaced by ethanol which alters the demineralized collagen matrix to a dehydrated and fully extended pattern.[5] The ethanol-suspended collagen matrix has less hydrophilicity and prevents phase separation of hydrophobic resin monomers dissolved in ethanol.[5,11] This technique shrinks the collagen fibrils and enlarges the interfibrillar spaces for hydrophobic monomers to infiltrate the matrix which could extend the longevity of resin–dentin bonds. Li et al. and Sadek et al. demonstrated that ethanol wet bonding displays a bond strength higher than or equal to water wet bonding.[12,13] Also Hosaka et al. showed increased bond strength and durability in ethanol wet bonding compared to water wet bonding.[6] Peumans et al. studied the clinical success rate of OptiBond FL over 13 years and showed a 12% failure rate. They also evaluated the success rate of Clearfil SE Bond over eight years and showed 97% success rate.[14,15] Since the ethanol wet bonding technique has not been compared with other bonding methods clinically, the present study aimed to evaluate and compare the clinical success rate of ethanol wet bonding technique with a three step etch and rinse gold standard adhesive (OptiBond FL) and a two step self-etch gold standard adhesive (Clearfil SE Bond) in one year clinical service. The null hypothesis tested was that there is no difference between the clinical success rates of restorations using different bonding protocols after one year.
MATERIALS AND METHODS
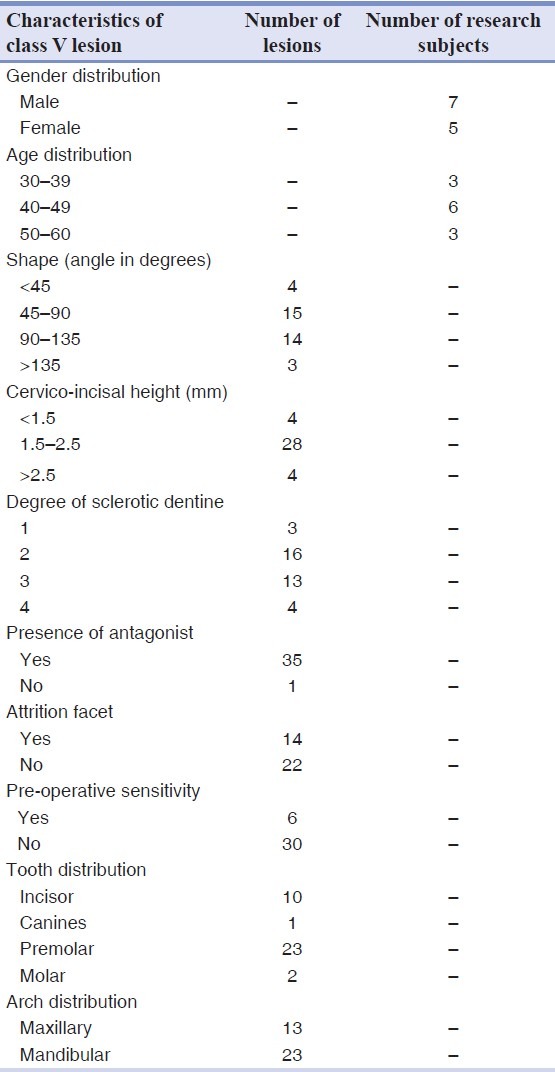
This randomized double blind clinical trial included 12 patients with at least three non-carious cervical lesions (NCCLs). The protocol and consent form were approved by Research Committee of Isfahan University of Medical Sciences and registered in Iranian Registry of Clinical Trials (registration code # IRCT 201111288242N1). The age of the patients varied between 30 and 60 years (seven males and five females). The patients who referred to the Department of Operative Dentistry at Isfahan Dental School were screened to see whether they met the inclusion criteria or not. Patients exhibiting severe or chronic periodontitis, untreated periodontal disease, uncontrolled caries, very poor oral hygiene, heavy bruxism and xerostomia were excluded. Other exclusion criteria were wearing removable prosthesis or orthodontics appliances, receiving bleaching treatments or fluoride supplements. Also breast feeding or pregnant women were excluded. Qualified patients who were systemically healthy and had good oral hygiene with normal occlusion were examined in order to identify NCCLs (abrasion, erosion, abfraction) visually and tacitly. NCCLs with at least 1 mm depth on vital teeth or patient reporting thermal sensitivity or both were selected. The incisal or occlusal margin of the cavity should end in enamel and the cervical margins should end in the dentin or cementum. The degree of the sclerotic dentine was measured according to Swift et al. principles.[16] The lesions were observed from lateral, and the cavities were classified into four groups according to the angle of the cavity (< 45°, 45–90, 90–135, >135°). The gingivo-occlusal or gingivo-incisal heights of the cavities were measured with a periodontal probe. The age, sex, type of tooth, and arch distribution of the NCCLs, degree of sclerotic dentine, cervico-incisal height of the cavities, angle of the cavities and other factors which were recorded in this study are summarized in Table 1. All patients were aware about the nature and objectives of the study and the procedures but blinded to the type of restorative technique. Written informed consents were taken from all patients and oral hygiene instructions were given to all patients prior to treatment.
Table 1.
Distribution of non-carious cervical lesions according to age and sex distribution, shape, cervico-incisal height of the lesion, degree of sclerotic dentin, presence of antagonist, presence of attrition facets, presence of preoperative sensitivity and tooth and arch distribution
Restorative procedures
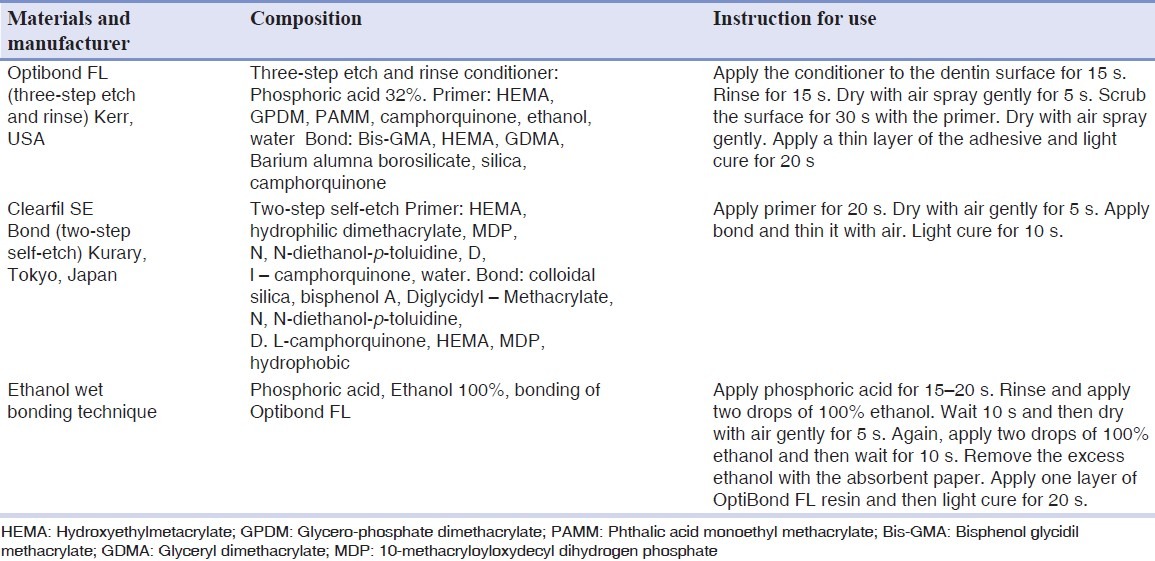
In the clinical phase of the present study, each patient received at least one restoration using the three-step etch and rinse protocol, one restoration using the two-step self-etch protocol with enamel etching and one restoration using the ethanol wet bonding protocol with the part of adhesive of OptiBond FL randomly. The teeth were cleaned with a prophylactic cup and fluoride-free pumice and water followed by rinsing and drying. After local anesthesia administration and shade selection, the teeth were isolated with rubber dam and rinsed with water/air spray. Occlusal or incisal margins were beveled (1 mm with 45° angle) in order to provide more surface area for bonding and to improve esthetics. The adhesives were applied according to the manufacturers’ instructions listed [Table 2]. All cavities were restored with nanohybrid composite resin (Grandio, Voco, Germany) incrementally. Each increment was cured with an LED light curing unit (Demi, Kerr, USA) with an output of 500 mW/cm2 for 40 s. All restorations were finished and polished with finishing diamond burs (Thin taper, Jota, Swiss), polishing disks (OptiDisc, Kerr, Switzerland) and diamond paste (Diamond polish product, 1 μ, Ultradent, USA). All of the restorative procedures were done by a single operator.
Table 2.
Composition and application procedures of the materials used
Clinical evaluation
All patients were recruited for follow-up examinations after 24 h, 6 months, 9 months and 12 months. Two operators whom were blinded about the type of restorative technique examined the restorations separately by use of dental mirror and explorer after tooth prophylaxy and then reached an agreement. Cohen's kappa statistic test which was performed for inter-examiner and intra-examiner calibration was over 72% in all criteria suggesting perfect agreement between examiners. During recalls, the following were examined according to the USPHS criteria: 1. Retention rate, which was evaluated by the presence or loss of the restoration; 2. Enamel or dentine marginal defect in which the restoration margins were examined with explorer and dental mirror; 3. Marginal discoloration, which was clinically observed; 4. Caries occurrence, which was visually inspected and 5. Postoperative sensitivity, which was assessed with application of air spray from a distance of 2–3 cm from the restoration for 3 s while the adjacent teeth were covered by finger. In the present study, the tooth vitality was assessed by a cold spray (Frisco spray, ad-Arztbedarf GmbH, Germany), in addition to the USPHS criteria. Finally the data were analyzed with Chi-square statistical test using SPSS software version 12; P value = 0.05 was considered as significant level.
RESULTS
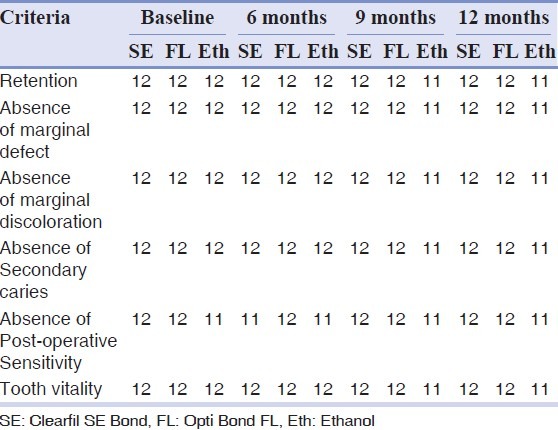
This randomized clinical trial evaluated 12 patients. A total of 36 teeth were restored in which 13 of them were placed in maxillary arch and 23 of them were placed in mandibular arch. Eleven restorations belonged to the anterior segment and 25 restorations belonged to the posterior region (molars and premolars). The results of this study are summarized in Table 3. The recall rate was 100% in 6 months, 9 months and also 12 months. The retention rate at baseline and at 6 months follow up for all three types of bonding protocols was 100%, though the teeth were scored as Alfa for the item “retention rate”. At 9 months follow up, in ethanol wet bonding group, one restoration was lost and the retention rate was 91.67%, although this group was scored as Bravo for the item ‘retention rate’. The comparison of the three types of techniques used showed no significant difference (p value = 0.358). 100% of restorations in three groups continued to be without any enamel or dentin marginal defects after 12 months and were scored Alfa for this item. None of the restored teeth showed marginal discoloration after 12 months (100% without marginal discoloration) and were scored Alfa for this item. None of the restorations in OptiBond FL group showed postoperative sensitivity in different time periods and were scored Alfa for this item. One of the teeth restored with ethanol wet bonding showed postoperative sensitivity after 24 h and was scored as Bravo for this item. After 6 months, two teeth showed postoperative sensitivity, in which one belonged to the ethanol wet bonding group and the other belonged to the Clearfil SE Bond group and were scored Bravo. At 9 months recall, none of the teeth were sensitive, since the restoration of sensitive tooth in ethanol wet bonding group was lost. None of the restored teeth in the three groups showed decay after 12 months (100% without caries); therefore all of them were scored as Alfa for this item. All teeth were vital after 12 months (100%). Therefore there was no statistically significant difference in the clinical success rate between these three groups after 12 months follow up (p value = 0.358).
Table 3.
Number of Evaluated Restorations according to the USPHS criteria in each item
DISCUSSION
Several possible mechanisms may be responsible for the improved durability of resin–dentin bonds made to acid-etched ethanol saturated dentin.[6] It is possible to coax completely hydrophobic monomer to acid-etched dentin with an ethanol wet bonding protocol that theoretically improves resin–dentin bond durability by minimizing water sorption through polymerized hydrophobic adhesive. Ethanol is a bipolar solvent with less hydrogen bond capacity than water, which leads to chemical dehydration of the demineralized collagen network.[1,5,8,17] Subsequently, interfibrillar and intrafibrillar spaces are filled with ethanol which is a better solvent for resin monomers than water. This fact results in better infiltration of resin monomers into the demineralized collagen network that is suspended in ethanol.[6,10,18,19] In water wet bonding technique, the penetration of Bis-GMA in collagen network has a gradual decrease but in ethanol wet bonding, a relatively homogenous distribution of hydrophobic Bis-GMA compounds is seen which inhibits phase separation.[11] Moreover, the interfibrillar collagen spaces contain a hydrogel of proteoglycans, which interferes with resin penetration in the bonding process. Ethanol removes water from these spaces.[5,20] Also ethanol shrinks the fibrils; therefore, the interfibrillar spaces are enlarged and allow more resin penetration.[6,21] The study of Sadek et al. showed that the resin–dentin bond formed with ethanol wet bonding and hydrophobic adhesives do not degrade after 18 months water storage without the presence of MMP inhibitors.[22] In the present study, the clinical success rate of ethanol wet bonding technique in comparison to the OptiBond FL (a three-step etch and rinse adhesive gold standard) and Clearfil SE Bond (a two-step self-etch adhesive gold standard) was evaluated. In this research, the retention rate of the OptiBond FL after 12 months clinical performance was high. Similar high retention rates were recorded for OptiBond FL in Wilder et al. and Boghosian et al. studies.[23,24] Also, Peumans et al. evaluated the clinical success rate of OptiBond FL in non-carious class V cervical lesions over 13 years follow up and stated a high retention rate confirming the bonding efficacy of OptiBond FL.[14] In this study the retention rate of Clearfill SE Bond after 12 months was 100% which is in agreement with the findings of Peumans et al. study. They evaluated the efficacy of Clearfill SE Bond over 8 years clinical performance with and without selective enamel etching and recorded a retention rate of 100% after 12 months for the etched enamel group; however after 8 years, 2 restorations were lost.[15] It can be concluded from their study that the retention rate decreases over the time and longer recalls is needed to get more reliable results. In their study, the percentage of marginal integrity of the etched enamel over one year was 70% while in our study none of the teeth bonded using Clearfill SE Bond showed marginal defect at the same period. Also in their study, after eight years, none of the teeth showed postoperative sensitivity, while in ours after 6 months one tooth that was bonded with Clearfil SE Bond showed postoperative sensitivity. Two-step self-etch adhesives are expected to cause less postoperative sensitivity compared to etch and rinse adhesives.[15] These adhesives do not remove the smear layer and leave the residual smear plugs which results in less dentinal fluid flow.[15] It must be pointed out that in this study similar to the Peumans et al. study, none of the teeth that restored with Clearfill SE Bond showed caries occurrence which is known as the main reason for failure of composite restorations. The better durability of the mild two-step self-etch adhesives such as Clearfil SE Bond is attributed to the use of a more hydrophobic resin layer on top of the hydrophilic self-etch primer and partial dissolution of apatite mineral which causes a protective effect on collagen degradation. In the present study, the ethanol wet bonding technique showed 91.67% retention rate after 12 months; it may be due to high technical sensitivity of ethanol wet bonding. Hosaka et al. studied the durability of resin bonded to water-saturated dentin versus ethanol-saturated dentin and demonstrated that ethanol-saturated dentin had a significantly higher bond strength than water which did not fell over the time. It must be pointed that the selective etching of enamel by use of phosphoric acid was performed in our study, since it improves the durability of bond.[6] Osorio et al. investigated the ethanol wet bonding technique sensitivity by Atomic Force Microscopy (AFM).[5] In both ethanol wet bonding protocols, evaporation of water from the water-saturated dentin resulted in the collapse of the collagen matrix. However, Osorio et al. showed that the collapsed collagen matrix was rehydrated and re-expanded with the aid of 50% water present in the 50% ethanol in the progressive method.[5] Thus the progressive method of ethanol wet bonding may be considered as less technique sensitive protocol; however, it is more time consuming.[5] Both of the mentioned technical methods could be responsible for its extreme technique sensitivity.[5] In the present research, the ethanol wet bonding protocol was compared to OptiBond FL and Clearfill SE bond and showed high clinical success rate in different aspect of USPHS criteria. According to the findings of the present study, there is no statistically significant difference between the clinical success rate of ethanol wet bonding technique with OptiBond FL and Clearfil SE bond after 12 months clinical service and the null hypothesis is accepted. Due to this fact that clinical studies have severe limitations in patient selection, unifying the lesions, unifying the degree of sclerotic dentin, type of restored tooth and occlusal loads which differs for posterior and anterior teeth, method of restoration and the number of increments used for the restoration, much more clinical studies with longer recalls are required in order to obtain reliable and practical results and to present ethanol wet bonding as a method for clinical use. It must be considered that class V lesions are not a good model to correlate the results of the present study to class I/II restorations,[15] or to cavities that are surrounded by enamel margins, since they are primarily dentin lesion and only have a smaller amount of enamel at the incisal side, and also the occlusal loads on class V restorations is not as great for class I/II restorations. Also the location of class V restorations and the easy accessibility to them is another limitation for correlating the results of the present study to class I/II restorations.
CONCLUSION
In the present clinical trial, the clinical success rate of ethanol wet bonding technique was compared to a three-step etch and rinse bonding system (OptiBond FL, Kerr, USA) and a two-step self-etch bonding system (Clearfil SE Bond, Kuraray, Japan) in recalls of 24 h, 6, 9 and 12 months. The difference between the three bonding methods was not statistically significant; therefore, ethanol wet bonding presented equal performance to the OptiBond FL and Clearfil SE Bond adhesives after 12 months of clinical functioning.
ACKNOWLEDGMENTS
This report is supported by Isfahan University of Medical Sciences. The study was registered in Iranian Registry of Clinical Trials (registration code # IRCT 201111288242N1) and was approved by the Medical Ethics and Research Committee of the Isfahan University of Medical Sciences and financially supported by this University (Grant Number #390350).
Footnotes
Source of Support: This report is based on a thesis which was submitted to the School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran, in partial fulfi llment of the requirements for the MSc degree in Operative Dentistry (#390350). The study was approved by the Medical Ethics and Research Office at the Isfahan University of Medical Sciences and financially supported by this University.
Conflict of Interest: The authors declare no conflicts of interest, real or perceived, financial or nonfi nancial.
REFERENCES
- 1.Liu Y, Tjäderhane L, Breschi L, Mazzoni A, Li N, Mao J, et al. Limitations in bonding to dentin and experimental strategies to prevent bond degradation. J Dent Res. 2011;90:953–68. doi: 10.1177/0022034510391799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Landuyt KL, Snauwaert J, De Munck J, Peumans M, Yoshida Y, Poitevin A, et al. Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials. 2007;28:3757–85. doi: 10.1016/j.biomaterials.2007.04.044. [DOI] [PubMed] [Google Scholar]
- 3.Peumans M, Kanumilli P, De Munck J, van Landuyt K, Lambrechts P, van Meerbeek B. Clinical effectiveness of contemporary adhesives: A systematic review of current clinical trials. Dent Mater. 2005;21:864–81. doi: 10.1016/j.dental.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Samimi P, Filsoufi A, Fathpour K. Composite-Dentin bond strength of two adhesives in different conditions. Dent Res J. 2008;4:36–9. [Google Scholar]
- 5.Osorio E, Toledano M, Aguilera FS, Tay FR, Osorio R. Ethanol wet-bonding technique sensitivity assessed by AFM. J Dent Res. 2010;89:1264–9. doi: 10.1177/0022034510376403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hosaka K, Nishitani Y, Tagami J, Yoshiyama M, Brackett WW, Agee KA, et al. Durability of resin-dentin bonds to water-vs. Ethanol-saturated dentin. J Dent Res. 2009;88:146–51. doi: 10.1177/0022034508328910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pashley DH, Tay FR, Yiu C, Hashimoto M, Breschi L, Carvalho RM, et al. Collagen degradation by host-derived enzymes during aging. J Dent Res. 2004;83:216–21. doi: 10.1177/154405910408300306. [DOI] [PubMed] [Google Scholar]
- 8.Nishitani Y, Yoshiyama M, Donnelly AM, Agee KA, Sword J, Tay FR, et al. Effects of resin hydrophilicity on dentin bond strength. J Dent Res. 2006;85:1016–21. doi: 10.1177/154405910608501108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mazzoni A, Pashley DH, Nishitani Y, Breschi L, Mannello F, Tjäderhane L, et al. Reactivation of inactivated endogenous proteolytic activities in phosphoric acid-etched dentine by etch-and-rinse adhesives. Biomaterials. 2006;27:4470–6. doi: 10.1016/j.biomaterials.2006.01.040. [DOI] [PubMed] [Google Scholar]
- 10.Breschi L, Mazzoni A, Ruggeri A, Cadenaro M, Di Lenarda R, De Stefano Dorigo E. Dental adhesion review: Aging and stability of the bonded interface. Dent Mater. 2008;24:90–101. doi: 10.1016/j.dental.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Shin TP, Yao X, Huenergardt R, Walker MP, Wang Y. Morphological and chemical characterization of bonding hydrophobic adhesive to dentin using ethanol wet bonding technique. Dent Mater. 2009;25:1050–7. doi: 10.1016/j.dental.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sadek FT, Braga RR, Muench A, Liu Y, Pashley DH, Tay FR. Ethanol wet-bonding challenges current anti-degradation strategy. J Dent Res. 2010;89:1499–504. doi: 10.1177/0022034510385240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li F, Liu X, Zhang L, Kang J, Chen J. Ethanol-wet Bonding Technique May Enhance the Bonding Performance of Contemporary Etch-and-Rinse Dental Adhesives. J Adhes Dent. 2012;14:113–20. doi: 10.3290/j.jad.a21853. [DOI] [PubMed] [Google Scholar]
- 14.Peumans M, De Munck J, van Landuyt KL, Poitevin A, Lambrechts P, van Meerbeek B. A 13-year clinical evaluation of two three-step etch-and-rinse adhesives in non-carious class-V lesions. Clin Oral Investig. 2012;16:129–37. doi: 10.1007/s00784-010-0481-z. [DOI] [PubMed] [Google Scholar]
- 15.Peumans M, De Munck J, van Landuyt K, Poitevin A, Lambrechts P, van Meerbeek B. Eight-year clinical evaluation of a 2-step self-etch adhesive with and without selective enamel etching. Dent Mater. 2010;26:1176–84. doi: 10.1016/j.dental.2010.08.190. [DOI] [PubMed] [Google Scholar]
- 16.Swift EJ, Jr, Perdigão J, Heymann HO, Wilder AD, Jr, Bayne SC, May KN, Jr, et al. Eighteen-month clinical evaluation of a filled and unfilled dentin adhesive. J Dent. 2001;29:1–6. doi: 10.1016/s0300-5712(00)00050-6. [DOI] [PubMed] [Google Scholar]
- 17.Becker TD, Agee KA, Joyce AP, Rueggeberg FA, Borke JL, Waller JL, et al. Infiltration/evaporation-induced shrinkage of demineralized dentin by solvated model adhesives. J Biomed Mater Res B Appl Biomater. 2007;80:156–65. doi: 10.1002/jbm.b.30580. [DOI] [PubMed] [Google Scholar]
- 18.Vaidyanathan J, Vaidyanathan TK, Yadav P, Linaras CE. Collagen-ligand interaction in dentinal adhesion: Computer visualization and analysis. Biomaterials. 2001;22:2911–20. doi: 10.1016/s0142-9612(01)00038-2. [DOI] [PubMed] [Google Scholar]
- 19.Vaidyanathan TK, Vaidyanathan J. Recent advances in the theory and mechanism of adhesive resin bonding to dentin: A critical review. J Biomed Mater Res B Appl Biomater. 2009;88:558–78. doi: 10.1002/jbm.b.31253. [DOI] [PubMed] [Google Scholar]
- 20.Scott JE, Thomlinson AM. The structure of interfibrillar proteoglycan bridges (‘shape modules’) in extracellular matrix of fibrous connective tissues and their stability in various chemical environments. J Anat. 1998;192:391–405. doi: 10.1046/j.1469-7580.1998.19230391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tay FR, Pashley DH, Kapur RR, Carrilho MR, Hur YB, Garrett LV, et al. Bonding BisGMA to dentin–a proof of concept for hydrophobic dentin bonding. J Dent Res. 2007;86:1034–9. doi: 10.1177/154405910708601103. [DOI] [PubMed] [Google Scholar]
- 22.Sadek FT, Castellan CS, Braga RR, Mai S, Tjäderhane L, Pashley DH, et al. One-year stability of resin-dentin bonds created with a hydrophobic ethanol-wet bonding technique. Dent Mater. 2010;26:380–6. doi: 10.1016/j.dental.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 23.Wilder AD, Jr, Swift EJ, Jr, Heymann HO, Ritter AV, Sturdevant JR, Bayne SC. A 12-year clinical evaluation of a three-step dentin adhesive in noncarious cervical lesions. J Am Dent Assoc. 2009;140:526–35. doi: 10.14219/jada.archive.2009.0220. [DOI] [PubMed] [Google Scholar]
- 24.Boghosian AA, Drummond JI, Lautenschlager E. Clinical evaluation of a dentin adhesive system: 13 year results. J Dent Re, Abst. 2007;86:228. [Google Scholar]


